Abstract
Intertrochanteric femur fracture nonunions are a rare complication that can be difficult to treat with limited evidence regarding treatment options. Revision fixation is typically reserved for well-aligned nonunions with sufficient femoral head bone stock. The most common implant used for revision fixation is a sliding hip screw implant. The use of a short cephalomedullary nail (CMN) for revision fixation has not been previously reported. This article presents a technique for reamed short CMN revision fixation of well-aligned nonunions with sufficient bone stock that is a simpler and potentially less morbid treatment option compared to open procedures with fixed-angle devices. For nonunions with poor femoral head bone stock and/or malaligned fractures, a fixed-angle implant, with or without a valgus osteotomy, may be necessary, while arthroplasty is reserved for nonunions with poor proximal femur bone stock that are not amenable to fixed-angle implant fixation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonunion is a rare complication after intertrochanteric fracture fixation, seen in less than 1% of cases [1,2,3]. The rare incidence and often subtle radiographic findings of intertrochanteric nonunion mean that providers must maintain a high level of suspicion in patients presenting with disabling pain after fracture fixation [4]. Surgical management of intertrochanteric nonunions depends on fracture alignment and femoral bone stock, with revision fixation being preferred for well-aligned fractures with sufficient bone stock [5, 6]. The most commonly reported implant used for isolated revision fixation of intertrochanteric nonunions is a sliding hip screw (SHS) [7, 8]. The use of cephalomedullary nail (CMN) for revision fixation is limited to a few patients in the literature, and furthermore, the use of a short CMN has not been described [5, 9, 10].
The purpose of this paper is to present a technique of revision fixation of well-aligned intertrochanteric nonunions after SHS fixation with sufficient proximal femur bone stock using a reamed short CMN, along with a case series, and a review of the literature.
Patient evaluation
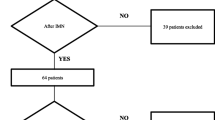
As intertrochanteric nonunions are rare and often present with subtle radiographic findings, surgeons should maintain a high suspicion when patients present with pain and difficulty ambulating several months after intertrochanteric fracture fixation [4]. A computed tomography (CT) scan can be helpful in evaluating these patients if the radiographic findings are inconclusive [5]. Once a femoral nonunion is identified, a laboratory nonunion workup is initiated, including estimated sedimentation rate (ESR), C-reactive protein (CRP), CBC with differential, Albumin, and a 25-hydroxy vitamin D (25-OH Vit D) [11, 12]. If the patient is a tobacco user or malnourished, they should be counseled on tobacco cessation and nutrition intake. If the ESR, CRP, or white blood count (WBC) is elevated, then a suspicion for infection should be maintained and a staged debridement considered prior to any revision surgery [13]. If the 25-OH vitamin D or albumin levels are low, the patient should be prescribed supplementation for correction [11, 14].
Revision fixation, with or without a reamed short CMN, should only be considered in patients with preserved bone stock and preserved alignment of the neck-shaft angle (NSA) [6, 8]. In the event of poor bone stock and/or varus alignment, other treatment options must be considered. These options will be discussed in detail in the discussion.
Technique
Once a nonunion after SHS fixation with a well-aligned NSA and sufficient proximal bone stock has been identified and nonunion risk factors have been addressed, revision fixation with a reamed short CMN can be performed.
The procedure is performed in the supine position on a fracture table. The previous incision from the index surgery is opened and the SHS is removed. Three deep tissue cultures are taken from the removed implant or its immediate vicinity along with a stat frozen pathology specimen to assess for occult infection. If there is no concern for infection, then revision fixation is performed. If purulence is encountered or intraoperative pathology reports acute inflammation (5 or more neutrophils per high powered field or any neutrophils in the setting of elevated inflammatory markers), then staged debridements and empiric antibiotic therapy are indicated prior to fixation [15]. It is the authors’ preference to place antibiotic beads, loaded with vancomycin and tobramycin, and return in 3 to 7 days for bead removal and repeat debridement. If the wound bed appears viable at that time, revision fixation can then be performed.
A wire is placed using a start point just medial to the greater trochanter on the anteroposterior image and centered with the femur on the lateral image (Fig. 1). The opening reamer is then used, ensuring that the opening reamer bypasses the area of fracture nonunion to disrupt the area of nonunion and deliver autologous bone graft to the area. Canal reaming may be necessary, depending on femur bone quality, in order to maximize the nail to femur diameter ratio and avoid iatrogenic fracture with nail insertion. If reaming is necessary, a ball-tip wire is inserted and standard reamers are sequentially used until adequate bony chatter is obtained. A short CMN with a diameter 1.5 mm less than the last canal reamer is then inserted and fixed proximally. An implant with a different cephalomedullary angle is chosen to allow for bony purchase that differs from the previous implant. Once placement is confirmed on biplanar fluoroscopy, the lag screw length that minimizes the tip-apex distance is placed. If there is any traction on the leg, this should be released prior to compressing the nonunion with the lag screw compression sleeve. Following compression, the set screw is inserted and locked in place to maintain the compression. One interlocking screw is then placed through the jig distally. Postoperatively, the patient is made weight-bearing as tolerated and seen at routine follow-up intervals until union.
Fluoroscopic images documenting the a coronal and b sagittal starting points for cephalomedullary nail placement. c Sizing of femoral canal to estimate nail diameter on fluoroscopy. A nail diameter with diaphyseal fit should be used if bone quality allows. d Fluoroscopy demonstrating difference between cephalomedullary nail neck-shaft angle and prior implant. A different neck-shaft-angle should be chosen to maximize bony purchase
Clinical outcomes
Case #1 (Fig. 2) was a 39-year-old female with a history of obesity (body mass index of 41), tobacco smoking (1/2 pack per day), alcohol abuse, and active methadone treatment for a history of heroin abuse who presented eight months after SHS fixation of an intertrochanteric fracture complaining of severe right lateral thigh pain that began three weeks prior. A computed tomography (CT) scan subsequently identified a nonunion. Her WBC, ESR, CRP, and 25-OH vitamin D levels were normal. The patient was counseled on smoking cessation and referred to the hospital’s tobacco treatment program. She was able to reduce her smoking intake but unable to completely stop prior to or after her revision procedure. Due to the sufficient femoral head bone stock and maintained alignment, the nonunion was addressed with hardware removal and insertion of a reamed short intramedullary nail. The operation was complicated by her morbid obesity and the presence of broken screws. The operative time was 4 h and 20 min with an estimated blood loss of 500 ml. Frozen pathology specimens during the procedure did not demonstrate any evidence of acute inflammation (< 5 neutrophils per high power field) and cultures had no growth. At the 15-month follow-up, the fracture was healed and the patient was able to ambulate without pain.
a 8-month follow-up anteroposterior (AP) radiographs after intertrochanteric fracture fixation demonstrate a loose de-rotational screw and two broken screws without apparent nonunion. b The patient complained of debilitating hip pain therefore a computed tomography scan was obtained demonstrating a nonunion. c Due to the maintained alignment and sufficient proximal bone stock, revision fixation was performed with a reamed short cephalomedullary nail. d At the 15-month follow-up, the nonunion was healed and the patient’s pain was resolved
Case #2 (Fig. 3) was a 68-year-old female with a history of Hepatitis C, cirrhosis with ascites, and pancytopenia who presented 5 months after SHS fixation complaining of disabling right hip pain. A CT scan was obtained and demonstrated a nonunion. Her WBC, ESR, CRP, and 25-OH vitamin D levels were normal. She was revised to a reamed short cephalomedullary nail. Operative time was 2 h, and the estimated blood loss was 400 ml. Intraoperative cultures had no growth. At the 16-month follow-up, her fracture was healed and her pain had resolved.
a 5-month follow-up anteroposterior (AP) radiographs after intertrochanteric fracture fixation demonstrating fracture collapse with an intact implant and no apparent nonunion. b The patient complained of debilitating hip pain therefore a computed tomography scan was ordered demonstrating a nonunion. c Due to the preserved alignment and sufficient proximal bone stock, revision fixation was performed with a reamed short cephalomedullary nail. d At the 16-month follow-up, the AP radiograph demonstrated a healed nonunion
Discussion
Sliding hip screw fixation has historically been the standard treatment for stable intertrochanteric femur fractures [1, 2]. Nonunion after SHS fixation is rare, occurring in less than 1% of cases and most commonly attributable to unstable fracture patterns, poor bone quality, patient comorbidities, or suboptimal reduction or implant position [1,2,3,4]. In a large randomized controlled study of intertrochanteric femur fractures, the nonunion rate was reported as 0.4% and 0.8% for CMN and SHS fixation [1]. When a nonunion does occur, the radiographic findings can be subtle, such as the cases presented in this article, with a clinical presentation that is usually marked by debilitating pain [4].
Due to the low incidence of intertrochanteric nonunions, the evidence for various treatment options in the literature is limited (Table 1) with union rates ranging from 80 to 100%. Revision fixation, as demonstrated in the above cases, is an option for nonunions that remain well-aligned with sufficient femoral head bone stock. The implant used for revision fixation has varied in the literature but most commonly has been reported to be SHS. To date, only 7 nonunions treated with CMN (none reportedly involving short CMN) have been reported in the literature, all of which are part of larger series with little focus on the specific details of each case [5, 6, 9, 10]. The purpose of this article was to describe the workup, indications, and technique for short CMN fixation of intertrochanteric nonunions in order to provide guidance that does not currently exist in the literature. Compared to other fixation options, a short CMN provides a relatively simple and minimally invasive solution.
It is essential to understand in what setting a short CMN can be used to treat an intertrochanteric nonunion. In the setting of insufficient central/superior femoral head bone stock, a fixed-angle device, such as a blade plate, that gains purchase in the inferior aspect of the femoral head is a more appropriate device. When nonunion occurs in the setting of varus malignment or vertically oriented fracture lines, a valgus producing osteotomy prior to fixation with a fixed-angle device is a preferred option to convert shear force across the fracture site to compressive force [7, 10].
Conclusion
Intertrochanteric fracture nonunions are rare complications that can be difficult to treat. This article reports a technique of reamed short CMN revision fixation for well-aligned nonunions with sufficient bone stock that is a simpler and potentially less morbid treatment option compared to open procedures with fixed-angle devices.
References
Parker MJ (2017) Sliding hip screw versus intramedullary nail for trochanteric hip fractures; a randomised trial of 1000 patients with presentation of results related to fracture stability. Injury 48:2762–2767. https://doi.org/10.1016/j.injury.2017.10.029
Arirachakaran A, Amphansap T, Thanindratarn P et al (2017) Comparative outcome of PFNA, Gamma nails, PCCP, Medoff plate, LISS and dynamic hip screws for fixation in elderly trochanteric fractures: a systematic review and network meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 27:937–952. https://doi.org/10.1007/s00590-017-1964-2
Hwang J, Hadeed M, Sapp T et al (2020) Varus displacement of intertrochanteric femur fractures on injury radiographs is associated with screw cutout. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-020-02820-1
Haidukewych GJ, Berry DJ (2005) Salvage of failed treatment of hip fractures. J Am Acad Orthop Surg 13:101–109. https://doi.org/10.5435/00124635-200503000-00003
Haidukewych GJ, Berry DJ (2003) Salvage of Failed Internal Fixation of Intertrochanteric Hip Fractures. Clin Orthop Relat Res 412:184–188. https://doi.org/10.1097/01.blo.0000071753.41516.27
Xue D, Yu J, Zheng Q et al (2017) The treatment strategies of intertrochanteric fractures nonunion: An experience of 23 nonunion patients. Injury 48:708–714. https://doi.org/10.1016/j.injury.2017.01.042
Dhammi IK, Jain AK, Singh AP et al (2011) Primary nonunion of intertrochanteric fractures of femur: An analysis of results of valgization and bone grafting. Indian J Orthop 45:514–519. https://doi.org/10.4103/0019-5413.87122
Said GZ, Farouk O, El-Sayed A, Said HG (2006) Salvage of failed dynamic hip screw fixation of intertrochanteric fractures. Injury 37:194–202. https://doi.org/10.1016/j.injury.2005.09.011
Mariani EM, Rand JA (1987) Nonunion of intertrochanteric fractures of the femur following open reduction and internal fixation. Results of second attempts to gain union. Clin Orthop Relat Res 218:81–89
Min BW, Lee KJ, Oh JK et al (2020) Salvage treatment of failed internal fixation of intertrochanteric fractures: what factors determine the failure of treatment? Injury 51:367–371. https://doi.org/10.1016/j.injury.2019.12.004
Brinker M, O’Connor D, Monla Y, Earthman T (2007) Metabolic and endocrine abnormalities in patients with nonunions. J Orthop Trauma 21:557–570. https://doi.org/10.1097/BOT.0B013E31814D4DC6
Govaert GAM, Kuehl R, Atkins BL et al (2020) Diagnosing fracture-related infection: current concepts and recommendations. J Orthop Trauma 34:8–17. https://doi.org/10.1097/BOT.0000000000001614
Metsemakers WJ, Fragomen AT, Moriarty TF et al (2020) Evidence-based recommendations for local antimicrobial strategies and dead space management in fracture-related infection. J Orthop Trauma 34:18–29. https://doi.org/10.1097/BOT.0000000000001615
Robertson DS, Jenkins T, Murtha YM et al (2015) Effectiveness of vitamin D therapy in orthopaedic trauma patients. J Orthop Trauma 29:e451–e453. https://doi.org/10.1097/BOT.0000000000000366
Simpson AHRW, Wood MK, Athanasou NA (2002) Histological assessment of the presence or absence of infection in fracture non-union. Injury 33:151–155. https://doi.org/10.1016/S0020-1383(01)00078-X
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors have no specific disclosures related to this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The institutional review board approved this study. Due to the retrospective nature of this work, informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
M. Mares, ., Hadeed, M.M. & Parry, J.A. Treatment of intertrochanteric nonunion after sliding hip screw fixation with a short cephalomedullary nail. Eur J Orthop Surg Traumatol 32, 1415–1421 (2022). https://doi.org/10.1007/s00590-021-03108-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-03108-8