Abstract
Background
Total joint arthroplasties aim to improve quality of life from joint-related pain. Jehovah’s Witnesses refuse blood products due to their religious beliefs. Surgeons may be reluctant to perform arthroplasty procedures on these patients for fear of uncontrolled bleeding. However, we hypothesize that through preoperative optimization, arthroplasty can be performed safely.
Methods
We retrospectively reviewed 184 total joint arthroplasties in Jehovah’s Witnesses between 2011 and 2019. Each patient was enrolled in the institutions’ Bloodless Medicine program. Hemoglobin levels were recorded through standard laboratory testing while in the hospital. Primary outcomes were changes in preoperative and postoperative hemoglobin measures, short-term outcomes measures, and complications.
Results
A total of 103 total knee arthroplasties (8 revisions) and 81 total hip arthroplasties (5 revisions) were performed. Hemoglobin drift was 2.5 ± 1.0 for primary TKA and 2.6 ± 1.3 for primary THA (p = 0.570). Hemoglobin drift was 1.9 ± 0.9 for revision TKA and 1.9 ± 0.2 for revision THA (p = 0.990). Only 2.7% of patients met the transfusion requirement of 7 g/dL. The major complication rate for the cohort was 1.6% systemic and 4.9% local, respectively, with no mortalities. The overall readmission rate was 2.7%.
Conclusion
To our knowledge, this is the largest reported sample of Jehovah’s Witness patients undergoing total joint arthroplasty. Postoperative hemoglobin values did not prompt additional intervention in the overwhelming majority of patients, and complication rates were acceptable. Our data suggest that primary arthroplasty is safe in the Jehovah's Witness population. Additionally, we show preliminary evidence that revision arthroplasty is safe in Jehovah’s Witness patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a chronic disease characterized by the gradual loss of articular cartilage [1]. OA is a significant cause of both hip and knee disability, as well as the most common indication for joint replacement procedures in elderly patients [2,3,4]. In 2013, OA was the second most expensive medical condition treated at US hospitals, costing over $16.5 billion [5]. Total joint arthroplasty, including total knee arthroplasty (TKA) and total hip arthroplasty (THA), aims to improve functional status and quality of life [6]. It is projected that the geriatric population in the USA (adults 65 +) will increase 192% by 2060 [7]. With this knowledge, it is expected that the incidence of both TKA and THA will increase dramatically in the next few decades [8,9].
Historically, the need for intraoperative and postoperative blood transfusion following THA and TKA has been high [10,11]. However, transfusions in patients undergoing total joint arthroplasty have decreased significantly in recent years [12]. This is thought to be a result of the addition of intraoperative tranexamic acid (TXA), lower hemoglobin transfusion threshold levels, standardized pain regimen, and early mobilization immediately following surgery [13]. At our institution, the rate of transfusion since 2016 has averaged 1.6% for all primary TKA and 1.3% for all primary THA.
Jehovah’s Witnesses are members of a Christian movement with over 8.5 million active members worldwide [14]. This group refuses blood products believing that the soul of a person is inherently linked to their blood, thus unable to be consumed: Genesis 9:4 states “Only you shall not eat flesh with its life, that is, its blood” [15]. Ideologically, this group is prohibited from receiving transfusions of either whole or particulate blood products, including autologous blood transfusions, believing their refusal of blood is based on God’s Word of the Bible [16]. Given this patient group’s strong religious hesitation to receive blood products, surgeons may be reluctant to perform total joint arthroplasty for fear of uncontrolled bleeding and poor outcomes [17].
Although the risks persist, there is a growing body of evidence suggesting that TKA and THA can be performed safely in the Jehovah’s Witness population [17,18]. At our institution, a Bloodless Medicine program was established in 2011 that works to pre- and postoperatively optimize patients who prefer to not receive blood transfusions. Given the existence of such protocols, we hypothesize that total joint arthroplasty can safely be performed with a minimal number of individuals meeting criteria for transfusion.
Methods
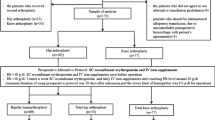
This is a retrospective review of 184 self-identified Jehovah’s Witness patients who underwent total joint arthroplasty from one of eight surgeons at either a single tertiary care academic center or a community hospital with the same academic affiliation between 2011 and 2019. IRB approval was obtained for this study. The IRB did not require written informed consent due to the retrospective nature of this chart review. Prior to the procedure, each patient was enrolled in the institution’s Bloodless Medicine program. This group acts as a support system throughout the preoperative and postoperative periods, ensuring proper preoperative optimization for all patients. The Bloodless Medicine interventions did not differ between the two surgery sites. Patient demographics and ASA class designation in the preoperative period were recorded for the majority of patients. In addition, postoperative Internal Medicine consultation, disposition location, and need for readmission were collected for all patients. An Internal Medicine consult was deemed necessary if the patient had a medical condition that the primary orthopedic team was not comfortable managing or had multiple comorbidities that required active intervention.
As part of the Bloodless Medicine approach to preoperative optimization, each patient was enrolled in a protocol including a complete blood count (CBC) obtained 6–12 weeks prior to the scheduled operation. [19,20,21] Pediatric tubes were used to minimize blood loss. Between 2004 and 2014, the protocol for anemia management was initiated for any patient with a preoperative hemoglobin of 12 g/dL or less. Intravenous or intraarticular tranexamic acid was used starting in 2014, allowing a drop in the hemoglobin threshold to 10 g/dL due to a resultant decrease in intraoperative blood loss. Patients that fell below these hemoglobin thresholds were treated with intravenous iron (iron sucrose) 200 mg and erythropoietin (epoetin alfa—Procrit) 40,000 units for one to three treatment doses, depending on their hemoglobin level. On the day of the procedure, a preoperative CBC was drawn to obtain a baseline value. Daily blood values were collected during the patient’s hospital admission. Nadir (lowest value recorded during treatment course), discharge, and drift (change in blood value between the preoperative period and discharge) were analyzed for both total hip and total knee arthroplasty groups. Patients were divided into cohorts based upon arthroplasty location and whether it was a primary or revision arthroplasty.
Statistical analysis
Primary outcome measures were changes in preoperative and postoperative hemoglobin values. Secondary outcomes included the need for Internal Medicine consultation postoperatively, disposition plans, complication rates, and need for readmission. Complications were divided into systemic versus local issues and subdivided into major and minor for each. Data for primary TKA and THA were compared through t test analysis and corrected via Bonferroni’s method. This manuscript adheres to the applicable Equator guidelines.
Results
A total of 184 patients were included in the retrospective cohort; 81 patients underwent THA (five revisions), while 103 underwent TKA (eight revisions) (Table 1). Patient demographics and hemoglobin parameters are detailed in Tables 2, 3 and 4. Our patients had an average age of 64.0 ± 8.9 years and an average BMI of 34.0 ± 7.2 kg/m2. Length of stay (LOS) following the procedures ranged from 1 to 10 days, with an average of 2.9 ± 1.3. Sixty-six patients (35.9%) were ASA class II, and 81 (44.0%) were ASA class III. An additional 37 patients (20.1%) who did not have ASA class identified in the electronic medical record were included in other analysis.
19.6% of patients required an Internal Medicine consult postoperatively. In total, 122 of the patients were discharged home, with or without home physical therapy, and 62 were discharged to an acute or subacute rehabilitation facility (66.3% vs. 33.7% respectively). Five of the total patient cohort were re-admitted following discharge. Three readmissions were within 90 days (C. difficile infection, deep infection, and superficial cellulitis), while two were delayed: one patient at 4 months and another at 8 months (deep infection and dislocation, respectively). The 30-day readmission rate was 1.1%, and the 90-day readmission rate was 1.6%. The overall readmission rate for our cohort was 2.7%.
When comparing the two primary arthroplasty populations, there was no significant difference in age between knee and hip arthroplasty patients (64.3 ± 8.1 vs. 63.4 ± 9.5; p = 0.505) (Table 3). There was a significantly higher BMI (35.4 ± 7.4 vs. 32.3 ± 6.4; p = 0.004) and length of stay (3.1 ± 1.3 vs. 2.6 ± 1.0; p = 0.006) in the TKA population compared to the THA population. The average preoperative hemoglobin value for TKA patients was 12.7 ± 1.2, which was not significantly different from that of THA patients at 13.0 ± 1.2 (p = 0.106). Postoperative hemoglobin levels were also similar in the two populations (TKA: 10.8 ± 1.3 vs THA: 11.1 ± 1.4; p = 0.149). There was a slightly larger decrease in hemoglobin levels for THA patients (1.9 ± 0.9) compared to TKA patients (1.7 ± 0.7); however, this difference was not significant (p = 0.104). Nadir hemoglobin levels during hospitalization were similar between the two cohorts (p = 0.163). TKA patients had a slightly lower hemoglobin level at discharge (10.1 ± 1.3) compared to THA patients (10.5 ± 1.5); however, this difference was not found to be significantly different (p = 0.064). Hemoglobin drift was similar for TKA and THA patients (2.5 ± 1.0 vs. 2.6 ± 1.3, respectively; p = 0.570).
There were no significant differences found between the TKA and THA revision arthroplasty cohorts in regard to demographics or hemoglobin values. There was an insignificantly increased age in the revision THA patients as compared to revision TKA patients (71.0 ± 12.9 vs. 61.8 ± 10.1; p = 0.178) (Table 4). Similar to the primary arthroplasty cohorts, revision THA patients had a lower BMI (30.0 ± 7.5) than revision THA patients (36.9 ± 8.8); however, this difference was not significant (p = 0.175). The average length of stay was insignificantly longer in revision THA as compared to revision TKA populations (p = 0.166). While comparing hemoglobin data, the preoperative and postoperative hemoglobin values were both slightly higher in the TKA patients than in the THA patients (13.4 ± 1.1 vs. 11.6 ± 3.4; p = 0.185 and 11.5 ± 1.4 vs. 10.0 ± 1.8; p = 0.119, respectively). Similarly, the nadir (10.6 ± 1.6 vs. 9.0 ± 2.7; p = 0.202) and discharge (10.7 ± 1.5 vs. 9.4 ± 2.9; p = 0.305) hemoglobin values were higher in the TKA population as compared to the THA population, respectively.
There were 30 postoperative complications noted in our cohort of 184 patients (Table 5). 46.7% of the complications were systemic in nature. The rate of major systemic complications was 1.6%; one patient had a pulmonary embolism (PE), and two patients had new onset acute kidney injuries. The rate of minor systemic complications was 6.0%: five patients with postoperative anemia, one with a deep venous thrombosis (DVT), two with postoperative nausea and vomiting, one with a C. difficile infection, one with postoperative atelectasis and one with a superficial venous thrombosis.
43.3% of the total complications were local in nature. The rate of major local complications was 4.9%: two patients with postoperative peripheral nerve injuries, one with significant intraoperative vascular injury requiring vascular surgery consult, two deep infections, one periprosthetic fracture, two patients with aseptic loosening, and two dislocations. The rate of minor local complications was 2.2%: three hematomas and one patient with persistent wound drainage postoperatively. Three (1.6%) patients had skin blisters with superficial wound infection in the postoperative period.
Discussion
Performing total joint arthroplasty in the Jehovah’s Witness population can be clinically and ethically challenging given the potential for blood loss and subsequent transfusion need. However, among our cohort of patients, our findings demonstrate that total joint arthroplasty (THA and TKA) is safe in the Jehovah’s Witness population. All but two patients in our study had a hemoglobin over the desired 10 g/dL threshold used by our institution’s Bloodless Medicine group at the time of surgery. One of these patients (9.2 g/dL) was a total hip revision for a periprosthetic fracture. The other patient (9.6 g/dL) was an otherwise healthy individual undergoing total hip arthroplasty. Similarly, only two patients had immediate postoperative hemoglobin values below the typical transfusion threshold of 7.0 g/dL. The patient with the lowest postoperative hemoglobin (6.5 g/dL) had a vascular complication requiring an intraoperative vascular consultation, likely accounting for the significant drop. She did not require intervention for her anemia and was asymptomatic. The other patient had a postoperative day zero hemoglobin of 6.8 g/dL despite an uncomplicated operation. However, on postoperative days one and two, the recorded hemoglobin values were 11.7 g/dL and 10.8 g/dL, respectively, without intervention. This suggests the initial value was in error. Three additional patients had nadir hemoglobin levels under 7 g/dL during the course of their admission; one of these patients underwent a revision THA for a previously infected implant. The other two patients had significant medical comorbidities, as one had cardiomyopathy with ejection fraction below 30%, and the other a failed renal transplant requiring hemodialysis.
At our institution, most patients receive blood transfusions for hemoglobin levels below 7.0 g/dL. With this threshold for transfusion, five (2.7%) of the 184 patients in this cohort would have received a blood transfusion during their hospital course. This is well below the currently accepted average number of patients that require transfusion following THA and TKA, at 9% and 4.5%, respectively [22]. Specifically at our institution, the overall transfusion rates for primary THA and TKA are 1.3% and 1.6%, respectively, during their hospital stay. As such, our data suggest that the Jehovah’s Witness arthroplasty is similar to the non-Jehovah’s Witness population in regard to meeting requirements for transfusion.
Additionally, in this cohort, the average drop in pre- to postoperative hemoglobin levels was under 2 g/dL for both primary and revision THA and TKA patients. This is below the currently reported values for blood loss in both arthroplasty populations [23,24,25,26]. THA has historically been associated with greater blood loss than TKA; however, our findings showed an insignificant difference in blood loss between primary and revision THA and TKA populations [27]. The decreased blood loss recorded in our population of Jehovah’s Witnesses, as well as the resultant decrease in blood transfusion as compared to prior reports, suggests that primary and revision arthroplasty procedures are safe in the blood product-refusing population. This may be attributed to the work of our institution’s Bloodless Medicine group in optimizing each patient’s preoperative status, minimizing perioperative blood loss, and minimizing postoperative phlebotomy through pediatric tubes. This study suggests that the inclusion of a Bloodless Medicine protocol in arthroplasty procedures may help minimize transfusion requirements in this patient population.
At discharge, 66.3% of our patients returned home with home services as opposed to transitioning to a rehabilitation facility. This demonstrates that nearly two-thirds of the patient population followed the expected postoperative course [28]. Recent studies indicate that admission to a skilled nursing facility (SNF) for rehabilitation following primary TKA and THA is 29.9% and 35.9%, respectively [29,30]. Given that the present cohort includes revision arthroplasty, thereby increasing the expected SNF admission rate, it appears that our inpatient rehabilitation rate of 33.7% is well within the accepted range and is consistent with the rate (12% to 28% for primary THA and TKA) for the entire patient population at our institution [31].
We found a systemic complication rate of 1.6% for major and 6.0% for minor complications. There were a similar number of both major and minor systemic complications following primary THA and TKA. One primary TKA patient was found to have a PE without a concurrent DVT on bilateral lower extremity duplex. Another patient in the TKA cohort was found to have a DVT postoperatively and was treated with an outpatient anticoagulation regimen. Unfortunately, DVTs are a known complication associated with arthroplasty, and this cohort’s DVT rate of 0.5% is within the range of currently reported values [32,33,34]. There were also 4 patients (2 primary TKA and 2 primary THA) with anemia who would have required a transfusion (under 7.0 g/dL). Looking at revision arthroplasty, patients undergoing revision THA had a higher number of systemic complications than that of the revision TKA population. Two of the revision THA patients developed a postoperative acute kidney injury and one revision THA patient had severe anemia. Interestingly, there were no systemic complications in the revision TKA cohort. It is worth mentioning that the low number of patients in the revision cohort makes it hard to draw definitive conclusions from their complication data.
Local complications associated with the procedures were slightly more prevalent in the primary and revision TKA patients. One patient in the primary TKA cohort had a significant vascular injury, requiring intraoperative vascular surgery consultation. This patient was anemic postoperatively likely due to the vascular injury, but their final length of stay was not outside of the average for TKA patients. Two patients (1 primary THA and 1 revision TKA) had a postoperative joint infection that required readmission and intervention. The TKA patient was readmitted 25 days postoperatively for an irrigation and debridement with a polyethylene liner exchange, while the THA patient was readmitted 4 months later for a two-stage revision. The 1.1% infection rate in this cohort is on the upper end of normal (0.5–1.0%) for prosthetic joint infection according to the current literature [35,36]. Other notable complications were a periprosthetic fracture in a revision THA patient that was treated nonoperatively, aseptic loosening in two TKA patients (one revision and one primary), and one postoperative dislocation in a revision TKA. Three TKA patients (one primary and two revisions) also presented with postoperative hematomas that led to a restriction in range of motion but did not require operative intervention.
There were five readmissions (three primary TKAs, one revision TKA and a revision THA) reported during the course of this study. Two of these readmissions (both primary arthroplasty patients) were within 30 days postoperatively; these included one with intractable pain four days postoperatively and one with a deep infection 25 days postoperatively. Our 30-day readmission rate was 1.1%. The 1.1% 30-day readmission rate is well below previously reported values of 4.2–5.8% [37,38,39]. Another readmission within the 90-day postoperative period was a primary TKA patient with newly diagnosed C. difficile at 45 days postoperatively. Our 90-day admission rate was 1.6%, which is also significantly below the reported values of 4.7–8.8% [39,40]. The other two readmissions outside of the 90-day period included one deep infection four months postoperatively in a revision THA patient who required irrigation and debridement, and a revision TKA patient with a dislocated knee eight months postoperatively, requiring revision components. Our overall readmission rate was 2.7% for arthroplasty patients in this cohort.
The primary strength of this study lies in its large sample of Jehovah’s Witness patients receiving total joint arthroplasty; to our knowledge, this is the largest cohort ever reported. In addition, our study includes the novel addition of a Bloodless Medicine group in the perioperative period to help prepare patients for surgery. The coordination between surgeon and Bloodless Medicine to ensure optimal outcomes for each patient has been cultivated over many years and is unique to our cohort.
There are limitations to this study; most notably its inclusion of only Jehovah’s Witness patients. As a result, it is unrepresentative of the entire population refusing blood products. Additionally, it is limited in its retrospective nature, as we were unable to report mid and long-term outcomes. Furthermore, because of our small revision cohorts, results comparing differences between the primary and revision arthroplasty patients are limited as is extrapolation of data from the revision cohorts independently. Another limitation was the lack of standardization in preoperative anticoagulation use for our patients. Finally, there were a few patients in the THA and TKA cohorts that did not have preoperative hemoglobin values recorded. All patients had postoperative hemoglobin values. This resulted in delta and drift values that are slightly skewed from what would be expected as they were only applicable to patients with both preoperative and postoperative hemoglobin values.
In conclusion, this is the largest reported cohort of Jehovah’s Witness patients receiving total joint arthroplasty. We present primary arthroplasties as well as revisions of both TKA and THA. As a whole, postoperative hemoglobin values did not meet transfusion criteria in the overwhelming majority of patients. As such, we believe arthroplasty can be performed safely in the Jehovah’s Witness population despite their inability to receive blood products. However, future studies with increased number of revision Jehovah’s Witness patients are needed to elucidate the role of revision arthroplasty in this population as we recognize our cohort numbers are difficult to interpret and make clinical decisions on given their small size.
Code availability
Not Applicable.
Data availability
Not Applicable.
References
Xia B, Chen Di, Zhang J, Hu S, Jin H, Tong P (2014) Osteoarthritis pathogenesis: a review of molecular mechanisms. Calcif Tissue Int 95(6):495–505. https://doi.org/10.1007/s00223-014-9917-
Zhang Y, Jordan JM (2010) Epidemiology of osteoarthritis [published correction appears in Clin Geriatr Med. 2013 May;29(2):ix]. Clin Geriatr Med 26(3):355–369. https://doi.org/10.1016/j.cger.2010.03.001
Hamel MB, Toth M, Legedza A, Rosen MP (2008) Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med 168(13):1430–1440
Gademan MG, Hofstede SN, Vliet Vlieland TP, Nelissen RG, Marang-van de Mheen PJ (2016) Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Musculoskelet Disord 17(1):463. https://doi.org/10.1186/s12891-016-1325-z
CM Torio MBJ Statistical Brief #204 (2016) National inpatient hospital costs: the most expensive conditions by Payer, 2013 Rockville agency for healthcare research and quality MD
Bottai V, Dell’Osso G, Celli F et al (2015) Total hip replacement in osteoarthritis: the role of bone metabolism and its complications. Clin Cases Miner Bone Metab 12(3):247–250. https://doi.org/10.11138/ccmbm/2015.12.3.247
https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html [Accessed 16 February 2020]
Sloan M, Premkumar A, Sheth NP (2018) Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am 100(17):1455–1460
Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S (2017) Projected increase in total knee arthroplasty in the United States—an alternative projection model. Osteoarthr Cartil 25(11):1797–1803
Slover J, Lavery JA, Schwarzkopf R, Iorio R, Bosco J, Gold HT (2017) Incidence and risk factors for blood transfusion in total joint arthroplasty: analysis of a statewide database. J Arthroplasty 32(9):2684
Kapoor A, Ellis A, Shaffer N et al (2017) Comparative effectiveness of venous thromboembolism prophylaxis options for the patient undergoing total hip and knee replacement: a network meta-analysis. J Thromb Haemost 15(2):284–294. https://doi.org/10.1111/jth.13566
Burnett RA, Bedard NA, DeMik DE, Gao Y, Liu SS, Callaghan JJ (2017) Recent trends in blood utilization after revision hip and knee arthroplasty. J Arthroplasty 32(12):3693–3697. https://doi.org/10.1016/j.arth.2017.08.038
De Burlet K, Windall J, Barton C, Gudimetla V, Duckett S (2016) Ehanced recovery protocol reduces transfusion requirements and hospital stay in patients undergoing an elective arthroplasty procedure. Adv Orthop Surg. https://doi.org/10.1155/2016/9846910
https://www.jw.org/en/jehovahs-witnesses/faq/how-many-jw-members/ [Accessed 16 February 2020]
https://wol.jw.org/en/wol/d/r1/lp-e/1101977010#h=387 [Accessed 16 February 2020]
https://www.transfusionguidelines.org/transfusion-handbook/12-management-of-patients-who-do-not-accept-transfusion/12-2-jehovah-s-witnesses-and-blood-transfusion [Accessed 16 February 2020]
Harwin SF, Issa K, Naziri Q, Johnson AJ, Mont MA (2013) Results of primary total knee arthroplasty in Jehovah’s witness patients. J Arthroplasty 28(1):49–55
Wolfson TS, Novikov D, Chen KK et al (2020) Total knee arthroplasty is safe in Jehovah’s witness patients-A 12-year perspective. J Knee Surg 33(1):34–41. https://doi.org/10.1055/s-0038-1676372
Chaturvedi S, Koo M, Dackiw L, Koo G, Frank SM, Resar LMS (2019) Preoperative treatment of anemia and outcomes in surgical Jehovah’s witness patients. Am J Hematol 94(2):E55–E58. https://doi.org/10.1002/ajh.25359
Scharman CD, Burger D, Shatzel JJ, Kim E, DeLoughery TG (2017) Treatment of individuals who cannot receive blood products for religious or other reasons. Am J Hematol 92(12):1370–1381. https://doi.org/10.1002/ajh.24889
Suh YS, Nho JH, Choi HS, Ha YC, Park JS, Koo KH (2016) A protocol avoiding allogeneic transfusion in joint arthroplasties. Arch Orthop Trauma Surg 136(9):1213–1226. https://doi.org/10.1007/s00402-016-2516-7
Bedard NA, Pugely AJ, Lux NR, Liu SS, Gao Y, Callaghan JJ (2017) Recent trends in blood utilization after primary hip and knee arthroplasty. J Arthroplasty 32(3):724–727
Cundy WJ, Theodoulou A, Ling CM, Krishnan J, Wilson CJ (2017) Blood loss in total knee arthroplasty. J Knee Surg 30(5):452–459. https://doi.org/10.1055/s-0036-1592147
Hu Y, Li Q, Wei BG et al (2018) Blood loss of total knee arthroplasty in osteoarthritis: an analysis of influential factors. J Orthop Surg Res 13(1):325. https://doi.org/10.1186/s13018-018-1038-0
Ugbeye ME, Lawal WO, Ayodabo OJ, Adadevoh IP, Akpan IJ, Nwose U (2017) An evaluation of intra- and post-operative blood loss in total hip arthroplasty at the national orthopaedic hospital. Lagos Niger J Surg 23(1):42–46. https://doi.org/10.4103/1117-6806.205750
Sucher MG, Giordani M, Figoni A, Nedopil AJ (2016) Peri-operative blood-loss after total hip arthroplasty can be significantly reduced with topical application of epsilon-aminocaproic acid. Int Orthop 40(10):2019–2023. https://doi.org/10.1007/s00264-015-3103-1
Carling MS, Jeppsson A, Eriksson BI, Brisby H (2015) Transfusions and blood loss in total hip and knee arthroplasty: a prospective observational study. J Orthop Surg Res 10:48. https://doi.org/10.1186/s13018-015-0188-6
Tarity TD, Swall MM (2017) Current trends in discharge disposition and post-discharge care after total joint arthroplasty. Curr Rev Musculoskelet Med 10(3):397–403. https://doi.org/10.1007/s12178-017-9422-7
Schwarzkopf R, Ho J, Quinn JR, Snir N, Mukamel D (2016) Factors influencing discharge destination after total knee arthroplasty: a database analysis. Geriatr Orthop Surg Rehabil 7:95–99. https://doi.org/10.1177/2151458516645635
L’Hommedieu CE, Gera JJ, Rupp G, Salin JW, Cox JS, Duwelius PJ (2016) Impact of anterior vs posterior approach for total hip arthroplasty on post-acute care service utilization. J Arthroplast 31:73–77. https://doi.org/10.1016/j.arth.2016.06.057
Nichols CI, Vose JG (2016) Clinical outcomes and costs within 90 days of primary or revision total joint arthroplasty. J Arthroplasty 31(7):1400-1406.e3. https://doi.org/10.1016/j.arth.2016.01.022
Parvizi J, Mui A, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH (2007) Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Joint Surg Am 89(1):27–32. https://doi.org/10.2106/JBJS.E.01443
Dua A, Desai SS, Lee CJ, Heller JA (2017) National Trends in deep vein thrombosis following total knee and total hip replacement in the United States. Ann Vasc Surg 38:310–314. https://doi.org/10.1016/j.avsg.2016.05.110
Loh JLM, Chan S, Wong KL, de Mel S, Yap ES (2019) Chemoprophylaxis in addition to mechanical prophylaxis after total knee arthroplasty surgery does not reduce the incidence of venous thromboembolism. Thromb J 17:9. https://doi.org/10.1186/s12959-019-0200-1
Chun KC, Kim KM, Chun CH (2013) Infection following total knee arthroplasty. Knee Surg Relat Res 25(3):93–99. https://doi.org/10.5792/ksrr.2013.25.3.93
Mallon CM, Gooberman-Hill R, Moore AJ (2018) Infection after knee replacement: a qualitative study of impact of periprosthetic knee infection. BMC Musculoskelet Disord 19(1):352. https://doi.org/10.1186/s12891-018-2264-7
Bottle A, Loeffler MD, Aylin P, Ali AM (2018) Comparison of 3 types of readmission rates for measuring hospital and surgeon performance After primary total hip and knee arthroplasty. J Arthroplasty 33(7):2014-2019.e2. https://doi.org/10.1016/j.arth.2018.02.064
Pugely AJ, Callaghan JJ, Martin CT, Cram P, Gao Y (2013) Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty 28(9):1499–1504. https://doi.org/10.1016/j.arth.2013.06.03
Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT (2016) Which hospital and clinical factors drive 30- and 90-day readmission after TKA? J Arthroplasty 31(10):2099–2107. https://doi.org/10.1016/j.arth.2016.03.045
Elmallah RK, Cherian JJ, Amin H, Jauregui JJ, Pierce TP, Mont MA (2015) Readmission rates in patients who underwent total hip arthroplasty. Surg Technol Int 27:215–217
Funding
Not Applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The author(s) declare that they have no competing interests.
Consent for participate
Not Applicable.
Consent for publication
Not Applicable.
Ethics approval
IRB obtained. This manuscript complies with the laws of the country in which the study was performed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mottla, J.L., Murphy, J.P., Keeling, L.E. et al. Role of arthroplasty in the Jehovah’s Witness population. Eur J Orthop Surg Traumatol 31, 1097–1104 (2021). https://doi.org/10.1007/s00590-020-02852-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02852-7