Abstract
Purpose
The primary aim of this study was to compare clinical outcomes in patients with associated both column (ABC) acetabular fractures with fracture of the posterior wall (PW), in which the PW underwent reduction and fragment-specific fixation versus those that were treated with column fixation alone. Secondary aims were to assess PW fracture incidence and morphology, as well as to compare radiographic outcomes including fracture healing and interval displacement of the PW in those that did and did not undergo fragment-specific fixation of the PW.
Methods
This was a retrospective series of ABC acetabular fractures treated at a single Level I trauma center. Separate fractures of the PW were identified, and associated features were assessed. Associated both column fractures that underwent reduction and fragment-specific fixation of the PW where then compared to ABC fractures with PW involvement that underwent column reconstruction alone. Radiographic and clinical outcomes were compared.
Results
Fractures of the PW occurred in 55.7% of ABC fractures and were associated with central displacement of the femoral head. The majority of PW fractures were large and involved the acetabular roof. All PW fractures healed without displacement by 3 months, regardless of whether or not reduction and stabilization was performed. Mid-term outcomes at 1-year were similar regardless of whether or not the PW was reduced and stabilized, with regards to Tönnis grade, Merle d'Aubigné-Postel score, and conversion to total hip arthroplasty.
Conclusion
Reduction and fragment-specific fixation of the PW component of ABC acetabular fractures did not improve outcomes in this small comparative study. Posterior wall fractures associated with ABC patterns are frequently large-sized fragments that involve the acetabular roof and are rendered stable after reconstruction of the columns.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Letournel’s series, concomitant fracture of the posterior wall (PW) occurred in 15% of associated both column (ABC) acetabular fractures [1], while a more recent series of 135 ABC fractures reported involvement of the PW in 35% of cases [2]. Posterior wall fractures that occur in the setting of an ABC fracture differ markedly from isolated PW fractures associated with posterior dislocation of the hip, and their treatment remains controversial [3,4,5,6].
While anatomic reduction of the acetabulum correlates with longevity of the hip joint [7], it is unclear whether reduction and fixation of PW injuries associated with ABC fractures affects prognosis. The primary aim of this study was to compare clinical outcomes in patients with ABC acetabular fractures with PW involvement in which the PW component was directly stabilized versus those that were treated with column fixation alone. Secondary aims were to assess PW fracture incidence and morphology, as well as to compare radiographic outcomes including fracture healing and interval displacement of the PW in those that did and did not undergo fragment-specific fixation of the PW component. We hypothesized that outcomes of ABC fractures with PW involvement would be similar regardless of PW reduction and fixation.
Patients and methods
Following institutional review board approval, patients with acetabular fractures who underwent open reduction and internal fixation from years 2003 to 2019 were identified using current procedural terminology code 27,228. All procedures were performed by three orthopedic traumatologists at an academic Level I trauma center. Pathologic fractures, nonunion and malunion cases, and patients aged less than 18 years were excluded. ABC fractures were then separated into groups with and without fracture of the PW. ABC fractures with PW components were then further separated into groups depending on whether or not the PW component underwent reduction and fragment-specific fixation.
Patient demographics (age, sex, body mass index (BMI), tobacco use), Injury Severity Score, and American Society of Anesthesiologists physical status class were extracted from the medical record. Injury mechanism was classified as “high energy” (motor vehicle accident, pedestrian-vehicle accident, fall from height, bicycle accident) or “low energy” (ground level fall). Injury radiographs and computed tomography (CT) scans were used to assess medial displacement of the femoral head, acetabular roof impaction, and complete fracture of the quadrilateral plate. Medial displacement of the femoral head was defined as none if the head remained under the roof, protrusion if the femoral head was subluxated medial to the roof (< ¼ head diameter), and dislocation if the femoral head was medially dislocated into the pelvis (> ¼ head diameter relative to the roof). Complete fracture of the quadrilateral plate was defined as separation of the quadrilateral plate from the posterior column, rendering it as a free segment. These variables were compared between ABC fractures with and without PW involvement.
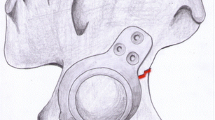
PW morphology was determined from 3D reconstructed images and was defined as quadrangular or crescent shaped (Fig. 1). The PW was assessed for roof involvement using axial CT cuts. Gap and step displacement of the PW from the anterior column at the level of the roof were assessed using sagittal CT cuts. Posterior wall size was determined according to the method described by Keith et al. [8]. Gap and step displacement of the PW from the posterior column at the level of the cotyloid fossa was assessed using axial CT cuts. Reduction accuracy of the PW was assessed on the immediate postoperative obturator oblique view (OOV) radiograph and was defined as < 1 mm, 1–2 mm, or > 2 mm of displacement at the articular surface. Interval displacement and union (as defined by disappearance of the fracture line) of the PW were determined from the 3-month postoperative OOV radiograph. Rates of interval displacement and union were compared between the groups.
Associated both column fractures with PW involvement with 1-year minimum follow-up were used to assess mid-term radiographic and clinical outcomes and were compared between those that had operative treatment of the PW versus fixation of the columns alone. The quality of articular reduction using immediate postoperative pelvic radiographs was classified using the Matta criteria [9]. Final radiographs were used to assess for femoral head osteonecrosis according to Ficat and Arlet [10], heterotopic ossification according to the modified-Brooker classification [11], and joint space narrowing using the Tönnis grade [12]. Only osteonecrosis stages II-IV were considered “positive” for osteonecrosis in the analysis. HO classes III-IV were considered severe HO [13]. Merle d'Aubigné-Postel (MAP) scores [14] from the last clinical note and rates of total hip arthroplasty (THA) conversion were recorded.
Standard descriptive statistics, including standard deviations, were calculated. Student’s t test and chi-square or Fisher’s exact test were utilized to compare continuous and categorical variables, respectively. The significance level was defined as a two-sided α < 0.05. To identify independent predictors of Tönnis grades, MAP scores, and THA conversion, any variables identified as significant on univariate analysis were tested in a multiple linear regression analysis. All statistical analyses were performed using R 4.0.2 (Boston, MA).
Surgical technique
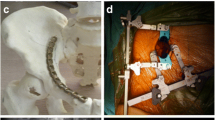
All acetabular fractures were accessed for reduction and fixation of the columns using the ilioinguinal or combined lateral window and anterior intrapelvic approaches. Fixation of the PW was then performed at the discretion of the surgeon. Of the PW fractures that underwent fragment-specific fixation, only one was addressed directly through a sequential Kocher-Langenbeck approach for reduction and buttress plate application. This was performed via a digastric trochanteric osteotomy for access given the cranial location of the PW fracture. The remaining cases were reduced using pointed reduction forceps inserted through the lateral ilioinguinal extension [15], or by percutaneous placement of a ball-spike pusher, and stabilized with a 3.5 mm cortical screw inserted from either the outer- or inner-iliac table (Fig. 2) [3]. Importantly, the PW was only stabilized if a reduction could be obtained. Hip stability was not routinely assessed after stabilization of the columns.
Heterotopic prophylaxis was not typically used. Patients were made 30 lb partial weight bearing for 8 weeks postoperatively and then advanced to full weight bearing thereafter.
Results
Incidence and associated risk factors
The incidence of PW fractures in our ABC fracture series (n = 88) was 55.7%. Age, sex, BMI, injury mechanism, complete quadrilateral plate separation, and acetabular roof impaction were similar between ABC fractures with and without PW involvement (Table 1). Associated both column fractures with PW involvement had more central displacement of the femoral head (p < 0.001, Table 1).
Posterior wall fracture morphology
The majority of PW fractures (n = 49) were quadrangular in shape (81.6%) and involved the acetabular roof (75.5%). Two consistent fracture planes were observed. The first was a coronal fracture line that bisected the acetabular roof or entered just posteriorly to it, separating the PW from the anterior column, and exited cranially. The second was a sagittal fracture line that continued caudally separating the PW from the posterior column. Mean PW size at the level of the fovea was 54.5 ± 18.5%. Mean PW gap and step displacement in the coronal plane at the level of the acetabular roof were 4.4 ± 2.9 mm and 1.0 ± 1.0 mm, respectively. Mean PW gap and step displacement in the sagittal plate at the level of the fovea were 6.4 ± 6.1 mm and 1.0 ± 1.4 mm, respectively.
Short-term radiographic outcomes
Eleven of the cases with PW components that were fixed and 29 of the cases with PW components that were not addressed had 3-month minimum follow-up and were included for this part of the analysis (Table 2). Aside from fixed PWs being more commonly male, demographics, injury characteristics, and PW morphology and displacement were similar between the groups (Table 2). Two patients with PW fixation had single-dose radiation therapy and the rest of both groups had no HO prophylaxis. Anatomic reduction (< 1 mm) of the PW was more common in the fixed group (p = 0.02, Table 2). All PW fractures went onto union by 3 months with no difference in interval displacement regardless of treatment strategy (Table 2).
Mid-term radiographic and clinical outcomes
Seven cases with PW components that were fixed (mean follow-up = 843 ± 802 days) and 14 cases with PW components treated with column fixation alone (mean follow-up = 1856 ± 1233 days) had 1-year minimum follow-up (Table 3). While the fixed PWs had an initial mean lower Matta reduction score (p = 0.02) that correlated with reduction of the PW, there was no difference in final Tönnis grade, MAP score, or THA conversion within the follow-up time period (Table 3). Femoral head osteonecrosis and severe HO were similar. Matta reduction score did not correlate with Tönnis grade, MAP score, or THA conversion in the multiple linear regression analysis.
Discussion
Associated both column acetabular fractures frequently have a fracture of the PW [1, 2]. After the surgeon reduces and stabilizes the columns back to the intact ilium, he or she must decide how to manage the PW component, if present. Options for reduction include clamp application through the lateral ilioinguinal extension and screw stabilization [3, 4], or direct reduction using an extended iliofemoral approach or sequential posterior approach for buttress plate application [4, 6]. Alternatively, the PW can be left to heal around the reconstructed columns if nondisplaced, or if the surgeon chooses to accept some level of displacement. While anatomic reduction has been shown to be critical in isolated PW acetabular fractures [9, 16,17,18], PW fractures in the setting on an ABC pattern represent a different injury, both in terms of morphology and instability, and it is unclear how management of the PW affects outcomes. This is the first study to compare outcomes in ABC acetabular fractures with PW involvement that were treated with or without reduction and fragment-specific fixation of the PW after column reconstruction. Similar results were found between the groups regardless of whether the PW was reduced and stabilized.
The current study found a higher incidence of supplemental PW fracture compared to others [1, 2], and identified central displacement of the femoral head as being an associated feature. In fact, patients with central dislocation of the femoral head were two-times more likely to have involvement of the PW. The majority of PW fractures were large [6], quadrangular in shape, involved the acetabular roof, and exited out of the supraacetabular ilium [3]. Mean PW size at the level of the fovea was > 50%, which is larger than the mean 32% reported by Shin et al. [6]. Gap displacement was greater than step-off, and the average magnitude of displacement from the anterior to posterior columns was similar.
All PW fractures healed by 3 months without interval displacement, regardless of fixation. This type of PW fracture typically fails laterally in tension as the femoral head displaces medially causing an avulsion of the PW via the intact capsulolabral complex [19], or as the femoral head impacts the hard superomedial acetabular bone creating a hinge for lateral tensile failure. This mechanism is distinct from the mechanism of other PW fractures that occur via a shearing mechanism, as the PW is “pushed” off by a posterior force directed through the proximal femur [1]. PW fractures in the setting of an ABC pattern are theoretically stable once the anterior and posterior columns have been reconstructed, and medial stability to the hip joint has been restored. Importantly, these characteristic PW fractures are not at risk for posterior instability. Shin et al. [6] dynamically assessed for posterior hip instability after column stabilization of ABC fractures with PW involvement and found none. The authors similarly found that all non-stabilized PW fractures healed without interval displacement. Posterior wall fractures associated with ABC fractures tend to be larger fragments with less displacement in comparison to PW fractures associated with posterior dislocation of the hip [3, 5].
Our results are consistent with previous studies examining clinical and radiographic outcomes following fragment-specific fixation [3, 4] or column fixation alone [6] of PW fractures in ABC patterns compared with ABC fractures without PW involvement, which reported no difference. Our results further suggest that outcomes are similar regardless of whether the PW is fixed or not. In addition, anatomic reduction of the PW may not be as critical as previously thought [3, 4, 6]. This is attributed to the fact that improved outcomes were not realized after anatomic reduction of the PW. Interestingly, there was no difference in the rate of HO in the abductor musculature between PW fractures that were fixed versus those that were not.
Based on the findings of the current study and others, the PW fracture should be assessed on the OOV [19] after anatomic reconstruction of both columns has been performed. If the PW is nondisplaced at the articular surface and superolateral ilium, it can be left alone (Fig. 3). If the PW is displaced, reduction may be attempted at the discretion of the surgeon using clamp application through the lateral ilioinguinal extension or placement of a percutaneous ball-spike pusher with subsequent screw fixation [3]. If the PW is unable to be reduced by these means, it can be ignored with confidence that the fracture will not displace further, render the hip unstable, or predispose the hip to accelerated osteoarthritis, regardless of PW size (Fig. 4). However, if displacement of the PW at the articular surface is severe, a sequential posterior approach may be considered if the risk of additional patient morbidity is acceptable (Fig. 5).
Intraoperative fluoroscopic images of the patient in Fig. 1a after reconstruction of the columns showing a residual extraarticular displacement of the posterior wall fracture and b percutaneous reduction using a ball-spike pusher. Given that there was minimal displacement at the articular surface, however, a decision was made not to stabilize the posterior wall and it was allowed to “spring back” to its original position. c Final radiograph showing healing of the posterior wall with articular congruency
a 3D reconstructed image showing a posterior wall fracture in a 63 year-old male. The superolateral posterior wall spike was unable to be “keyed” and was left alone accepting some displacement at the joint. b Immediate postoperative radiograph showing residual displacement of the posterior wall that is greater at the supracetabular ilium (arrow) compared with the radiologic roof (arrow-head). c Final radiograph after 5 years showing a congruent articular surface. The patient did have radiographic osteoarthritic changes but clinically had no pain and excellent function of the hip
a 3D reconstructed image showing a large posterior wall fracture in a 87 year-old male. The posterior wall was unable to be reduced by less invasive methods after reconstruction of the columns. A sequential posterior approach was considered but abandoned to minimize morbidity given the patients age and medical comorbidities. b Immediate postoperative radiograph showing a double arc at the radiologic roof, which represents residual displacement of the posterior wall. c Radiograph at 2 years showing a congruent appearing joint but with progression of osteoarthritic changes. This patient had worsening hip pain and was eventually converted to a total hip arthroplasty
This study has several limitations including its retrospective design, small number of patients, and limited follow-up. Long-term follow-up is always desired for articular injuries but can be difficult to obtain in the trauma patient population. It is possible that a larger cohort with greater follow-up may demonstrate improved longevity of the hip joint and lower rates of THA conversion after anatomic reduction of the PW, with or without stabilization. The majority of the PW fractures in this series were treated using indirect reductions methods with unconventional PW fixation. Furthermore, CT scans were not obtained postoperatively, which would have provided a more accurate assessment of PW reduction. Posterior wall reduction methods and fixation techniques were not compared, as only one patient in our series underwent a sequential posterior approach for direct reduction and buttress plate application. However, the lack of interval PW displacement observed in this series would suggest that screw fixation provides sufficient stability after reduction, for this type of PW fracture.
Conclusions
The PW component of ABC acetabular fractures is a large supplemental fracture that is rendered stable after reconstruction of the columns. Equivalent outcomes were observed regardless of whether the PW fracture was anatomically reduced and fixed in this small series. A larger comparative series with greater follow-up is warranted to confirm these findings.
References
Letournel E, Judet R (1993) Fractures of the acetabulum, 2nd edn. Springer, New York
Gänsslen A, Frink M, Hildebrand F, Krettek C (2012) Both column fractures of the acetabulum: epidemiology, operative management and long-term-results. Acta Chir Orthop Traumatol Cech 79(2):107–113
Wang H, Utku K, Zhuang Y, Zhang K, Fu YH, Wei X et al (2017) Post wall fixation by lag screw only in associated both column fractures with posterior wall involvement. Injury 48(7):1510–1517
Min BW, Lee KJ, Jung JW, Kim GW, Song KS, Bae KC et al (2018) Outcomes are equivalent for two-column acetabular fractures either with or without posterior-wall fractures. Arch Orthop Trauma Surg 138(9):1223–1234
Tian S, Chen Y, Yin Y, Zhang R, Hou Z, Zhang Y (2019) Morphological characteristics of posterior wall fragments associated with acetabular both-column fracture. Sci Rep 9(1):20164
Shin KH, Choi JH, Han SB (2020) Posterior wall fractures associated with both-column acetabular fractures can be skilfully ignored. Orthop Traumatol Surg Res 106(5):885–892
Tannast M, Najibi S, Matta JM (2012) Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am 94(17):1559–1567
Keith JE, Brashear HR, Guilford WB (1988) Stability of posterior fracture-dislocations of the hip. Quantitative assessment using computed tomography. J Bone Joint Surg Am. 70(5):711–714
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am 78(11):1632–1645
Ficat P, Arlet J, (1980) Necrosis of the Femoral Head. Ischemia and necrosis of bone. Williams & Wilkins, Baltimore , pp 53–74
Moed BR, Smith ST (1996) Three-view radiographic assessment of heterotopic ossification after acetabular fracture surgery. J Orthop Trauma 10(2):93–98
Tönnis D, Heinecke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 81(12):1747–1770
Bosse MJ, Poka A, Reinert CM, Ellwanger F, Slawson R, McDevitt ER (1988) Heterotopic ossification as a complication of acetabular fracture. Prophylaxis with low-dose irradiation. J Bone Joint Surg Am. 70(8):1231–1237
D’Aubigne RM, Postel M (1954) Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am 36-A(3):451–475
Gorczyca JT, Powell JN, Tile M (1995) Lateral extension of the ilioinguinal incision in the operative treatment of acetabulum fractures. Injury 26(3):207–212
Bhandari M, Matta J, Ferguson T, Matthys G (2006) Predictors of clinical and radiological outcome in patients with fractures of the acetabulum and concomitant posterior dislocation of the hip. J Bone Joint Surg Br 88(12):1618–1624
Moed BR, Carr SE, Gruson KI, Watson JT, Craig JG (2003) Computed tomographic assessment of fractures of the posterior wall of the acetabulum after operative treatment. J Bone Joint Surg Am 85(3):512–522
Moed BR, McMichael JC (2007) Outcomes of posterior wall fractures of the acetabulum. J Bone Joint Surg Am 89(6):1170–1176
Tosounidis TH, Giannoudis PV (2017) Use of inlet-obturator oblique view (leeds view) for placement of posterior wall screws in acetabular fracture surgery. J Orthop Trauma 31(4):e133–e136
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.J.G. receives personal fees from Pacira Pharmaceuticals, Biocomposites, BoneSupport AB, Conventus, Globus Medical, StabilizOrtho, Synthes, and from KCI outside of the submitted work. J.A.B. receives personal fees from Globus Medical and Innomed outside of the submitted work. None of the remaining authors has anything to disclose.
Ethical approval
This article contained only de-identified human participant information and was approved by an institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, M.J., Hollyer, I., Wadhwa, H. et al. Management of the posterior wall fracture in associated both column fractures of the acetabulum. Eur J Orthop Surg Traumatol 31, 1047–1054 (2021). https://doi.org/10.1007/s00590-020-02850-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02850-9