Abstract
Introduction
Revision knee arthroplasty surgery can range from patella resurfacing or polyethylene exchange, to staged revision and revision to a more constrained implant. Subsequently, the ability to elicit outcomes becomes difficult to obtain and hence information on functional outcome and survivorship for all modes of failure with a single revision system is valuable.
Methods
We retrospectively assessed 100 consecutive revision knee replacements that were converted from a primary knee replacement to a Triathlon total stabilizer (TS) knee system (Stryker Orthopaedics, Mahwah, NJ). Inclusion criteria included failure of a primary knee replacement of any cause converted to a Stryker TS knee system. Midterm outcome of at least 5 years was required. Implants survivorship, Oxford Knee Score (OKS), Forgotten Joint Score (FJS-12), Short Form (SF-) 12, reported patient satisfaction and radiographic analysis were recorded.
Results
The all-cause survival rate at 5 years was 89.0% [95% confidence interval (CI) 87.3 to 90.7]. The all-cause survival rate was generally static after the first 4 years. The mean OKS was 27 (SD 11.9, range 0 to 46), FJS was 32.3 (SD 30.4, range 0 to 100), SF-12 physical component summary was 40.6 (SD 17.6, range 23.9 to 67.1), and mental component summary was 48.3 (SD 15.5, range 23.9 to 69.1). Reported patient satisfaction in patients who were not re-revised was 82%.
Conclusion
The midterm survivorship of cemented Stryker Triathlon TS knee revision for all-cause mode of failure is good to excellent; however, future follow-up is required to ensure this survivorship is observed into the long term. Despite limited functional outcome, overall patient satisfaction rates are high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the increase in primary total knee arthroplasty (TKA) procedures, there is a corresponding predicted increase in the need for revision knee arthroplasty (RKA) in the future [1,2,3,4]. Together with functional outcome and complication profile, the success of a primary TKA will be determined by the survivorship of the prosthesis. Failure of a primary TKA will likely necessitate the need for revision surgery. The burden of knee revision surgery in the USA has been estimated to reach 268,000 cases annually by 2030 [1], while in England and Wales the number of RKA surgeries may have increased by 332% by that same time [2]. Resource allocation for these highly complex procedures, as well as the employment and training of orthopaedic surgeons to undertake these surgeries, is now subject to projection analysis and health care planning [3]. With an increase in the number of RKA surgeries, research into the outcome and survivorship of these revisions must be undertaken and the cause of failure leading to multiple revised knee joint arthroplasties should be investigated.
Revision knee arthroplasty surgery can range from patella resurfacing or polyethylene exchange, to staged revision and revision to a more constrained implant or endoprosthesis [5]. Subsequently, the ability to elicit outcomes becomes difficult to obtain due to, in part, the nature of the variable modes of failure and the revision surgery that has been undertaken. To this extent, information on functional outcome and survivorship for differing modes of a failure with a single revision system is valuable. Implants that can aid in knee stability may be advantageous to the functional outcome and survivorship of RKA [6]. Despite the mode of failure, the goals of revision surgery remain the same, a well-aligned, well-balanced stable implant that is free of sepsis and provides relatively pain-free functional range of movement [7].
We have studied the outcomes of a specific total stabilizer knee system for revision of all modes of primary failure. There are currently limited studies that explore the short- to midterm outcomes of this system for RKA [8, 9]. The primary aim of this study was to determine midterm all-cause survivorship of the Stryker Triathlon total stabilizer knee revision system. The secondary aims were to assess midterm functional outcome, patient satisfaction and radiographic outcome.
Methods
Retrospective cohort study assessed the first 100 consecutive revision knee replacements performed at the study centre using the Triathlon total stabilizer (TS) knee system (Stryker Orthopaedics, Mahwah, NJ). The surgeries were performed in a single institution by orthopaedic surgeons who specialize in arthroplasty. Inclusion criteria included failure of a primary TKA of any cause (Fig. 1) converted to a Stryker Triathlon TS knee system (Fig. 2). The revision implant consisted of at least a TS base plate and stem, TS polyethylene with reinforcement post and TS femoral component with stem. In all cases, the stems on both the tibial and femoral side were cemented into bone. The patella was not routinely revised if it had previously been resurfaced. Primary resurfacing in the setting of revision surgery was at the discretion of the surgeon. The patella was revised in cases of revision for infection. Prosthetic joint infection was recorded as the mode of failure where positive culture samples had been obtained either before surgery or at the time of surgery. Culture negative infected prosthetic joint replacements were recorded by the treating surgeon in cases where there was sufficient supporting clinical evidence. A minimum of 5 years of follow-up was required. Data were collected from 2008 to 2011 and included patient demographics, index implant, primary mode of failure of the index prosthesis, patient survivorship and intra-/post-operative complications.
AP and lateral radiographs of the knee from Fig. 1 following revision to a cemented Stryker Triathlon TS knee system
Functional assessment
Follow-up questionnaires assessed outcome using the Oxford Knee Score (OKS) [10], Forgotten Joint Score (FGJ-12) [11, 12], Short Form (SF-) 12 [13] and patient satisfaction. The OKS consists of 12 questions that assess the patient’s pain and function. Each item is answered on a five-point response scale ranging from 0 to 4 and generates a summed total score ranging from 0 to 48, where 0 indicates the worst possible outcome and 48 indicates the best possible function. The FJS-12 assesses joint awareness during the activities of daily living (for example, climbing stairs, walking for more than 15 min, in bed at night, etc.). It consists of 12 questions assessed using a five-point Likert response format. Item scores are summed and linearly transformed to a 0 to 100 scale, a high value reflecting the ability of the patient to forget about the affected/replaced joint during the activities of daily living. The SF-12 Health Survey is a 12-item quality of life questionnaire often used in large population health surveys. The transformed scores for each health domain reflect a patient’s poor (0) to excellent (100) health status. Two separate outputs are generated: a generic physical component summary (PCS) score and mental component summary (MCS) score. Normative-based scoring is used for each component: the population mean score is 50. Patients were asked whether overall they were satisfied or dissatisfied with their RKA. The results were recorded either satisfied or dissatisfied.
Radiographic assessment
The patients’ radiographic series were reviewed on digital radiographs (Kodak© Picture Archiving and Communication System on a liquid crystal display) for evidence of radiolucent lines (< 2 mm) with or without progression, lysis (> 2 mm) and loosening (subsidence) for patients that had not undergone re-revision. The areas of radiolucency were documented by site and radiographic evidence of progression recorded. A modification of the Ewald [14] classification was used to enable assessment of the tibial and femoral stems, as their original classification does not take these into account. Both antero-posterior (AP) and lateral views of the knee were assessed. Five zones for the tibia and five zones for the femur in both the AP and lateral radiographs were allocated to give reference to the area of radiolucency and lysis (Fig. 4).
Prosthesis and technique
The Stryker Triathlon TS knee system is a single-radius prosthesis centred on the epicondylar axis and is designed to provide ligament isometry in the entire range of movement. The high degree of prosthesis conformity and ± 2 degrees of varus/valgus constraint provided by the larger post are designed to allow increased stability of the joint and for the post-cam engagement to occur at 40–45 degrees of flexion, replicating what studies have shown to occur in natural knees [15].
The technique for revision knee surgery using the TS system has been standardized through intercollegiate teaching by the staff specialists at the Royal Infirmary of Edinburgh through the college of surgeons of Edinburgh in consultation with the University of Edinburgh. The principles of bone preservation, joint line restoration, increased posterior condylar offset and meticulous soft tissue dissection are taught and practised by the surgeons in the arthroplasty unit [16].
Statistical analysis
Statistical Package for Social Sciences version 17.0 (SPSS Inc., Chicago, IL, USA) was used to analyse the data. An unpaired Student’s t test and analysis of variance (ANOVA) were used to compare linear variables between groups. Pearson’s correlation was used to assess the relationship between linear variables. Dichotomous variables were assessed using a chi-square test. Kaplan–Meier methodology and a life table were used to investigate implant survival. Cox regression analysis was used to identify independent predictors of implant survival. A p value of ≤ 0.05 determined statistical significance.
Ethical approval was obtained for this study from the regional ethics committee.
Results
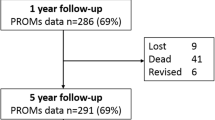
No patient was lost to follow-up from survival assessment; however, 27 patients died during the study period. The mean age of the cohort at the time of surgery was 69.9 years [standard deviation (SD) 10.2, range 42 to 92 years]. There were 42 male patients and 58 female patients with a mean age of 70.9 (SD 11.2) years and 69.1 (SD 9.5) years, respectively (p = 0.39 t test). The median follow-up for all patients, including those who were deceased or had been revised (taken as time of revision), was 7.2 years with an interquartile range of 5.0 to 7.8 years. Fifteen patients underwent revision to a TS for septic reasons and 85 for aseptic reasons.
Implant survival
There were 12 re-revisions during the study period. There were six post-operative infections, all of which were in patients that had revision for aseptic indications. Three patients were re-revised to a hinge for instability, of which all had their original TS revision for infection. Two retained the prosthesis and underwent patella resurfacing for patella femoral pain. One incurred a peri-prosthetic fracture that subsequently became infected and underwent re-revision. The all-cause survival rate at 5 years was 89.0% [95% confidence interval (CI) 87.3 to 90.7] (Table 1). The all-cause survival rate was generally static after the first 4 years (Fig. 3). The survival rate for aseptic causes (n = 85) at 5 years remained at 89.0% (95% CI 85.8 to 92.2); however, this decreased for septic causes (n = 15) to 87% (95% CI 83.3 to 90.7), but this was not significantly different (log rank p = 0.43). Interestingly, if the two patients who had a subsequent patella resurfacing were not classed as re-revisions (with retention of implant) the survival aseptic survival rate is 92.0% (95% CI 88.5 to 95.5). Gender (p = 0.85), surgeon (p = 0.51), date of index procedure (p = 0.54) or indication for revision (p = 0.36) were not significant predictors of revision (Cox regression analysis). Age was, however, demonstrated to be an independent predictor of survival (hazard ratio 0.93, 95% CI 0.88 to 0.99, p = 0.01), so for each increasing year of age the risk of revision decreased by 7%.
There were 88 patients that had not been revised during the study period, 27 of these had died and an additional 16 patients were not willing or unable to participate in the completion of their functional outcome. Of the remaining 45 patients, there were 19 males and 26 females with a mean age of 67.8 years, who completed both the functional measures and satisfaction assessments at a mean follow-up of 7.4 (range 5.2 to 10.6) years. The mean OKS was 27 (SD 11.9, range 0 to 46), FJS was 32.3 (SD 30.4, range 0 to 100), SF-12 PCS was 40.6 (SD 17.6, range 23.9 to 67.1), and MCS was 48.3 (SD 15.5, range 23.9 to 69.1). According to the Clement et al. [17] grading of the post-operative OKS, there were 16 (35.6%) excellent, 11 (24.4%) good and 18 (40.0%) fair-to-poor outcomes. Despite the fact that more than a third had a fair or poor outcome according to their OKS which is supported by the low FJS, 37 (82.2%) patients reported overall satisfaction with their RKA, while eight (17.7%) patients reported dissatisfaction.
Radiographic assessment
The most recent radiographs for the 88 TS knee systems that had not been re-revised were assessed for radiolucent lines, progressive lysis or loosening. An absence of lysis or radiographic signs of loosening were observed in 78 of the 88 studied cases. Nine post-operative radiographs demonstrated non-progressive radiographic lucent lines with no evidence of loosening. Four of these presented with non-progressive zone 1 AP tibia radiolucent lines, and three demonstrated lateral femur zone 1 non-progressive radiolucent lines. One presented with AP tibia zone 5, and one with lateral tibia zone 1 non-progressive radiolucent lines. One radiograph demonstrated progression of radiographic lucent lines and lysis in an 88-year-old man. These were seen in the AP and lateral tibia zone 1 and AP femur zone 1 and 2. Due to the asymptomatic nature and his comorbidities, he is not currently scheduled for revision of his TS knee prosthesis and will continue to be reviewed annually.
Discussion
This study has demonstrated an acceptable early- to midterm survivorship and functional outcome, with a high rate of patient satisfaction for the Stryker Triathlon TS knee system for all-cause RKA.
Revision knee arthroplasty continues to increase with published data from the UK National Joint Registry (NJR) recording 60,680 knee joint revision operations and 4518 re-revision operations as of 2017 [18]. Debate regarding the level of constraint required in revision knee surgery continues. Meijer et al. demonstrated that the use of primary TKA implants was not acceptable with survivorship at 5 years being only 44% [19]. Scuderi recommended that the least constrained prosthesis for stability was used [20], while Cottino et al. report improved outcomes with the use of contemporary rotating hinge prosthesis [21]. The authors advocate for the partially constrained varus/valgus post of the TS system where collateral ligaments are intact and adequate bone stock is present. The NJR data record infection, aseptic loosening and instability as the main indications for re-revision [18]. For such cases, it is typical for our centre to implant cemented stem TS knee systems with or without augmentation or cone, adhering to the principles of joint line restoration and optimizing posterior condylar offset [16, 22].
The all-cause survival rate at 5 years with conversion to a Stryker TS knee system was 89.0%. Gwam et al. reported a survivorship of 94% for revision of aseptic knee replacement to TS knee system with a mean follow-up of 4 years [8]. Hamilton et al. reported no re-revision operations in 53 patients undergoing revision of aseptic knee replacements to TS knee systems at 2-year follow-up at the same study centre [9]. The inclusion criteria for their study cohort were strict, and their main outcome was function at 2 years not survivorship. Our results found no re-revisions within the first year and a static re-revision rate after 4 years. It is interesting that the three patients required re-revision to a hinged prosthesis that underwent a TS for septic causes and may indicate a higher level of restraint that may be needed for such patients after surgical debridement of the soft tissues.
Patient satisfaction was relatively high at 82% despite a lower-than-expected functional outcome as assessed by the OKS, where 40% of patients had fair-to-poor outcomes. The SF-12 Physical Health Composite Scale (PCS) in this cohort was also lower than average (50) with a mean score of 40.6, while the Mental health Composite Score was near normal at a mean of 48.3. A greater improvement in the OKS and SF-12 score has been demonstrated to correlate with an increased rate of patient satisfaction with the outcome of their primary total knee arthroplasty [17, 23]. The lower-than-expected OKS, which is a joint-specific score, may relate to the patients overall poor generic health which is illustrated by their poor SF-12 PCS score. After primary total knee replacement, patients with a poor overall physical health have an associated worse OKS but have an equivalent satisfaction rate, which is consistent in the presented revision cohort [23,24,25].
Radiographic analysis found one case from the 88 non re-revised knees which showed signs of progression of radiolucent lines, and an additional nine (10%) knees were found to have static radiolucent lines. This is not an unexpected finding as previous studies have shown a higher prevalence of radiolucent lines after revision surgery when compared to primary knee arthroplasty [26, 27]. Radiographs are an important diagnostic tool, especially in predicting the need for asymptomatic progression of lysis and impending implant construct failure. The single case with progression of lucent lines identified in this series was asymptomatic, of advanced age and with significant comorbidities, and he remains under follow-up.
To the authors’ knowledge, this is the first study to report all-cause revision outcomes, both in survivorship and in outcome with a minimum 5-year review for the Stryker TS knee system. This is a single-centre, multi-surgeon analysis. The arthroplasty department has adopted revision technique principles and techniques that help to standardize the approach and revision procedure [16]. A weakness of our study is that a proportion of patients (n = 43) were lost to clinical follow-up. This was mainly due to death (n = 27) from unrelated causes or due to refusal/inability to complete the questionnaire (n = 16). The inability to attend or refusal was chiefly due to advanced age, the presence of comorbidities.
Conclusion
The midterm survivorship of cemented Stryker Triathlon TS knee revision for all-cause mode of failure is good to excellent; however, future follow-up is required to ensure that this survivorship is observed into the long term. Current radiographic assessment is reassuring for longevity of fixation. Despite limited functional outcome, overall patient satisfaction rates are high.
References
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. JBJS Am 89:780–785
Patel A, Pavlou G, Mujica-Mota RE, Toms AD (2015) The epidemiology of revision total knee and hip arthroplasty in England and Wales. JBJS 97-B:1076–1081
Guerrero-Luduena RE, Comas M, Espallargues M et al (2016) Predicting the burden of revision knee arthroplasty: simulation of a 20-year horizon. Value Health 19(5):680–687
Hamilton DF, Howie CR, Burnett R, Simpson AHRW, Patton JT (2015) Dealing with the predicted increase in demand for revision total knee arthroplasty challenges, risks and opportunities. Bone Joint J 97-B:723–728
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, knee & shoulder arthroplasty: 2017 Annual Report. Adelaide: AOA, 2017: 198
Kim YH, Kim JS (2009) Revision total knee arthroplasty with use if a constrained condylar knee prosthesis. JBJS Am 91-A(6):1440–1447
Thienpont E (2016) Revision knee surgery techniques. EFORT Open Rev 1:233–238
Gwam CU, Chughtai M, Khlopas A et al (2017) Short-to-midterm outcomes of revision total knee arthroplasty patients with a total stabilizer knee system. J Arthroplasty 32:2480–2483
Hamilton DF, Simpson PM, Patton JT, Howie CR, Burnett R (2017) Aseptic revision knee arthroplasty with total stabilizer prosthesis achieves similar functional outcomes to primary total knee arthroplasty at 2 years: a longitudinal cohort study. J Arthroplasty 32:1234–1240
Dawson J, Fitzpatrick R, Murray D, Carr A (1998) Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg (Br) 80:63–69
Behrend H, Giesinger K, Giesinger JM, Kuster MS (2012) The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty 27:430–436
Hamilton DF, Loth FL, Giesinger JM, Giesinger K, MacDonald DJ et al (2017) Validation of the English language Forgotten Joint Score-12 as an outcome measure for total hip and knee arthroplasty in a British population. Bone Joint J 99-B(2):218–224
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Ewald FC (1989) The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res 248:9–12
Fu FH, Harner CD, Johnson DL, Miller MD, Woo SL (1993) Biomechanics of knee ligaments: basic concepts and clinical application. JBJS 75:1716–1727
Sampson AJ, Hamilton DF, Loh B, MacPherson G, Burnett R (2018) Optimizing posterior condylar offset and joint line restoration in revision total knee arthroplasty using a contemporary implant system. Tech Orthop 1:1. https://doi.org/10.1097/bto.0000000000000314(published ahead of print)
Clement ND, Macdonald D, Burnett R (2013) Predicting patient satisfaction using the Oxford knee score: where do we draw the line? Arch Orthop Trauma Surg 133(5):689–694
National Joint Registry (2017) National Joint Registry for England, Wales and Northern Ireland; 11th annual report
Meijer MF, Reininga IHF, Boerboom AL, Stevens M, Bulstra SK (2013) Poorer survival after primary implant during revision total knee arthroplasty. Int Orthop 37(3):415–419
Scuderi GR (2001) Revision total knee arthroplasty: how much constraint is enough? Clin Orthop Relat Res 392:300–305
Cottino U, Abdel MP, Perry KI, Mara KC, Lewallen DG, Hanssen AD (2017) Long-term results after total knee arthroplasty with contemporary rotating-hinge prosthesis. J Bone Joint Surg Am 99(4):324–330
Clement ND, MacDonald DJ, Hamilton DF, Burnett R (2017) Posterior condylar offset is an independent predictor of functional outcome after revision total knee arthroplasty. Bone Joint Res 6(3):172–178
Clement ND, Burnett R (2013) Patient satisfaction after total knee arthroplasty is affected by their general physical well-being. Knee Surg Sports Traumatol Arthrosc 21(11):2638–2646
Clement ND, MacDonald D, Simpson AHRW (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(8):1933–1939
Clement N, MacDonald D, Patton JT, Burnett R (2015) Post-operative Oxford knee score can be used to indicate whether patient expectations have been achieved after primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23(6):1578–1590
Jacobs MA, Hungerford DS, Krackow KA, Lennox DW (1998) Revision total knee arthroplasty for aseptic failure. Clin Orthop Relat Res 226:78–85
Insall JN, Dethmers DA (1982) Revision of total knee arthroplasty. Clin Orthop Rel Res. 170:123–130
Author information
Authors and Affiliations
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stevens, J.M., Clement, N.D., MacDonald, D. et al. Survival and functional outcome of revision total knee arthroplasty with a total stabilizer knee system: minimum 5 years of follow-up. Eur J Orthop Surg Traumatol 29, 1511–1517 (2019). https://doi.org/10.1007/s00590-019-02449-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02449-9