Abstract
Purpose
The purpose of this study was to evaluate the clinical and functional outcomes of failed plate fixation in distal tibia fractures salvaged with hexapod circular fixators.
Materials and methods
The database of a specialized limb reconstruction center was searched for all patients with failed plate fixation undergoing limb reconstruction with a circular external fixator between 2008 and 2017. Patients between the ages of 18–65 years, with a symptomatic distal tibia malunion or non-union following plate and screw fixation were included. The SF-12 and Foot Function Index (FFI) scoring systems were used to measure clinical and functional outcomes.
Results
Ten patients with a mean age of 38 ± 13 years met the inclusion criteria. Seven patients had an infected non-union, two hypertrophic non-unions, and one a malunion. The mean follow-up was 41.7 ± 28.3 months. The mean duration of external fixation was 232.9 ± 146.6 days. The SF-12 demonstrated a mean score of 49.4 ± 7.7 for the physical component and a mean score of 55.3 ± 8.1 for the mental component. Five patients (50%) scored above 45 points for the SF12 physical component, and nine patients (90%) scored above 45 points for the mental component, indicating good outcome can be achieved. The mean FFI score was 24.9 ± 19.9, and six patients had a score below 14 points (good outcome). Radiological union was observed in all 10 patients at a mean of 29 ± 14 months.
Conclusions
The results of this study suggest that hexapod circular external fixation is an attractive surgical alternative for the treatment of failed plate fixation of distal tibial fractures, and can reliably achieve bony union and result in very satisfactory clinical outcomes.
Level of Evidence
Level IV case series.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal tibia fractures are often high-energy complex injuries, prone to complications, and can later present chronic problems that may be difficult to resolve [1]. Surgical treatment is generally indicated, and techniques considered include plate osteosynthesis, external fixation, intramedullary nailing, and minimally invasive techniques [2, 3]. Potential complications following operative treatment include wound breakdown, deep infection, malunion, and non-union [4], reportedly involving up to fifty percent [5]. In a large retrospective analysis of tibia fracture, the reported non-union rate was 12% [6], and Vallier et al. identified a malunion rate of 8.3% with medial plating of distal tibial fractures [7]. One of the challenges in treating these injuries is that the distal fragment is often short with flaring of the metaphyseal bone, and plates or nails may not provide adequate stability to achieve rapid union [8].
Periarticular distal tibial non-union can be even more difficult to treat [9]. Small distal bone fragments, disuse osteopenia, soft tissue atrophy, infection, and adjacent joint contractures create genuine challenges. Various treatment options exist including primary arthrodesis or joint preservation [9]. Fixation techniques include blade-plates, conventional plates, external fixation, or circular external fixation with or without bone transport, shortening, distraction osteogenesis, or a combination of these techniques.
The use of external fixators in distal tibia fractures is well established [10,11,12]. Hybrid and Ilizarov fixation allows early weight bearing and ankle motion, and good outcomes have been described [8, 13]. For the treatment of distal tibial non-unions or infections following fracture fixation, limb salvage is possible, but commonly involves ankle fusion, microvascular free tissue transfers, and bone grafting [14, 15]. The diagnosis of deep infection is generally associated with considerable morbidity and often requires multiple procedures and a protracted course of treatment [16, 17]. Although successful limb salvage can be achieved in approximately 80% of cases, amputation is not uncommon [16,17,18]. Given these uncertain outcomes, it was therefore the purpose of this study to evaluate functional outcomes following failed plate fixation in distal tibia fractures salvaged with hexapod circular fixators. We hypothesized that salvage with circular hexapod fixation would result in joint preservation, bony union, and limb salvage with acceptable functional outcomes.
Methods
Patient Identification and Data Collection
This study was conducted with a retrospective cross-sectional design. Prior approval to conduct this investigation was obtained from the local Institutional Review Board and Human Research Ethics Committee. Patients who were treated for failed plate fixation of distal tibial fractures between 2008 and 2017 were identified from the database of a specialized limb reconstruction and trauma center. Patients were included if aged between 18 and 65 years, and had a failure of plate fixation of the distal one-third of the tibia with an existing non-union or malunion, whether infected or not. Malunion was defined as a coronal deformity of greater than 5º varus or 10º valgus, or a sagittal deformity of greater than 15º [19]. Non-union was defined as the lack of any clinical or radiological evidence of union at 6 months [20]. The Cierny–Mader classification system for chronic osteomyelitis was utilized to stage cases with infection [21]. Patients were excluded if the initial fracture was more than 5 cm proximal to the ankle joint, was a segmental or intra-articular fracture, or had a history of previous ipsilateral tibial fractures, polytrauma, or closed head injuries. The medical records and radiographs were screened by an independent research associate. To preserve patient confidentiality, each case was allocated a unique study identification number.
Surgical treatment protocol
All patients had their implants removed and treatment followed a standardized protocol, described previously [22]. Briefly, this treatment protocol includes eight defined steps:
(1) debridement, PMMA spacer with the Masquelet technique [23], and provisional stabilization with external fixation, (2) soft tissue coverage and wound closure, (3) definite fracture fixation with a hexapod capable circular frame, (4) later removal of the PMMA spacer and corticotomy, (5) latency period and gradual distraction, (6) docking site modification, (7) functional rehabilitation, (8) frame removal, long-term surveillance. These steps served as a guide and were applied according to the clinical requirements, individualized to the specific characteristics of each patient. This protocol adheres to the established principles of staged management for complex limb salvage and reconstruction, particularly when treating infected non-unions and chronic osteomyelitis [24, 25].
Outcome measures
Functional outcomes were evaluated with the SF-12v2 [26, 27] and Foot Function Index [28]. The SF-12v2 is a validated score consisting of twelve questions in eight health domains; physical function, bodily pain, general health perception, vitality, physical role functioning, emotional role functioning, mental health, and social role functioning. It uses an algorithm to generate the physical and mental health composite scores. An individual mean score of less than 45 for physical and mental scores indicates impairment of function [26]. The FFI was used to assess foot and ankle function, and has been used previously [7, 29]. The FFI consists of twenty-three items covering pain, disability, and activity restriction; the values for each aspect range from zero to one. The total foot function score is then calculated as the mean of the three subscale scores, expressed in percentages by multiplying the final score by 100. A higher FFI score indicates greater impairment and is indicative of a poorer outcome. To reduce interviewer bias, participants were asked to complete both questionnaires without assistance from the research associate.
Radiographic union was assessed using the criteria from Whelan et al. [30] and defined as the presence of bridging callus of at least three cortices at the fracture site with a RUST score of ≥ 9. This scoring system has been shown to be reliable and valid with an ICC above 0.8 for both intra- and inter-observer correlations [30]. The duration each patient spent in a frame and any complications that developed were extracted from the medical records.
Statistical analysis
Descriptive statistics (means and standard deviation) were used for the demographic variables, as well as FFI and SF-12 scores. All analyses were conducted using STATA SE (Version 12.0; Stata Corp, College Station, Texas, USA) for Windows.
Results
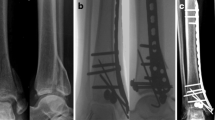
Twelve patients met the inclusion criteria, nine males and three females, although two patients could not be contacted and were excluded. Pertinent demographic details and outcome scores are summarized in Table 1. The mean age of participants was 38 ± 13 years, with a mean follow-up was 41.7 ± 28.3 months. The mechanism of injury was a fall in seven, motorbike accident in two, and motor vehicle accident in one patient. In seven cases, the etiology of fixation failure was infection (Cierny–Mader IVA), and in two cases, inadequate surgical fixation with fracture instability. One patient presented with a malunion and talar subluxation. His original injury was recorded as a Gustilo–Anderson IIIA open distal tibial fracture following a motor vehicle accident, and initial treatment occurred at another center with a medial distal tibial plate (Figs. 1, 2, 3).
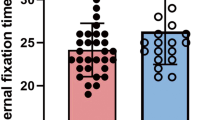
The course of treatment was often difficult and protracted, and the mean duration of external fixation was 232.9 ± 146.6 days. Although the sample size was small and the distribution into groups unequal; there was a very large discrepancy in the time course of treatment between cases that were infected compared to aseptic cases. For the patients with septic non-unions (n = 7), the mean duration of external fixation was 274.1 ± 154.8 days. For the aseptic cases (n = 3), the mean duration of external fixation was 136.7 ± 71.1 days.
The SF-12 mean score was 49.4 ± 7.7 for the physical component, and 55.3 ± 8.1 for mental component. Overall five patients had good outcomes with a physical component score (PCS) above 45 (Table 1). Eight patients had good mental health outcomes, indicated by a MSC score above 50 (Table 1). The Foot Function Index had a mean value of 24.9 ± 18.9 points. In six patients, the FFI score was less than 14, indicating good outcomes. One of the patients had a score above 62, indicating an unsatisfactory outcome; this was the individual with a tibial malunion following a high-energy motor vehicle accident. When compared to the contralateral extremity, seven patients displayed normal ankle movement, one patient had restricted plantar- and dorsiflexion, and two patients had a stiff ankle in the neutral position allowing mobilization. However, one of the patients with a stiff ankle relied on a CAM boot for ambulation. Eight patients returned to work, one went into early retirement, and one patient was unable to work because of depression despite minimal pain.
Radiographic union was achieved in all 10 patients; the time from the salvage procedure to union was a mean of 29 ± 14 weeks. Seven patients did not demonstrate any radiographic evidence of osteoarthritis, and three patients showed Takakura stage I degenerative changes. The mean duration in a frame was 233 ± 147 days. The overall complication rate was 40%. The distal wire broke in one patient and had to be replaced 4 weeks after the index procedure; similarly, one half pin broke 4 weeks after the index procedure. One wire was removed on the proximal ring in another case because of soft tissue irritation, and one patient was treated for recurring deep infection which settled with aggressive debridement, irrigation, and reapplication of the external fixator.
Discussion
The most important finding of this study was that distal tibia fractures that had previously failed to unite with plate fixation could be successfully treated with hexapod external fixation. Bone union was achieved in all cases, and the functional outcome was rated good in over 60% of patients.
Distal tibial non-unions are difficult to treat, and the small distal fragment presents a major challenge for the surgeon [9]. Several authors have reported on the outcomes of treating distal tibial non-unions [9, 14, 15, 31, 32]. Earlier studies have used ankle arthrodesis as a salvage procedure [14, 15], while more recent studies have attempted to preserve the integrity of the ankle joint [9, 31, 32]. Marsh et al. [15] treated seven patients with distraction osteogenesis and ankle arthrodesis and achieved union in six cases at an average of 7.9 months; one patient required a below knee amputation. Of their six patients treated successfully, three had good, two fair, and one poor outcome, with lower SF 36 scores than the standard age-matched population [15]. Zalavras et al. [14] reported on their experience treating infected distal tibial metaphyseal fractures. They used a similar staged protocol to that employed in the current study, with debridement, antibiotic cement spacers, external fixation, soft tissue coverage, and ankle fusion. Union was achieved in all of their cases, and all patients were able to walk without assistive devices and were pain free at a mean follow-up of 5.5 years [14]. These results are similar to our findings, although seven of the ten patients in our cohort were infected non-unions. Union was achieved in all seven cases, and the outcome scores indicated a high functional recovery in six of the seven patients with excellent mental health scores in four patients. Our results demonstrate that limb salvage without ankle fusion is an attractive option, achieving, very similar, if not better, outcomes.
Richmond et al. [31] suggested treating non-unions of the distal tibia with reamed intramedullary nailing. Seven of their 32 patients had a history of infection, but none had any signs of active infection at the time of surgery. They reported a union rate of 91% at a mean of 3.5 months, but 43% of the previously infected cases developed deep infection requiring further surgical interventions [31]. The functional outcomes were not reported. Obviously, this technique is only suitable if there is sufficient distal bone stock available.
More recently, Laklouk et al. [32] reported on their experience with 13 cases of failed internal fixation, of which three had an infected non-union. Following treatment with Ilizarov external fixation, union was achieved in all cases. They used the ASAMI score, and eleven patients had good and fair outcomes at a mean of 24-month follow-up [32]. Eralp et al. [9] also treated 13 cases of infected non-union of the juxta-articular region of distal tibia. The Ilizarov fixator was used in 12 cases, and the Taylor Spatial Frame was used in one [9]. Union was achieved in all cases, and 12 patients had good or excellent results when the functional outcomes and bone healing were assessed using Paley’s criteria. However, five patients (38%) required an ankle arthrodesis. Eralp et al. [9] have utilized the Ilizarov fixator which allows compression, distraction, lengthening, bone transport, and deformity correction, all by manipulating the frame configuration, similar to a hexapod system. In contrast to Eralp [9], none of our patients required ankle arthrodesis after a very similar period of follow-up.
Arvesen et al. [33] assessed the efficacy of hexapod external fixation for the treatment of distal tibial non-unions with associated complex deformities. They reported a 94% union rate and reduced a mean 18 degree pre-operative deformity to less than 5 degrees after. Functional outcomes were not reported. Hexapod external fixation and its ability to perform 6-axis manipulation of the limb allows highly accurate correction of complex, multifocal deformities. To achieve reliable and reproducible results with a high rate of union, it is important to follow a formal standardized and structured approach. It may be argued that these difficult cases should be treated in a specialized center to achieve better outcomes. This argument is certainly supported by the published trauma surgery literature [34, 35]. Demetriades et al. demonstrated better outcome for level I trauma centers for specific injuries, and Cudnik et al. [34, 35] showed that level I trauma centers had improved survival and better functional outcomes when compared to level II hospitals.
Limb salvage using a hexapod external fixation system without ankle fusion remains a very attractive surgical option for distal tibial non-unions. Early soft tissue management, restoration of limb length, deformity correction, and the ability to weight-bear promote functional recovery [22]. However, typical treatment times are long and complications are frequent [15], and patients should be informed about the expected time in frame and the associated high complication rate.
The mean duration of external fixation was 233 days, considerably longer than in previous publications. This clinical series has revealed a very large discrepancy in the time course of treatment between cases that were infected compared to aseptic cases. In this study, infected cases spent twice as long in an external fixator. For patients with septic non-unions, the mean duration of external fixation was 274 days, and for the aseptic cases, the mean duration of external fixation was only 137 days. However, the sample size was small and the distribution into groups unequal, and no meaningful statistical comparison can be performed.
Laklouk et al. [32] used the Ilizarov fixator to treat failed internal fixation in distal tibial fractures and reported a mean duration of external fixation of 146 days. However, they only treated 3 cases (23%) of deep infection, while in the current study 70% of the cases were infected. With any infected case, time to union is generally longer and union more difficult to achieve, and the results of this study support this contention. Eralp et al. treated 13 patients with infected non-unions and reported a mean time in external fixation of 198 days, further corroborating this argument [9]. In contrast, Zalavras treated six patients with infected distal tibial metaphyseal and plafond fractures and reported a mean duration of external fixation of only 174 days [14]. There are many potential confounding factors, and the duration of external fixation can depend on multiple other aspects such as the patient’s immune status, presence of comorbidities, and the type and chronicity of the infection. It is also possible that an arthrodesis allows more aggressive debridement, radically removing bone and allowing bone transport of healthy well-perfused bone, potentially reducing the time in external fixation.
Limb salvage is often associated with a high rate of complications [18, 22]. The overall complication rate in this series was 40%, similar to the rate of complications reported previously [9, 14, 15, 31, 32]. One broken wire and one broken half pin were successfully treated by removal and replacement. In one patient, a recurrence of infection 1 month after the index procedure required frame removal, repeat debridement, and application of an suction/irrigation system. Following resolution of the infection, a new hexapod fixator was applied and the fracture united with a duration of external fixation of 150 days.
This study has several important limitations. The sample size was small, typical of all published studies reporting on limb salvage with complex trauma. The retrospective study design introduces the possibility of selection bias. The study was performed at a single center specialized in limb reconstruction limiting its external validity, and the results reported here may be difficult to replicate in less experienced trauma units. However, treatment of distal tibial non-unions and osteomyelitis is a highly complex clinical condition and requires experience and specialized knowledge to achieve satisfactory outcomes. It is acknowledged that over 70% of these cases had chronic osteomyelitis, and the inclusion of more non-infected cases may have resulted in higher functional outcomes and a reduced duration of external fixation.
Conclusion
The results of this study suggest that hexapod circular external fixation is an attractive surgical alternative for the treatment of failed plate fixation of distal tibial fractures and can reliably achieve bony union and result in very satisfactory clinical outcomes.
References
Sirkin M, Sanders R (2001) The treatment of pilon fractures. Orthop Clin North Am 32:91–102. https://doi.org/10.1016/S0030-5898(05)70196-6
Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M (2006) Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma 20:76–79. https://doi.org/10.1097/01.bot.0000202997.45274.a1
Gao H, Zhang CQ, Luo CF, Zhou ZB, Zeng BF (2009) Fractures of the distal tibia treated with polyaxial locking plating. Clin Orthop Relat Res 467:831–837. https://doi.org/10.1007/s11999-008-0459-1
Bozkurt M, Ocquder DA, Uguru M, Kalkan T (2008) Tibial Pilon Fracture repair using Ilizarov External Fixation, Capsuloligamentotaxis and early Rehabilitation of the ankle. J Foot Ankle Surg 47(4):302–306. https://doi.org/10.1053/j.jfas.2008.02.013
Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P et al (2010) Distal tibia fractures: management and complications of 101 cases. Int Orthop 34:583–588. https://doi.org/10.1007/s00264-009-0832-z
Antonova E, Le Burge TKR, Mershon J (2013) Tibia shaft fractures: costly burden of nonunions. BMC Musculoskeletal Disord 14:42. https://doi.org/10.1186/1471-2474-14-42
Vallier HA, Cureton BA, Patterson BM (2011) Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma 25:736–741. https://doi.org/10.1097/BOT.0b013e318213f709
Barcak E, Collinge CA (2016) Metaphyseal distal tibia fractures: a cohort, single-surgeon study comparing outcomes of patients treated with minimally invasive plating versus intramedullary nailing. J Orthop Trauma 30(5):169–174. https://doi.org/10.1097/BOT.0000000000000530
Eralp IL, Kocaoglu M, Goksel D, Azam ME, Balci HI, Bilen E (2016) Treatment of infected non-unions of the juxta-articular region of distal tibia. Acta Orthop Traumatol Turc 50(2):139–146
Richard RD, Kubiak E, Horwitz DS (2014) Techniques for the surgical treatment of distal tibia fractures. Orthop Clin N Am 45:295–312. https://doi.org/10.1016/j.ocl.2014.04.001
Piper KJ, Won HY, Ellis AM (2005) Hybrid external fixation in complex tibial plateau and plafond fractures: an Australian audit outcomes. Injury 36:178–184. https://doi.org/10.1016/j.injury.2004.04.006
Leung F, Kwok HY, Pun TS, Chow SP (2004) Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury 35:278–283. https://doi.org/10.1016/S0020-1383(03)00172-4
Guo JJ, Tang N, Yang HL, Tang TS (2010) A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg 92:984–988
Zalavras CG, Patzakis MJ, Thordarson DB, Shah S, Sherman R, Holtom P (2004) Infected fractures of the distal tibial metaphysis and plafond, achievement of limb salvage with free flaps, bone grafting and ankle fusion. Clin Orthop Relat Res 427:57–62
Marsh JL, Rattay RE, Dulaney T (1997) Results of ankle arthrodesis for treatment of supramalleolar non-union. Foot Ankle Int 18:138–143
Molina CS, Stinner DJ, Fras AR, Evans JM (2015) Course of treatment and rate of successful salvage following the diagnosis of deep infection in patients treated for pilon fractures(AO/OTA:43). J Orthop 12:S18–S24. https://doi.org/10.1016/j.jor.2015.01.023
Green SA, Roesler S (1987) Salvage of the infected pilon fracture. Techniques in Orthopedics 2(3):37–41
Van der Merwe L, Birkholtz F, Tetsworth K, Hohmann E (2016) Functional and psychological outcomes of delayed lower limb amputation following failed lower limb reconstruction. Injury 47:1756–1760. https://doi.org/10.1016/j.injury.2016.05.027
Borrelli J, Leduc S, Gregush R, Ricci W (2009) Tricortical bone grafts for treatment of malaligned tibias and fibulas. Clin Orthop Relat Res 467:1056–1063. https://doi.org/10.1007/s11999-008-0657-x
Wyrsch B, Mcferran M, McAndrew M, Limbird T, Harper M, Johnson K et al (1996) Operative treatment of fractures of the tibial plafond. A randomized, prospective study. J Bone Joint Surg Am 78:1646–1657. https://doi.org/10.2106/00004623-199611000-00003
Cierny G 3rd, Mader JT, Penninck JJ (2003) A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res 414:7–24. https://doi.org/10.1097/01.blo.0000088564.81746.62
Hohmann E, Birkholtz F, Glatt V, Tetsworth K (2017) The “road to union” protocol for the reconstruction of isolated complex high-energy tibial trauma. Injury 48(6):1211–1216. https://doi.org/10.1016/j.injury.2017.03.018
Masquelet AC, Begue T (2010) The concept of induced membranes for reconstruction of long bone defects. Orthop Clin North Am 41:27–37. https://doi.org/10.1016/j.ocl.2009.07.011
Tetsworth K, Cierny G 3rd (1999) Osteomyelitis debridement techniques. Clin Orth Relat Res 360:87–96. https://doi.org/10.1097/00003086-199903000-00011
Heitmann C, Patzakis MJ, Tetsworth KD, Levin LS (2003) Musculoskeletal sepsis: principles of treatment. Instr Course Lect 52:733–743
Maruish M (2012) User’s manual for the SF-12v2 Health Survey, 3rd edn. Lincoln, London
Swiontkowski MF, Engelberg R, Martin DP, Agel J (1999) Short Musculoskeletal function assessment Questionnaire validity, Reliability and Responsiveness. JBJS 81A(9):1245–1260
Budiman-Mak E, Condrad KL, Roach KE (1991) The foot function index a measure of foot pain and disability. J Clin Epidemiol 44(6):561–570. https://doi.org/10.1016/0895-4356(91)90220-4
Harris AM, Patterson BM, Sontich JK, Vallier HA (2006) Results and outcomes after operative treatment of high-energy tibial plafond fractures. Foot Ankle Int 27(4):256–265. https://doi.org/10.1177/107110070602700406
Whelan DB, Bhandari M, Stephen D, Kreder H, McKee MD, Zdero R et al (2010) Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation. J Trauma 68:629–632. https://doi.org/10.1097/TA.0b013e3181a7c16d
Richmond J, Colleran K, Borens O, Kloen P, Helfet DL (2004) Nonunions of the distal tibia treated by reamed intramedullary nailing. J Orthop Trauma 18:603–610. https://doi.org/10.1097/00005131-200410000-00005
Laklouk MAS (2003) Ilizarov fixator as a method of treatment of failed internal fixation of distal tibial fractures. Egypt Orthop J 48:88–94
Arvesen JE, Watson T, Israel H (2017) Effectiveness of treatment for distal tibial nonunions with associated complex deformities using a hexapod external fixator. J Orthop Trauma 31:e43–e48. https://doi.org/10.1097/BOT.0000000000000726
Demetriades D, Martin M, Salim A, Rhee P, Brown C, Chan L (2005) The effect of trauma center designation and trauma volume on outcome in specific severe injuries. Ann Surg 242:512–519. https://doi.org/10.1097/01.sla.0000184169.73614.09
Cudnik MT, Newgard CD, Sayre MR, Steinberg SM (2009) Level I versus Level II trauma centers: an outcomes-based assessment. J Trauma 66(5):1321–1326. https://doi.org/10.1097/TA.0b013e3181929e2b
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in relation to the presented body of research.
Human and animal rights
This project was approved by the University of Pretoria, South Africa, Institutional Review Board and Human Research Ethics Committee.
Rights and permissions
About this article
Cite this article
Molepo, M., Barnard, AC., Birkholtz, F. et al. Functional outcomes of the failed plate fixation in distal tibial fractures salvaged by hexapod external fixator. Eur J Orthop Surg Traumatol 28, 1617–1624 (2018). https://doi.org/10.1007/s00590-018-2231-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2231-x