Abstract
Purpose
The purpose of this study is to perform a systematic review and meta-analysis of all available level I prospective randomized controlled trials comparing arthroscopic single-row (SR) with double-row (DR) rotator cuff repairs by both clinical outcomes and radiological re-tear rates.
Methods
PubMed, EMBASE, Google Scholar, and Cochrane databases search was done for level I RCTs comparing clinical and radiological outcomes after SR versus DR rotator cuff repair. Clinical outcomes included UCLA, ASES, Constant, WORC, and SANE scores; structural outcomes included MRI, MRA, or US.
Results
Seven level I studies were included (5 mid-term and 2 short-term). Postoperative ASES, Constant, WORC, and SANE scores showed nonsignificant slightly better function of DR groups. Only, UCLA score showed significantly better scores with DR repair (p = 0.007). Full-thickness re-tear incidence was reported in 15/174 (8.6%) in DR group and 20/175 (11.4%) in SR group (p = 0.44). Partial-thickness re-tear rate was reported in 18/174 patients (10.3%) in DR group and 41/175 patients (23.4%) in SR group (p = 0.009).
Conclusion
Within the domain of level I mid-term and short-term studies, DR repair showed significant better UCLA score only. (ASES, Constant, WORC, and SANE scores showed no significance.) This may correlate weakly with the significant lower partial-thickness re-tear rates of DR repairs. In contrary, long-term level III studies showed a direct correlation of both functional outcomes and cuff structural integrity, with significant superiority of DR over SR repair techniques.
Level of evidence
Level 1, systematic review and meta-analysis.
Similar content being viewed by others

Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arthroscopic rotator cuff repair (RCR) has become popular in the last decades as it avoids large skin incisions, deltoid detachment, dysfunction, and postoperative pain, and it allows the surgeon to detect and treat other associated shoulder pathologies [1].
Earlier arthroscopic single-row (SR) repair methods achieved only partial restoration of the original footprint of the tendons of the rotator cuff. Subsequently, double-row (DR) repair methods showed better restoration of the footprint area, less micro-movements, and better homogeneous compression pressure through the tendon [2].
The former biomechanical advantages aided higher healing rates with DR repair as concluded by Ma et al. [3]. These data lead to a paradigm shift in arthroscopic RCR to the DR techniques, which unfortunately failed to give better clinical results over SR repair in further studies [2, 4,5,6,7].
Many systematic reviews [8,9,10,11] and meta-analyses [1, 2, 5, 6, 12,13,14,15,16,17,18] were done to compare the two repair techniques. However, the inclusion of level II [1, 13, 14, 16, 17] and III [12, 19] trials or level I trials [5, 10, 15] that do not strictly rely on both functional and radiographic evaluations creates a potential source of heterogeneity that interferes with accurate analysis of the relation of the function to the cuff integrity after both techniques [20]. Consequently, their evidence supports the equivocal integrity and functional outcomes of both SR and DR techniques, which does not correlate with the proven biomechanical advantage of DR technique. Moreover, due to the paucity of long-term studies, most of these studies depend on short- and mid-term results, which do not give enough time for DR technique to show significant functional and structural superiority over SR repair.
The purpose of this study is to perform a meta-analysis of only level I prospective RCTs strictly studying both clinical outcomes and radiological re-tear rates of arthroscopic single-row versus double-row rotator cuff repairs until November 2017. Our hypothesis assumes that when considering the simultaneous analysis of both functional outcomes together with the structural integrity, DR repair technique gives better clinical outcomes and lower re-tear rate.
Materials and methods
Study design
This systematic review and meta-analysis were started in October 2016 according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [21] and the protocol described by Harris et al. [22]. Only level I randomized controlled clinical trials comparing both clinical and structural outcomes after arthroscopic single-row and double-row rotator cuff repairs were included. The latest date for this search was May 18, 2017.
Search technique
Electronic databases, including PubMed, EMBASE, Google scholar, and the Cochrane Central Register of Controlled Trials were searched for full-text trials from January 2000 till May 2017. The search was language unrestricted and used the following terms: (1) Rotator cuff tear, (2) rotator cuff arthroscopic repair, (3) single-row repair, (4) double-row repair, (5) structural and clinical outcomes of rotator cuff tear repair. The references of retrieved articles were further searched for potential eligible trials. When necessary, included articles’ authors were contacted for further data. Two reviewers independently reviewed the titles and abstracts to identify articles meeting the eligibility criteria.
Eligibility criteria
Studies were included in meta-analysis only if met the following inclusion criteria:
Inclusion criteria
Type of studies Level I evidence prospective randomized controlled trials (RCTs), comparing both structural and clinical outcomes of SR versus DR RCR.
Type of subjects Rotator cuff tear with a thickness larger than 10 mm, of any age, gender, physical, or sports activity.
Type of surgeries Arthroscopic rotator cuff repairs using suture anchors.
Duration of follow-up Postoperative follow-up should be at least 1 year.
Type of clinical outcome measures Either University of California Los Angeles (UCLA) [23], American Shoulder and Elbow Surgeons (ASES) [24], Constant [25], Western Ontario Rotator Cuff Index (WORC) [26], or Single Assessment Numerical Evaluation (SANE) [27] scores should be used as measures for clinical evaluation.
Type of structural evaluation Either MRI, MRA, or US should be used as a radiological tool for structural evaluation of healing or re-tear [8, 28,29,30].
Exclusion criteria
-
1.
Non-randomized controlled trials.
-
2.
Retrospective studies.
-
3.
Trials that did not use arthroscopic or suture anchors techniques.
-
4.
Trials that did not involve imaging for structural evaluation.
-
5.
Trials that did not include both single-row and double-row repairs.
-
6.
Trials published before the year 2000.
Data extraction
Retrieved studies methodological quality, procedures, and outcomes were reviewed independently by 2 reviewers (AHK, MRH). Disagreements were resolved by discussion until consensus was reached. If the 2 reviewers could not reach a consensus, the third author (MHS) was asked for a final opinion, resulting in a group agreement.
Data synthesis and statistical methods
Extracted data from the included studies were pooled for meta-analysis using RevMan® v5.3.5 software (Nordic Cochrane Centre, Copenhagen, Denmark). Continuous data (UCLA score, ASES score, Constant score, WORC index, and SANE score) were reported as standardized mean differences using the inverse variance statistical method and random effects analysis model. Dichotomous data (MRA/MRI/US detected re-tear rate) were reported as odds ratio using Mantel–Haenszel statistical method and random effects analysis model. Heterogeneity was determined by estimating the proportion of between-study inconsistencies due to actual differences between studies, rather than differences due to random error or chance, using the I2 statistics. Study confidence interval (CI) was adjusted at the 95% level.
Results
Study selection
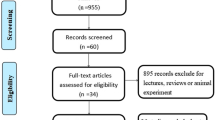
From the 3993 retrieved articles, only 747 are chosen after removal of duplicates and exclusion of non-arthroscopic studies. Only 139 studies remained after exclusion of non-comparative studies and decreased to 17 after selecting articles comparing SR versus DR repairs. With thorough review of the studies, only 7 studies met our eligibility criteria (Table 1, Fig. 1):
-
1.
Franceschi et al [31].
-
2.
Burks et al. [32].
-
3.
Koh et al. [33].
-
4.
Lapner et al. [34].
-
5.
Carbonel et al. [35].
-
6.
Barber [36].
-
7.
Franceschi et al. [37].
The last two studies have never been included in any previous systematic review or meta-analysis.
Study characteristics and patients population
The seven studies included 500 patients underwent rotator cuff repairs (only 477 were available at the final follow-up), 241 with single-row technique and 236 with double-row technique (Fig. 1). All the seven RCTs compared postoperative clinical outcomes and radiological (MRA/MRI/US) re-tear rate between both techniques. Only Burks et al. [32] used all the proposed clinical outcome scores (ASES, UCLA, Constant, WORC, and SANE), two studies [33, 35] used 3 scores (ASES, Constant, and UCLA), while Lapner et al. [34] used other 3 scores (ASES, Constant, and WORC). Barber et al. [36] used other 3 scores (ASES, Constant, and SANE). Franceschi et al. [31, 37] used only the UCLA score.
All the included studies (465 out of 477 patients) used radiological assessment to detect postoperative re-tear rate, but only 5 studies [31, 33, 35,36,37] stratified the re-tears into partial and full-thickness tears (349 patients). Barber et al. [36] and Burks et al. [32] were short-term studies (minimum 12 months), while other included studies [31, 33,34,35, 37] were mid-term studies (minimum 24 months) (Table 2).
Quality assessment
The methodological quality of included studies was appraised with CONSORT (Consolidated Standards on Reporting Trials) checklist and scoring system [46]. Included studies scored between 15 and 20 points, which was consistent with excellent to good quality (Table 3).
Risk of bias
Two reviewers independently assessed each trial’s risk of bias that may inhibit study interpretation using the Cochrane Collaboration’s tool [47]. The bias risk of the seven studies was mainly of attritional type (71%) due to incomplete MRI/MRA/US assessments for all subjects in 2 studies [32, 34]. Other types of bias were all of low risk among included studies (Fig. 2).
Operative details
Details of surgical procedures done for every study (no of suture anchors, material and operative techniques and rehabilitation program) are shown in Table 4.
Clinical outcome scores (Fig. 3)
UCLA Score was reported in 5 of the included studies [31,32,33, 35, 37]. It was done on 182 patients enrolled in DR repair, and 182 enrolled in SR repair. It was the only score that showed statistically significant better scores with DR repair (p = 0.004).
The postoperative UCLA, ASES, Constant, WORC, and SANE scores mean difference analysis between SR and DR using the inverse variance statistical method with forest plots, and heterogeneity calculation. Note that only UCLA score that showed statistically significant better clinical outcome for DR repairs
ASES and Constant Scores were reported in 5 of the included studies [32,33,34,35,36]. They were reported for 185 patients enrolled in the DR, and 190 patients enrolled in the SR. Although DR scored slightly higher means for both scores, they were statistically nonsignificant (p = 0.10 and 0.32, respectively).
WORC Index was reported only in 2 studies [32, 34]. It was done on 54 patients enrolled in the DR, and 59 patients enrolled in the SR. Also, it showed no statistical significance between both groups (p = 0.92).
SANE Score was reported in 2 studies [32, 36]. It was done on 80 patients divided equally between DR and SR techniques. Also, it showed no statistical significance between both techniques (p = 0.86).
Radiographic outcomes (Fig. 4)
Included studies mainly used MR to assess re-tear rate; Lapner et al. [34] used 65 US/11 MRIs, while Franceschi et al. [31, 37] used MRA in two studies as the most sensitive tool to detect re-tears after RCR [28].
Overall re-tear rate including partial and full-thickness re-tears was reported in all studies. Data showed a lower re-tear rate of DR group (45/231 patients), as compared to SR group (76/234 patients). This difference was statistically significant (p = 0.001).
Only 5 studies stratified detected re-tears into partial and full thickness [31, 33, 35,36,37]. Full-thickness re-tear incidence was reported in 15 of the 174 patients enrolled to the DR group, and 20 of the 175 patients enrolled to the SR group, which showed no significance between both groups (p = 0.44).
Partial-thickness re-tear rate was reported in 18 of the 174 patients in DR group and 41 of the 175 patients in SR group. This showed a statistical significance between both groups (p = 0.009) (Fig. 4).
Discussion
Generally, there is a development of optimal RC repair evidence over time due to improvements in learning curves, arthroscopic techniques, anchors geometry, suture material, and study designs. That was reflected on the results of different systematic reviews and meta-analysis over time (Table 5). Earlier studies were of systematic review nature and of equivocal results between the two techniques, while more recent studies are of meta-analysis nature and with a tendency to show lower re-tear rate after DR repairs. Moreover, both are of short- and mid-term outcomes.
The current study provides an evidence based only on level I RCTs to avoid the possible bias associated with cohorts, and exclusively on studies which used functional and radiological evaluations together. The inclusion of studies with either evaluation creates a potential source of heterogeneity with that interferes with accurate analysis of the relationship between the cuff integrity and function.
Clinical outcomes (Fig. 3)
Although our study showed better clinical outcomes (UCLA, ASES, and Constant) of the DR over SR repairs, only UCLA score showed a statistical significance between both groups. This evidence is consistent with previous meta-analyses [1, 12, 18]. But, this DR superiority could be attributed to the large number of cases enrolled in Carbonel et al. [35] study (weight = 65.4%), which was the only study with significant higher UCLA score of the DR technique. This pushed the authors further to study the actual sample size needed to detect statistical significance for every score. To avoid a β-error for any study, it should be powered to detect a mean difference of 2 points for UCLA score, and 5 points for Constant and ASES scores [12, 13]. Unfortunately, only Carbonel et al. [35] who reached the needed sample size to avoid this type-II error for UCLA score only, but not for ASES nor Constant scores. Other included studies [31,32,33,34, 36, 37] did not achieve that goal either. This raises a flag that adequately calculated sample sizes may give significant functional outcome differences with other scores.
Moreover, despite the wide use of UCLA score, it has poor responsiveness, reliability, and validity [48,49,50]. Other scores ASES, Constant, and WORC are well validated for rotator cuff repair. Single Assessment Numeric Evaluation (SANE) is simple but not validated, and in our analysis, it was used only in 2 included studies, same for WORC score. So, the evidence of the WORC and SANE scores in our study was not enough to support any conclusion. Therefore, it is advised to study an adequate sample size with a well-validated score for rotator cuff repair to support either repair techniques.
Subgroup analysis according to tear size is a very appealing approach, as evidence showed differences between the DR and SR techniques only in large to massive tears. Park et al. [44] were the first investigators who stratified their data according to tear size and found better function and lower re-tear rates with DR technique in large tears only. Carbonel et al. [35] did the same subgroup analysis and found only better functional scores with DR repairs in tears larger than 3 cm. Ma et al. [3] found only superior shoulder strength with DR repairs in 3–5 cm tears, but could not detect any difference as regard the integrity or the functional outcomes between the two techniques. In our meta-analysis, this subgrouping was not possible, as Carbonel et al. study [35] was the only included study with such categorization according to tear size. Subsequently, we strongly recommend further RCTs studying the differences of DR and SR techniques according to tear size.
Imaging outcomes (Fig. 4)
The radiographic results of our meta-analysis showed statistical significance between DR and SR in the overall and partial-thickness re-tear incidence. While, full-thickness re-tear incidence results showed no statistical significance between both techniques, indicating that the overall re-tear incidence is mainly due to partial-thickness type which occurs more after SR repairs. This was consistent with the results of Millet et al. [5]. and Chen et al. [12] , but they concluded that cuff integrity does not correlate with shoulder function. In our meta-analysis, DR repairs showed better cuff integrity that correlated with better functional outcomes that was significant only with UCLA score.
The relation between clinical and imaging outcomes
The relationship between cuff integrity and function is complex [20], and when we analyzed all the studies with the whole spectrum of follow-up periods, we found that this relation follows a tri-phasic pattern over time. While short-term studies [32, 36] tend to give equivocal results for both techniques, mid-term studies [31, 33,34,35, 37] tend to give the same function but lower re-tear rate with DR technique. However, long-term level III studies [40, 51,52,53] show a direct correlation between function and integrity with significant superiority of DR repairs. Moreover, partial re-tears after SR repairs eventually would turn into full-thickness tears over time with a dramatic deterioration of shoulder function. Unfortunately, these studies are not included in our meta-analysis due its lower level of evidence, but, it is the strongest available evidence with the longest follow-up periods. Consequently, the phrase of “cuff integrity does not correlate with shoulder function” turns invalid over time and should be abandoned.
Limitations
There were many limitations encountered during making this study.
First limitation was the paucity of RCTs that met our inclusion criteria, with the consequent relative decreased effect size. But the strong construct, level of evidence, and the thoroughly scrutinized included studies gave the current study a strong consistency.
Second was the unavoidable lack of standard measures used in all studies like the different operative techniques, no. of anchors, knot types, follow-up periods, and rehabilitation protocols created an unavoidable performance bias that could affect the final results.
Third, we tried to include more clinical outcomes like ROM and strength, but that was not applicable due to the heterogeneous classification systems used in every study to assess these aspects.
Fourth, the heterogeneous radiographic modalities of different studies raise a potential source of assessment bias.
Finally, we also were unable to stratify the results of our meta-analysis according to the initial tear size, due to the paucity of the studies comparing single-row and double-row according to tear sizes. Up till now, to our knowledge, only Carbonel randomized controlled trial is the only level I study comparing the clinical and imaging results between SR and DR arthroscopic techniques, according to the tear size [35].
Recommendations
Future more powered and high-level trials and meta-analyses should be directed to be more consistent with the procedures and assessments, and to be with longer follow-ups, and to study the following variables effects;
-
Initial tear size.
-
Muscle atrophy or fatty infiltration.
-
Other repair methods: suture bridge, transosseous, speed fix, etc.
-
Anchor type: metal, PEEK, biodegradable, vented, etc.
-
Number of sutures per anchor.
-
Suture type: high-tensile sutures and suture tapes.
-
Suture technique: sliding versus half hitches, or simple, mattress, and modified Mason Alan.
-
Immobilization and rehabilitation technique.
Conclusion
Within the domain of level I mid-term and short-term studies, DR repair showed significant better UCLA score only. (ASES, Constant, WORC, and SANE scores showed no significance.) This may correlate weakly with the significant lower partial-thickness re-tear rates of DR repairs. In contrary, long-term level III studies showed a direct correlation of both functional outcomes and cuff structural integrity, with significant superiority of DR over SR repair techniques.
References
Xu C, Zhao J, Li D (2014) Meta-analysis comparing single-row and double-row repair techniques in the arthroscopic treatment of rotator cuff tears. J Shoulder Elbow Surg 23(2):182–188. https://doi.org/10.1016/j.jse.2013.08.005
DeHaan AM, Axelrad TW, Kaye E, Silvestri L, Puskas B, Foster TE (2012) Does double-row rotator cuff repair improve functional outcome of patients compared with single-row technique? A systematic review. Am J Sports Med 40(5):1176–1185. https://doi.org/10.1177/0363546511428866
Ma HL, Chiang ER, Wu HT, Hung SC, Wang ST, Liu CL, Chen TH (2012) Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthrosc J Arthrosc Relat Surg 28(1):16–24. https://doi.org/10.1016/j.arthro.2011.07.003
Spiegl UJ, Euler SA, Millett PJ, Hepp P (2016) Summary of meta-analyses dealing with single-row versus double-row repair techniques for rotator cuff tears. Open Orthop J 10:330–338. https://doi.org/10.2174/1874325001610010330
Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ (2014) Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg 23(4):586–597. https://doi.org/10.1016/j.jse.2013.10.006
Brown MJ, Pula DA, Kluczynski MA, Mashtare T, Bisson LJ (2015) Does Suture technique affect re-rupture in arthroscopic rotator cuff repair? A meta-analysis. Arthrosc J Arthrosc Relat Surg 31(8):1576–1582. https://doi.org/10.1016/j.arthro.2015.02.004
Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D (2007) Can a double-row anchorage technique improve tendon healing in arthroscopic rotator cuff repair?: A prospective, nonrandomized, comparative study of double-row and single-row anchorage techniques with computed tomographic arthrography tendon healing assessment. Am J Sports Med 35(8):1247–1253. https://doi.org/10.1177/0363546507301661
Duquin TR, Buyea C, Bisson LJ (2010) Which method of rotator cuff repair leads to the highest rate of structural healing? A systematic review. Am J Sports Med 38(4):835–841. https://doi.org/10.1177/0363546509359679
Saridakis P, Jones G (2010) Outcomes of single-row and double-row arthroscopic rotator cuff repair: a systematic review. J Bone Joint Surg Am 92(3):732–742. https://doi.org/10.2106/JBJS.I.01295
Trappey GJ, Gartsman GM (2011) A systematic review of the clinical outcomes of single row versus double row rotator cuff repairs. J Shoulder Elbow Surg 20(2 Suppl):S14–S19. https://doi.org/10.1016/j.jse.2010.12.001
Wall LB, Keener JD, Brophy RH (2009) Clinical outcomes of double-row versus single-row rotator cuff repairs. Arthrosc J Arthrosc Relat Surg 25(11):1312–1318. https://doi.org/10.1016/j.arthro.2009.08.009
Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y (2013) Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Orthopedics 29(8):1437–1449. https://doi.org/10.1016/j.arthro.2013.03.076
Perser K, Godfrey D, Bisson L (2011) Meta-analysis of clinical and radiographic outcomes after arthroscopic single-row versus double-row rotator cuff repair. Sports Health 3(3):268–274. https://doi.org/10.1177/1941738111403106
Prasathaporn N, Kuptniratsaikul S, Kongrukgreatiyos K (2011) Single-row repair versus double-row repair of full-thickness rotator cuff tears. Arthrosc J Arthrosc Relat Surg 27(7):978–985. https://doi.org/10.1016/j.arthro.2011.01.014
Sheibani-Rad S, Giveans MR, Arnoczky SP, Bedi A (2013) Arthroscopic single-row versus double-row rotator cuff repair: a meta-analysis of the randomized clinical trials. Arthrosc J Arthrosc Relat Surg 29(2):343–348. https://doi.org/10.1016/j.arthro.2012.11.019
Shen C, Tang ZH, Hu JZ, Zou GY, Xiao RC (2014) Incidence of retear with double-row versus single-row rotator cuff repair. Orthopedics 37(11):e1006–e1013. https://doi.org/10.3928/01477447-20141023-58
Ying ZM, Lin T, Yan SG (2014) Arthroscopic single-row versus double-row technique for repairing rotator cuff tears: a systematic review and meta-analysis. Orthop Surg 6(4):300–312. https://doi.org/10.1111/os.12139
Zhang Q, Ge H, Zhou J, Yuan C, Chen K, Cheng B (2013) Single-row or double-row fixation technique for full-thickness rotator cuff tears: a meta-analysis. PLoS ONE 8(7):e68515. https://doi.org/10.1371/journal.pone.0068515
Slabaugh MA, Nho SJ, Grumet RC, Wilson JB, Seroyer ST, Frank RM, Romeo AA, Provencher MT, Verma NN (2010) Does the literature confirm superior clinical results in radiographically healed rotator cuffs after rotator cuff repair? Arthrosc J Arthrosc Relat Surg 26(3):393–403. https://doi.org/10.1016/j.arthro.2009.07.023
Dines JS, Bedi A, ElAttrache NS, Dines DM (2010) Single-row versus double-row rotator cuff repair: techniques and outcomes. JAAOS J Am Acad Orthop Surg 18(2):83–93
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62(10):e1–e34. https://doi.org/10.1016/j.jclinepi.2009.06.006
Harris JD, Quatman CE, Manring MM, Siston RA, Flanigan DC (2014) How to write a systematic review. Am J Sports Med 42(11):2761–2768. https://doi.org/10.1177/0363546513497567
Ellman H, Hanker G, Bayer M (1986) Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am 68(8):1136–1144
Tashjian RZ, Hollins AM, Kim HM, Teefey SA, Middleton WD, Steger-May K, Galatz LM, Yamaguchi K (2010) Factors affecting healing rates after arthroscopic double-row rotator cuff repair. Am J Sports Med 38(12):2435–2442. https://doi.org/10.1177/0363546510382835
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Kirkley A, Alvarez C, Griffin S (2003) The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med 13(2):84–92
Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC (1999) Comparison of the single assessment numeric evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med 27(2):214–221. https://doi.org/10.1177/03635465990270021701
de Jesus JO, Parker L, Frangos AJ, Nazarian LN (2009) Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol 192(6):1701–1707. https://doi.org/10.2214/AJR.08.1241
Prickett WD, Teefey SA, Galatz LM, Calfee RP, Middleton WD, Yamaguchi K (2003) Accuracy of ultrasound imaging of the rotator cuff in shoulders that are painful postoperatively. J Bone Joint Surg Am 85A(6):1084–1089
Saccomanno MF, Cazzato G, Fodale M, Sircana G, Milano G (2015) Magnetic resonance imaging criteria for the assessment of the rotator cuff after repair: a systematic review. Knee Surg Sports Traumatol Arthrosc 23(2):423–442. https://doi.org/10.1007/s00167-014-3486-3
Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V (2007) Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med 35(8):1254–1260. https://doi.org/10.1177/0363546507302218
Burks RT, Crim J, Brown N, Fink B, Greis PE (2009) A prospective randomized clinical trial comparing arthroscopic single- and double-row rotator cuff repair: magnetic resonance imaging and early clinical evaluation. Am J Sports Med 37(4):674–682. https://doi.org/10.1177/0363546508328115
Koh KH, Kang KC, Lim TK, Shon MS, Yoo JC (2011) Prospective randomized clinical trial of single- versus double-row suture anchor repair in 2- to 4-cm rotator cuff tears: clinical and magnetic resonance imaging results. Arthrosc J Arthrosc Relat Surg 27(4):453–462. https://doi.org/10.1016/j.arthro.2010.11.059
Lapner PL, Sabri E, Rakhra K, McRae S, Leiter J, Bell K, Macdonald P (2012) A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am 94(14):1249–1257. https://doi.org/10.2106/JBJS.K.00999
Carbonel I, Martinez AA, Calvo A, Ripalda J, Herrera A (2012) Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop 36(9):1877–1883. https://doi.org/10.1007/s00264-012-1559-9
Barber FA (2016) Triple-loaded single-row versus suture-bridge double-row rotator cuff tendon repair with platelet-rich plasma fibrin membrane: a randomized controlled trial (some data retrieved with personal communication). Orthop J Sports Med 32(5):753–761. https://doi.org/10.1016/j.arthro.2015.11.020
Franceschi F, Papalia R, Franceschetti E, Palumbo A, Del Buono A, Paciotti M, Maffulli N, Denaro V (2016) Double-row repair lowers the retear risk after accelerated rehabilitation (some data retrieved with personal communication). Am J Sports Med 44(4):948–956. https://doi.org/10.1177/0363546515623031
Nicholas SJ, Lee SJ, Mullaney MJ, Tyler TF, Fukunaga T, Johnson CD, McHugh MP (2016) Functional outcomes after double-row versus single-row rotator cuff repair: a prospective randomized trial. Orthop J Sports Med 4(10):1–8. https://doi.org/10.1177/2325967116667398
Gartsman GM, Drake G, Edwards TB, Elkousy HA, Hammerman SM, O’Connor DP, Press CM (2013) Ultrasound evaluation of arthroscopic full-thickness supraspinatus rotator cuff repair: single-row versus double-row suture bridge (transosseous equivalent) fixation Results of a prospective, randomized study. J Shoulder Elbow Surg 22(11):1480–1487. https://doi.org/10.1016/j.jse.2013.06.020
Denard PJ, Jiwani AZ, Ladermann A, Burkhart SS (2012) Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthrosc J Arthrosc Relat Surg 28(7):909–915. https://doi.org/10.1016/j.arthro.2011.12.007
Mihata T, Watanabe C, Fukunishi K, Ohue M, Tsujimura T, Fujiwara K, Kinoshita M (2011) Functional and structural outcomes of single-row versus double-row versus combined double-row and suture-bridge repair for rotator cuff tears. Am J Sports Med 39(10):2091–2098. https://doi.org/10.1177/0363546511415660
Aydin N, Kocaoglu B, Guven O (2010) Single-row versus double-row arthroscopic rotator cuff repair in small- to medium-sized tears. J Shoulder Elbow Surg 19(5):722–725. https://doi.org/10.1016/j.jse.2009.11.053
Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C (2009) Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthrosc J Arthrosc Relat Surg 25(1):4–12. https://doi.org/10.1016/j.arthro.2008.09.018
Park JY, Lhee SH, Choi JH, Park HK, Yu JW, Seo JB (2008) Comparison of the clinical outcomes of single- and double-row repairs in rotator cuff tears. Am J Sports Med 36(7):1310–1316. https://doi.org/10.1177/0363546508315039
Sugaya H, Maeda K, Matsuki K, Moriishi J (2005) Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: single-row versus dual-row fixation. Arthrosc J Arthrosc Relat Surg 21(11):1307–1316. https://doi.org/10.1016/j.arthro.2005.08.011
Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P, Group C (2008) Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med 148(4):295–309
Higgins JP, Altman DG (2011) Assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions Version 5.2.0. The Cochrane Collaboration. Wiley, Hoboken
Kirkley A, Griffin S, Dainty K (2003) Scoring systems for the functional assessment of the shoulder. Arthrosc J Arthrosc Relat Surg 19(10):1109–1120. https://doi.org/10.1016/j.arthro.2003.10.030
Romeo AA, Bach BR Jr, O’Halloran KL (1996) Scoring systems for shoulder conditions. Am J Sports Med 24(4):472–476. https://doi.org/10.1177/036354659602400411
Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW (2012) Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am 94(3):277–285. https://doi.org/10.2106/JBJS.J.01744
Kluger R, Bock P, Mittlbock M, Krampla W, Engel A (2011) Long-term survivorship of rotator cuff repairs using ultrasound and magnetic resonance imaging analysis. Am J Sports Med 39(10):2071–2081. https://doi.org/10.1177/0363546511406395
Kyrola K, Niemitukia L, Jaroma H, Vaatainen U (2004) Long-term MRI findings in operated rotator cuff tear. Acta Radiol 45(5):526–533
Vastamaki M, Lohman M, Borgmastars N (2013) Rotator cuff integrity correlates with clinical and functional results at a minimum 16 years after open repair. Clin Orthop Relat Res 471(2):554–561. https://doi.org/10.1007/s11999-012-2494-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have nothing to disclose.
Rights and permissions
About this article
Cite this article
Sobhy, M.H., Khater, A.H., Hassan, M.R. et al. Do functional outcomes and cuff integrity correlate after single- versus double-row rotator cuff repair? A systematic review and meta-analysis study. Eur J Orthop Surg Traumatol 28, 593–605 (2018). https://doi.org/10.1007/s00590-018-2145-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2145-7