Abstract
The ideal implant for the treatment of an unstable intertrochanteric femoral fracture is still a matter of discussion. The aim of this systematic review is to conduct a network meta-analysis of randomized controlled trials (RCTs) comparing clinical outcomes between dynamic hip screws (DHS), Medoff sliding plating, percutaneous compression plating (PCCP), proximal femoral nails (PFN), Gamma nails and less invasive stabilization system fixation in femoral trochanteric fractures in the elderly. These clinical outcomes consist of total intra-operative time, intra-operative fluoroscopy time, intra-operative blood loss, blood component transfusion, length of hospital stay, postoperative general complications, wound complications, late complications and reoperation rates. This systematic review was conducted using PubMed and Scopus search engines for RCTs comparing clinical outcomes between treatments from inception to February 22, 2015. Thirty-six of 785 studies identified were eligible. Compared to the other implants, PCCP showed the lowest total operative time and units of blood transfusion with an unstandardized mean difference (UMD) of 29.27 min (95% CI 5.24, 53.50) and 0.89 units (95% CI 0.52, 1.25). The lowest incidence of general complications, wound complications and late complications of PCCP was 0.09 (95% CI 0.04, 0.18), 0.01 (95% CI 0.01, 0.04) and 0.05 (95% CI 0.02, 0.11), respectively, when compared to others. The lowest fluoroscopic time was with DHS with an UMD of 0.24 min (95% CI 0.16, 0.32), whereas the lowest blood loss and shortest hospital stay were with PFN with an UMD of 233.61 ml of blood loss (95% CI 153.17, 314.04) and 7.23 days of hospital stay (95% CI 7.15, 7.31) when compared to all other fixation methods. Reoperation rates of all implants had no statistically significant difference. The network meta-analysis suggested that fixation with PCCP significantly shortens operative time and decreases the units of blood transfusion required, while also lowering risks of general complications, wound complications and late complications when compared to fixation. Use of PFN showed the least intra-operative blood loss and shortest hospital stay. Multiple active treatment comparisons indicate that PCCP fixation in trochanteric fractures in the elderly is the treatment of choice in terms of intra-operative outcomes and postoperative complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Options for treating intertrochanteric fractures include extramedullary fixation [dynamic hip screw (DHS), percutaneous compression plate (PCCP), Medoff sliding plate (MSP), less invasive stabilization system (LISS)] and intramedullary fixation [Gamma nail and proximal femoral nail with anti-rotating (PFNA)]. The ideal implant for the treatment is still a matter of discussion. DHS, the most representative implant of extramedullary fixation, has been considered the gold standard for treatment of intertrochanteric fractures. However, the failure rate of DHS is higher [10, 21] in the unstable and reverse oblique fracture, which limits its clinical use [11, 16]. Gotfried developed the PCCP technique; however, the PCCP lengthens operation time and increases biomechanical complications [12]. The MSP evolved from the DHS has produced remarkably good results in prospective trials in both unstable trochanteric and subtrochanteric fractures with a rate of failure of 2–4% [27]. LISS (the use of the distal femoral LISS in the proximal femur) has some advantages in the treatment of complex proximal femoral fractures in a more stable construct with higher pullout resistance [26]. Gamma nail has been widely used for many years because of its inspiring clinical results [2, 5]. Long-term studies, however, revealed that Gamma nail might cause higher intra-operative and late complications that often require revision surgery [4, 6]. PFNA provides angular and rotational stability, which is especially important in osteoporotic bone, and allows early mobilization and weight bearing on the affected limb [13, 17]. From literature review, we found 8 systematic reviews were published and dealing with the type of fixation of intertrochanteric fracture [7, 8, 15, 19, 22, 28,29,30]. However, none of the reviews compared all the implants, and none incorporated their comparative effectiveness using a network meta-analysis approach. The objective of the study was to assess the comparative effectiveness of different types of implants for intertrochanteric fracture fixation by combining direct and indirect evidence in a systematic review and network meta-analysis of RCTs with the aim of comparing relevant clinical outcomes between all implants.
Materials and methods
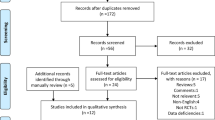
This systematic review and network meta-analysis were conducted following guideline in the preferred reporting items for systematic reviews and meta-analyses (PRISMA), extension of network meta-analyses [9].
Search strategy
The MEDLINE and Scopus databases were used to identify relevant studies published in English from the date of inception to February 22, 2015. The PubMed and Scopus search engines were used to locate studies using the following search terms: ((fracture intertrochanteric) (elder) OR (fracture femur)) AND ((proximal femural nail) OR (dynamic hip screw) OR (Gamma nail) OR (proximal femural nail anti rotation)) AND ((blood loss) OR (hospital stay) OR (failure rate) OR (femeral shaft fracture) OR (operative time) OR (complication)) AND (clinical trial or randomized controlled trial). Search strategies for MEDLINE and Scopus are described in “Appendix.” Relevant studies from the reference lists of identified studies and previous systematic reviews were also explored.
Selection of studies
Identified studies were selected by one author (JK) and randomly checked by (AA). Their titles and abstracts were initially screened, and full papers were retrieved if a decision could not be made from the abstracts. The reasons for ineligibility or exclusion of studies were recorded (Fig. 1).
Inclusion criteria
Randomized controlled trials or quasi-experimental designs that compared clinical outcomes between proximal femoral nail with anti-rotating, Gamma nails, percutaneous compression plate, Medoff sliding plate, less invasive stabilization system and dynamic hip screws for fixation in elderly trochanteric fractures were eligible if they met following criteria:
-
Compared clinical outcomes between proximal femoral nail with anti-rotating, Gamma nails, percutaneous compression plate, Medoff sliding plate, less invasive stabilization system and dynamic hip screws.
-
Compared at least one of following outcomes: operative time, fluoroscopy time, operative blood loss, length of hospital stays, wound complication (hematoma, infection and dehiscent), general complication (pneumonia, thromboembolic complications, fixation failure and fracture), late complication (fracture, malunion and nonunion) and reoperation.
-
Had sufficient data to extract and pool, i.e., the reported mean, standard deviation (SD), the number of subjects according to treatments for continuous outcomes, and the number of patients according to treatment for dichotomous outcomes.
Data extraction
Two reviewers (JK and AA) independently performed data extraction using standardized data extraction forms. General characteristics of the study (e.g., mean age, gender, body mass index (BMI), ASA status and mean follow-up time at baseline) were extracted. The number of subjects, mean, and SD of continuous outcomes (i.e., operative time, fluoroscopy time, operative blood loss and length of hospital stays) between groups were extracted. Cross-tabulated frequencies between treatment and all dichotomous outcomes (wound complication (hematoma, infection and dehiscent), general complication (pneumonia, thromboembolic complications, fixation failure, and fracture), late complication (fracture, malunion and nonunion) and reoperation) were also extracted. Any disagreements were resolved by discussion and consensus with a third party (TA).
Risk of bias assessment
Two authors (JK and AA) independently assessed risk of bias for each study. Six study quality domains were considered, consisting of sequence generation, allocation concealment, blinding (participant, personnel and outcome assessors), incomplete outcome data, selective outcome reporting and other sources of bias [28]. Disagreements between two authors were resolved by consensus and discussion with a third party (TA).
Outcomes
The outcomes of interest were operative time (OT), fluoroscopic time (FT), blood loss (BL), unit transfusion (UT), early postoperative (general complications and wound complications), hospital stay (HS), late postoperative complication and reoperation due to failure fixation. Methods of measure for these outcomes were used according to the original studies. Briefly, the operative time (min), fluoroscopic time (min), blood loss (ml), unit transfusion (unit), early postoperative [general complications (cut though, fracture, malposition, DVT) and wound complications (dehiscent and infection)], hospital stay (days), late postoperative complication (nonunion, fracture and failure fixation) and reoperation due to failure fixation were considered.
Statistical analysis
Direct comparisons of continuous outcomes measured at the end of each study between proximal femoral nail with anti-rotating, Gamma nails, percutaneous compression plate, Medoff sliding plate, less invasive stabilization system and dynamic hip screws were pooled using an unstandardized mean difference (UMD). Heterogeneity of the mean difference across studies was checked using the Q-statistic, and the degree of heterogeneity was quantified using the I 2 statistic. If heterogeneity was present as determined by a statistically significant Q-statistic or by I 2 > 25%, the UMD was estimated using a random effects model; otherwise, a fixed effects model was applied.
For dichotomous outcomes, a relative risk (RR) of postoperative complication of treatment comparisons at the end of each study was estimated and pooled. Heterogeneity was assessed using the previous method. If heterogeneity was present, the Dersimonian and Laird method [1] was applied for pooling. If not, the fixed effects model by inverse variance method was applied. Meta-regression was applied to explore the source of heterogeneity [e.g., mean age, percentage of females, body mass index (BMI), follow-up time and ASA status] if data were available. Publication bias was assessed using contour-enhanced funnel plots [18, 20] and Egger tests [3].
For indirect comparisons, network meta-analyses were applied to assess all possible effects of treatment if summary data were available for pooling [14, 23]. A linear regression model, weighted by inverse variance, was applied to assess the treatment effects for continuous outcomes. For postoperative complications (early and late) and reoperation, a mixed-effect Poisson regression was applied to assess treatment effects [14]. Summary data were expanded to individual patient data using the “expand” command in STATA. Treatment was considered as a fixed effect, whereas the study variable was considered as a random effect in a mixed-effect model. The pooled RR and its 95% confidence intervals (CIs) were estimated by exponential coefficients of treatments. All analyses were performed using STATA version 14.0 [25]. A p value <0.05 was considered statistically significant, except for the test of heterogeneity where <0.10 was used.
Results
Eighty and 743 studies from MEDLINE and Scopus were identified, respectively; 38 studies were duplicate, leaving 785 studies for review of titles and abstracts. Of these, 36 studies were reviewed and extracted. Characteristics of the 36 studies are described in Table 1. Among 28 dynamic hip screws studies, the comparators included proximal femoral nail with anti-rotating in 8 studies, Gamma nails in 14 studies, percutaneous compression plate in 5 studies and Medoff sliding plate in 2 studies. Comparing to proximal femoral nail with anti-rotating, the comparators included Gamma nail in 4 studies, LISS in 2 studies and PCCP in 1 study. Only one study compared Gamma nail to Medoff plate. Most studies included proximal femoral fracture type 31-A1–A3, followed by type 31-A2–A3 and type 31-A2. Mean age, BMI, type 3–4/1–2 ASA status ratio and follow-up time after surgery varied from 54 to 84 years, 21.8 to 24.3 kg/m2, 0.2 to 0.95 and 3 to 40 months, respectively. Percentage of females ranged from 30 to 88%. Various outcomes were compared between treatment groups (Fig. 1).
Risk of bias in included studies
Risk of bias assessment is described in Table 2.
Direct comparisons
Data for direct comparisons of all treatments and outcomes measured at the end of each study are described in Table 1. Pooling according to outcomes was performed if there were at least two studies for each comparison, as clearly described below.
Operative time
The mean operative time of PFNA was −22.6 min (95% CI −37.9, −7.3) statistically significant lower than LISS, whereas PFNA was 13.5 min (95% CI 7.54, 19.45) statistically significant higher than PCCP. There were no significant differences between Gamma nail, PFNA, PCCP and Medoff when compared to DHS. Comparing to Gamma nail, PFNA and Medoff were no statistically significant different (Table 3).
Fluoroscopic time
The mean fluoroscopic time of DHS was −0.50 (95% CI −0.79, −0.21) statistically significant lower than PFNA, while PFNA was −0.21 (95% CI −0.35, −0.08) statistically significant lower than LISS. There were no significant differences between DHS and PFNA when compared to Gamma nail (Table 3).
Blood loss
The mean blood loss of DHS was 30.12 (95% CI 1.30, 58.94) and 136.03 (95% CI 6.69, 265.37) statistically significant higher than Gamma nail and PFNA, whereas DHS was −195 (95% CI −312.16, −77.84) statistically significant lower than Medoff. Mean blood loss of PFNA was −60.67 (95% CI −71.55, 49.79) and −80.47 (95% CI −160.97, 0.04) statistically significant lower than Gamma nail and LISS (Table 3).
Unit transfusion
The mean unit transfusion of DHS was 0.34 unit (0.07, 0.61) statistically significant higher than PCCP. However, there were no significant differences between Gamma nail and PFNA groups when compared to DHS (Table 3).
Hospital stay
The mean hospital stay of DHS was 0.87 days (95% CI 0.28, 1.45) statistically significant longer than Gamma nail. When compared to PFNA, Gamma nail was longer hospital stay for more 0.20 days (0.13, 0.27), while LISS has statistically significant shorter hospital stay of 2.72 days (1.47, 3.97) when compared to PFNA.
Complications (general, wound and late) and reoperation
In terms of (general, wound and late) complications and reoperation, there were no significant differences risk between Gamma nail, PFNA and Medoff when compared to DHS (Table 3). And, there were no significant differences in risk between PCCP and LISS when compared to PFNA (Table 3). Three studies were pooled wound complication of DHS was 2.78 (95% CI 1.58, 4.89) which showed a significantly higher risk when compared with PCCP, and no heterogeneity (I 2 = 0) was present (Table 3), while five studies were pooled late complication of Gamma nail was 0.72 (95% CI 0.54, 0.97) which showed a significantly lower risk when compared with PFNA, and no heterogeneity (I 2 = 0) was present (Table 3).
Network meta-analysis
Operative time
Data from 31 studies: the regression analysis suggested that the mean operative time was lowest in the PCCP with an overall mean of 29.3 (95% CI 5.24, 53.3) followed by DHS (53.7, 95% CI 40.1, 67.3), PFN (60.6, 95% CI 56.6, 64.6), Gamma nail (62.3, 95% CI 56.3, 64.6) and LISS (84.2, 95% CI 76.1, 92.2) (as given in Table 4; Fig. 2). Multiple comparisons indicated that there was statistically significant higher operative time of DHS, Medoff, Gamma nail, PFN and LISS when compared to PCCP. While LISS was statistically significant lower operative time of DHS, Medoff, Gamma nail, PFN and PCCP when compared to LISS.
Network meta-analysis of treatment effects on operative time. A line in the figure represents treatment comparisons, with arrows and tails referring to intervention and comparators, respectively. Bold and dashed lines refer to direct and indirect comparisons, respectively. The number at the line indicates chance of treatment responsiveness, in which <0 indicates favors intervention vs the comparator. * p < 0.05 with Bonferroni correction
Fluoroscopic time
Data from 12 studies: the regression analysis suggested that the mean fluoroscopic time was lowest in the DHS with an overall mean of 0.24 min (95% CI 0.16, 0.32), while Gamma nail was highest with an overall mean of 1.83 min (95% CI −0.71, 4.37) (as given in Table 4; Fig. 2). Multiple comparisons indicated that there was no statistically significant difference in operative time of DHS, Gamma nail, PFN and LISS.
Blood loss
Data from 15 studies: the regression analysis suggested that the mean blood loss was lowest in the PFN with an overall mean of 233.6 (95% CI 153.2, 314.0) followed by DHS (266.8, 95% CI 256.6, 277), Gamma nail (276, 95% CI 264.1, 287.9), LISS (279.2, 95% CI 43.5, 514.9), PCCP (432.9, 95% CI −270.7, 1136.5) and Medoff (611.9, 95% CI 242.7, 981.5) (as given in Table 4; Fig. 2). Multiple comparisons indicated that there was no statistically significant blood loss of DHS, PCCP, Medoff, Gamma nail, PFN and LISS.
Unit transfusion
Data from 11 studies: the regression analysis suggested that the mean unit transfusion was lowest in the PCCP with an overall mean of 0.89 unit (95% CI 0.52, 1.25) followed by DHS (1.31, 95% CI 0.74, 1.88), PFN (1.54, 95% CI 0.52, 2.56), Gamma nail (1.6, 95% CI 0.58, 2.62) (as given in Table 4; Fig. 2). Multiple comparisons indicated that there was no statistically significant difference in unit transfusion of PCCP, DHS, PFN and Gamma nail.
Hospital stay
Data from 20 studies: the regression analysis suggested that the mean hospital stay was lowest in the PFN with an overall mean of 7.23 days (95% CI 7.15, 7.31), while DHS was highest with an overall mean of 10.31 days (95% CI 7.54, 13.08) (as given in Table 4; Fig. 2). Multiple comparisons indicated that there was statistically significant lower hospital stay of PCCP, Gamma nail and PFN when compared to Medoff.
Complications (general, wound and late) and reoperation
The regression analysis suggested that the incidence of having complications (general, wound and late) was lowest in the PCCP with an overall incidence of 0.09 (95% CI 0.04, 0.18), 0.01 (95% CI 0.01, 0.04) and 0.05 (95% CI 0.02, 0.11), respectively. The incidence of having general and late complications was highest in the LISS with an overall incidence of (0.21, 95% CI 0.06, 0.72 and 0.18, 95% CI 0.07, 0.11), while DHS has an incidence of wound complications of 0.05 (95% CI 0.04, 0.08). In terms of reoperation, there was no statistically significant difference between all implants.
Discussion
We have performed a systematic review and a network meta-analysis comparing effects of proximal femoral nail with anti-rotating, Gamma nails, percutaneous compression plate, Medoff sliding plate, less invasive stabilization system and dynamic hip screws for fixation in elderly trochanteric fractures. Relevant clinical outcomes included operative time, fluoroscopic time, blood loss, unit transfusion, early postoperative (general complications) and wound complications), hospital stay, late postoperative complications and reoperation due to failure fixation were pooled. Our results indicate that PCCP was the lowest operative time, unit transfusion and the chance of complications (general, wound and late) when compared to the other treatments. PFN was the lowest blood loss and hospital stay when compared to the other treatments, while the lowest fluoroscopic time was DHS fixation. Medoff plate was the highest blood loss and hospital stay when compared to the other treatments. Gamma nail was the highest fluoroscopic time and unit transfusion when compared to the other treatments, while LISS was the highest operative time and late complication when compared to the others (see Tables 4, 5). In terms of reoperation, there have no different chances of having reoperation between treatment groups.
The results of this study were consistent to previous meta-analyses [8, 15, 19, 22, 29, 30]; five studies were to compare proximal femoral nail (with or without anti-rotation). Three studies suggest that PFN can reduce blood loss, operative time, blood transfusion and fewer complications in the treatment of intertrochanteric fractures when compared with DHS, whereas two studies show the same effectiveness as DHS. One study was to compare PCCP and DHS; the review found that PCCP was associated with reduced blood loss and less transfusion need, but similar to DHS in operative time, hospital stay, mortality, complications and reoperation rate (Table 6). We, however, have added more evidences which supports that the PCCP, PFN and DHS may be a better choice than the others in the treatment of pertrochanteric fractures.
The direct meta-analysis suggests a potential benefit of PCCP for lowest operative time and unit transfusion while PFN and DHS for hospital stay and fluoroscopic time, but there was no different for complications and reoperation of all implants fixation. Performing a direct meta-analysis is limited by the small number of studies that evaluated each particular pair of treatments, but a network meta-analysis circumvents this problem by creating indirect comparisons between active treatments that can identify the most effective therapy.
This study has a number of strengths. We have applied a network meta-analysis to increase the power of the tests and reduce type I errors [14, 23, 24]. We applied a regression model taking into account study effects to assess treatment effects. The network meta-analysis ‘borrows’ treatment information from other studies and increases the total sample size. As a result, treatment effects that could not be detected in direct meta-analysis could be identified. All possible treatment comparisons are mapped and displayed (see Figs. 2, 3, 4, 5, 6). Although our pooled estimates were heterogeneous, the regression model with cluster effect takes into account variations at the study level. None of RCTs compared proximal femoral nail with anti-rotating, Gamma nails, percutaneous compression plate, Medoff sliding plate, less invasive stabilization system and dynamic hip screws in the treatment of pertrochanteric fractures.
Network meta-analysis of treatment effects on fluoroscopic time. A line in the figure represents treatment comparisons, with arrows and tails referring to intervention and comparators, respectively. Bold and dashed lines refer to direct and indirect comparisons, respectively. The number at the line indicates chance of treatment responsiveness, in which <0 indicates favors intervention vs the comparator. *p < 0.05 with Bonferroni correction
Network meta-analysis of treatment effects on blood loss. A line in the figure represents treatment comparisons, with arrows and tails referring to intervention and comparators, respectively. Bold and dashed lines refer to direct and indirect comparisons, respectively. The number at the line indicates chance of treatment responsiveness, in which <0 indicates favors intervention vs the comparator. *p < 0.05 with Bonferroni correction
Network meta-analysis of treatment effects on unit transfusion. A line in the figure represents treatment comparisons, with arrows and tails referring to intervention and comparators, respectively. Bold and dashed lines refer to direct and indirect comparisons, respectively. The number at the line indicates chance of treatment responsiveness, in which <0 indicates favors intervention vs the comparator. *p < 0.05 with Bonferroni correction
Network meta-analysis of treatment effects on hospital stay. A line in the figure represents treatment comparisons, with arrows and tails referring to intervention and comparators, respectively. Bold and dashed lines refer to direct and indirect comparisons, respectively. The number at the line indicates chance of treatment responsiveness, in which <0 indicates favors intervention vs the comparator. *p < 0.05 with Bonferroni correction
Although all studies were RCTs, 58.3% of the studies were unclear in the randomization sequence generations and allocation concealment; hence, selection bias or confounding factors may be present. Some pooled results were heterogeneous, but we were unable to explore the source of heterogeneity due to limitations of the reported data.
In conclusion, the network meta-analysis suggested that the fixation with PCCP has significantly shorten the operative time and unit transfusion with lower the risk of general complication, wound complication and late complication when compared to others, whereas PFN was the lowest in blood loss and hospital stay. Multiple active treatment comparisons indicated that PCCP fixation in elderly trochanteric fractures was the best treatment choices in terms of intra-operative outcomes and postoperative complication. But many countries have concern about hospital stay due to the high cost of hospitalization than PFN should be used.
Abbreviations
- RCTs:
-
Randomized controlled trials
- DHS:
-
Dynamic hip screws
- PCCP:
-
Percutaneous compression plating
- PFN:
-
Proximal femoral nails
- LISS:
-
Less invasive stabilization system
References
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ (Clin Res ed) 326(7382):219
Bojan AJ, Beimel C, Speitling A, Taglang G, Ekholm C, Jonsson A (2010) 3066 consecutive Gamma nails. 12 years experience at a single centre. BMC Musculoskelet Disorders 11:133. doi:10.1186/1471-2474-11-133
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ (Clin Res ed) 315(7109):629–634
Ekstrom W, Karlsson-Thur C, Larsson S, Ragnarsson B, Alberts KA (2007) Functional outcome in treatment of unstable trochanteric and subtrochanteric fractures with the proximal femoral nail and the Medoff sliding plate. J Orthop Trauma 21(1):18–25. doi:10.1097/BOT.0b013e31802b41cf
Forte ML, Virnig BA, Eberly LE, Swiontkowski MF, Feldman R, Bhandari M, Kane RL (2010) Provider factors associated with intramedullary nail use for intertrochanteric hip fractures. J Bone Joint Surg Am 92(5):1105–1114. doi:10.2106/jbjs.i.00295
Handoll HH, Parker MJ (2008) Conservative versus operative treatment for hip fractures in adults. Cochrane Datab Syst Rev 3:CD000337. doi:10.1002/14651858.CD000337.pub2
Huang X, Leung F, Liu M, Chen L, Xu Z, Xiang Z (2014) Is helical blade superior to screw design in terms of cut-out rate for elderly trochanteric fractures? A meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 24(8):1461–1468. doi:10.1007/s00590-014-1429-9
Huang X, Leung F, Xiang Z, Tan PY, Yang J, Wei DQ, Yu X (2013) Proximal femoral nail versus dynamic hip screw fixation for trochanteric fractures: a meta-analysis of randomized controlled trials. Sci World J 2013:805805. doi:10.1155/2013/805805
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784. doi:10.7326/m14-2385
Kim WY, Han CH, Park JI, Kim JY (2001) Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop 25(6):360–362
Knobe M, Gradl G, Ladenburger A, Tarkin IS, Pape HC (2013) Unstable intertrochanteric femur fractures: is there a consensus on definition and treatment in Germany? Clin Orthop Relat Res 471(9):2831–2840. doi:10.1007/s11999-013-2834-9
Kosygan KP, Mohan R, Newman RJ (2002) The Gotfried percutaneous compression plate compared with the conventional classic hip screw for the fixation of intertrochanteric fractures of the hip. J Bone Joint Surg Br 84(1):19–22
Kristek D, Lovric I, Kristek J, Biljan M, Kristek G, Sakic K (2010) The proximal femoral nail antirotation (PFNA) in the treatment of proximal femoral fractures. Coll Antropol 34(3):937–940
Lu G, Ades AE (2004) Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med 23(20):3105–3124. doi:10.1002/sim.1875
Ma KL, Wang X, Luan FJ, Xu HT, Fang Y, Min J, Luan HX, Yang F, Zheng H, He SJ (2014) Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop Traumatol Surg Res 100(8):859–866. doi:10.1016/j.otsr.2014.07.023
Matre K, Havelin LI, Gjertsen JE, Vinje T, Espehaug B, Fevang JM (2013) Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian Hip Fracture Register. Injury 44(6):735–742. doi:10.1016/j.injury.2012.12.010
Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachie N (2009) The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury 40(4):428–432. doi:10.1016/j.injury.2008.10.014
Palmer TMPJ, Sutton AJ, Moreno SG (2008) Contour-enhanced funnel plots in meta-analysis. STATA J 8(2):242–254
Parker MJ, Handoll HH (2010) Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Datab Syst Rev 9:CD000093. doi:10.1002/14651858.CD000093.pub5
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2008) Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J Clin Epidemiol 61(10):991–996. doi:10.1016/j.jclinepi.2007.11.010
Saarenpaa I, Heikkinen T, Ristiniemi J, Hyvonen P, Leppilahti J, Jalovaara P (2009) Functional comparison of the dynamic hip screw and the Gamma locking nail in trochanteric hip fractures: a matched-pair study of 268 patients. Int Orthop 33(1):255–260. doi:10.1007/s00264-007-0458-y
Shen L, Zhang Y, Shen Y, Cui Z (2013) Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res 99(4):377–383. doi:10.1016/j.otsr.2012.12.019
Song F, Altman DG, Glenny AM, Deeks JJ (2003) Validity of indirect comparison for estimating efficacy of competing interventions: empirical evidence from published meta-analyses. BMJ (Clin Res ed) 326(7387):472. doi:10.1136/bmj.326.7387.472
Song F, Harvey I, Lilford R (2008) Adjusted indirect comparison may be less biased than direct comparison for evaluating new pharmaceutical interventions. J Clin Epidemiol 61(5):455–463. doi:10.1016/j.jclinepi.2007.06.006
StataCorp. (2014) Stata 14 base reference manual. Stata Press, College Station
Tao R, Lu Y, Xu H, Zhou ZY, Wang YH, Liu F (2013) Internal fixation of intertrochanteric hip fractures: a clinical comparison of two implant designs. Sci World J 2013:834825. doi:10.1155/2013/834825
Watson JT, Moed BR, Cramer KE, Karges DE (1998) Comparison of the compression hip screw with the Medoff sliding plate for intertrochanteric fractures. Clin Orthop Relat Res 348:79–86
Yuan X, Yao Q, Ni J, Peng L, Yu D (2014) Proximal femoral nail antirotation versus dynamic hip screw for intertrochanteric fracture in elders: a meta-analysis. Nat Med J China 94(11):836–839. doi:10.3760/cma.j.issn.0376-2491.2014.11.009
Zhang K, Zhang S, Yang J, Dong W, Wang S, Cheng Y, Al-Qwbani M, Wang Q, Yu B (2014) Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: a meta-analysis. Med Sci Monit 20:1628–1633. doi:10.12659/msm.890962
Zhang L, Shen J, Yu S, Huang Q, Xie Z (2014) Percutaneous compression plate versus dynamic hip screw for treatment of intertrochanteric Hip fractures: a meta-analyse of five randomized controlled trials. Sci World J 2014:512512. doi:10.1155/2014/512512
Acknowledgements
All authors declare that no funding source or any sponsor involvement in the study design, collection, analysis and interpretation of the data; in writing of the manuscript; and in the submission to submit the manuscript for publication.
Authors’ contributions
AA was involved in conception and design, analysis and interpretation of the data, drafting of the article, critical revision of the article for important intellectual content, final approval of the article, collection and assembly of data. TA was involved in conception and design, drafting of the article, critical revision of the article for important intellectual content, final approval of the article, collection and assembly of data. PT was involved in conception and design, drafting of the article, critical revision of the article for important intellectual content, final approval of the article. PP was involved in conception and design, drafting of the article, critical revision of the article for important intellectual content, final approval of the article. PS was involved in conception and design, drafting of the article, critical revision of the article for important intellectual content, final approval of the article. JK was involved in conception and design, analysis and interpretation of the data, drafting of the article, critical revision of the article for important intellectual content, final approval of the article, statistical expertise, collection and assembly of data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interests.
Ethical standards
This article does not contain any studies with human participants performed by any of the authors.
Appendix: Search term and search strategy
Appendix: Search term and search strategy
#1 Fracture intertrochanteric
#2 Elder
#3 Fracture femur
#4 Proximal femural nail
#5 Dynamic hip screws
#6 Gamma nail
#7 Proximal femural nail anti rotation
#8 Blood loss
#9 Hospital stay
#10 Failure rate
#11 Femeral shaft fracture
#12 Operative times
#13 Complications
#14 #1 or #2 or #3
#15 #4 or #5 or #6 or #7
#16 #8 or #9 or #10 or #11 or #12 or #13
#17 #14 and #15 and #16.
Rights and permissions
About this article
Cite this article
Arirachakaran, A., Amphansap, T., Thanindratarn, P. et al. Comparative outcome of PFNA, Gamma nails, PCCP, Medoff plate, LISS and dynamic hip screws for fixation in elderly trochanteric fractures: a systematic review and network meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 27, 937–952 (2017). https://doi.org/10.1007/s00590-017-1964-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-017-1964-2