Abstract
This prospective randomized study aims at evaluating the electrophysiological results of endoscopic and open carpal ligament release in patients with carpal tunnel syndrome. Included in the study were 41 patients diagnosed with carpal tunnel syndrome (21 hands in the endoscopic group and 20 hands in the open group). The Boston questionnaire was administered preoperatively and postoperatively to the patients, and their functional capacities and symptom severities were recorded. Physical examination was carried out preoperatively and in the postoperative sixth month. Demographic data and preoperative Boston symptomatic and functional scores were similar between both groups. A significant improvement was obtained in the Boston symptomatic and functional scores of both groups, but no significant difference was found between the groups in terms of improvement in the symptomatic and the functional scores. A significant shortening in median nerve motor distal latency and an increase in the velocity of sensory conductions were determined in both groups in the postoperative electromyography, but no difference was found between them in terms of improvement in the electromyography values. It was shown both clinically and electrophysiologically that endoscopic carpal tunnel surgery was as effective as open surgery as a treatment method for carpal tunnel syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel syndrome (CTS) is a common entrapment neuropathy of the median nerve as it passes through the carpal tunnel [1]. The diagnosis of CTS is often made clinically; however, electrophysiological methods, specifically electromyography (EMG), are the golden standard in diagnosis [2]. Demyelization that develops as the median nerve is squeezed in the canal and is shown objectively by EMG. Staging is carried out by assessing median nerve motor distal latency and sensory conduction velocity [3]. Conservative or surgical methods are applied in the treatment of CTS. Conservative treatments are primarily preferred in Stages 1 and 2 [4]. Surgical methods are used on Stage 1 and Stage 2 patients who do not benefit from physical treatment and on patients after Stage 3 [5]. In surgical treatment, the aim is to incise the transverse carpal ligament to broaden the canal and lower the pressure in the canal. Various methods are used in surgical treatment. Open release has been administered as the standard procedure for many years [6]. Despite the accumulation of knowledge and experience on open release, cosmetic concerns regarding scar and pain around the incision have led to the search for new techniques. Thanks to endoscopic methods that have been developed, surgical incision has been downsized and taken away from that part of the hand which receives pressure [7]. Furthermore, endoscopic surgery is advantageous in terms of the time period of pain and before going back to work [8–11]. However, results were reported regarding the complication rates of these methods [10–19] (Table 1).
We believe there is similar effectiveness between endoscopic and open release in the treatment of carpal tunnel syndrome, but endoscopic release has some advantages for patients after surgery such as early return to work, patient satisfaction and low scar pain. The aim of this prospective and randomized study was to compare clinically and electrophysiologically the effectiveness of endoscopic release surgery versus open surgery in the treatment of carpal tunnel syndrome.
Patients and methods
Approval of the hospital ethics committee was obtained for this study. Patients who applied to our polyclinic between the years 2009 and 2010 and who were considered to have carpal tunnel syndrome were subjected to EMG examination by the standard protocol to confirm their carpal tunnel syndrome diagnosis. The patients who were diagnosed with CTS were informed about the treatment of their disease. Those who supplied their written acceptance were included in the study. Conservative treatment was primarily applied on the Stage 1 and Stage 2 patients. Surgical treatment was administered to those patients in whom the conservative treatment was ineffective.
Those patients who had motor deficit, cervical disk pathology, metabolic disease that can cause peripheral neuropathy, history of upper extremity injury and surgery, and limitation of movement in the wrist were excluded.
Fifty patients who supplied their acceptance to participate were divided into two groups by a simple, random sampling (heads or tails), and 22 of them were treated with endoscopic surgery and 28 with open carpal tunnel release surgery. However, only 41 patients (21 in the endoscopic surgery group and 20 in the open surgery group) completed the study assessment period.
For the open surgery, the technique with single incision as described by Taleisnik [6] was used. For the endoscopic surgery, the technique with two incisions as described by Chow [20] was used (Ectra 2, Smith & Nephew) (Figs. 1, 2). Both of the surgical methods were applied by a single surgeon under standard intravenous regional anesthesia. In both groups, bleeding was controlled by tight compressive bandage after the operation. The bandage was loosened at the postoperative thirtieth minute. All of the patients were discharged within the first 24 h postoperatively. The discharged patients were followed up by weekly checks in terms of their carpal tunnel complaints and wound healing.
All of the patients were evaluated at the beginning of the study (baseline) and postoperatively at 6 months by a reviewer (S.A.G.) who was blinded to the study, using the Boston scale.
Two subscales of the Boston scale were used for the evaluation of CTS: the symptom severity and functional status scales. Each item was rated by the patient from 1 to 5 points (5 = most severe), and higher scores indicated more pain and disability. Scores for each scale were calculated independently and were not combined. The score was calculated as the unweighted mean of all answered items for the scale (range 1–5).
Grip strength difference is a very important factor to evaluate the treatment effect after carpal tunnel release, but we could not perform the grip strength test because there was not an hydraulic hand dynamometer in our clinic [21, 22]. This is a limitation of our study.
Electrophysiological assessment was performed by the same neurologist (B.E.) in the neurology clinic of our hospital at the beginning of the study (baseline) and postoperatively at 6 months. While patients were laid in the supine position, the elbow was kept in extension, the forearm in supination and the wrist in the neutral position. Sensory and motor conduction of the median nerve in the symptomatic hand were tested. Median nerve motor distal latency (MDL), compound muscle action potential (CMAP), sensory conduction velocity (SCV) and sensory nerve action potential (SNAP) were examined, and staging was carried out. The EMG assessments were carried out in accordance with the CTS diagnosis criteria as determined by the American Association of Electrodiagnostic Medicine as follows: Stage 1, slight CTS (slowing SCV [<50 m/s]); Stage 2, average CTS (slowing SCV [<50 m/s] and extending MDL [>4.5 ms]); and Stage 3, severe CTS (no DSAP) [3].
In our study, there was no difference according to potentially confounding variables such as age, sex, complaint period, affected hand and Boston scores between the groups of patients at baseline. But, there are only differences between CMAP values the groups of the patients at baseline, 5.12 ± 2.21 for endoscopic and 7.35 ± 2.39 for open release.
Statistical analysis
The SPSS software (version 15.0; SPSS Inc, Chicago, USA) was used to analyze the data. All data were compared using a 95 % confidence interval. Parametric data are presented as mean ± SD. Intra-group comparisons were performed using paired sample t tests, and the Wilcox test was used when the numeric variable was not normally distributed. In inter-group comparisons, nonparametric data and categorical variables, such as sex and operated hand, were compared using the Chi-square test, and the sample t test was used when the numeric variables, such as age and EMG, were normally distributed. Statistical analysis of the measurement data was carried out by the independent samples t test, and Mann–Whitney U test was used when the numeric variables were not normally distributed.
Results
There was no difference between the endoscopic and open surgery group at the beginning of the study. Demographic data are presented in Table 2.
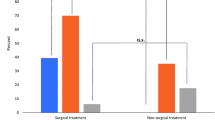
The mean baseline symptom severity and functional capacity scores of the endoscopic and open surgery groups were not significantly different. However, the mean symptom severity and functional capacity scores of both groups improved significantly at 6 months after treatment versus the baseline scores. The night complaints of all the patients decreased in the early period after the treatment. In inter-group comparisons, the mean symptom severity and functional capacity scores in the groups were not significantly different at 6 months. When the preoperative EMG values were compared, no difference was found between the two groups in terms of MDL, SCV and CTS stage. Significant shortening in MDL, increase in SCV and decline in CTS stage were observed in both groups in the postoperative EMG. All results in the preoperative and postoperative term are summarized in Table 3.
One patient in the open surgery group developed superficial infection. There were signs of a superficial infection such as swelling, fever, redness and severe pain. He did not have leucocytosis, but he had mild neutrophilia. We could not make a culture, because there was no discharge from the injury area or abscess formation. This patient was treated with 375 mg ampicillin–sulbactam, orally, twice daily for a week. In the examination that was carried out in the postoperative sixth week, scar pain was determined in three patients in the open surgery group. Fifth finger flexor digitorum superficialis injury occurred in one patient in the endoscopic surgery group. The injury was noticed perioperatively. The incision was extended, and the tendon primer was repaired. Therefore, this study subject began as endoscopic surgery, but ended as open surgery. Therefore, in order not to confuse study results these cases were excluded. Due to residual pain and numbing in a patient who was administered endoscopic surgery, open release was performed in the postoperative third month after endoscopic surgery. The complication rate in the ECTR group was detected as 15.52 % (2/19), while the complication rate in the OCTR group was detected as 5.26 % (1/19) (p = 0.52).
We have not performed a cost–benefit analysis, which is a limitation of our study. However, we believe that when all costs, including loss of productivity and cost of rehabilitation are included, ECTR is more advantageous than OCTR. Further studies are needed for cost–benefit analysis.
The mean Boston scores and EMG values for the ECTR and OCTR groups did not differ significantly when comparing one group to the other at the baseline assessment or at the 6-month evaluation. The complication rate after surgery for the ECTR group was more than the OCTR group, but there was no statistically significant difference.
Discussion
Carpal tunnel syndrome (CTS) is the most common entrapment neuropathy of the upper limb, and various surgical methods have been used in its treatment [1, 6, 23]. Although good results are obtained by the standard open surgical treatment, some complications, which are difficult to treat, such as scar pain, hypothenar or thenar pain are frequently observed [24]. To avoid such complications, a mini-transverse wrist incision technique is increasingly performed and patient satisfaction, the mean duration of operation and the mean length of scar are all better than the standard approach. However, this technique does not allow the surgeon to fully visualize all important structures [25]. Therefore, the endoscopic surgery technique has been developed for protecting all important structures during the transverse ligament release [20]. In this study, we have compared clinically and electrophysiologically the effectiveness of the endoscopic release surgery versus open surgery in treatment of carpal tunnel syndrome. The mean Boston scores and EMG values for the ECTR and OCTR groups did not differ significantly when comparing one group to the other at the baseline assessment or at the 6-month evaluation. The complication rate for the ECTR group was higher than the OCTR group after surgery, but there was no statistically significant difference.
Many studies that have compared the effectiveness of open and endoscopic surgeries found that endoscopic surgery was as effective as open surgery in diminishing postoperative symptoms [13, 15, 25, 26]. Endoscopic surgery has some advantages like fast healing, low postoperative pain and morbidity, minimal scar formation and high patient satisfaction [7, 25, 27]. On the other hand, it has some disadvantages like a longer learning curve, tendon and nerve injury, incomplete release and excessive financial burden [8, 26, 28–30]. Cost-effectiveness is very important to choosing the surgical procedure. Particularly, the high cost of endoscopic carpal tunnel surgery, due to specific instrumentation, is a cause of concern [15, 16]. Despite an increase in medical costs for endoscopic carpal tunnel release, the procedure has a potential to decrease overall costs (need for rehabilitation, scar treatment, late return to job) by lowering losses in productivity and wage reimbursement [8, 15, 16]. Saw et al. [16] reported that ECTR has the advantage of a quicker return to work for employed people, and ECTR provides an economic benefit of £438 over OCTR for each employed person. We also believe that when all costs, including loss of productivity and cost of rehabilitation are included, ECTR is more advantageous than OCTR, although further studies are needed for a cost–benefit analysis.
Many studies reported that no difference exists between open and endoscopic release in terms of symptomatic improvement [15, 27] (Table 4). Michelotti et al. [17] reported that no difference was found between the open and the endoscopic surgery groups who had bilateral release surgeries, according to functional results and symptom severity, but patient satisfaction was significantly higher in the endoscopic surgery group. Sayegh et al. [31] could not find a long-term difference between the open and endoscopic surgery groups in their meta-analysis, but they reported that return to professional life and activities were better in endoscopic surgery groups. In their meta-analysis, Vasiliadis et al. [32] reported that endoscopic surgery was more useful in improving grasping strength, although open and endoscopic surgery had similar effectiveness in relieving symptoms and improving functional status. They also stated that there was no difference between the rates of major complications, although minor complications were seen less in endoscopic surgery. Similar to the literature, our study determined a significant decrease in the Boston scores of symptom severity and functional capacity.
In a study in which they evaluated the result of endoscopic carpal tunnel release, Chow et al. [9] found a 95 % success rate, 0.5 % recurrence and no serious complications. Mavrogenis et al. [33] evaluated 31 patients who were re-operated on due to complications after carpal tunnel release and reported that the most common complications were median and ulnar nerve lacerations at the wrist and thenar regions (8 patients), neuroma, (8 patients), wound infection (2 patients), and painful hypertrophic scar (2 patients). Additionally, they reported incomplete release which caused recurrent symptoms in eight patients. Although this study design cannot give a comparison between open and endoscopic surgeries, the authors reported that major nerve injuries occurred after open surgery, and in their clinical practice, the complication rate was much higher with open surgery than endoscopic or mini-incision techniques. In our study, fifth finger flexor digitorum superficialis injury occurred in one patient in the endoscopic surgery group. The injury was noticed perioperatively. The incision was extended, and the tendon primer was repaired. In addition, due to residual pain and numbing in one patient who was administered endoscopic surgery, open release was performed in the postoperative third month. In our study, the complication rate in the ECTR group was determined as 15.52 % (2/9), while the complication rate in the OCTR group was determined as 5.26 % (1/19). We believe that some complications may be seen during the early periods of ECTR due to the endoscopic surgery learning curve. Although the success rate (90 %) is compatible with the literature, the high rate of recurrence (4.5 %) might be due to the low number in our sample. We believe that most complications of carpal tunnel surgery can be prevented by specialized training of the operating surgeon in hand surgery and proper operative technique, including a properly placed incision and exposure under magnification and direct vision [33].
Clinical measurements were frequently used in those studies which showed that endoscopic surgery was more helpful than open surgery [13, 15, 25]. EMG, which is an objective tool of assessment, has been used only in a few studies for postoperative assessment [10, 26, 30]. The criterion for the diagnosis of CTS was a MDL of more than 4.3 ms or an SCV of <45 m/s. Surgery was indicated if the MDL was 5.5 ms or more, or if the SCV was <40 m/s. In our study, all patients were abnormal in both MDL and SCV in the electromyographic evaluation [34]. Senda et al. [34] reported that the difference between preoperative and final follow-up MDL values (7.2 ± 2.2 and 4.3 ± 0.6 ms, respectively) and SCV values (27.3 ± 8.8 and 40.8 ± 6.7 m/s, respectively) was significant. Similarly, significant improvement was observed in both MDL and SCV values in our study.
Itsubo et al. [35] reported that significant improvement was observed in the patient-oriented questionnaires, and the MDL and neurophysiological stage of the disease, but nerve conduction studies and patient-oriented questionnaires were not parallel. Ejiri et al. [26] reported that there was no significant difference between the open and the endoscopic surgery groups in terms of postoperative short-term electrophysiological results. In another study, Uchiyama et al. [30] showed the same level of improvement in both groups in the electrophysiological assessment carried out in the postoperative 12 month. Malhotra et al. [10] reported that the distal latency (motor and sensory) of the median nerve decreased, and nerve conduction velocity increased in both groups at the first month after treatment. They stated that, at the end of a 6-month follow-up, the distal latency decreased from 4.7 to 3.7 m/s in the endoscopic surgery group and from 4.8 to 4.0 m/s in the open surgery group, while the conduction velocity increased from 40 to 50 m/s in the endoscopic group and from 40 to 48 m/s in the open surgery group. They stated, however, that no significant difference existed between these surgical groups. In our study, EMG was performed, in addition to clinical measurements, for the patients in the postoperative sixth month. When compared to the preoperative EMG, significant shortening in MDL, increase in SCV and decrease in CTS were observed in the postoperative EMG in both groups. When the rates of recovery in the two groups were compared, no significant difference was found between them. This result shows that endoscopic surgery is as effective as open surgery.
As a consequence, incomplete release and nerve and tendon injuries may be seen during the early periods of ECTR due to an endoscopic surgery learning curve and problems with appropriate surgical methods, including site of insertion and exposure. Although a few complications occurred in the first cases, we showed both clinically and also electrophysiologically that endoscopic carpal tunnel surgery is as effective as open surgery as a treatment method for CTS.
References
Alfonso C, JannS Massa R, Torreggiani A (2010) Diagnosis, treatment and follow-up of the carpal tunnel syndrome: a review. Neurol Sci 31:243–252
Werner RA, Andary M (2002) Carpal tunnel syndrome: pathophysiology and clinical neurophysiology. ClinNeuro physiol 113:1373–1381
Stevens JC (1997) AAEM minimonograph #26: the electro diagnosis of carpal tunnel syndrome. American association of electro diagnostic medicine. Muscle Nerve 20:1477–1486
Prime MS, Palmer J, Khan WS, Goddard NJ (2010) Is there light at the end of the tunnel? Controversies in the diagnosis and management of carpal tunnel syndrome. Hand 5:354–360
Duncan KH, Lewis RC Jr, Foreman KA, Nordyke MD (1987) Treatment of carpal tunnel syndrome by members of the American Society for Surgery of the Hand: results of a questionnaire. J Hand Surg Am 12:384–391
Taleisnik J (1973) The palmar cutaneous branch of the median nerve and the approach to the carpal tunnel. An anatomical study. J Bone Joint Surg [Am] 55:1212–1217
Agee JM, McCarroll HR Jr, Tortosa RD, Berry DA, Szabo RM, Peimer CA (1992) Endoscopic release of the carpal tunnel: a randomized prospective multicenter study. J Hand Surg Am 17:987–995
Palmer DH, Paulson JC, Lane-Larsen CL, Peulen VK, Olson JD (1993) Endoscopic carpal tunnel release: a comparison of two techniques with open release. Arthroscopy 9(5):498–508
Chow JC, Hantes ME (2002) Endoscopic carpal tunnel release: thirteen years’ experience with the Chow technique. J Hand Surg Am 27(6):1011–1018
Malhotra R, Kiran EK, Dua A, Mallinath SG, Bhan S (2007) Endoscopic versus open carpal tunnel release: a short-term comparative study. Indian J Orthop 41:57–61
Vasiliadis HS, Xenakis TA, Mitsionis G, Paschos N, Georgoulis A (2010) Endoscopic versus open carpal tunnel release. Arthroscopy 26(1):26–33
Jerosch-Herold C, Leite JC, Song F (2006) A systematic review of outcomes assessed in randomized controlled trials of surgical interventions for carpal tunnel syndrome using the International Classification of Functioning, Disability and Health (ICF) as a reference tool. BMC Musculoskelet Disord 5(7):96
Hasegawa K, Hashizume H, Senda M, Kawai A, Inoue H (1999) Evaluation of release surgery for idiopathic carpal tunnel syndrome: endoscopic versus open method. Acta Med Okayama 53(4):179–183
Faraj AA, Ahmed MH, Saeed OM (2012) A comparative study of the surgical management of carpal tunnel syndrome by mini-transverse wrist incisions versus traditional longitudinal technique. Eur J Orthop Surg Traumatol 22:221–225
Ferdinand RD, MacLean JG (2002) Endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome. A prospective, randomised, blinded assessment. J Bone Joint Surg Br 84(3):375–379
Saw NL, Jones S, Shepstone L, Meyer M, Chapman PG, Logan AM (2003) Early outcome and cost-effectiveness of endoscopic versus open carpal tunnel release: a randomized prospective trial. J Hand Surg Br 28(5):444–449
Michelotti B, Romanowsky D, Hauck RM (2014) Prospective, randomized evaluation of endoscopic versus open carpal tunnel release in bilateral carpal tunnel syndrome: an interim analysis. Ann Plast Surg 73(2):157–160
Heidarian A, Abbasi H, Hasanzadeh HM, Hajialibeyg A, Kalantar MSM, Seifirad S (2013) Comparison of knifelight surgery versus conventional open surgery in the treatment of carpal tunnel syndrome. Iran Red Crescent Med J 15(5):385–388
Kang HJ, Koh IH, Lee TJ, Choi YR (2013) Endoscopic carpal tunnel release is preferred over mini-open despite similar outcome: a randomized trial. Clin Orthop Relat Res 471(5):1548–1554
Chow JC (1993) The Chow technique of endoscopic release of the carpal ligament for carpal tunnel syndrome: four years of clinical results. Arthroscopy 9:301–314
Levine DW, Simmons BP, Koris MJ, Kawai A, Inoue H (1993) A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am 75(11):1585–1592
Katz JN, Punnett L, Simmons BP, Fossel AH, Mooney N, Keller RB (1996) Workers’ compensation recipients with carpal tunnel syndrome: the validity of self-reported health measures. Am J Public Health 86(1):52–56
Lewis C, Mauffrey C, Newman S, Lambert A, Hull P (2010) Current concepts in carpal tunnel syndrome: a review of the literature. Eur J Orthop Surg Traumatol 20:445–452
Louis DS, Greene TL, Noellert RC (1985) Complications of carpal tunnel surgery. J Neurosurg 62:352
Wong KC, Hung LK, Ho PC, Wong JM (2003) Carpal tunnel release. A prospective, randomised study of endoscopic versus limited-open methods. J Bone Joint Surg Br 85(6):863–868
Ejiri S, Kikuchi S, Maruya M, Sekiguchi Y, Kawakami R, Konno S (2012) Short-term results of endoscopic (Okutsu method) versus palmar incision open carpal tunnel release: a prospective randomized controlled trial. Fukushima J Med Sci 58(1):49–59
Moharram AN, Kaptan WT, Hegazi MM, Kamal TT (2007) Carpal tunnel decompression: a randomised controlled trail of endoscopic versus open release. Pan Arab J Orth Trauma 11(1):96–101
Brown RA, Gelberman RH, Seiler JG et al (1993) Carpal tunnel release: a prospective randomized assessment of open and endoscopic methods. J Bone Joint Surg Am 75(9):1265–1275
Murphy RX Jr, Jennings JF, Wukich DK (1994) Major neurovascular complications of endoscopic carpal tunnel release. J Hand Surg Am 19(1):114–118
Uchiyama S, Toriumi H, Nakagawa H, Kamimura M, Ishigaki N, Miyasaka T (2002) Postoperative nerve conduction changes after open and endoscopic carpal tunnel release. Clin Neurophysiol 113(1):64–70
Sayegh ET, Strauch RJ (2015) Open versus endoscopic carpal tunnel release: a meta-analysis of randomized controlled trials. Clin Orthop Relat Res 473(3):1120–1132
Vasiliadis HS, Georgoulas P, Shrier I, Salanti G, Scholten RJ (2014) Endoscopic release for carpal tunnel syndrome. Cochrane Database Syst Rev 31;1: CD008265
Mavrogenis AF, Papagelopoulos PJ, Ignatiadis IA, Spyridonos SG, Efstathopoulos DG (2009) Complications of open carpal tunnel surgery: avoiding the pitfalls. Eur J Orthop Surg Traumatol 19(1):11–17
Senda M, Hashizume H, Terai Y, Inoue H, Nagashima H (1999) Electromyographic evaluation after endoscopic carpal tunnel release in idiopathic carpal tunnel syndrome. J Orthop Sci 4(3):187–190
Itsubo T, Uchiyama S, Momose T, Yasutomi T, Imaeda T, Kato H (2009) Electrophysiological responsiveness and quality of life (Quick DASH, CTSI) evaluation of surgically treated carpal tunnel syndrome. J Orthop Sci 14(1):17–23
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no conflict of interests exists in the preparation and publication of this paper.
Rights and permissions
About this article
Cite this article
Gümüştaş, S.A., Ekmekçi, B., Tosun, H.B. et al. Similar effectiveness of the open versus endoscopic technique for carpal tunnel syndrome: a prospective randomized trial. Eur J Orthop Surg Traumatol 25, 1253–1260 (2015). https://doi.org/10.1007/s00590-015-1696-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-015-1696-0