Abstract
Background
Proximal junctional kyphosis (PJK) is a common complication following corrective surgery for adolescent idiopathic scoliosis (AIS) with a Lenke 5 curve. Previous studies have suggested that PJK may be associated with osteopenia, which is prevalent in AIS patients. MRI-based vertebral bone quality (VBQ) scores have been proposed as a valuable tool to assess preoperative bone quality. However, accurately measuring VBQ scores in Lenke 5 AIS patients with a structural lumbar curve can be challenging. Recently, a simplified S1 VBQ score has been proposed as an alternative method when the traditional VBQ score is not applicable. This study aims to evaluate the predictive value of the simplified S1 VBQ score in predicting the occurrence of PJK after corrective surgery for Lenke 5 AIS.
Methods
We conducted a retrospective analysis of patient data to assess the predictive utility of the S1 VBQ score for PJK in Lenke 5 AIS patients. Demographic, radiographic, and surgical data were collected, and S1 VBQ scores were calculated based on preoperative T1-weighted MRI images. Univariate analysis, linear regression, and multivariate logistic regression were performed to identify potential risk factors for PJK and to assess the correlation between other variables and the S1 VBQ score. Receiver operating characteristic analysis and area under the curve values were used to evaluate the predictive efficiency of the S1 VBQ score for PJK.
Results
A total of 105 patients (aged 15.50 ± 2.36 years) were included in the analysis, of whom 24 (22.9%) developed PJK. S1 VBQ scores were significantly higher in the PJK group compared to the non-PJK group (2.83 ± 0.44 vs. 2.48 ± 0.30, P < 0.001), and there was a significant positive correlation between the S1 VBQ score and proximal junctional angle (PJA) (r = 0.46, P < 0.0001). Multivariate analysis revealed that the S1 VBQ scores and preoperative thoracic kyphosis (TK) were significant predictors of PJK.
Conclusion
This study provided evidence that higher S1 VBQ scores were independently associated with PJK occurrence following corrective surgery for Lenke 5 AIS. Preoperative measurement of the S1 VBQ score on MRI may serve as a valuable tool in planning surgical correction for Lenke 5 AIS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescent idiopathic scoliosis (AIS) is a complex deformity that involves axial rotation of the vertebral body, lateral curvature of the spine on the coronal plane, and abnormal sagittal alignment [1]. Proximal junctional kyphosis (PJK), which is defined as a postoperative proximal junctional angle (PJA) greater than 10°, is among the most common postoperative complications encountered in Lenke 5 AIS patients [2].
Although the etiology of proximal PJK remained poorly understood, several studies have suggested that osteopenia/osteoporosis may be an important risk factor after spinal correction surgery [3,4,5,6]. It has been reported that a significant proportion of AIS patients have lower bone mineral density (BMD) compared to the general population [7,8,9,10]. Although dual-energy X-ray absorptiometry (DEXA) is considered the gold standard for detecting BMD, it is not routinely used as a preoperative examination for adolescent idiopathic scoliosis (AIS) patients. Instead, Ehresman et al. proposed a novel MRI-based vertebral bone quality (VBQ) score, which has been validated as a useful tool for evaluating bone mineral density [11]. The VBQ score involves calculating the signal intensity (SI) values of the L1–L4 vertebral bodies and normalizing them by dividing by the mean SI value of the cerebrospinal fluid (CSF) at L3 from the midsagittal plane of a lumbar spinal non-contrast-enhanced T1-weighted MRI.
However, obtaining midsagittal plane L1–L4 vertebral body SI values in Lenke 5 AIS patients can be challenging due to the lateral curvature of the lumbar spine. Recently, a novel simplified S1 VBQ score has been verified as a promising alternative method to assess bone mineral density (BMD) for patients with lumbar degenerative diseases [12]. This method can be utilized when L1–L4 SI values are not available, such as trauma, infection, or deformity in related regions. In this study, we firstly evaluated the efficacy of the simplified S1 VBQ score in predicting the incidence of PJK in Lenke 5 AIS patients.
Methods
Patient selection
A retrospective study was conducted to investigate the relationship between proximal junctional kyphosis (PJK) after Lenke 5 adolescent idiopathic scoliosis (AIS) surgery and vertebral body quality (VBQ) scores. We included Lenke 5 AIS patients who underwent posterior fusion surgery at our department of West China Hospital between January 2010 and May 2020. The inclusion criteria were: (1) patient age ranging from 11 to 18 years at the time of the surgical intervention; (2) possession of a preoperative T1-weighted non-contrast-enhanced MRI scan without any prior lumbar instrumentation; (3) possession of both immediate postoperative and the most recent follow-up full-length lateral radiographs; and (4) a minimum radiographic follow-up of 24 months. Patients who had surgical intervention for conditions, such as malignancies, infections, trauma, or those diagnosed with chronic liver disease, renal failure, and metabolic bone disease other than osteopenia or osteoporosis, were excluded from the study. All procedures and methods were approved by the research ethics committee of West China Hospital, and informed consent was obtained from all participants. All protocols were conducted in accordance with the research principles set forth in the Declaration of Helsinki.
Surgical procedure
All surgeries in this study were performed by two senior surgeons from the same surgical team. Prior to fusion, a Smith-Petersen osteotomy was conducted. polyaxial screws were placed at the upper and lower instrumented vertebrae (UIV and LIV), while monoaxial screws were employed at other levels. To correct scoliosis and lumbar spine rotation, intraoperative techniques such as rod rotation, apical vertebral derotation via direct vertebral rotation, convex compression, and concave distraction were implemented.
Radiographic assessment
All patients in this study underwent standing full-length posteroanterior plain radiography. Radiographic measurements of various parameters were obtained before surgery, 3 days post-surgery, and at the final follow-up. The parameters included the main Cobb angle, lumbar Cobb angle, reduced bending angle, correction rate of the two curves, pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), lumbar lordosis (LL), PI–LL, thoracic kyphosis (TK), proximal junctional angle (PJA), and sagittal vertical axis (SVA). Risser sign, an indicator of skeletal maturity, was also assessed.
VBQ score calculation
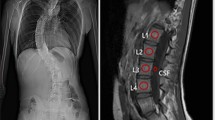
As described in previous literature [12], the VBQ score was determined using SI measurements taken from the midsagittal plane of non-contrast-enhanced T1-weighted magnetic resonance imaging (MRI) of the spine. The SI of the S1 vertebra was measured by placing a region of interest (ROI) on the S1 vertebra on the midsagittal slice, while the SI of CSF at the L3 level is also recorded in Fig. 1. The S1 VBQ score was then calculated in a similar manner to the L1–4 VBQ score:
A: a typical standing full-length posteroanterior plain radiography of Lenke 5 AIS, which clearly showed that the structural lumbar curve makes it extremely difficult to measure the VBQ score in the same plane. B: The signal intensity of regions of interest (circles) used for computing S1 vertebral bone quality (VBQ) score on sagittal non-contrast-enhanced T1-weighted MRI
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics Version 23.0 (IBM Analytics, New York, USA), and figures were generated using GraphPad Prism version 9.3.0 (GraphPad Software, San Diego, California USA). Continuous variables were presented as mean ± standard deviation (SD), and intergroup differences were evaluated by Student's t test for statistical significance. All data normality was tested by Kolmogorov–Smirnov test. All relevant clinical risk factors were subsequently included in a multivariate logistic regression model. Cutoff values were determined by the Youden index via receiver operating characteristic (ROC) curve analysis, and the area under the curve (AUC) of significant continuous variables was calculated. The correlation between PJA and VBQ score was evaluated by univariate linear regression. Model residuals had a normal distribution and showed no heteroscedasticity. P < 0.05 was considered statistically significant.
Results
General characteristics of study population
A total of 105 patients, including 83 females and 22 males, were included in this study, with a mean age of 15.50 ± 2.36 years. The mean Risser sign in the PJK and non-PJK groups was 2.96 ± 1.94 and 3.48 ± 1.64, respectively. The average follow-up period was 42.58 ± 12.45 months and 42.49 ± 11.17 months for the non-PJK and PJK groups. Preoperative general characteristics did not differ significantly between the non-PJK and PJK groups (Table 1). During the follow-up period, two patients with PJK underwent revision surgery due to low back pain, as well as loosening of internal fixation.
Predictors of PJK/PJF
Upon univariate analysis, the following factors were identified as significant risk factors for proximal junctional kyphosis (PJK) when comparing patients with and without PJK: VBQ score (2.83 ± 0.44 vs. 2.48 ± 0.30, P < 0.01), TK (preoperative: 27.06 ± 11.12 vs. 19.14 ± 7.58, P < 0.01; postoperative: 26.12 ± 5.87 vs. 20.50 ± 4.81, P < 0.01), and postoperative LL (54.49 ± 8.91 vs. 50.55 ± 8.84, P = 0.05), as presented in Table 2. Notably, a statistically significant positive correlation between VBQ score and posterior junctional angle (PJA) was observed (r = 0.46, P < 0.01; Fig. 2). Multivariate logistic regression analysis revealed that VBQ score and preoperative TK were independent predictor associated with PJK, with an odds ratio of 26.49 and 1.118, respectively (Table 3, Fig. 3).
Predictive efficiency and inter-association of VBQ score
To assess the accuracy of VBQ scores in predicting PJK, a receiver operating characteristic (ROC) curve was generated with a diagnostic accuracy of 75.0% (95% CI = 61.83–88.17%; Fig. 4). The Youden index identified an optimal cutoff value for the VBQ score at 2.715, which demonstrated a sensitivity of 66.67% and a specificity of 85.19%. Additional univariate linear regression analyses were conducted to investigate potential associations between patient-related general characteristics and the VBQ score. However, the results showed no significant correlation between patient general characteristics and VBQ scores (Table 4).
Discussion
Since the introduction of vertebral bone quality (VBQ) score as a promising tool for assessing bone mineral density (BMD), numerous studies have demonstrated its utility in evaluating complications of spinal surgery, such as screw loosening and cage subsidence after lumbar fusion [13, 14]. Unlike traditional bone quality assessment methods including dual-energy X-ray absorptiometry (DEXA) and computed tomography (CT), which involves radiation exposure, VBQ score was readily available via MRI and was thus more acceptable to patients. PJK, as one of the most common postoperative complications of AIS, has been shown to be closely associated with osteopenia [3]. However, before the introduction of VBQ score, we rarely performed bone quality assessment in AIS patients before surgery, VBQ score makes up for insufficient preoperative understanding of bone quality in AIS patients. Nevertheless, due to the structural lumbar curve in Lenke 5 AIS, it was difficult to accurately measure the VBQ score using traditional measurement methods. Recently, the S1 VBQ score was demonstrated to be a promising tool for identifying poor bone quality in patients with lumbar degenerative diseases, particularly when the L1–L4 VBQ method was unavailable. The study demonstrated that the S1 VBQ scoring exhibited good homogeneity when compared with traditional bone density evaluation methods, such as DEXA and quantitative computed tomography (QCT) [12]. Building on this finding, we initially confirmed that the newly reported S1 VBQ score exhibited good predictive efficacy for the incidence of PJK following Lenke 5 AIS surgery.
In our study, the preoperative and postoperative TK, postoperative LL and S1 VBQ scores were significantly larger in PJK group compared with non-PJK group. According to previous literature, PJK might be a compensatory mechanism due to a change in spinal balance, and the patients with higher TK were reported to have a greater risk of PJK [15], which was consistent with our findings. In addition, the cause of PJK may also be overcorrection of LL [16]. Hence, larger postoperative LL could lead to PJK after surgery. In multivariate logistic regression analysis, the S1 VBQ scores and preoperative TK became the significant predictors for PJK occurrence, indicating that after excluding the interference of other factors, S1 VBQ score was still a relatively sensitive parameter to evaluate the risk of PJK.
As a novel approach to assessing bone quality, the VBQ scoring system offered the advantage of being radiation-free due to its reliance on MRI examinations. This may potentially expand our understanding of preoperative bone quality in patients for whom traditional radiation-based bone density assessments were not recommended. Moreover, the accuracy of traditional DEXA measurements has been questioned for certain degenerative diseases due to the presence of osteophyte proliferation [17, 18]. To date, numerous studies have reported the application of VBQ scoring in predicting cage subsidence, vertebral fragility fractures, and screw loosening [13, 19, 20]. However, as mentioned previously, the conventional lumbar VBQ scoring may be limited in its application for specific conditions, as it requires capturing MRI signal intensity from L1–L4. Since MRI can also obtain images from different planes, future MRI-based VBQ scores, like the S1 VBQ score, may be developed to target individual vertebrae or other specific levels. This would enable us to assess preoperative bone quality in patients from a broader range of perspectives. In conclusion, this study demonstrated that in Lenke 5 AIS patients with preoperative S1 VBQ scores exceeding 2.715, it may be necessary to exercise greater caution in surgical planning to achieve improved prognoses for spine surgeons.
The study also had some limitations. Firstly, it is a single-center, retrospective investigation with a relatively limited sample size. In addition, the absence of a preoperative DEXA scan for patients with AIS prevents a meaningful comparison of VBQ score. Moreover, laboratory values including calcium, phosphorus, glomerular filtration rates, bone-specific alkaline phosphatase, parathyroid hormone, and vitamin D levels were not considered in the analyses, thereby warranting further investigation.
Conclusion
This was the first study assessing the prognostic utility of the novel simplified S1 VBQ score for predicting the occurrence of PJK after Lenke 5 AIS correction surgery. The S1 VBQ score demonstrated a diagnostic precision of 75% in PJK risk prediction. Hence, S1 VBQ score evaluation may be an effective alternative way when classic VBQ score was difficult to measure and held promise in advancing bone quality assessment and PJK prediction among Lenke 5 AIS patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kuznia AL, Hernandez AK, Lee LU (2020) Adolescent idiopathic scoliosis: common questions and answers. Am Fam Physician 101(1):19–23
Zhao J, Yang M, Yang Y, Chen Z, Li M (2018) Proximal junctional kyphosis following correction surgery in the Lenke 5 adolescent idiopathic scoliosis patient. J orthop sci off j Jpn Orthop Assoc 23(5):744–749
Kim JS, Phan K, Cheung ZB, Lee N, Vargas L, Arvind V et al (2019) Surgical, radiographic, and patient-related risk factors for proximal junctional kyphosis: a meta-analysis. Glob spine j 9(1):32–40
Elarjani T, Basil GW, Kader MZ, Pinilla Escobar V, Urakov T, Wang MY et al (2021) A single institution experience with proximal junctional kyphosis in the context of existing classification schemes—systematic review. J clin neurosci off j Neurosurg Soc Australas 88:150–156
Bjerke BT, Zarrabian M, Aleem IS, Fogelson JL, Currier BL, Freedman BA et al (2018) Incidence of osteoporosis-related complications following posterior lumbar fusion. Glob spine j 8(6):563–569
Karikari IO, Metz LN (2018) Preventing pseudoarthrosis and proximal junctional kyphosis: how to deal with the osteoporotic spine. Neurosurg Clin N Am 29(3):365–374
Nishida M, Yagi M, Suzuki S, Takahashi Y, Nori S, Tsuji O et al (2022) Persistent low bone mineral density in adolescent idiopathic scoliosis: A longitudinal study. J orthop sci off j Jpn Orthop Assoc 28(5):1099–1104
Almomen FA, Altaweel AM, Abunadi AK, Hashem AE, Alqarni RM, Alsiddiky AM (2021) Determining the correlation between Cobb angle severity and bone mineral density in women with adolescent idiopathic scoliosis. J Taibah Univ Med Sci 16(3):365–368
Yang KG, Lee WYW, Hung ALH, Hung VWY, Tang MF, Leung TF et al (2022) Decreased cortical bone density and mechanical strength with associated elevated bone turnover markers at peri-pubertal peak height velocity: a cross-sectional and longitudinal cohort study of 396 girls with adolescent idiopathic scoliosis. Osteoporos int j establ result coop between Eur Found Osteoporos Natl Osteoporos Found USA 33(3):725–735
Lau RW, Cheuk KY, Ng BK, Tam EM, Hung AL, Cheng JC et al (2021) Effects of a home-based exercise intervention (e-fit) on bone density, muscle function, and quality of life in girls with adolescent idiopathic scoliosis (ais): a pilot randomized controlled trial. Int j environ res public health 18(20):10899
Ehresman J, Pennington Z, Schilling A, Lubelski D, Ahmed AK, Cottrill E et al (2020) Novel MRI-based score for assessment of bone density in operative spine patients. spine j off j N Am Spine Soc 20(4):556–562
Huang W, Gong Z, Wang H, Zheng C, Chen Y, Xia X et al (2023) Use of MRI-based vertebral bone quality score (VBQ) of S1 body in bone mineral density assessment for patients with lumbar degenerative diseases. Eur spine j off public Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 32(5):1553–1560
Chen Z, Lei F, Ye F, Zhang H, Yuan H, Li S et al (2023) prediction of pedicle screw loosening using an mri-based vertebral bone quality score in patients with lumbar degenerative disease. World neurosurg 171:e760–e767
Soliman MAR, Aguirre AO, Kuo CC, Ruggiero N, Azmy S, Khan A et al (2022) Vertebral bone quality score independently predicts cage subsidence following transforaminal lumbar interbody fusion. spine j off j N Am Spine Soc 22(12):2017–2023
Clément JL, Pesenti S, Ilharreborde B, Morin C, Charles YP, Parent HF et al (2021) Proximal junctional kyphosis is a rebalancing spinal phenomenon due to insufficient postoperative thoracic kyphosis after adolescent idiopathic scoliosis surgery. Eur spine j off public Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 30(7):1988–1997
Sun Z, Qiu G, Zhao Y, Guo S, Wang Y, Zhang J et al (2015) Risk factors of proximal junctional angle increase after selective posterior thoracolumbar/lumbar fusion in patients with adolescent idiopathic scoliosis. Eur spine j off public Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 24(2):290–297
Deshpande N, Hadi MS, Lillard JC, Passias PG, Linzey JR, Saadeh YS et al (2023) Alternatives to DEXA for the assessment of bone density: a systematic review of the literature and future recommendations. J Neurosurg Spine 38(4):436–445
Dheeraj D, Chauhan U, Khapre M, Kant R (2022) Comparison of quantitative computed tomography and dual x-ray absorptiometry: osteoporosis detection rates in diabetic patients. Cureus 14(3):e23131
Huang Y, Chen Q, Liu L, Feng G (2023) Vertebral bone quality score to predict cage subsidence following oblique lumbar interbody fusion. J Orthop Surg Res 18(1):258
Li W, Zhu H, Liu J, Tian H, Li J, Wang L (2023) Characteristics of MRI‑based vertebral bone quality scores in elderly patients with vertebral fragility fractures. Eur spine j off public Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc
Acknowledgements
Not applicable.
Funding
This study was supported by Sichuan Science and Technology Program (2022ZDZX0029, MZGC20230019), the National Natural Science Foundation of China (81871772; 82172495; 82072434 and 82272546), and the 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (2021HXFH003).
Author information
Authors and Affiliations
Contributions
JW and CZ conceived and designed the study, as well as drafted the initial manuscript. YA, YH, QC, and HD performed the preliminary analyses. GF, LL, and YS critically reviewed and revised the manuscript to ensure significant intellectual content. All authors have approved the final manuscript for submission and accept responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Ethics statement
This study was approved by the Ethics Committee of the West China Hospital. The participant consent was written and was performed in accordance with the ethical standards of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, J., Zhu, C., Ding, H. et al. Simplified S1 vertebral bone quality (vbq) score to assess proximal junctional kyphosis after Lenke 5 adolescent idiopathic scoliosis surgery. Eur Spine J 33, 732–738 (2024). https://doi.org/10.1007/s00586-023-07993-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-023-07993-x