Abstract
Purpose
This study aimed to evaluate the clinical outcomes of full-endoscopic foraminoplasty and lumbar discectomy (FEFLD), unilateral biportal endoscopic (UBE) discectomy, and microdiscectomy (MD) in the treatment of symptomatic lumbar disc herniation (LDH).
Methods
From January 2020 and May 2021, 128 patients with single-level LDH at L4-5 or L5-S1 received FEFLD, UBE discectomy or MD. Patients were divided into three groups according to surgical method: the FEFLD group (n = 43), the UBE group (n = 42), and the MD group (n = 43). Operative time, fluoroscopy frequency, in-bed time, length of hospital stays, total expenses, complications, visual analogue scale (VAS, 0–10), and Oswestry Disability Index (ODI, 0–100%) were assessed and compared among three groups.
Results
There were no significant differences in VAS or ODI scores at 12 months after surgery among three groups. In comparison with the MD group, the FEFLD and UBE group yield better VAS scores for back pain on the first day following surgery (P < 0.05). The FEFLD group was superior to the UBE group or MD group with less time in bed and shorter hospital stay (P < 0.05). The operation time and total expenses in the UBE group were significantly longer and higher than those in the FEFLD group or MD group (P < 0.05).
Conclusions
FEFLD and UBE discectomy yield comparable results to conventional MD concerning pain relief and functional outcomes. In addition, FEFLD and UBE discectomy enable less back pain in the immediate postoperative period. FEFLD offers advantages in rapid recovery. Conventional MD is still an efficient and cost-effective surgical procedure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The radicular syndrome caused by lumber disc herniation affects millions of people throughout the world [1, 2]. Surgery is recommended for patients who are refractory to conservative treatments [3,4,5]. Since Caspar and Yasargil introduced the microsurgical technique in 1977, microdiscectomy (MD) was considered to be the standard treatment for LDH [1, 6,7,8]. However, its subperiosteal approach requires the disruption of paravertebral muscles, which is related to the failed back pain syndrome and spinal instabilities [9, 10]. Tubular microdiscectomy (TMD) was the technique addressing this shortcoming. TMD was performed through a muscle-splitting approach, and in theory, was superior to the open MD in minimizing soft tissue damages [11,12,13]. However, randomized controlled trials (RCTs) showed no significant difference between TMD and open MD in terms of functional outcomes and time to recovery [12, 13].
With the introduction of endoscopes and other related instruments, minimally invasive spine surgery (MISS) for LDH was constantly evolving in recent years. Percutaneous endoscopic lumbar discectomy (PELD) was one of the well-developed endoscopic techniques [14,15,16]. Using one working tunnel with a diameter less than 10 mm, this technique allowed direct visualizations of extruded or prolapsed discs with minimal bony and soft tissue disruptions [15]. Intervertebral foramen enlargement was the key procedure to guarantee adequate decompression of nerve roots via the posterolateral approach [17]. Recently, the application of endoscopic-guided foraminoplasty has been documented [18, 19]. The full-endoscopic foraminoplasty (FEF) has shown advantages in saving intraoperative fluoroscopy and reducing the risk of nerve damages compared to fluoroscopy-guided options [18]. Favourable clinical outcomes were observed in treating highly migrated discs using this technique [20]. It was suggested that the full-endoscopic foraminoplasty and lumbar discectomy (FEFLD) might be a safe and effective alternative for LDH [19].
Since the application of arthroscopy in spine surgery, unilateral biportal endoscopic (UBE) technique also gained popularity for the treatment of lumbar disc disease [21,22,23,24]. UBE surgery was performed through two independent portals on the unilateral side, one portal for the visualization and another for working instruments [23]. Compared with conventional MD, UBE enables percutaneous endoscopic discectomy which reduces the destruction of paraspinal muscles, while providing a magnified and clear field of vision. In addition, the separation of working and visualizing portals facilitates surgical manipulation compared to single-portal endoscopic surgery, which is beneficial for the extraction of prolapsed discs. Case series and comparative studies have shown that UBE surgery could achieve favourable results in treating LDH [21, 22, 24, 25]. However, it still requires the basic skills of endoscopic manipulation, specifically, the establishment of a submuscular space, keeping irrigation outflow and endoscopic haemostasis [26, 27].
As the latest endoscopic spine surgery, FEFLD and UBE discectomy have their own technical characteristics. Whether FEFLD is superior to UBE discectomy or not is worthy of discussion today. The aim of present study is to compare the efficacy and safety of FEFLD, UBE discectomy and conventional MD for the treatment of symptomatic LDH.
Methods
Patient population
This retrospective study was approved by the Ethical Board Review of our hospital, and all patients provided written informed consents. We retrospectively reviewed the database of hospitalized patients who underwent FEFLD, UBE discectomy, or open MD by the same spine surgeons (D.L.Y. and J.X.X.) between January 2020 and May 2021. The inclusion criteria were: (1) patients with the single-level, intraspinal soft herniated disc at the L4/L5 or L5/S1, (2) patients who complained of persistent back pain (BP) and/or radicular pain for more than 12 weeks despite conservative treatment, (3) patients who complained of BP and/or leg pain with new-onset sensorial and/or motor deficit, and (4) the findings of magnetic resonance image (MRI) or computed tomography (CT) were in accordance with the symptoms. Patients were excluded if they were associated with the intervertebral instability (defined as > 3 mm translation, or > 5° angulation), spondylolisthesis, recurrent LDH, cauda equina syndrome, spinal stenosis, fracture, infection, tumour, or with previous lumbar operation at the same level. Two experienced doctors (H.R.C. and J.Y.S.) independently reviewed the patient’s information and the imaging database (including radiographs, MR images, and CT scans). Patients were excluded if any of the exclusion criteria were met. A third senior doctor (J.X.X.) would give objective advises when any inconsistencies exist.
Overall, one hundred and thirty-six patients (90 men and 46 women) with symptomatic LDH at L4-5 or L5-S1 were selected for inclusion in our study. A total of eight patients were excluded because they were lost to follow-up. Consequently, we enrolled 128 patients who underwent surgical treatment and completed a 12-month follow-up. Patients were divided into three groups according to the surgical intervention: the FEFLD group, the UBE group and the MD group. The baseline characteristics of included subjects are shown in Table 1.
Surgical techniques of FEFLD, UBE discectomy, and MD
FEFLD
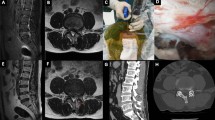
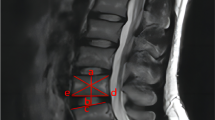
First of all, the standard anteroposterior (AP) and lateral radiographs should be guaranteed for the clear demonstration of superior articular process (SAP) which is an important landmark of lumbar puncture. Surgery was performed under local anaesthesia with patients in the prone position. The entry point was 10–14 cm lateral to the midline of the spinous process in avoidance of the iliac crest. Under the guidance of fluoroscopy, an 18-gauge needle was introduced from the entry point to the SAP of the lower vertebra. The needle tip was directed towards the exterior margin of SAP in the AP view, and towards the ventral SAP in the lateral view. Then, the needle core was removed, and a guide wire was inserted through the needle. An 8-mm incision was made, and sequential dilators were placed along the guide wire. Finally, a U-head working channel (UNINTECH, Shanghai, China) was introduced over the final dilator and docked firmly with the SAP (Fig. 1a). At this time, AP and lateral radiographs were needed to make sure the location of the working channel.
Under endoscopic visualization (Joimax, Karlsruhe, Germany), soft tissues were removed using the nucleus forceps, and the osseous part of SAP was exposed (Fig. 2a). The ventral SAP was partially resected using the endoscopic trephine (Fig. 1b). The trephine rotated and advanced carefully along the working channel. The depth of the trephine was monitored by the scale on its inner surface (Fig. 2b). The drilling was stopped once any rotation of the osseous core was noted, a suggestion that the spinal canal was about to be entered, and this is a warning sign to the surgeon (Fig. 2c, d). The sawn bone cylinder is removed entirely or in pieces with forceps. Subsequently, the inner T-head cannula was pushed forward into the spinal canal (Fig. 1a), and the ligamentum flavum was directly removed with forceps. Finally, the herniated disc was identified and removed until the nerve root was seen to move freely during Valsalva's manoeuvre. The wound was sutured after careful haemostasis using a radiofrequency coagulator. No drainage was required. In cases of highly migrated discs, repeated foraminoplasty was necessary and could be easily achieved under the guidance of endoscope. The representative case is presented in Fig. 3a–i.
Full-endoscopic visualized foraminoplasty procedures. a, Soft tissues were removed using the nucleus forceps, and the osseous part of SAP was exposed. b, The trephine was docked firmly at the osseous part of SAP. The depth of the trephine was monitored by the scale on its inner surface. c, The drilling was stopped once any rotation of the osseous core was noted. d, Foraminoplasty was completed, and the ligamentum flavum (asterisk) and the herniated disc (triangle) were detected
A 58-year-old female patient diagnosed with L4-5 disc herniation underwent the FEFLD surgery. a and b, Preoperative magnetic resonance imaging (MRI) scans. c, The trephine was docked firmly at the osseous part of SAP. d, The trephine rotated and advanced carefully along the working channel. e, When foraminoplasty was completed, the position of the trephine was shown in the AP fluoroscopic view. f, The herniated nucleus pulposus was extracted. g, Sufficient decompression of the traversing nerve root (asterisk) was ensured. h and i, MRI scans 12 months after the surgery
UBE
Take the left approach as an illustration. The UBE discectomy was performed under general anaesthesia with patients in the prone position. The affected disc was confirmed using C-arm fluoroscopy. Two incisions centred on the target intervertebral space were made on the left side. The incisions were 3 cm apart from each other and 1.0–1.5 cm lateral to the midline. The cranial portal provided an endoscopic field of view and continuous irrigation, and the caudal portal is used for surgical instruments. Under fluoroscopy, two guide rods were inserted through the portals and met with each other at the junction of spinous process and lamina of the upper vertebra. Then, the soft tissue was bluntly dissected by sequential dilators. The endoscope (Stryker, Kalamazoo, MI, USA) and radiofrequency (RF) ablation (GAOTON, Xi’an, China) were placed through the observational and working channel, respectively. Firstly, the soft tissue within the field of view was cleaned using RF ablation and forceps, and the lower aspect of the upper lamina was exposed. A partial laminotomy was performed using automatic drills (XIYI, Tianjin, China) and Kerrison punches. The extent of bony decompression complied with the following standards: (1) the cranial decompression reached the attachment of ligamentum flavum; and (2) the lateral decompression should approach the medial aspect of pedicles. The ligamentum flavum was removed using Kerrison punches, followed by the identification of the dural sac and nerve root. The traversing nerve root was gently retracted towards the midline of spinal canal, and discectomy was performed using nucleus forceps. Finally, the absence of residual fragments was confirmed using a 90° hooked probe. After meticulous haemostasis, a drainage tube was placed outside the lamina and the wounds were sutured. The representative case is presented in Fig. 4a–i.
A 30-year-old male patient diagnosed with L5-S1 disc herniation underwent the UBE discectomy. a and b, Preoperative magnetic resonance imaging (MRI) scans. c, d and e, Under fluoroscopy, two guide rods were inserted through the portals and met with each other at the junction of spinous process and lamina of the upper vertebra. Then, the soft tissue was bluntly dissected by sequential dilators. f, The lower aspect of the L5 lamina was partially resected using automatic drills. e, When foraminoplasty was completed, the position of the trephine was shown in the AP fluoroscopic view. f, The herniated nucleus pulposus was extracted, and sufficient decompression of the traversing nerve root (asterisk) was ensured. h and i, MRI scans 12 months after the surgery
MD
The MD was performed under general anaesthesia with patients in the prone position. The affected disc was confirmed using C-arm fluoroscopy. A 4- to 5-cm longitudinal incision was made on the affected side. The paraspinal musculature from the hemilamina was partially detached in a subperiosteal fashion. The interlaminar space was then visualized, and a hemilaminar retractor was placed into position. A lateral fluoroscopy was needed to confirm the correct level. Subsequently, a partial laminotomy was performed using Kerrison punches, and the extent of decompression was similar to that of UBE. After the resection of the ligamentum flavum, the dura sac, nerve root, and protruded disc were exposed, and discectomy was performed for complete decompression. All techniques were performed with the aid of microscopic magnification.
Clinical evaluation
Perioperative information (operative time, fluoroscopy frequency, in-bed time, length of hospital stays, total expenses, and complications) was assessed via clinical records and video documents. Operative time for MD or UBE discectomy was measured as incision to closure, and for FEFLD was measured as local anaesthesia to closure. Length of stay was defined as the number of days that a patient stayed at the hospital after surgery. Pain intensity and quality of daily living were analysed using the visual analogue scale (VAS) and Oswestry Disability Index (ODI), respectively. VAS score for leg pain and back pain (0–10) was evaluated preoperatively and at 1-day, 3-month, and 12-month postoperatively. ODI (0–100%) was evaluated preoperatively and at 12-month postoperatively. Patient satisfaction was evaluated according to the modified MacNab criteria (excellent, good, fair, and poor). Lumbar MR images were obtained at the time of the latest follow-up examinations.
Statistical analysis
Statistical analysis was performed using SPSS 21.0 (SPSS Inc., Chicago, IL). A probability value 0.05 was considered to indicate a statistically significant difference. The Mann–Whitney U test, Kruskal–Wallis test for nonparametric data and Student t test, one-way analysis of variance (ANOVA) for parametric data were used to compare the variables. Least-significant difference (LSD) post hoc test was utilized for subgroup comparison after ANOVA test.
Results
The mean age of the 128 patients was 35.8 ± 13.0 years (range 14–66 years), and male patients accounted for 70.3% (90/128) of the total. Of the 128 patients, 43 patients received FEFLD, 42 patients received UBE discectomy, and 43 patients received MD. As proven by P values greater than 0.05, no statistically significant differences were found with regard to baseline characteristics and clinical profiles of three groups. Paracentral herniation was the most common type of herniation in each group of patients, which accounted for 51.2% of cases in the FEFLD group, 50.0% in the UBE group, and 46.5% in the MD group.
In this study, the mean operative times were 101.4 ± 35.0 min in the FEFLD group, 144.4 ± 43.1 min in the UBE group, and 97.1 ± 39.7 min in the MD group, respectively (Table 2). The mean duration of surgery in the UBE group was significantly longer than that in the FEFLD group (P < 0.001) or MD group (P < 0.001) (Fig. 5a). Intraoperative fluoroscopy was most frequently used in the FEFLD surgery (Fig. 5b). However, postoperative in-bed time (1.1 ± 0.4 days) and length of hospital stays (1.8 ± 1.0 days) in the FEFLD group were significantly shorter than those in the UBE group (2.9 ± 0.9 days and 4.7 ± 1.8 days, respectively) and MD group (3.2 ± 1.2 days and 5.1 ± 2.6 days, respectively) (Fig. 5c, d). In addition, the total hospital cost was significantly higher in the UBE group (¥37,249.7 ± 7860.0) compared with the FEFLD group (¥21,953.0 ± 4538.0, P < 0.001) and MD group (¥20,873.4 ± 3882.3, P < 0.001) (Fig. 5e).
In this series, only one case in the UBE group converted to an open surgery due to intraoperative incidental durotomy. The total complication rate was 11.6% (n = 5) for the FEFLD group, 14.3% (n = 6) for the UBE group, and 16.3% (n = 7) for the MD group (Table 2). The difference was not statistically significant among three groups (P = 0.824). Both UBE and MD group had one case of dural tear, whereas no incidental durotomy was observed in the FEFLD group. Neural injury was rare in this series and occurred in one patient in the UBE group. Two cases of wound hematoma and two cases of wound infection were documented in the MD group. Residue/recurrence of herniation occurred in two patients in the FEFLD group, one patient in the UBE group, and one patient in the MD group. At 1 year, the reoperation rate was 2.3% (n = 1) after FEFLD and 9.3% (n = 4) after MD. The specific information of the secondary operation of three groups is recorded in Table 3.
We compared VAS, ODI and patient satisfaction of three groups according to the type of disc herniation. Results showed that postoperative VAS and ODI score improved significantly in all three groups for each type of disc herniation (Tables 4, 5, 6). In the treatment of prolapsus/sequestered herniation, the FEFLD and UBE group achieved better VAS scores for BP on the first day following surgery in comparison with the MD group (P < 0.05). No significant differences existed in VAS and ODI scores at 3 month and 12 months after surgery (P > 0.05). According to the modified MacNab criteria, the good to excellent rate of FEFLD group was 88.9% for central disc herniation, 90.9% for paracentral herniation and 83.3% for prolapsus/sequestered herniation. The satisfaction rates were 100%, 85.7% and 100% for UBE group, and 100%, 85% and 86.7% for MD group, respectively.
Discussion
In most circumstances, patients prefer a minimally invasive approach to their treatment due to quick postoperative recovery [28, 29]. Whether MISS can achieve comparable clinical outcomes to open surgery has always been a concern of spine surgeons. FEFLD and UBE discectomy are both newly proposed MISS techniques. Evidence from case series reported satisfactory results of two methods in the treatment of LDH [19,20,21, 30]. However, to date, limited studies have compared the clinical outcomes from FEFLD, UBE, and open MD. The results of this retrospective study demonstrated that FEFLD, UBE discectomy and MD can achieve equivalent and satisfactory outcomes at 12 months follow-up. FEFLD is associated with faster recovery of patients which is reflected in shorter in-bed time and length of hospital stays. UBE discectomy can achieve reliable clinical results with 100% satisfaction for central and sequestered herniation, but at the cost of highest expenses. MD is still an efficient and cost-effective surgical procedure.
Compared with conventional foraminoplasty, the FEF technique has the following advantages. First of all, the trajectory of needle puncture is closer to the caudal side of intervertebral foramen, and the exiting root is less susceptible to irritation. Once the sawn bone cylinder became mobile, surgeons could realize that foraminoplasty is about to finish. This warning sign is also helpful for avoiding traversing root injuries. According to the literature, the incidence of nerve root injuries was reported as 0–1.2% through FEFLD [18, 19, 31]. There was no case of neurological complication in FEFLD group of the present study. In addition to improved safeness, surgical procedures of FEF are simplified accordingly with no need to change instruments repeatedly during foraminoplasty. Ouyang et al. compared the clinical outcomes by using the FEFLD and conventional PELD for the treatment of lumbar disc herniation [18]. They found that the operation time and fluoroscopy time of FEFLD group were significantly shorter than that of PELD group. In this study, FEFLD group achieved significantly shorter operation time than UBE group (101.4 ± 35.0 vs 144.4 ± 43.1, P < 0.001). Although intraoperative fluoroscopy was most frequently used in the FEFLD group, it has been reduced significantly compared with those of conventional PELD in previous studies [32,33,34].
UBE discectomy shared the same interlaminar approach with MD [26, 35]. The separation of viewing and working portals was one notable distinction between UBE technique and uniportal endoscopic discectomy. This characteristic enables UBE to take advantages of both MD (e.g. high flexibility in manipulation) and PELD (e.g. clear and amplified visualization) [23, 35]. However, this technique still has a steep learning curve for most beginners [36]. Published data from comparative studies showed that the mean operation time of UBE discectomy was longer than that of PELD or MD [25, 37]. In this study, the mean operation time was longest in UBE group, indicating that UBE has no advantages in reducing the operation time. In our experience, the establishment of working space and intraoperative haemostasis are time intensive in UBE discectomy. With the accumulation of surgical experience, the operation time should be gradually shortened.
We compared the clinical outcomes of three approaches for different types of LDHs. In the treatment of sequestered herniations, FEFLD and UBE discectomy have advantages in alleviating back pain at the first day after surgery. Our results demonstrated that FEFLD, UBE and MD group all achieved remarkable improvement of VAS and ODI scores for each type of herniation at the last follow-up. Although there was no significant difference between the groups based on the scoring system, we still concluded some indications for each surgery. Actually, the indications of transforaminal discectomy have been constantly expanding with the development of endoscopic instruments and foraminoplasty techniques [30]. In our experience, FEFLD is competent for direct removal of paracentral herniations and sequestered herniations either in downward or upward direction. When dealing with the highly downward-migrated LDHs, foraminoplasty or partial pediculectomy is usually needed for the detection of disc fragments [20, 30]. As for massive central herniations, intradisc decompression combined with neurolysis is effective in relieving symptoms. Some studies suggested that the transforaminal approach was difficult for patients with L5-S1 pathologies and high iliac crests [38,39,40]. Although the foraminoplasty could handle this problem to some extent, considering the difficulty, safety and benefits of the surgery, we considered that the interlaminar access was more suitable for these patients. UBE technique shares a wide variety of indications with conventional MD. Our results showed that the UBE group achieved excellent satisfaction rate (100%) for both central and sequestered disc herniations. However, its efficacy for upward-migrated LDHs remains limited due to the extent of bony decompression. Benefiting from the greater flexibility of instruments, conventional MD is able to solve this problem by expanding decompression, such as hemilaminectomy and spinous process resection.
In the present study, the postoperative in-bed time and length of hospital stays in FEFLD group were significantly shorter than those in UBE group and MD group, which meant that patients underwent FEFLD were allowed to have rapid mobilization, rehabilitation, and a quicker return to daily life. These factors are important especially for young patients who have willingness to return to their jobs earlier. Our study showed that patients treated with UBE discectomy would pay more admission fee compared with MD and FEFLD technique. This result may be related to the expensive endoscopic instruments in UBE surgery.
Our study showed no significant difference regarding to the total complication rate among three groups. It is worth noting that two cases of wound infection and two cases of wound hematoma were identified in the MD group, whereas, no such complication occurred in the FEFLD or UBE group. This result showed the advantage of MISS technique in reducing wound complications after surgery. The recurrence rate is a major concern for FEFLD or UBE discectomy, with an incidence ranged from 0–6.9% [22, 24, 25, 41,42,43]. Patients treated with FEFLD were expected to have higher rates of recurrent disc herniation due to limited flexibility in manipulation and reduced disc removal. Even though the recurrence rate of three groups was similar at 12 months follow-up in the present study, studies with longer follow-up are needed to verify this conclusion.
The present study had some limitations that should be mentioned. First of all, this study has a relatively small sample size and a short-term follow-up period. Therefore, further prospective studies with randomized controlled design for FEFLD and UBE are required to verify the present results. In addition, only patients with intraspinal disc herniations were included, while those with lumbar foraminal or extraforaminal disc herniations on magnetic resonance imaging were excluded. For these patients, the herniated disc is often removed without the need of a foraminoplasty. Hence, there is no reason to assume that the results of this study are valid for these patients.
Conclusions
FEFLD and UBE discectomy yield comparable results to conventional MD concerning pain relief and functional outcomes at 12 months postoperatively. In addition, FEFLD and UBE discectomy enable less back pain in the immediate postoperative period. FEFLD offers advantages in rapid recovery. UBE discectomy can achieve reliable clinical results with 100% satisfaction for central and sequestered herniation, but at the cost of highest expenses. Conventional MD is still an efficient and cost-effective surgical procedure. Because this study is a retrospective study with only 1 years of follow-up, further prospective, randomized controlled trials are needed to verify our current findings.
Data and materials availability
Raw data would be made available on reasonable request and with the permission of the institution where the data were generated. Hengrui Chang was the person to be contacted if someone wants to request the data from this study.
References
Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, Cho CH, DePalma MJ, Dougherty P 2nd, Fernand R, Ghiselli G, Hanna AS, Lamer T, Lisi AJ, Mazanec DJ, Meagher RJ, Nucci RC, Patel RD, Sembrano JN, Sharma AK, Summers JT, Taleghani CK, Tontz WL Jr, Toton JF (2014) An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J : Off J N Am Spine Soc 14:180–191. https://doi.org/10.1016/j.spinee.2013.08.003
Koes BW, van Tulder MW, Peul WC (2007) Diagnosis and treatment of sciatica. BMJ (Clin Res Ed) 334:1313–1317. https://doi.org/10.1136/bmj.39223.428495.BE
Gibson JN, Waddell G (2007) Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev: Cd001350. https://doi.org/10.1002/14651858.CD001350.pub3
Ahn SS, Kim SH, Kim DW, Lee BH (2016) Comparison of outcomes of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for young adults: a retrospective matched cohort study. World Neurosurg 86:250–258. https://doi.org/10.1016/j.wneu.2015.09.047
Weinstein JN, Tosteson TD, Lurie JD, Tosteson AN, Hanscom B, Skinner JS, Abdu WA, Hilibrand AS, Boden SD, Deyo RA (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the spine patient outcomes research trial (SPORT): a randomized trial. JAMA 296:2441–2450. https://doi.org/10.1001/jama.296.20.2441
Imhof HG, von Ammon K, Yasargil MG (1994) Use of the microscope in surgery of lumbar disk hernia. Aktuelle Probl Chir Orthop 44:15–20
Caspar W, Campbell B, Barbier DD, Kretschmmer R, Gotfried Y (1991) The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery 28:78–86. https://doi.org/10.1097/00006123-199101000-00013
Awad JN, Moskovich R (2006) Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res 443:183–197. https://doi.org/10.1097/01.blo.0000198724.54891.3a
Casal-Moro R, Castro-Menéndez M, Hernández-Blanco M, Bravo-Ricoy JA, Jorge-Barreiro FJ (2011) Long-term outcome after microendoscopic diskectomy for lumbar disk herniation: a prospective clinical study with a 5-year follow-up. Neurosurgery 68:1568–1575; discussion 1575. https://doi.org/10.1227/NEU.0b013e31820cd16a
Wenger M, Mariani L, Kalbarczyk A, Gröger U (2001) Long-term outcome of 104 patients after lumbar sequestrectomy according to Williams. Neurosurgery 49:329–334. https://doi.org/10.1097/00006123-200108000-00013
Franke J, Greiner-Perth R, Boehm H, Mahlfeld K, Grasshoff H, Allam Y, Awiszus F (2009) Comparison of a minimally invasive procedure versus standard microscopic discotomy: a prospective randomised controlled clinical trial. Eur Spine J : Off Publ Euro Spine Soc, Euro Spinal Deform Soc, Euro Sect Cerv Spine Res Soc 18:992–1000. https://doi.org/10.1007/s00586-009-0964-2
Arts MP, Brand R, van den Akker ME, Koes BW, Bartels RH, Peul WC (2009) Tubular diskectomy vs conventional microdiskectomy for sciatica: a randomized controlled trial. JAMA 302:149–158. https://doi.org/10.1001/jama.2009.972
Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V (2008) Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery 62:174–181. https://doi.org/10.1227/01.Neu.0000311075.56486.C5
Lee DY, Shim CS, Ahn Y, Choi YG, Kim HJ, Lee SH (2009) Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J Korean Neurosurg Soc 46:515–521. https://doi.org/10.3340/jkns.2009.46.6.515
Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine 33:931–939. https://doi.org/10.1097/BRS.0b013e31816c8af7
Yeung AT, Tsou PM (2002) Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine 27:722–731. https://doi.org/10.1097/00007632-200204010-00009
Zhao Y, Yuan S, Tian Y, Liu X (2020) Necessity of routinely performing foraminoplasty during percutaneous endoscopic transforaminal discectomy (PETD) for lumbar disc herniation. Br J Neurosurg. https://doi.org/10.1080/02688697.2020.1817853
Ouyang ZH, Tang M, Li HW, Zou MX, Li XL, Wang WJ, Yan YG (2021) Full-endoscopic foraminoplasty using a visualized bone reamer in the treatment of lumbar disc herniation: a retrospective study of 80 cases. World Neurosurg 149:e292–e297. https://doi.org/10.1016/j.wneu.2021.02.033
Hua W, Zhang Y, Wu X, Gao Y, Li S, Wang K, Yang S, Yang C (2019) Full-endoscopic visualized foraminoplasty and discectomy under general anesthesia in the treatment of L4–L5 and L5–S1 disc herniation. Spine 44:E984-e991. https://doi.org/10.1097/brs.0000000000003014
Cai H, Liu C, Lin H, Wu Z, Chen X, Zhang H (2022) Full-endoscopic foraminoplasty for highly down-migrated lumbar disc herniation. BMC Musculoskelet Disord 23:303. https://doi.org/10.1186/s12891-022-05254-4
Kim SK, Kang SS, Hong YH, Park SW, Lee SC (2018) Clinical comparison of unilateral biportal endoscopic technique versus open microdiscectomy for single-level lumbar discectomy: a multicenter, retrospective analysis. J Orthop Surg Res 13:22. https://doi.org/10.1186/s13018-018-0725-1
Jiang HW, Chen CD, Zhan BS, Wang YL, Tang P, Jiang XS (2022) Unilateral biportal endoscopic discectomy versus percutaneous endoscopic lumbar discectomy in the treatment of lumbar disc herniation: a retrospective study. J Orthop Surg Res 17:30. https://doi.org/10.1186/s13018-022-02929-5
Lin GX, Huang P, Kotheeranurak V, Park CW, Heo DH, Park CK, Park JY, Kim JS (2019) A systematic review of unilateral biportal endoscopic spinal surgery: preliminary clinical results and complications. World Neurosurg 125:425–432. https://doi.org/10.1016/j.wneu.2019.02.038
Soliman HM (2013) Irrigation endoscopic discectomy: a novel percutaneous approach for lumbar disc prolapse. Euro Spine J : Off Publ Euro Spine Soc, Euro Spinal Deform Soc, Euro Sect Cerv Spine Res Soc 22:1037–1044. https://doi.org/10.1007/s00586-013-2701-0
Hao J, Cheng J, Xue H, Zhang F (2022) Clinical comparison of unilateral biportal endoscopic discectomy with percutaneous endoscopic lumbar discectomy for single l4/5-level lumbar disk herniation. Pain Pract: Off J World Inst Pain 22:191–199. https://doi.org/10.1111/papr.13078
Kim JE, Choi DJ (2018) Unilateral biportal endoscopic decompression by 30° endoscopy in lumbar spinal stenosis: technical note and preliminary report. J Orthop 15:366–371. https://doi.org/10.1016/j.jor.2018.01.039
Choi DJ, Choi CM, Jung JT, Lee SJ, Kim YS (2016) Learning curve associated with complications in biportal endoscopic spinal surgery: challenges and strategies. Asian Spine J 10:624–629. https://doi.org/10.4184/asj.2016.10.4.624
White CA, Patel AV, Butler LR, Amakiri UO, Yeshoua BJ, Steinberger JM, Cho SK, Kim JS (2022) Comparison of patient preference, understanding, and sentiment for minimally invasive versus open spine surgery. Spine 47:309–316. https://doi.org/10.1097/brs.0000000000004134
Narain AS, Hijji FY, Duhancioglu G, Haws BE, Khechen B, Manning BT, Colman MW, Singh K (2018) Patient perceptions of minimally invasive versus open spine surgery. Clin Spine Surg 31:E184-e192. https://doi.org/10.1097/bsd.0000000000000618
Chen CM, Lin GX, Sharma S, Kim HS, Sun LW, Wu HH, Chang KS, Chen YC (2020) Suprapedicular retrocorporeal technique of transforaminal full-endoscopic lumbar discectomy for highly downward-migrated disc herniation. World Neurosurg 143:e631–e639. https://doi.org/10.1016/j.wneu.2020.08.038
He J, Tang J, Jiang X, Ren H, Cui J, Liang Z, Zhang J, Liang D (2020) Efficacy and safety of foraminoplasty performed using an endoscopic drill to treat axillary disc herniation. World Neurosurg 138:e413–e419. https://doi.org/10.1016/j.wneu.2020.02.143
Ahn Y, Kim CH, Lee JH, Lee SH, Kim JS (2013) Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine 38:617–625. https://doi.org/10.1097/BRS.0b013e318275ca58
Iprenburg M, Wagner R, Godschalx A, Telfeian AE (2016) Patient radiation exposure during transforaminal lumbar endoscopic spine surgery: a prospective study. Neurosurg Focus 40:E7. https://doi.org/10.3171/2015.11.Focus15485
Fan G, Gu X, Liu Y, Wu X, Zhang H, Gu G, Guan X, He S (2016) Lower learning difficulty and fluoroscopy reduction of transforaminal percutaneous endoscopic lumbar discectomy with an accurate preoperative location method. Pain Physician 19:E1123-e1134
Hwa Eum J, Hwa Heo D, Son SK, Park CK (2016) Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine 24:602–607. https://doi.org/10.3171/2015.7.Spine15304
Chen L, Zhu B, Zhong HZ, Wang YG, Sun YS, Wang QF, Liu JJ, Tian DS, Jing JH (2022) The learning curve of unilateral biportal endoscopic (UBE) spinal surgery by CUSUM analysis. Front Surg 9:873691. https://doi.org/10.3389/fsurg.2022.873691
Choi KC, Shim HK, Hwang JS, Shin SH, Lee DC, Jung HH, Park HA, Park CK (2018) Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg 116:e750–e758. https://doi.org/10.1016/j.wneu.2018.05.085
Li M, Yang H, Yang Q (2015) Full-endoscopic technique discectomy versus microendoscopic discectomy for the surgical treatment of lumbar disc herniation. Pain Physician 18:359–363
Choi KC, Park CK (2016) Percutaneous endoscopic lumbar discectomy for L5–S1 disc herniation: consideration of the relation between the iliac crest and L5–S1 disc. Pain Physician 19:E301-308
Lee SH, Kang HS, Choi G, Kong BJ, Ahn Y, Kim JS, Lee HY (2010) Foraminoplastic ventral epidural approach for removal of extruded herniated fragment at the L5–S1 level. Neurol Med Chir 50:1074–1078. https://doi.org/10.2176/nmc.50.1074
Chen Z, Zhang L, Dong J, Xie P, Liu B, Wang Q, Chen R, Feng F, Yang B, Shu T, Li S, Yang Y, He L, Pang M, Rong L (2018) Percutaneous transforaminal endoscopic discectomy compared with microendoscopic discectomy for lumbar disc herniation: 1-year results of an ongoing randomized controlled trial. J Neurosurg Spine 28:300–310. https://doi.org/10.3171/2017.7.Spine161434
Zhou C, Zhang G, Panchal RR, Ren X, Xiang H, Xuexiao M, Chen X, Tongtong G, Hong W, Dixson AD (2018) Unique complications of percutaneous endoscopic lumbar discectomy and percutaneous endoscopic interlaminar discectomy. Pain Physician 21:E105-e112
Hoogland T, Schubert M, Miklitz B, Ramirez A (2006) Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine 31:E890-897. https://doi.org/10.1097/01.brs.0000245955.22358.3a
Acknowledgements
None.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
WYD designed the study; HRC and JXX searched relevant studies; HRC, JXX and DLY analysed and interpreted the data; HRC wrote the manuscript; and WYD approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors reported no conflicts of interest to declare in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chang, H., Xu, J., Yang, D. et al. Comparison of full-endoscopic foraminoplasty and lumbar discectomy (FEFLD), unilateral biportal endoscopic (UBE) discectomy, and microdiscectomy (MD) for symptomatic lumbar disc herniation. Eur Spine J 32, 542–554 (2023). https://doi.org/10.1007/s00586-022-07510-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07510-6