Abstract
Purpose
We show a systematic review of known complications during intraoperative neuromonitoring (IONM) using transcranial electric stimulation motor evoked potentials (TES-MEP) on cervical spine surgery, which provides a summary of the main findings. A rare complication during this procedure, cardiac arrest by cardioinhibitory reflex, is also described.
Methods
Findings of 523 scientific papers published from 1995 onwards were reviewed in the following databases: CENTRAL, Cochrane Library, Embase, Google Scholar, Ovid, LILACS, PubMed, and Web of Science. This study evaluated only complications on cervical spine surgery undergoing TES-MEP IONM.
Results
The review of the literature yielded 13 studies on the complications of TES-MEP IONM, from which three were excluded. Five studies are case series; the rest are case reports. Overall, 169 complications on 167 patients were reported in a total of 38,915 patients, a global prevalence of 0.43%. The most common complication was tongue-bite in 129 cases, (76.3% of all complication events). Tongue-bite had a prevalence of 0.33% (CI 95%, 0.28–0.39%) in all patients on TES-MEP IONM. A relatively low prevalence of severe complications was found: cardiac-arrhythmia, bradycardia and seizure, the prevalence of this complications represents only one case in all the sample. Alongside, we report the occurrence of cardiac arrest attributable to TES-MEP IONM.
Conclusions
This systematic review shows that TES-MEP is a safe procedure with a very low prevalence of complications. To our best knowledge, asystole is reported for the first time as a complication during TES-MEP IONM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraoperative multimodal neuromonitoring (IOMN) has been demonstrated to be an accurate and safe procedure in the early identification of spinal cord damage during cervical spine surgery due to trauma, degenerative diseases, or spine deformity [1,2,3,4,5,6,7]. There is a wide variety of methods for its monitoring, such as continuous electromyography (EMG), evoked EMG, urethral and anal sphincter EMG, compound muscle action potential (CMAP), motor evoked potentials (MEP), and spinal cord mapping [3, 5, 8,9,10].
Recently, several methods involving non-invasive transcranial stimulation of the human motor cortex have been used for physiological research and therapeutic purposes [11, 12]. The most common procedures are transcranial electrical stimulation, transcranial magnetic stimulation, and direct transcranial stimulation [11, 13,14,15,16,17,18]. Intraoperative neuromonitoring with transcranial electrical stimulation motor evoked potential monitoring (TES-MEP) is a broadly used procedure and standardized by guidelines regarding anesthesia, equipment, performance, personnel, risk criteria, and documentation in brain, spine, carotid, and aorta surgery [7, 14, 19, 20].
TES-MEP consists of the application of a high voltage electric stimulus through electrodes in the scalp. The stimuli cause contralateral muscular contractions that can be monitored by electromyography; in other words, it provokes motor evoked potentials [11]. Despite its advantages, TES-MEP presents some complications [7]; in brain and spine surgery, they include mouth and tongue laceration, mandibular fractures, dental luxation, endotracheal cannula rupture, bradycardia, asystole, and seizures (clinical and subclinical) [14, 21,22,23, 24].
In this work, we present a systematic review on IONM complications during cervical spine surgery using TES-MEP and describe an event of bradycardia and asystole mediated by TES-MEP.
Case report
History and examination
We report the case of a 58-year-old man with a history of hyperuricemia treated with allopurinol as the only previously known medical condition, who initially presented with radicular symptoms such as pain in the left upper limb that radiated to the left interscapulo-vertebral area. On neurological examination, the patient showed left palmar weakness and decreased tricipital deep-tendon reflex. A cervical spine MRI was obtained and revealed a herniated foraminal disk on the C6-7 level (Fig. 1). Symptoms did not improve after medical treatment and physical therapy for three months. His preoperative cardiac, pulmonary and renal evaluation was normal, and was determined as ASA II preoperative risk from the American Society of Anesthesiologists [25]. No pre-operative MEP by transcranial magnetic stimulation (TMS) testing was performed. This technique is seldom performed in cases of suspected unstable cervical spine due to potential TMS-induced damage.
Operation and IONM
The patient consented to the performing of posterior cervical foraminotomy under intraoperative neuromonitoring. Neuromonitoring was implemented continuously until the patient emerged from anesthesia. He was induced with 0.97 mg/kg of 2% lidocaine, 2 mg/kg of propofol, 1.5 µg/kg of fentanyl, and 0.60 mg/kg of rocuronium. Endotracheal intubation, central venous and arterial line catheter and urinary catheterization with a Foley catheter were executed, and subdermal electrodes were placed for neurophysiological monitoring, without complications. A soft bite block was placed (four 4 × 4-inch absorbent pads with radiopaque marker, rolled and moistened in saline solution) to prevent the possibility of biting the tongue. The head was supported and fixed with a Mayfield head holder with three pins placed at 60 lbs, and the patient was carefully turned to the prone position; for this maneuver, anesthesia was maintained with an infusion of propofol and fentanyl. There were no unusual events in the hemodynamic response. In this phase of the procedure, the patient maintained a mean heart rate of 82 bpm, blood pressure 110/72 mmHg, arterial saturation 100%, and end-tidal carbon dioxide pressure (ETCO2) of 32 mmHg. Figure 2 depicts basal vital parameters.
IONM of the spinal cord and cervical roots was carried out using Natus equipment, 32-channel XLTEK Protektor. The integrity of the motor and sensory tracts of the spinal cord was evaluated by TES-MEP and somatosensory evoked potentials (SEPs), respectively.
The integrity of the nerve roots was monitored with spontaneous electromyographic activity and TES-MEP of the upper limbs by the administration of short trains of high-voltage, low-duration pulses (50–75 μs) through the scalp to activate the corticospinal tract. The constant voltage stimulus was applied through subdermal electrodes placed at C-1 and C-2 (International System 10–20) overlying the primary motor cortex; the cortical potentials were recorded with cup electrodes (Grass Instruments, Quincy, Massachusetts) set at Cpz, Cp3, and Cp4 and referenced to Fpz (International System 10–20). Anodal stimulation was delivered in trains of 3–7 pulses at 500–1000 pulses per second, with intensities in the range of 300–700 V. The TES-MEP response was captured by needle electrodes inserted in the deltoids, biceps, and the first dorsal interosseous muscles, as well as in the tibialis anterior and abductor hallucis muscles, bilaterally after short duration high voltage anodal electrical stimulus trains ((400 to 1000-V, pulse width = 50 µS, N = 3–7, interval interpulse = 1 to 5 ms). The motor responses were filtered between 10 and 1500 HZ. SEPs of the four extremities were also monitored to evaluate the afferent sensory tracts, and the spontaneous electromyographic activity of the four extremities was also observed. These stimuli were given by two corkscrew electrodes (A-Gram, Glenn Rock, New Jersey) inserted over the regions of the primary motor cortex in C1 and C2 (international system 10–20), produced by the same equipment of neuromonitoring.
Intravenous general anesthesia was maintained using continuous infusions of propofol (120 µg/kg/min) and fentanyl (1.5 µg/kg/h). The use of inhaled anesthetics was purposely avoided to optimize IONM. Only an initial dose of rocuronium was used to facilitate intubation and initial surgical exposure.
The surgical procedure started without complications. Once the patient was positioned and the surgical incision site marked and corroborated by fluoroscopy, an extensive antiseptic wash with Iodine Povacrylex [0.7% available iodine] and Isopropyl Alcohol, 74% (3 M™ DuraPrep™ Surgical Solution) of the posterior cervical region was performed; the skin was covered with sterile drapes, and antimicrobial incise drape (3 M™ Ioban™).
During base line testing with TES-MEP performed by 125 mA, 1 ms duration and 500 Hz frequency 5 pulses trains, before starting the decompression procedure, when the stimulation and recording of TES-MEP and SEPs began to, an episode of bradycardia and brief asystole was observed, it was confirmed that the isoelectric line of the electrocardiogram (ECG) of the monitor coincided with flattening of the plethysmography curve and abatement of the capnogram, a few seconds later a return to spontaneous circulation was observed with normalization of the mentioned monitoring parameters. After the anesthesiologist reported these changes, the surgical procedure was aborted, before the start of the planed surgery, and the stimulation and recording of TES-MEP and SEPs were repeated to corroborate the causality of the phenomenon, which was repeated immediately after stimulation. The surgical procedure was suspended, and the patient was turned in the supine position and the Mayfield head holder removed. The patient emerged from anesthesia without complications, was extubated, sent to the recovery room for 90 min, and was discharged from the hospital the following day, after a cardiovascular evaluation that included 24-h Holter monitoring, transesophageal echocardiography, and speed- and incline-based test with the Bruce Protocol that resulted normal. Figure 3 depicts the event footage in the anesthesia monitor. Written informed consent for publication of medical details was obtained from the patient. He was lost to long follow-up after two monthly follow up appointments.
Methods
Literature review
We followed the PRISMA-P recommendations [26]. The literature search was conducted in the following databases: CENTRAL, Cochrane Library, Embase, Google Scholar, Ovid, LILACS, Pubmed, and Web of Science. The search strategy was based on the medical subject headings (MeSH) and keywords: "transcranial electrical stimulation," "motor evoked potentials," "Transcranial Electric Motor Evoked Potential Monitoring," "complication" "adverse effects, " "Cervical spine surgery." The search was limited to publications in English, French, Spanish, and Japanese languages and to publications from 1995 onwards. In order to broaden the search, we use the "related articles" function of the search engines, and we examine the references of some selected publications. We consulted experts on the subject with the intention of identifying cases reported in gray literature, which our search would not have recognized.
Inclusion and exclusion criteria
Medical articles were included if they reported the presence of complications and adverse events in patients undergoing cervical spine surgery procedures in which transcranial electrical stimulation was used for IONM with evoked motor potentials. Articles that did not report the presence of complications or adverse effects, those that describe surgical procedures other than cervical spine interventions, those that report on direct transcranial stimulation and transcranial magnetic stimulation, and those carried out in animals were excluded.
Procedure
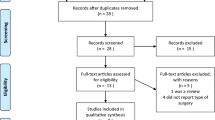
Titles and abstracts were carefully analyzed independently by two investigators and selected as appropriate for inclusion or exclusion. Covidence software (Veritas Health Innovation Covidence systematic review software 2017, available at https://www.covidence.org/home) was used to administer the selection process. Figure 4 is a PRISMA flow chart of the systematic literature review process. Univariate descriptive statistics were carried out using Excel (Microsoft Office, Version 2015) and SPSS (IBM SPSS Statistics for Windows, Version 24.0) programs. The method used to calculate the confidence interval of a proportion is the Wilson score method without continuity correction [27].
Results
The initial search yielded 523 results. Thirteen articles met the inclusion criteria and were carefully reviewed. Seven studies are case series collected retrospectively; two of them are case series [28, 29], three of them are multicenter case series [5, 22, 23], and two are non-systematic reviews of the literature coupled with unpublished anecdotal case reports [7, 21]. Five studies are case reports [28,29,30,31,34]. One study is a prospective study that evaluates a soft bite-lock device [35] (Fig. 4).
Two of the retrospective review articles were eliminated due to the vague description of the data because they included multiple types of surgical interventions and because they included verbal reports of isolated cases [7, 21]. The article evaluating a design was eliminated from this analysis because it is focused on the creation of a device and includes only two cases of minor abrasion of the tongue or lips [35]. The bibliographic data of the ten articles that were analyzed [5, 22, 23, 26,27,28,29,30,31,34] are shown in Table 1.
In these ten articles, 169 complications occurred in 167 patients, out of a total of 38,915 patients studied, which provides an overall prevalence of complications of 0.43% (95% CI 0.37–0.50%). Complications and their global prevalence are shown in Table 2; the most frequent complication was tongue biting in 129 cases (76.3% of complications, prevalence 0.33%, 95% CI 0.28–0.39%). The rarest are the potentially serious ones: a case of cardiac arrhythmia (0.6% of complications, prevalence of 0.003%, 95% CI 0.000–0.015%), a case of bradycardia (prevalence of 0.003%, 95% CI 0.000–0.015%), and a seizure (prevalence of 0.003%, CI 95% 0.000–0.015%).
In two cases, the complication was attributed to local irritation of the electrodes: one case of hair loss (prevalence of 0.003%, 95% CI 0.000–0.015%), and one case of nasal bleeding (prevalence of 0.003%, CI 95% 0.000–0.015%). The argumentative cause of the complications is expressed in Table 3; in 97% of cases, the cause is a muscle contracture produced by transcranial electrical stimulation.
Discussion
IONM is a discipline in constant evolution that allows identifying damage to nerve structures in reversible stages [36], and that includes several techniques; for spine surgery, EMG, MEP, somatosensory evoked potentials, and TES-MEP monitoring is commonly used IONM [37].
Iatrogenic neurological injuries produced during cervical spinal surgery have an estimated prevalence of 0.25–1.75% [37]. Despite the low prevalence, the appearance of these lesions can be devastating for the patient, their families, and for the surgeons [1,2,3,4,5]. Monitoring with TES-MEP is considered safe and valuable in preventing complications in vertebral surgical procedures [1,2,3,4,5, 9, 13, 14, 38]. These data have led to the adoption of neurophysiological monitoring as a recommendation and standard treatment practice in many centers around the world dealing with severe spinal disorders in which surgical procedures could lead to damage of neural structures [39, 40], it however, may be of limited value in routine, non-traumatic or non-severe deformity cases [41], since some authors consider that its utility, a least in anterior cervical decompression and fusion remains a topic of debate [41]. The ideal intraoperative neurophysiological monitoring technique should have a very high sensitivity (a low false-negative rate) and high specificity (a low false-positive rate), be easy to implement during surgical intervention, its cost should be moderate, and should not produce adverse effects or complications. There is a vast number of papers regarding these three topics, as its briefly illustrated below.
Sutter [42], in a large retrospective and prospective cohort of patients that underwent all-level spine surgery for degenerative, deformative, and neoplastic conditions, found for IOMN, 93% sensitivity, 99.1% specificity, and positive and negative predictive values of 82.3% and 99.7%, respectively. Their prevalence of neurological complications related to the surgical procedure was 4.2%. This work also addresses that the average time for IONM was 5 h and 5 min per patient, which includes an average of 45 min for calibrating baseline data and 15 min for electrode removal, they also registered that an average of 15 min was also required for case preparation and data analysis.
Thirumala [37] has published a concise, systematic review and meta-analysis of 7 neurophysiological monitoring studies in spinal surgery of patients with idiopathic scoliosis and has found mixed results for the detection of complications in the surgical procedure associated with TES-MEP. Overall, Thirumala found a false-positive rate of 5.1% (95% CI 2.7–9.3%), 29.4% false-negative rate (95% CI 16.5–46.6), 70.6% sensitivity (95% CI 53.4–83.5%), 95.9% specificity (95% CI 90.7–97.3%). Although these results indicate that in a third of the cases in which a complication occurs (95% CI 16.5–46.6%), it is not detected by TES-MEP, the cost-effectiveness of neurophysiological monitoring compared to the costs of permanent care associated with paraplegia has led to the routine adoption of the procedure in complex spinal surgery [43].
Pastorelli et al. [38], in a study not included in the one by Thirumala [37], retrospectively reviewed 40 patients who underwent posterior spinal fusion and instrumentation for scoliosis, who underwent monitoring with SEP and TES-MEP. They did not find false negatives in the detection of complications, but they reported 13.8% of false positives. Also, Bhalodia et al. [1] have reviewed the efficacy of TES-MEP undergoing cervical spine surgery and have found a lesion of the C5 root with a prevalence of 5.1%; the sensitivity and specificity they found to detect neurological lesions was 100% and 99%, respectively.
Ney and Kessler [44] have reviewed another aspect of neurophysiological monitoring, the longitudinal costs related to long follow-up outcomes. They found that IONM was significantly associated with increased spending during index admission of $1,229 USD, but significantly decreased spending after 12-months post-discharge of $1615 USD and concluded that IONM “was associated with administrative markers suggesting improved health outcomes after cervical spine surgery without greater costs for the year”.
These data are focused on the accuracy (sensitivity, specificity, and positive and negative predictive values) and cost/benefit of IONM, but regardless of its virtuousness, well-designed longitudinal studies assessing effectiveness of IONM are lacking [44], the accuracy in detecting a possible injury to anatomical structures does not necessarily translates in the possibility of avoiding them; no studies in humans have directly measured the efficacy of operative and/or anesthetic interventions in these cases [45].
As with any diagnostic procedure, the benefits of neurophysiological monitoring in spinal surgery must be evaluated considering the potential risks [14]; the complications related to the neurophysiological monitoring procedure are a less explored topic. Intraoperative monitoring with TES-MEP appears to be highly safe; after an extensive systematic review of the literature, we have found an extremely low prevalence of complications, 0.43% (95% CI 0.37–0.50%).
Most of these complications, which reached 97% in the series reviewed, are traumatic events related to the muscular contraction of the electrical stimulus to induce the registration of motor potentials: bite of the tongue, lips, oral mucosa, fracture, or dental dislocation, which occur with a prevalence of 0.42% (95% CI 0.36–0.49%) and are not complications considered serious by the authors. It is probable that for this reason, they are reported below their true index, as has been suggested [5]; Machii et al. [46] consider that the most common adverse effect in their practice is a moderate headache and postoperative neck pain. The most commonly reported complication in this series is tongue biting, which occurred in 76.3% of complications and has a prevalence of 0.33% (95% CI 0.28–0.39%).
Even though complications are so infrequent, it is recommended to prevent them as much as possible, and for this, the use of bilateral soft bite locks could be routinely used [7, 32, 47], since it has been suggested that rigid ones increase the risk of injuries traumatic injuries to the tongue, lips or teeth [23], or otherwise the use of specially designed anti-bite devices [35]. Hair loss on the scalp and one with a nosebleed, both constitute 1% of complications with a prevalence of 0.01% (95% CI 0.001–0.019%). No fatal complications are documented in this series.
Reported potentially serious or fatal complications are very rare: one case of endotracheal tube rupture during a prolonged operation with the patient in the prone position [30] (0.6% of complications, prevalence 0.003%, 95% CI 0.000–0.015%), one seizure episode [32] (0.6% of complications, prevalence 0.003%, 95% CI 0.000–0.015%), and two cardiac complications: one patient with arrhythmia and one patient with bradycardia [5, 31] (1% of complications, prevalence 0.01%, CI 95% 0.001–0.019%). In the bite-related complications, this systematic review includes a case of a ruptured endotracheal tube [30]. The surgical team, particularly anesthesiologists, must be aware of, and forewarned, that a complication of this type may occur, and have a repair strategy in case it appears with compromising patient positions for emergency re-intubation, for example, patients in supine position with the head fixed on the Mayfield head holder.
Ponder et al. [31], in a case report, reported a 59-year-old man, also with heart disease history, who suffered an episode of acute bradycardia immediately after TES-MEP stimulation. Until this work, Ponder's report is the only one in the reviewed literature that narrates a phenomenon of this nature. They observed that repetitively and invariably, TES was accompanied by a sudden and significant drop in heart rate, which spontaneously returned to normal upon cessation of stimulation, during an anterior cervical discectomy and fusion, which was successfully completed.
The case reported in this study is that of a 58-year-old male patient with no history of heart disease, who suffered a serious, life-threatening complication: bradycardia and asystole on repeated occasions immediately after TES-MEP stimulation, in the prone position, with the head fixed on the Mayfield head holder. There is a case similar to ours in the literature; Morano and Tung [24] have reported a case of bradycardia and asystole that required cardiopulmonary resuscitation in a patient who underwent a craniotomy for a metastatic lesion of the frontal lobe in whom monitoring was carried out with TES-MEP.
Cardiac arrhythmias, bradycardia, and bradycardia followed by asystole are atypical findings associated with TES-MEP. Cardiac arrhythmias must be differentiated from TES artifacts that appear on electrocardiographic monitoring [7, 48]. The cause of cardiac arrhythmias, bradycardia, and asystole associated with TES-MEP stimulation is not known [21, 31, 48]. It is possible that the phenomenon is mediated by vasovagal or optical vagus nerve reflex, due to a combination of inappropriate interactions of the sympathetic and parasympathetic responses that follow TES-MEP [31, 49], or that is mediated by deep-traveling indirect vagal stimulation that stimulates the hypothalamus, brainstem, or autonomic neurons of the reticular formation [7].
Even when uncommon, the serious or potentially fatal complications that may be associated with IONM deserve a special mention, specially related to cases where the severity of the neurological condition is minor, as in the one reported here: the worse outcome in a simple case with radiculopathy, in absence of myelopathy may have been an irreversible cardiac arrest.
There is a growing body of literature against the routine use of IONM during “low-risk” procedures such as cervical decompressions [49,50,52]. The possibility of a serious or potentially fatal complication as the one described in this paper adds to the other two reasons often cited by opponents of IONM for cervical anterior decompression and fusion: increased health care cost and a lack of correlation between IONM abnormalities and postoperative neurological deficits [50]. These arguments may add to the practice of some institutions to avoid “pre-defined list of indications for monitoring”, and decide in which cases to use IONM upon considering each case individually [42].
As occurs in other conditions, in contemporary medicine, all the described possible complications perhaps should be stated in the surgical informed consent, even when it might be considered as hyper‐informing patients ‘just to be safe'” [53], since the informed consent requires that “The physician must provide adequate information, with a minimum being the diagnosis, the procedure with its risks, benefits, and the alternatives” [54].
Conclusions
This systematic review shows that TES-MEP is a safe procedure with a very low prevalence of complications, which does not reach 0.5%. Efforts should be made to prevent bite-related complications by soft bite locks. Evidence does not support a relation between TES-MEP and seizures or heart-rhythm-related complications to emit a prophylaxis statement. To our best knowledge, asystole is reported for the first time as a complication during TES-MEP in cervical spine IONM; therefore, it should be considered in the broad spectrum of associated complications.
References
Bhalodia VM, Schwartz DM, Sestokas AK, Bloomgarden G, Arkins T, Tomak P, Gorelick J, Wijesekera S, Beiner J, Goodrich I (2013) Efficacy of intraoperative monitoring of transcranial electrical stimulation-induced motor evoked potentials and spontaneous electromyography activity to identify acute-versus delayed-onset C-5 nerve root palsy during cervical spine surgery: clinical article. J Neurosurg Spine 19:395–402. https://doi.org/10.3171/2013.6.Spine12355
Hilibrand AS, Schwartz DM, Sethuraman V, Vaccaro AR, Albert TJ (2004) Comparison of transcranial electric motor and somatosensory evoked potential monitoring during cervical spine surgery. J Bone Joint Surg Am 86:1248–1253. https://doi.org/10.2106/00004623-200406000-00018
Kelleher MO, Tan G, Sarjeant R, Fehlings MG (2008) Predictive value of intraoperative neurophysiological monitoring during cervical spine surgery: a prospective analysis of 1055 consecutive patients. J Neurosurg Spine 8:215–221. https://doi.org/10.3171/spi/2008/8/3/215
Schwartz DM, Auerbach JD, Dormans JP, Flynn J, Drummond DS, Bowe JA, Laufer S, Shah SA, Bowen JR, Pizzutillo PD, Jones KJ, Drummond DS (2007) Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Joint Surg Am 89:2440–2449. https://doi.org/10.2106/jbjs.F.01476
Schwartz DM, Sestokas AK, Dormans JP, Vaccaro AR, Hilibrand AS, Flynn JM, Li PM, Shah SA, Welch W, Drummond DS, Albert TJ (2011) Transcranial electric motor evoked potential monitoring during spine surgery: is it safe? Spine (Phila Pa 1976) 36:1046–1049. https://doi.org/10.1097/BRS.0b013e3181ecbe77
Schwartz DM, Sestokas AK, Hilibrand AS, Vaccaro AR, Bose B, Li M, Albert TJ (2006) Neurophysiological identification of position-induced neurologic injury during anterior cervical spine surgery. J Clin Monit Comput 20:437–444. https://doi.org/10.1007/s10877-006-9032-1
Macdonald DB (2006) Intraoperative motor evoked potential monitoring: overview and update. J Clin Monit Comput 20:347–377. https://doi.org/10.1007/s10877-006-9033-0
Kothbauer KF, Novak K (2004) Intraoperative monitoring for tethered cord surgery: an update. Neurosurg Focus 16:E8. https://doi.org/10.3171/foc.2004.16.2.1
Quinones-Hinojosa A, Gulati M, Lyon R, Gupta N, Yingling C (2002) Spinal cord mapping as an adjunct for resection of intramedullary tumors: surgical technique with case illustrations. Neurosurgery 51:1199–1206. https://doi.org/10.1097/00006123-200211000-00015
Shi YB, Binette M, Martin WH, Pearson JM, Hart RA (2003) Electrical stimulation for intraoperative evaluation of thoracic pedicle screw placement. Spine (Phila Pa 1976) 28:595–601. https://doi.org/10.1097/01.Brs.0000049926.43292.93
Di Lazzaro V, Rothwell JC (2014) Corticospinal activity evoked and modulated by non-invasive stimulation of the intact human motor cortex. J Physiol 592:4115–4128. https://doi.org/10.1113/jphysiol.2014.274316
Amassian VE, Stewart M, Quirk GJ, Rosenthal JL (1987) Physiological basis of motor effects of a transient stimulus to cerebral cortex. Neurosurgery 20:74–93
Padberg AM, Thuet ED (2006) Intraoperative electrophysiologic monitoring: considerations for complex spinal surgery. Neurosurg Clin N Am 17(205–226):v. https://doi.org/10.1016/j.nec.2006.05.008
Legatt AD, Emerson RG, Epstein CM, MacDonald DB, Deletis V, Bravo RJ, López JR (2016) ACNS guideline: transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol 33:42–50. https://doi.org/10.1097/wnp.0000000000000253
Merton PA, Morton HB (1980) Stimulation of the cerebral cortex in the intact human subject. Nature 285:227–227. https://doi.org/10.1038/285227a0
Rothwell JC (1991) Physiological studies of electric and magnetic stimulation of the human brain. Electroencephalogr Clin Neurophysiol Suppl 43:29–35
Nitsche MA, Cohen LG, Wassermann EM, Priori A, Lang N, Antal A, Paulus W, Hummel F, Boggio PS, Fregni F, Pascual-Leone A (2008) Transcranial direct current stimulation: state of the art 2008. Brain Stimul 1:206–223. https://doi.org/10.1016/j.brs.2008.06.004
Nitsche MA, Paulus W (2011) Transcranial direct current stimulation–update 2011. Restor Neurol Neurosci 29:463–492. https://doi.org/10.3233/rnn-2011-0618
American Electroencephalographic Society (1994) Guideline eleven: guidelines for intraoperative monitoring of sensory evoked potentials. J Clin Neurophysiol 11:77–87
American Clinical Neurophysiology Society (2006) Guideline 9A: guidelines on evoked potentials. J Clin Neurophysiol 23:125–137. https://doi.org/10.1097/00004691-200604000-00010
MacDonald DB (2002) Safety of intraoperative transcranial electrical stimulation motor evoked potential monitoring. J Clin Neurophysiol 19:416–429. https://doi.org/10.1097/00004691-200210000-00005
Tamkus A, Rice K (2012) The incidence of bite injuries associated with transcranial motor-evoked potential monitoring. Anesth Analg 115:663–667. https://doi.org/10.1213/ANE.0b013e3182542331
Yoshida G, Imagama S, Kawabata S, Yamada K, Kanchiku T, Fujiwara Y, Tadokoro N, Takahashi M, Wada K, Yamamoto N, Ushirozako H, Kobayashi K, Yasuda A, Ando M, Tani T, Matsuyama Y (2019) Adverse events related to transcranial electric stimulation for motor-evoked potential monitoring in high-risk spinal surgery. Spine (Phila Pa 1976) 44:1435–1440. https://doi.org/10.1097/brs.0000000000003115
Morano JM, Tung A (2019) Bradycardic arrest during somatosensory-evoked potential monitoring: a case report. A A Pract 13:461–463. https://doi.org/10.1213/xaa.0000000000001123
Meyer S (1941) Grading of patients for surgical procedures. Anesthesiology 2(3):281–284. https://doi.org/10.1097/00000542-194105000-00004
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group PP (2015) Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 4:1. https://doi.org/10.1186/2046-4053-4-1
Newcombe RG (1998) Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med 17:857–872. https://doi.org/10.1002/(sici)1097-0258(19980430)17:8%3c857::aid-sim777%3e3.0.co;2-e
Kuwahara Y, Taguchi S, Kuroda M, Kawamoto M (2011) Adverse events during transcranial muscle evoked potential monitoring. Masui 60:692–696
Yata S, Ida M, Shimotsuji H, Nakagawa Y, Ueda N, Takatani T, Shigematsu H, Motoyama Y, Nakase H, Kirita T, Kawaguchi M (2018) Bite injuries caused by transcranial electrical stimulation motor-evoked potentials’ monitoring: incidence, associated factors, and clinical course. J Anesth 32:844–849. https://doi.org/10.1007/s00540-018-2562-0
Duma A, Novak K, Schramm W (2009) Tube-in-tube emergency airway management after a bitten endotracheal tube caused by repetitive transcranial electrical stimulation during spinal cord surgery. Anesthesiology 111:1155–1157. https://doi.org/10.1097/ALN.0b013e3181b8f694
Ponder BL, Conner TF, Floyd DT, Tao C, Enyia OK (2003) Acute bradycardia as a result of intraoperative transcranial electric motor evoked potential stimulation: a case report. Am J Electroneurodiagn Technol 43:98–104. https://doi.org/10.1080/1086508X.2003.11079424
Davis SF, Altstadt T, Flores R, Kaye A, Oremus G (2013) Report of seizure following intraoperative monitoring of transcranial motor evoked potentials. Ochsner J 13:558–560
Mahmoud M, Spaeth J, Sadhasivam S (2008) Protection of tongue from injuries during transcranial motor-evoked potential monitoring. Paediatr Anaesth 18:902–903. https://doi.org/10.1111/j.1460-9592.2008.02704.x
Davis SF, Kalarickal P, Strickland T (2010) A report of two cases of lip and tongue bite injury associated with transcranial motor evoked potentials. Am J Electroneurodiagn Technol 50:313–320
Oshita K, Saeki N, Kubo T, Abekura H, Tanaka N, Kawamoto M (2016) A novel mouthpiece prevents bite injuries caused by intraoperative transcranial electric motor-evoked potential monitoring. J Anesth 30:850–854. https://doi.org/10.1007/s00540-016-2220-3
Gonzalez AA, Jeyanandarajan D, Hansen C, Zada G, Hsieh PC (2009) Intraoperative neurophysiological monitoring during spine surgery: a review. Neurosurg Focus 27:E6. https://doi.org/10.3171/2009.8.Focus09150
Thirumala PD, Huang J, Thiagarajan K, Cheng H, Balzer J, Crammond DJ (2016) Diagnostic accuracy of combined multimodality somatosensory evoked potential and transcranial motor evoked potential intraoperative monitoring in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 41:1177–1184. https://doi.org/10.1097/brs.0000000000001678
Pastorelli F, Di Silvestre M, Vommaro F, Maredi E, Morigi A, Bacchin MR, Bonarelli S, Plasmati R, Michelucci R, Greggi T (2015) Intraoperative monitoring of somatosensory (SSEPs) and transcranial electric motor-evoked potentials (tce-MEPs) during surgical correction of neuromuscular scoliosis in patients with central or peripheral nervous system diseases. Eur Spine J 24(Suppl 7):931–936. https://doi.org/10.1007/s00586-015-4282-6
Sutter M, Deletis V, Dvorak J, Eggspuehler A, Grob D, Macdonald D, Mueller A, Sala F, Tamaki T (2007) Current opinions and recommendations on multimodal intraoperative monitoring during spine surgeries. Eur Spine J 16(Suppl 2):S232-237. https://doi.org/10.1007/s00586-007-0421-z
Bhagat S, Durst A, Grover H, Blake J, Lutchman L, Rai AS, Crawford R (2015) An evaluation of multimodal spinal cord monitoring in scoliosis surgery: a single centre experience of 354 operations. Eur Spine J 24:1399–1407. https://doi.org/10.1007/s00586-015-3766-8
Lee HJ, Kim IS, Sung JH, Lee SW, Hong JT (2016) Significance of multimodal intraoperative monitoring for the posterior cervical spine surgery. Clin Neurol Neurosurg 143:9–14. https://doi.org/10.1016/j.clineuro.2016.02.007
Sutter M, Eggspuehler A, Jeszenszky D, Kleinstueck F, Fekete TF, Haschtmann D, Porchet F, Dvorak J (2019) The impact and value of uni- and multimodal intraoperative neurophysiological monitoring (IONM) on neurological complications during spine surgery: a prospective study of 2728 patients. Eur Spine J 28:599–610. https://doi.org/10.1007/s00586-018-5861-0
Buckwalter JA, Yaszay B, Ilgenfritz RM, Bastrom TP, Newton PO (2013) Analysis of intraoperative neuromonitoring events during spinal corrective surgery for idiopathic scoliosis. Spine Deform 1:434–438. https://doi.org/10.1016/j.jspd.2013.09.001
Ney JP, Kessler DP (2018) Neurophysiological monitoring during cervical spine surgeries: longitudinal costs and outcomes. Clin Neurophysiol 129:2245–2251. https://doi.org/10.1016/j.clinph.2018.08.002
Scibilia A, Terranova C, Rizzo V, Raffa G, Morelli A, Esposito F, Mallamace R, Buda G, Conti A, Quartarone A, Germanò A (2016) Intraoperative neurophysiological mapping and monitoring in spinal tumor surgery: sirens or indispensable tools? Neurosurg focus 41:E18. https://doi.org/10.3171/2016.5.focus16141
Machii K, Cohen D, Ramos-Estebanez C, Pascual-Leone A (2006) Safety of rTMS to non-motor cortical areas in healthy participants and patients. Clin Neurophysiol 117:455–471. https://doi.org/10.1016/j.clinph.2005.10.014
Deiner SG, Osborn IP (2009) Prevention of airway injury during spine surgery: rethinking bite blocks. J Neurosurg Anesthesiol 21:68–69. https://doi.org/10.1097/ANA.0b013e31818d205e
MacDonald DB, Deletis V (2008) Safety issues during surgical monitoring. Handb Clin Neurophysiol 8:882–898
Pereiro L (1996) Practical procedures. Update Anesthesia 6:1
Ajiboye RM, D’Oro A, Ashana AO, Buerba RA, Lord EL, Buser Z, Wang JC, Pourtaheri S (2017) Routine use of intraoperative neuromonitoring during ACDFs for the treatment of spondylotic myelopathy and radiculopathy is questionable: a review of 15,395 cases. Spine 42:14–19. https://doi.org/10.1097/brs.0000000000001662
Cole T, Veeravagu A, Zhang M, Li A, Ratliff JK (2014) Intraoperative neuromonitoring in single-level spinal procedures: a retrospective propensity score-matched analysis in a national longitudinal database. Spine 39:1950–1959. https://doi.org/10.1097/brs.0000000000000593
Lee JY, Hilibrand AS, Lim MR, Zavatsky J, Zeiller S, Schwartz DM, Vaccaro AR, Anderson DG, Albert TJ (2006) Characterization of neurophysiologic alerts during anterior cervical spine surgery. Spine 31:1916–1922. https://doi.org/10.1097/01.brs.0000228724.01795.a2
Schmitz D, Reinacher PC (2006) Informed consent in neurosurgery–translating ethical theory into action. J Med Ethics 32:497–498. https://doi.org/10.1136/jme.2005.013144
Cocanour CS (2017) Informed consent-It’s more than a signature on a piece of paper. Am J Surg 214:993–997. https://doi.org/10.1016/j.amjsurg.2017.09.015
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Revilla-Pacheco, F., Watanabe, S., Rodríguez-Reyes, J. et al. Transcranial electric stimulation motor evoked potentials for cervical spine intraoperative monitoring complications: systematic review and illustrative case of cardiac arrest. Eur Spine J 31, 2723–2732 (2022). https://doi.org/10.1007/s00586-022-07297-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07297-6