Abstract
Purpose
To determine predictors of failure to achieve minimal clinical important difference (MCID) for pain and disability at discharge after mechanical diagnosis and therapy (MDT)-based multimodal rehabilitation for neck pain (NP).
Methods
Pre- and post-treatment numerical pain rating scale (NPRS) and neck disability index (NDI) in patients with mechanical NP were analysed in this retrospective study. Multivariate analysis was performed to investigate the effect of covariates such as age, gender, lifestyle, body mass index, presentation, diabetes, osteoporosis, response to repeated movement testing, treatment sessions, compliance rate, and pre-treatment NPRS and NDI scores on failure to achieve MCID of ≥ 30% for NPRS and NDI scores post-treatment.
Results
In the 4998 patients analysed for this study, 7% and 14.5% of patients failed to achieve MCID for NPRS and NDI scores, respectively, at the end of treatment. Age > 70 years, diabetes, osteoporosis, partial or non-response to repeated movements, lesser treatment sessions, and lower compliance rate were associated with increased risk for failure to achieve MCID for NPRS and NDI scores. A higher pre-treatment NDI score was associated with failure to achieve MCID for NPRS score, whereas lower pre-treatment NPRS and NDI scores were associated with failure to achieve MCID for NDI score.
Conclusion
Although MDT-based multimodal rehabilitation helped to achieve significant reduction in pain and disability in mechanical NP, several baseline risk factors were associated with failure to achieve MCID for pain and disability after treatment. Identifying and modifying these factors as part of rehabilitation treatment may help to achieve better outcomes in mechanical NP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite high prevalence and the socio-economic burden due to the associated pain and disability, neck pain (NP) receives much less attention when compared to low back pain (LBP) [1, 2]. The most common cause of NP is mechanical NP which is associated with long-standing poor posture and reduction in function and strength of cervical muscles [3, 4]. Although several rehabilitation treatment modalities are commonly employed, there is no consensus regarding the most effective management strategies for mechanical NP. Several reports have supported the use of a combination of different physical therapy modalities in the treatment of mechanical NP [5]. A recent trial by Domingues et al. [6] reported that a combination of manual therapy and exercises was more effective than usual care in improving disability and pain in patients with non-specific chronic NP.
Although mechanical diagnosis and treatment (MDT)-based treatment has been reported to be effective and superior to other interventions such as manual therapy and exercises for chronic LBP [7], few reports have studied the effect of MDT on NP. A systematic review of 5 trials by Takasaki and May et al. [8] reported that although MDT may improve pain than ‘wait and see’ or other treatment approaches such as strengthening exercises and cognitive behaviour therapy, the difference in effect may not be clinically important and that MDT does not have a greater effect on disability than ‘wait and see’ or other treatment approaches. Although centralisation of pain on repeated movement testing and patient age have been reported as an important prognostic factors affecting outcomes after MDT in patients with LBP [9, 10], studies have not reported prognostic factors affecting outcomes in patients treated with MDT for NP, especially as part of a multimodal rehabilitation program.
Baseline variables can help to predict treatment outcomes in patients undergoing rehabilitation treatment for NP and several prognostic factors can affect outcomes after treatment. Improvement in pain and functional ability in the short term (at the end of treatment) is perceived by patients as a sign of improvement in their spine condition, and is a useful indicator of clinical outcomes as a direct effect of the treatment intervention [11, 12]. Furthermore, a minimal clinical important difference (MCID) between the pre- and post-treatment outcome variables is recommended to identify patients who achieved a clinically significant improvement with rehabilitation treatment for spine pain [13, 14].
Hence, the aim of the present study was to determine the predictors of failure to achieve an MCID for pain and disability at the end of an MDT-based multimodal rehabilitation treatment for mechanical NP.
Materials and methods
Study design
In this retrospective study, electronic records of routinely collected clinical data of patients treated with physical rehabilitation for NP from 2016 to Dec 2020 at a chain of outpatient spine rehabilitation clinics (QI Spine Clinic, India) were analysed. This study was approved by an Institutional Review Board and Ethics Committee, and informed consent was taken from all patients at the start of treatment regarding the use of their anonymized demographic and clinical data for research.
Study participants
The inclusion criteria were all patients > 20 years of age presenting with NP who underwent rehabilitation treatment at our clinics. The exclusion criteria were patients with red flags conditions (tumour, infection, fracture, and instability), inflammatory NP (rheumatoid arthritis, spondyloarthropathy), cervical myelopathy or cord compression, patients with incomplete clinical records, and patients who took < 6 sessions or > 36 sessions of treatment at the centre. Patients who did not complete a minimum of 6 treatment sessions were excluded. Similarly, patients who underwent treatment of > 36 sessions were excluded to minimize the possibility that improvement in NP and function was due to time rather than a direct effect of the rehabilitation treatment. Mechanical NP was defined as pain which arose from the cervical spine or its surrounding soft-tissue structures, often showed improvement with rest, and aggravated during specific neck movements or activities [15]. Non-mechanical NP secondary to inflammatory condition (e.g. rheumatoid arthritis or spondyloarthropathies) or any red flag condition (e.g. infection, tumour, and fractures) were ruled out during first consultation based on history and presentation, clinical examination, and investigations (radiological and blood) wherever available.
Demographic data including age, gender, body mass index (BMI), lifestyle, and history of diabetes and osteoporosis were collected at the time of the first consultation. Lifestyle was categorised as sedentary if it involved prolonged sitting at work, during leisure time and lack of physical activity/exercise or movement during most part of the day; as active if there was daily moderate-to-vigorous physical activities as per the American College of Sports Medicine (ACSM) recommendations [16, 17]; and as semi-active if the lifestyle was more active than sedentary but did not involve performing daily moderate-to vigorous physical activities. Based on the presentation, patients with mechanical NP were categorised into “central NP with or without above elbow pain” (along the extent of the cervical spine posteriorly with or without pain radiating along the trapezius and into the arm till the elbow) similar to the “above elbow derangement” subgroup used in the MDT classification, and “central NP with below elbow pain” (along the extent of the cervical spine posteriorly with pain radiating into the upper limb below the elbow) similar to the “below elbow derangement” subgroup used in the MDT classification.
All patients were clinically examined for head and neck posture, cervical spine range of motion, motor and sensory function (myotomal and dermatomal loss) by a physiotherapist in the clinic. Repeated movement testing was performed using the MDT method to determine directional preference and response [18]. Before and at the end of treatment, NP intensity was measured using the numerical pain rating scale (NPRS), with pain intensity ranging from “0” (no pain) to “10” (worst pain imaginable), and functional disability was measured using the Neck Disability Index (NDI) [19, 20]. The total duration of treatment (in days) was also derived from the records for all patients.
Rehabilitation protocol
An MDT-based multimodal rehabilitation protocol using a combination of patient education, pain management with mechanical diagnosis and treatment (MDT)-based directional movements [18] and adjuvant frequency-specific microcurrents (FSM) application [21], and strengthening and stabilisation of cervical and upper back muscles were used in all patients. All treatment was provided by senior spine physiotherapists at each clinic who had undergone internal training in the MDT-based multimodal rehabilitation protocol conducted by a central team. The central team consisted of a clinic director and a national clinical expert (both with > 10 years of experience in spine rehabilitation) who were trained in the MDT technique and had a certified diploma from the McKenzie Institute International® (Paraparaumu, New Zealand). The internal training program was designed and delivered by these MDT-certified professionals and involved training all physiotherapists within the system on the multimodal rehabilitation treatment protocol. After the initial training, all physiotherapists underwent continued education training and internal assessment by the central team to qualify for promotion to senior positions within the system. Furthermore, an internal referral or escalation system was part of our clinical care delivery system where senior physiotherapists at each clinic can refer/escalate patients (who were non-responders or slow responders) to their clinic heads or the central team to confirm the MDT diagnosis and treatment technique being followed for the patient.
Patient education involved information on avoiding pain-aggravating neck movements, postures and activities, and ways of self-care at home during the course of treatment. Pain management was done using MDT-based repeated directional movements and adjuvant FSM application. The FSM modality involved application of low-voltage pulsed microamperage (one millionth of ampere) current generated by an FSM unit and delivered using 4 leads applied around the cervical spine (one on the posterior aspect of the neck on midline, one on either shoulder, and one on the upper back midline) [21]. This was administered to patients with higher baseline pain intensity (NPRS score > 3). Previous studies have reported the efficacy of FSM as an adjuvant for pain management in spine and musculoskeletal pain [22,23,24,25]. Based on the directional preference and response, patients were instructed to perform directional movements under the supervision of the treating physiotherapist, which was to be repeated at home at regular intervals. At home, patients were asked to repeat their directional preference movements 4–5 times a day (10 repetitions per session). Patients were asked to avoid or discontinue the movement if it aggravated or peripheralized their pain (i.e. symptoms migrating away from the midline of the body and towards the upper limb or from a proximal to distal direction in the upper limb) and inform their therapist. Once the pain reduced to mild (NPRS score ≤ 3), paraspinal muscle strength and spine mobility were assessed using a pressure biofeedback cuff and cervical goniometer and the patient was put on a customised strengthening and stabilisation exercise regimen. For patients without a directional preference (non-responders), pain was managed using FSM application, and strengthening and stabilisation exercises were initiated early and gradually progressed from basic to intermediate to advanced intensity of exercises based on patient response and tolerance. All patients were advised to undergo a minimum of 6 supervised rehabilitation sessions at the clinic. Patients included in the study took anywhere between 6 and 36 treatment sessions. The number of sessions done by the patient was decided by the treating physiotherapist or by the clinic head or central team (during escalation) based on baseline pain and disability, response to repeated movement testing, and progress in improvement from baseline pain and disability levels during the treatment. Hence, patients with higher baseline disability, partial or non-response to repeated movement testing, and slower progression in improvement of pain and disability during the treatment were prescribed more number of treatment sessions and had a longer treatment duration.
Study outcome variables
Our chain of outpatient spine rehabilitation clinics used a dedicated EMR software where treating physiotherapists were required to enter pre- and post-treatment NPRS and NDI scores for all patients who underwent treatment at our clinics. Furthermore, a clinic head (who was a senior physiotherapist in charge of the clinic) and a central team performed frequent reviews of patient records and ensured that patient information such as demographic, clinical presentation, response to MDT testing, treatment, and pain (NPRS score) and disability (NDI score) outcome details were complete before the discharge of the patient.
Pre- and post-treatment (at the time of discharge) NRPS and NDI scores were collected in all patients. The NPRS and NDI scores were collected from all patients using self-administered scales in the clinic before the consultation (pre-treatment) and at the time of discharge or end of treatment (post-treatment). To determine significant change in NPRS and NDI scores at the end of treatment, an MCID between pre-and post-treatment NPRS and NDI scores were calculated. Based on the recommendations by Ostelo et al. [10], MCID threshold was set at ≥ 30% improvement from baseline or pre-treatment NPRS and NDI scores. Based on the NPRS score, patients were categorised into 3 subgroups (≤ 3, 4–7, > 7), and based on NDI score into 4 subgroups (minimal, moderate, severe, crippled/bed-bound). Treatment compliance rate was calculated as the percentage of treatment sessions completed out of their prescribed total treatment sessions. Patients who attended less than 80% of their treatment sessions were termed as non-compliant to the treatment. The primary treatment outcomes in this study were MCID of ≥ 30% improvement for NPRS and NDI scores from pre-treatment values at the end of treatment, whereas the secondary treatment outcomes were NPRS and NDI scores at the end of treatment.
Statistical analysis
Demographic data including age, gender, body mass index (BMI), lifestyle, prevalence of diabetes and osteoporosis, response to repeated movements, number of treatment sessions, and treatment duration were analysed. Percentage of patients who achieved MCID of ≥ 30% for NPRS and NDI after treatment were calculated using pre- and post-treatment NPRS and NDI scores. Categorical data were compared using the Fisher’s test or Chi-square test and continuous data using the two-way analysis of variance (ANOVA) or Kruskal–Wallis test (for not normal distributed or ordinal data). For the univariate logistic regression analysis, pre-treatment variables were sub grouped and the percentage of patients who achieved MCID for NPRS and NDI after treatment were compared between subgroups for each variable using Chi-square test. The pre-treatment variables which were sub grouped included gender (male and female), age (< 30, 30–49, 50–69, and ≥ 70 years), BMI (< 25, 25.0–29.9, and ≥ 30 kg/m2), lifestyle (sedentary and active/semi-active), diabetes (yes and no), osteoporosis (yes and no), clinical presentation (central NP with or without above elbow pain and central NP with below elbow pain), response to repeated movements (responder, partial responder, and non-responder), number of treatment sessions (6, 7–12, 13–18, and > 18), treatment compliance rate (< 80% and ≥ 80%), pre-treatment NPRS score (≤ 3, 4–7, and > 7), and pre-treatment NDI score (≤ 20, > 20–40, > 40–60, and > 60). Pre-treatment variables which were found to be significant on univariate logistic regression analysis were included in a multivariate logistic regression analysis to determine odd’s ratio for these variables as risk factors for not achieving the ≥ 30% MCID for post-treatment NPRS and NDI scores. An Odds ratio (OR) > 1 indicated a higher probability of not achieving MCID, and an OR < 1 indicated a lower probability of not achieving MCID or higher probability of achieving MCID for NPRS and NDI scores. A p-value of < 0.05 was considered significant. Statistical analysis was performed using the SPSS (ver. 20.0) statistical analysis software (SPSS Science Inc, Chicago, IL).
Results
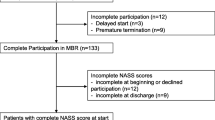
Based on the inclusion criteria, a total of 6402 patients with NP underwent rehabilitation treatment at our clinics. Based on the exclusion criteria, 421 patients were excluded due to red flag conditions, cord compression, or inflammatory NP and 5981 patients were treated for mechanical NP. In patients with mechanical NP, 915 patients either completed < 6 or > 36 sessions, and 68 patients took telerehabilitation treatment. Therefore, data from 4998 patients with NP who underwent in-clinic multimodal rehabilitation treatment were analysed for this study. The patients analysed included 2698 males and 2300 females with a mean age of 46.1 ± 13.3 years who took a mean 15 ± 7 treatment sessions at a mean treatment (or follow-up) duration of 84.5 ± 107 days. The MCID for NPRS score was achieved in 93% of patients, and for NDI score was achieved in 85.5% of patients at the end of treatment. The mean treatment of 15 ± 7 sessions was done in patient group which achieved MCID for NPRS and NDI was significantly higher (p < 0.0001) when compared to the mean treatment of 11 ± 5 sessions done in the patient group which did not achieve MCID for NPRS and NDI. The baseline characteristics of patients in this study are summarised in Table 1
Univariate analysis of MCID achieved for NPRS and NDI scores
The MCID achieved for NPRS score at the end of treatment were significantly higher in younger patients (p < 0.0001), in patients without diabetes (p = 0.02) and osteoporosis (p = 0.002), among responders to repeated movement testing (p < 0.0001), among patients with pre-treatment NPRS score 4–7 (p = 0.01), among patients with pre-treatment NDI score < 40 (p < 0.0001), among patients who did higher number of treatment sessions (p < 0.0001), and among patients with compliance rate of ≥ 80% (p < 0.0001) (Table 2). However, there were no significant difference when subgroups were compared based on gender, BMI, lifestyle, and presentation.
Similarly, the MCID achieved for NDI score at the end of treatment were significantly higher in younger patients (p < 0.0001), in patients without diabetes and osteoporosis (p < 0.0001), among responders to repeated movement testing (p < 0.0001), among patients with pre-treatment NPRS score 4–7 (p = 0.01), among patients with pre-treatment NDI score > 20 (p < 0.0001), among patients who did higher number of treatment sessions (p < 0.0001), and among patients with compliance rate of ≥ 80% (p < 0.0001) (Table 2). However, there were no significant difference when subgroups were compared based on gender, BMI, lifestyle, and presentation.
Predictors of failure to achieve MCID for post-treatment NPRS and NDI scores
Multivariate analysis showed that age > 70 years, diabetes, osteoporosis, partial or non-response to repeated movement testing, lesser number of treatment sessions, lower compliance rate, and higher pre-treatment NDI score were associated with increased risk for failure to achieve MCID for NPRS score after treatment (Table 3). Similarly, age > 70 years, diabetes, osteoporosis, partial or non-response to repeated movement testing, lesser number of treatment sessions, lower compliance rate, and lower pre-treatment NPRS and NDI scores were associated with increased risk for failure to achieve MCID for NDI score after treatment (Table 3).
Discussion
The results of this study showed that 7% of patients failed to achieve MCID of ≥ 30% for NPRS score, whereas 14.5% of patients failed to achieve MCID of ≥ 30% for NDI score at the end of treatment. Age > 70 years, diabetes, osteoporosis, partial or non-response to repeated movement testing, lesser number of treatment sessions, and lower compliance rate were associated with increased risk for failure to achieve MCID for NPRS and NDI scores after treatment. A higher pre-treatment NDI score was associated with increased risk for failure to achieve MCID for NPRS score after treatment, whereas lower pre-treatment NPRS and NDI scores were associated with increased risk for failure to achieve MCID for NDI score after treatment.
The effect of pre-treatment or baseline NPRS and NDI scores on treatment outcome in NP is unclear with contrary findings in the literature. De Pauw et al. [26] in a retrospective analysis of 437 patients with chronic NP treated with multimodal treatment (back school education and exercise therapy), reported that a high NDI score, high NRS score for radicular pain in the upper extremities, a low NRS score for NP, and history of trauma decreased the odds of patient responding to the given treatment. However, Bohman et al. [27], in a longitudinal cohort study of 89 women with chronic, non-specific NP, reported increasing age and lower baseline neck disability as important predictors associated with poor short- and long-term improvement after 11 weeks of physiotherapy interventions (coordination exercise, strength training and massage) similar to our study. A possible explanation for our finding of lower pre-treatment NPRS and NDI scores associated with risk for failure to achieve MCID for NDI could be due to difference in study population demography (larger patient numbers, lower mean age, gender ratio, type of treatment administered) and other confounding factors such as duration of pain, episodes of recurrence, cervical active ROM, and baseline mental health which may have significantly affected post-treatment disability [27, 28].
Our results were in accordance with the findings of previously published studies regarding the effect of risk factors such as number of treatment sessions [29], and response to repeated movement testing [30] on treatment outcome. Although diabetes mellitus and osteoporosis have been associated with increased incidence of NP [31, 32], their effect as risk factors for treatment outcomes has seldom been analysed. Weigl et al. [28], in a prospective cohort study of 112 patients with chronic NP treated with multidisciplinary rehabilitation, reported no correlation between co-morbidities and treatment outcome. However, our results indicate that the presence of baseline diabetes and osteoporosis were risk factors for failure to achieve MCID for pain and disability. Diabetes can negatively alter the structural composition and mechanical properties of the intervertebral disc increasing susceptibility to disc prolapse [31], whereas osteoporosis can aggravate degenerative changes in the cervical spine, especially with increasing age, in patients with NP [32].
To the best of our knowledge, the current study is the largest study which determined predictors of MCID for pain and disability after an MDT-based multimodal rehabilitation treatment and the first study to evaluate the association between diabetes, osteoporosis, number of treatment sessions, and treatment compliance on treatment outcome. However, there are some limitations to this study. First, the retrospective study design had its inherent limitations and biases such as selection bias. Second, predictors of failure to achieve minimal clinical important difference were analysed at the end of a mean treatment duration of 3 months in the current study and not for longer duration of 6 and 12 months. However, previous studies have reported that predictors of treatment outcome at the end of treatment were similar to factors which affected treatment outcomes after 6 and 12 months [26,27,28]. Third, at-home self-treatment compliance for the patient of the prescribed MDT-based repeated movements, an integrated part of the MDT technique, maybe an important factor which may influence MCID and has been not been factored in in this study. Fourth, the duration of the pain or the disability was not used for analysis in the current study. Patients presented at our clinic with a wide variety of self-reported patterns of symptom duration which included acute mild, acute severe, chronic mild, chronic severe, acute aggravation of chronic pain, subacute pain, episodic pain, and recurrent pain. Furthermore, pain duration may change with the use of pain medications or activity modification done before presentation at our clinic. Therefore we avoided subgrouping our patients into the broad categories of acute, subacute, chronic NP based on symptom duration as it may have not represented the actual clinical course of their NP. Hence we focused on the characteristics of the current pain episode in terms of pain intensity and disability and classified them into mechanical or non-mechanical NP from a pathological point of view and as responders or non-responders to repeated movement testing for mechanical NP. Therefore, the results of our study are applicable to mechanical NP with or without a response to repeated movement testing and the effect of treatment based on baseline pain intensity and disability rather than to NP categorised as acute, subacute, or chronic. Lastly, while the current study has included several variables, including diabetes, osteoporosis, number of treatment sessions, and compliance rate in the model, there may still be other factors such as tobacco use, and psychosocial factors that could help predict the outcome more precisely and needs to be included in the future studies.
Conclusion
In conclusion, age > 70 years, diabetes, osteoporosis, partial or non-response to repeated movement testing, lesser number of treatment sessions, and lower compliance rate, were associated with increased risk for failure to achieve MCID for NPRS and NDI scores after treatment. A higher pre-treatment NDI score was associated with failure to achieve MCID for NPRS score, and lower pre-treatment NPRS and NDI scores were associated with failure to achieve MCID for NDI score. Identifying and addressing some of the modifiable risk factors as part of rehabilitation treatment may help achieve better outcomes in mechanical NP.
Data availability
All data and material related to the current study are available from the corresponding author on reasonable request.
References
Safiri S, Kolahi AA, Hoy D, Buchbinder R, Mansournia MA, Bettampadi D, Ashrafi-Asgarabad A, Almasi-Hashiani A, Smith E, Sepidarkish M, Cross M, Qorbani M, Moradi-Lakeh M, Woolf AD, March L, Collins G, Ferreira ML (2020) Global, regional, and national burden of neck pain in the general population, 1990–2017: systematic analysis of the global burden of disease study 2017. BMJ 368:m791. https://doi.org/10.1136/bmj.m791
Cohen SP, Hooten WM (2017) Advances in the diagnosis and management of neck pain. BMJ 358:j3221. https://doi.org/10.1136/bmj.j3221
Jun D, Zoe M, Johnston V, O’Leary S (2017) Physical risk factors for developing non-specific neck pain in office workers: a systematic review and meta-analysis. Int Arch Occup Environ Health 90:373–410. https://doi.org/10.1007/s00420-017-1205-3
Hogg-Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, Côté P, Haldeman S, Ammendolia C, Carragee E, Hurwitz E, Nordin M, Peloso P (2008) The burden and determinants of neck pain in general population: results of the bone and joint decade 2000–2010 task force on neck pain and it associated disorders. Spine 33:S39–S51. https://doi.org/10.1016/j.jmpt.2008.11.010
Martin-Gomez C, Sestelo-Diaz R, Carrillo-Sanjuan V, Navarro-Santana MJ, Bardon-Romero J, Plaza-Manzano G (2019) Motor control using cranio-cervical flexion exercises versus other treatments for non-specific chronic neck pain: a systematic review and meta-analysis. Musculoskelet Sci Pract 42:52–59. https://doi.org/10.1016/j.msksp.2019.04.010
Domingues L, Pimentel-Santos FM, Cruz EB, Sousa AC, Santos A, Cordovil A, Correia A, Torres LS, Silva A, Branco PS, Branco JC (2019) Is a combined programme of manual therapy and exercise more effective than usual care in patients with non-specific chronic neck pain? A randomized controlled trial. Clin Rehabil 33:1908–1918. https://doi.org/10.1177/0269215519876675
Lam OT, Strenger DM, Chan-Fee M, Pham PT, Preuss RA, Robbins SM (2018) Effectiveness of the McKenzie method of mechanical diagnosis and therapy for treating low back pain: literature review with meta-analysis. J Orthop Sports Phys Ther 48:476–490. https://doi.org/10.2519/jospt.2018.7562
Takasaki H, May S (2014) Mechanical diagnosis and therapy has similar effects on pain and disability as ‘wait and see’ and other approaches in people with neck pain: a systematic review. J Physiother 60:78–84. https://doi.org/10.1016/j.jphys.2014.05.006
Long A, May S, Fung T (2008) The comparative prognostic value of directional preference and centralization: a useful tool for front-line clinicians? J Man Manip Ther 16:248–254. https://doi.org/10.1179/106698108790818332
Petersen T, Christensen R, Juhl C (2015) Predicting a clinically important outcome in patients with low back pain following McKenzie therapy or spinal manipulation: a stratified analysis in a randomized controlled trial. BMC Musculoskelet Disord. https://doi.org/10.1186/s12891-015-0526-1
Beattie PF, Silfies SP, Jordon M (2016) The evolving role of physical therapists in the long-term management of chronic low back pain: longitudinal care using assisted self-management strategies. Braz J Phys Ther 20:580–591. https://doi.org/10.1590/bjpt-rbf.2014.0180
Setchell J, Costa N, Ferreira M, Hodges PW (2019) What decreases low back pain? A qualitative study of patient perspectives. Scand J Pain 19:597–603. https://doi.org/10.1515/sjpain-2019-0018
Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, Bouter LM, de Vet HC (2008) Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 33:90–94. https://doi.org/10.1097/BRS.0b013e31815e3a10
Pires D, Cruz E, Canhão H, Nunes C (2020) Minimum important change values for pain and disability: which is the best to identify a meaningful response in patients with chronic nonspecific low back pain? Physiother Theory Pract. https://doi.org/10.1080/09593985.2020.1843210
Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, Sopky BJ, Godges JJ, Flynn TW, Association APT (2008) Neck pain: clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopedic section of the american physical therapy association. J Orthop Sports Phys Ther 38:A1–A34. https://doi.org/10.2519/jospt.2008.0303
Locke CT, Craig CL, Thyfault JP, Spence JC (2013) A step defined sedentary lifestyle index <5000 steps/day. Appl Physiol Nutr Metab 38(2):100–114. https://doi.org/10.1139/apnm-2012-0235
Oja P, Titze S (2011) Physical activity recommendations for public health: development and policy context. EPMA J 2(3):253–259. https://doi.org/10.1007/s13167-011-0090-1
McKenzie R, May S (2003) The Cervical and thoracic spine: mechanical diagnosis and therapy, 2nd edn. Spinal Publications, Wellington
Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 30:1331–1334. https://doi.org/10.1097/01.brs.0000164099.92112.29
Vernon H (2008) The neck disability index: state-of-the-art, 1991–2008. J Manip Physiol Ther 31:491–502. https://doi.org/10.1016/j.jmpt.2008.08.006
McMakin CR (2011) Frequency specific microcurrent in pain management. Churchill Livingstone-Elsevier, Philadelphia
Alexander R, Ole H, Natalia CB, Susanne MW, Alexander C, Martin B (2020) Microcurrent therapy in the treatment of knee osteoarthritis: could it be more than a placebo effect? A randomized controlled trial. Eur J Phys Rehabil Med. https://doi.org/10.23736/S1973-9087.20.05921-3
Koopman JSHA, Vrinten DH, van Wijck AJM (2009) Efficacy of microcurrent therapy in the treatment of chronic nonspecific back pain: a pilot study. Clin J Pain 25(6):495–499. https://doi.org/10.1097/AJP.0b013e31819a6f3e
Saranya B, Ahmed J, Shenoy N, Ongole R, Sujir N, Natarajan S (2019) Comparison of transcutaneous electric nerve stimulation (TENS) and microcurrent nerve stimulation (MENS) in the management of masticatory muscle pain: a comparative study. Pain Res Manag 2019:1–5. https://doi.org/10.1155/2019/8291624
Shetty GM, Rawat P, Sharma A (2020) Effect of adjuvant frequency-specific microcurrents on pain and disability in patients treated with physical rehabilitation for neck and low back pain. J Bodyw Mov Ther 24(4):168–175. https://doi.org/10.1016/j.jbmt.2020.07.013
De Pauw R, Kregel J, De Blaiser C, Van Akeleyen J, Logghe T, Danneels L, Cagnie B (2015) Identifying prognostic factors predicting outcome in patients with chronic neck pain after multimodal treatment: a retrospective study. Man Ther 20:592–597. https://doi.org/10.1016/j.math.2015.02.001
Bohman T, Bottai M, Björklund M (2019) Predictive models for short-term and long-term improvement in women under physiotherapy for chronic disabling neck pain: a longitudinal cohort study. BMJ Open 9:e024557. https://doi.org/10.1136/bmjopen-2018-024557
Weigl M, Letzel J, Angst F (2021) Prognostic factors for the improvement of pain and disability following multidisciplinary rehabilitation in patients with chronic neck pain. BMC Musculoskelet Disord 22:330. https://doi.org/10.1186/s12891-021-04194-9
Zebis MK, Andersen CH, Sundstrup E, Pedersen MT, Sjøgaard G, Andersen LL (2014) Time-wise change in neck pain in response to rehabilitation with specific resistance training: implications for exercise prescription. PLoS ONE 9:e93867. https://doi.org/10.1371/journal.pone.0093867
Edmond SL, Cutrone G, Werneke M, Ward J, Grigsby D, Weinberg J, Oswald W, Oliver D, McGill T, Hart DL (2014) Association between centralization and directional preference and functional and pain outcomes in patients with neck pain. J Orthop Sports Phys Ther 44:68–75. https://doi.org/10.2519/jospt.2014.4632
Jimenez-Garcia R, Del Barrio JL, Hernandez-Barrera V, de Miguel-Díez J, Jimenez-Trujillo I, Martinez-Huedo MA, Lopez-de-Andres A (2018) Is there an association between diabetes and neck pain and lower back pain? Results of a population-based study. J Pain Res 11:1005–1015. https://doi.org/10.2147/JPR.S158877
Wang XR, Kwok TCY, Griffith JF, Man YBW, Leung JCS, Wáng YXJ (2019) Prevalence of cervical spine degenerative changes in elderly population and its weak association with aging, neck pain, and osteoporosis. Ann Transl Med 7(18):486–486. https://doi.org/10.21037/atm.2019.07.80
Funding
No benefits or funds were received in support of this study by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent to participate
Informed consent was taken from all patients regarding the use of their anonymized demographic and clinical data for this study.
Consent for publication
Informed consent was taken from all patients regarding publication of their anonymized demographic and clinical data for this study.
Ethical approval
This study has been approved by an Institutional Ethics Committee and has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shetty, G.M., Vakil, P., Jain, S. et al. Predictors of failure to achieve minimal clinical important difference for pain and disability after mechanical diagnosis and therapy (MDT)-based multimodal rehabilitation for neck pain: a retrospective analysis of 4998 patients. Eur Spine J 31, 1291–1299 (2022). https://doi.org/10.1007/s00586-022-07167-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-022-07167-1