Abstract
Purpose
To investigate the optimal lowest instrumented vertebra (LIV) in the treatment of Scheuermann kyphosis (SK) with different curve patterns.
Methods
Fifty-two SK patients who underwent posterior surgery between January 2010 and December 2017 with a minimum follow-up of 2 years were retrospectively reviewed. Patients were divided into two groups based on the curve pattern: the Scheuermann thoracic kyphosis (STK group) or Scheuermann thoracolumbar kyphosis (STLK group). Based on the relationship between the sagittal stable vertebra (SSV) and LIV, both groups were further divided into the SSV group and SSV-1 group. Radiographic parameters, distal junctional kyphosis (DJK) incidence and SRS-22 questionnaire scores were evaluated.
Results
In STK and STLK groups, there were no significant differences in most pre- and postoperative radiographic assessments between SSV and SSV-1 subgroups. DJK incidence showed no significant differences between groups during follow-up (P > 0.05). LIV-PSVL was significantly more negative in the SSV-1 group than that in the SSV group (P < 0.001). Within the SSV-1 group, patients with DJK showed a more negative LIV-PSVL (P = 0.039). Moderate correlation was observed between preoperative LIV-PSVL and DJK with a Spearman coefficient of − 0.474 (P = 0.035). Receiver operative characteristic curve analysis showed that the threshold value of preoperative LIV-PSVL to predict DJK was − 37.35 mm (area under the curve 0.882).
Conclusion
Shorter fusion stopping at SSV-1 achieved comparable clinical outcomes and did not increase the risk of DJK for both STK and STLK patients. For patients whose preoperative LIV-PSVL < − 37.35 mm, extending fusion to SSV is an acceptable solution to prevent DJK.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Scheuermann kyphosis (SK) is a common cause of structural hyperkyphosis and occurs during childhood and adolescence [1]. This condition is mainly characterized by wedging of the vertebral body, an irregular vertebral end plate, and diminished anterior vertebral growth [2]. Indications for surgical intervention include progressive kyphosis (> 70°) despite brace compliance, neurologic deficit, persistent back pain, or cosmetic deformity [3].
Several treatment strategies have been explored through the development of instrumentation and surgical techniques. The one-stage posterior-only surgical approach is currently used to treat SK with a satisfying sagittal profile and a low risk of complications [4]. Selective fusion of the rigid curve is the priority in young patients to preserve lumbar vertebral segments. However, improper selection of fusion levels can lead to junctional problems and remains a critical issue because of its complicated management. Most spinal surgeons agree that the upper instrumented vertebra (UIV) should include the proximal end vertebra in the measured kyphosis to prevent proximal junctional kyphosis (PJK) [5,6,7]. However, the criteria for selection of the lower instrumented vertebra (LIV) have not been well established.
Previous reports have demonstrated good outcomes when the sagittal stable vertebra (SSV), defined as the proximal vertebra touched by the posterior sacral vertical line (PSVL), is selected as the LIV [8, 9]. However, some studies stated that fusion to the first lordotic vertebra (FLV) results in comparable rates of distal junctional kyphosis (DJK) compared with fusion to SSV [6, 10, 11]. In addition, SK has two different curve patterns: Scheuermann thoracic kyphosis (STK) and Scheuermann thoracolumbar kyphosis (STLK) [12]. A previous study suggested that extending fusion to SSV was appropriate for patients with STK, while a shorter fusion ending at FLV was indicated as sufficient for STLK patients [13]. However, the optimal distal fusion level for SK with different curve patterns remains unclear.
In this study, we analyzed the clinical and radiographic outcomes in patients with either STK or STLK with different distal fusion levels and investigated whether a short fusion strategy is an appropriate alternative for the treatment of SK. Special attention was paid to the curve correction and the occurrence of DJK during the postoperative period.
Materials and methods
Patients and groups
The current study was performed in accordance with STROBE guidelines. This study was approved by the institutional review board committee of our hospital. Patients who underwent deformity correction surgery for SK between January 2010 and December 2017 were identified in our database. The inclusion criteria for patients were as follows: (1) diagnosed with SK [14] (2) underwent one-stage all pedicle screw instrumentation and fusion with multi-level Ponte osteotomies; (3) the LIV was selected at either SSV or FLV as previously described [6, 8]; and (4) complete radiographic data with a minimum follow-up of 2 years. Exclusion criteria were as follows: (1) patients with any other spinal deformities; and (2) previous spinal trauma or surgery.
A total of 52 patients with SK were recruited in this study. FLVs were found to be one level higher than SSVs in 34 patients, while SSVs and FLVs were the same vertebra for 18 patients. When FLV was selected as LIV, the vertebra was either the same vertebra as SSV or the vertebra above SSV in these patients. Therefore, we simplify the LIV selection strategy as fusion to SSV or SSV-1.
Based on the location of the kyphotic apex, the patients were divided into two groups: patients with the kyphotic apex at T10 or above were defined as the STK group and patients with the kyphotic apex located below T10 were assigned to the STLK group [17]. The patients in the two groups were further subdivided into two groups based on the level of the distal fusion: the SSV group and the SSV-1 group.
Surgical procedure
The surgeries were performed by a single surgical team. Following thorough exposure of the spine, multi-level Ponte osteotomies were performed across the apex of the kyphosis, with resection of supra- and inter-spinous ligaments, ligamentum flavum, and the whole facet joints, followed by cephalad and caudad widening of the osteotomy gap up to 8–10 mm [15]. After placement of the pedicle screws at the intended fusion levels, pre-contoured rods were attached into the screws, followed by segmental compression. During rod placement, two to three rounds of compression in the area with Ponte osteotomies were used to enhance kyphosis correction. The final tightening was then performed, and a mixture of allografts and harvested autografts were placed within the prepared bone graft bed. Specific care was made to preserve the posterior ligamentous structures during the surgical procedure, especially at the upper and lower levels.
Somatosensory evoked potential (SEP) and motor evoked potential (MEP) were used to monitor the function of the spinal cord during the operation, and a wake-up test was conducted at the end of the procedure.
Radiographic and clinical evaluation
Radiographs were acquired with each patient by standing full spine X-ray preoperatively, postoperatively, and at the latest follow-up. We measured the following parameters in the sagittal plane: (1) global kyphosis (GK), the angle from upper to lower most tilted end vertebrae; (2) lumbar lordosis (LL), the angle between the vertical line of the superior end plate of L1 and that of the superior end plate of S1 on the sagittal plane; (3) sagittal vertical axis (SVA), the distance between the C7 plumb line (C7PL) and the posterosuperior corner of S1; negative values indicated that the C7PL fell behind the sacrum; (4) LIV-PSVL, defined as the distance from the center of the LIV to the posterior sacral vertical line (PSVL); negative values also indicated that the center of the LIV was placed behind the sacrum; (5) pelvic incidence (PI), the angle between the line perpendicular to the sacral plate at its midpoint and the line connecting the point to the middle axis of the femoral heads; (6) pelvic tilt (PT), the angle between the line connecting the midpoint of the sacral plate to the middle axis of the femoral heads and the gravity line; and (7) the sacral slope (SS), the angle between the sacral plate and the horizontal plane.
DJK was defined as an abnormal distal junctional angle ≥ 10° between the superior end plate of the lowest instrumented vertebra and the inferior end plate of the adjacent distal vertebra [16]. If a disc just distal to the LIV that was lordotic preoperatively became neutral or kyphotic after surgery, it was also defined as DJK [17]. All radiographic parameters were conducted using Surgimap (v2.3.2.1). Two spinal surgeons who were independent of the operations measured the radiographic assessments, and the mean values were calculated for analysis. The inter-observer variations were further estimated by intraclass correlation coefficient (ICC).
All patients completed the Scoliosis Research Society-22 questionnaire (SRS-22), which has been found to be suitable for evaluating patients with kyphosis [18, 19]. Patient-reported outcomes using SRS-22 were obtained before surgery and at the last follow-up.
Statistical analysis
All statistical analyses were performed using SPSS version 22.0, and data are presented as mean ± SD. Normality of the data was ensured with Kolmogorov–Smirnov test. Comparisons between the subgroups according to the distal fusion level were made with Mann–Whitney U test. The parameters were also compared between patients with and without DJK for patients whose LIV was at SSV-1. Chi-square analysis was applied to assess the categorical variables. Spearman’s correlation coefficient was performed to examine the correlation between preoperative LIV-PSVL and DJK. Receiver operative characteristic (ROC) curve analysis was performed to identify the threshold values of preoperative LIV-PSVL to predict the development of DJK. A P value of < 0.05 was considered as statistically significant.
Results
Demographic data
A total of 52 patients were included in this study. The mean age of the patients at the time of surgery was 17.2 ± 4.2 years old. The average number of Ponte osteotomy levels was 5.8 ± 1.5 and the average number of fused vertebrae was 11.8 ± 1.6. No obvious SEP and MEP change or loss was observed intraoperatively. The mean follow-up time was 35.7 ± 7.9 months. Inter-observer reliability assessments gave values above 0.9, which indicated excellent reliability of all parameters between the two observers. Based on the Kolmogorov–Smirnov test, all measured parameters were normally distributed.
The STK group included 21 patients with fusion to SSV and 12 patients with fusion to SSV-1; the STLK group consisted of 11 patients with fusion to SSV and 8 patients with fusion to SSV-1. As shown in Table 1, the distributions of SSV and LIV were significantly different for patients with different curve patterns (P < 0.001). For patients with STK, most of the SSVs were located at L2 and L3 (87.9%), while for patients with STLK, most of the SSVs were located at L3 and L4 (89.5%).
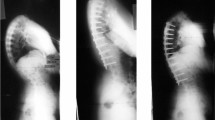
Comparison between SSV and SSV-1 groups in STK patients
For patients with STK, no significant difference was found in most preoperative radiographic assessments (GK, LL, SVA, PI, PT, SS) and scores of the SRS-22 questionnaire between the SSV and SSV-1 groups (Table 2). In the SSV group (Fig. 1a–c), GK significantly decreased from 78.9° ± 9.8° to 41.5° ± 7.6°, with a correction rate of 47.5% ± 6.6%. No significant correction loss was observed (1.4% ± 3.4%) at final follow-up. For the SSV-1 group (Fig. 1d–f), GK significantly decreased from 80.3° ± 10.6° to 41.8° ± 8.0° and maintained up to 44.0° ± 7.8° at the last follow-up. No significant differences were observed in postoperative curve correction rates (47.5% ± 6.6% vs. 47.8% ± 8.4%, P = 0.940) and correction loss (1.4% ± 3.4% vs. 2.8% ± 2.3%, P = 0.349) between groups. However, with regard to the positions of LIV, LIV-PSVL was significantly more negative in the SSV-1 group than in the SSV group preoperatively, postoperatively and at last follow-up (P < 0.001).
a A 16-year-old male STK patient with the apex of the kyphotic curve at T9. The preoperative GK was 92°. L2 was SSV, which was selected as LIV. b After surgery, GK was corrected to 41° with a correction rate of 55.4%. c The 2-year postoperative radiograph showed no distal decompensation. GK maintained at 46° with no obvious correction loss (5.4%). d A 19-year-old male STK patient with the apex of the kyphotic curve at T7. The preoperative GK was 94°. L2 was SSV, while LIV was selected as L1. e After surgery, GK was corrected to 45° with a correction rate of 52.1%. f The 4-year postoperative radiograph showed no distal decompensation. GK maintained at 45° with no obvious correction loss (0.0%)
As shown in Table 2, no significant differences in SRS-22 evaluation were observed between groups at the final follow-up. Three patients (14.3%) in the SSV group and two (16.7%) in the SSV-1 group developed DJK during follow-up; no significant difference in incidence was observed between the two groups (P = 0.854).
Comparison between SSV and SSV-1 groups in STLK patients
The subgroup analysis for patients in STLK group is summarized in Table 3. Before surgery, no significant differences were observed in most preoperative radiographic parameters (GK, LL, SVA, PI, PT, SS) and scores of the SRS-22 questionnaire between the SSV and SSV-1 groups (Fig. 2). The kyphosis deformities in both groups were corrected postoperatively (37.9° ± 6.9° vs. 40.4° ± 5.5°, P = 0.592), with a similar correction rate (45.9% ± 10.5% vs. 43.6% ± 6.1%, P = 0.502). Moreover, the corrections were maintained at last follow-up (39.9° ± 6.4° vs. 44.0° ± 5.0°, P = 0.062) and no significant difference was found in correction loss (2.9% ± 6.5% vs. 5.6% ± 9.1%, P = 0.323) between groups. However, on account of the different distal fusion strategy, LIV-PSVL was significantly more negative in the SSV-1 group than SSV group before surgery, after surgery and at last follow-up (P < 0.001).
a A 18-year-old male STLK patient with the apex of the kyphotic curve at T11. The preoperative GK was 70°. L3 was SSV, which was selected as LIV. b After surgery, GK was corrected to 36° with a correction rate of 48.6%. c The 2-year postoperative radiograph showed no distal decompensation. GK maintained at 39° with no obvious correction loss (4.3%). d A 15-year-old male STLK patient with the apex of the kyphotic curve at T11. The preoperative GK was 73°. L3 was SSV, while LIV was selected as L2. e After surgery, GK was corrected to 34° with a correction rate of 53.4%. f The 4-year postoperative radiograph showed no distal decompensation. The GK maintained at 37° with no obvious correction loss (4.1%)
The preoperative and postoperative SRS-22 scores for the SSV and SSV-1 groups are presented in Table 3. No significant difference was found in any of the five domains between the two groups before surgery and at the final follow-up (P > 0.05). In each subgroup, one patient developed DJK at the latest follow-up and there was no significant difference in DJK incidence between groups (9.1% vs. 12.5%, P = 0.811).
Radiographic and clinical outcomes between patients with and without DJK
In the whole patient cohort, four patients (12.5%) in the SSV group and three (15.0%) in the SSV-1 group developed DJK during the follow-up period, and the incidence was equivalent (P = 0.711). None of the patients in this cohort required revision surgery. Neurologic defecits, rod breakage, and pseudoarthrosis were not observed during follow-up.
Within the SSV-1 group, no significant difference was found in GK, LL, PI, PT, and SS before and after surgery between the patients with and without DJK. No significant difference was noted in any of the SRS-22 domains before surgery. However, the function scores of SRS-22 in the SSV-1 group were significantly higher than those of the SSV-1 group at the final follow-up (P = 0.047, Table 4). Moreover, the LIV-PSVL was significantly more negative in patients with DJK preoperatively compared with patients without DJK (− 40.2 ± 2.2 vs. − 31.2 ± 6.6, P = 0.039, Fig. 3). The Spearman correlation coefficient between preoperative LIV-PSVL and the occurrence of DJK was − 0.474 (P = 0.035).
In ROC curve analysis, the threshold value was determined as − 37.35 mm, indicating that patients with preoperative LIV-PSVL < − 37.35 mm were more likely to show postoperative DJK (area under the ROC curve = 0.882 (95%CI: 0.721 ~ 1.000); specificity = 76.5%; sensitivity = 100.0%; Fig. 4).
Discussion
DJK is a common complication related to instrumentation after surgery for correction of SK, with a reported incidence of 20.8% [20]. DJK is often accompanied with biomechanical changes in adjacent segments and the loss of the physiological lumbar lordosis angle, resulting in progressive intervertebral disc degeneration and unsatisfactory clinical outcome. Proper selection of fusion levels is the key factor to minimize the risk of DJK [10, 21]. Nevertheless, precise criteria for the selection of fusion levels in SK have not been well established.
Cho et al. [8] first introduced the concept of SSV, which served to guide the selection of LIV. Mikhaylovskiy et al. [9] further evaluated the validity of the Cho–Lenke method for selecting LIV and confirmed the superiority of SSV in preventing DJK. However, Yanik et al. [11] conducted a prospective analysis of 54 SK patients and reported that fusion to FLV is sufficient and economized one fusion level. In addition, Kim et al. [22] concluded that selecting SSV as LIV may reduce complications secondary to DJK, but at the expense of incorporating more fusion levels. Zhu et al. [13] divided SK patients into two curve patterns and recommended selecting SSV as LIV for patients with STK and selecting FLV as LIV for STLK patients. However, the previous study did not compare STK fused to SSV or FLV or comparison between STLK fused to FLV or SSV.
This is the first study to systematically investigate the optimal distal fusion strategy in SK patients with different curve patterns. Subgroup analysis showed no significant difference with regard to the kyphosis correction and the incidence of DJK (P > 0.05) between patients with STK and STLK. In addition, our results revealed that a more negative preoperative LIV-PSVL was associated with a higher risk for developing DJK in the SSV-1 group (r = − 0.474, P = 0.035). To provide a more practical approach to predict postoperative DJK, we used ROC curve to identify the cut-off points for preoperative LIV-PSVL. ROC curve analysis indicated that a preoperative LIV-PSVL < − 37.35 mm predicted a high risk of DJK.
In the lateral radiographs, the discrepancy of segmental angles in the disc spaces is quite small in the transitional thoracolumbar junction area [13]. As a result, clearly distinguishing the first lordotic disk is difficult, making the identification of FLV sometimes inaccurate and unreliable [22]. In this study, when FLV selected as LIV, the vertebra was either the same vertebra as SSV or only one level above SSV, which were consistent with previous literatures [11, 13, 17]. Therefore, we proposed the concept of “SSV-1” and simplified the LIV selection strategy as fusion to SSV or SSV-1. Our results indicated that selection of SSV-1 or SSV as the distal fusion level obtained comparable deformity corrections and did not lead to a higher incidence of DJK for both patients with STK and STLK. We hypothesized that one of the reasons for the similar outcomes was that multi-level Ponte osteotomies were performed across the apex of the deformity in our study. Ponte osteotomy is an efficient method to restore sagittal alignment in the treatment of Scheuermann’s disease [20], which could afford approximately 5°–10° of correction per level [23], thus improving the spinal flexibility and obtaining satisfying correction for such rigid kyphosis. After the posterior column structure is completely released, the stress of the instrumentation system in contact with vertebrae can be reduced to decrease the risk of rod fracture as well as the development of DJK. In addition, it is worth noting that the hybrid instrumentation system including hook constructs was used previous studies [8, 9] and is less stable and more prone to result in junctional problems related to more soft tissue dissection [10, 24, 25]. However, all of our patients were treated with posterior pedicle-only screw instrumentation and fusion. The powerful correction ability of this technique may lead to completely different postoperative curve behavior in comparison with hook and hybrid instrumentations, allowing for better correction maintenance [17]. Hence, our results suggest the utility in stopping the fusion above the SSV with the aim of preserving more mobile segment.
Our data also showed that the preoperative LIV-PSVL should be emphasized. To maintain the global sagittal balance and stability of the spine after operation, the distal end of the fusion should be placed within the center of gravity. In other words, the center of SSV-1 should be relatively close to the posterior sacrum vertical line, so that the distal fusion mass is maintained over the sacrum. In this circumstance, it would be easier to get the LIV into the stable zone and potentially economize a fusion segment. Hence, we recommended that the location of the LIV and the distance between preoperative LIV to PSVL should be taken into consideration when selecting the distal fusion level strategy.
This study has several limitations. First, our findings are limited by the small sample size with a low percentage of cases with DJK. Second, because of the retrospective design of this study, the potential selection bias cannot be completely avoided. Therefore, a larger sample size of SK patients and a randomized prospective study are warranted for an in-depth evaluation to verify these results. Moreover, this study had a short follow-up period. Therefore, it is necessary to validate the current results in future studies with a long-term follow-up.
Conclusion
Shorter fusion stopping at SSV-1 achieves comparable clinical outcomes and does not increase the risk of DJK for both patients with STK and STLK. However, for patients with a preoperative LIV-PSVL < − 37.35 mm, extending fusion to SSV is an acceptable solution to prevent DJK.
References
Lowe TG, Line BG (2007) Evidence based medicine: analysis of Scheuermann kyphosis. Spine 32(19 Suppl):S115–S119. https://doi.org/10.1097/BRS.0b013e3181354501
Bezalel T, Carmeli E, Been E, Kalichman L (2014) Scheuermann’s disease: current diagnosis and treatment approach. J Back Musculoskelet Rehabil 27(4):383–390. https://doi.org/10.3233/BMR-140483
Palazzo C, Sailhan F, Revel M (2014) Scheuermann’s disease: an update. Joint Bone Spine 81(3):209–214. https://doi.org/10.1016/j.jbspin.2013.11.012
Koller H, Lenke LG, Meier O et al (2015) Comparison of anteroposterior to posterior-only correction of Scheuermann’s kyphosis: a matched-pair radiographic analysis of 92 patients. Spine Deform 3(2):192–198. https://doi.org/10.1016/j.jspd.2014.09.048
Papagelopoulos PJ, Klassen RA, Peterson HA, Dekutoski MB (2001) Surgical treatment of Scheuermann’s disease with segmental compression instrumentation. Clin Orthop Relat Res 386:139–149. https://doi.org/10.1097/00003086-200105000-00018
Lowe TG, Kasten MD (1994) An analysis of sagittal curves and balance after cotrel-dubousset instrumentation for kyphosis secondary to Scheuermann’s disease. A review of 32 patients. Spine 19(15):1680–1685. https://doi.org/10.1097/00007632-199408000-00005
De Jonge T, Illes T, Bellyei A (2001) Surgical correction of Scheuermann’s kyphosis. Int Orthop 25(2):70–73. https://doi.org/10.1007/s002640100232
Cho KJ, Lenke LG, Bridwell KH, Kamiya M, Sides B (2009) Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine 34(8):765–770. https://doi.org/10.1097/BRS.0b013e31819e28ed
Mikhaylovskiy MV, Sorokin AN, Novikov VV, Vasyura AS (2015) Selection of the optimal level of distal fixation for correction of Scheuermann’s hyperkyphosis. Folia Med (Plovdiv) 57(1):29–36. https://doi.org/10.1515/folmed-2015-0016
Denis F, Sun EC, Winter RB (2009) Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum 5-year follow-up. Spine 34(20):E729–E734. https://doi.org/10.1097/BRS.0b013e3181ae2ab2
Yanik HS, Ketenci IE, Coskun T, Ulusoy A, Erdem S (2016) Selection of distal fusion level in posterior instrumentation and fusion of Scheuermann kyphosis: is fusion to sagittal stable vertebra necessary? Eur Spine J 25(2):583–589. https://doi.org/10.1007/s00586-015-4123-7
Jiang L, Qiu Y, Xu L et al (2014) Sagittal spinopelvic alignment in adolescents associated with Scheuermann’s kyphosis: a comparison with normal population. Eur Spine J 23(7):1420–1426. https://doi.org/10.1007/s00586-014-3266-2
Zhu W, Sun X, Pan W et al (2019) Curve patterns deserve attention when determining the optimal distal fusion level in correction surgery for Scheuermann kyphosis. Spine J 19(9):1529–1539. https://doi.org/10.1016/j.spinee.2019.04.007
Makurthou AA, Oei L, El Saddy S et al (2013) Scheuermann disease: evaluation of radiological criteria and population prevalence. Spine 38(19):1690–1694. https://doi.org/10.1097/BRS.0b013e31829ee8b7
Geck MJ, Macagno A, Ponte A, Shufflebarger HL (2007) The Ponte procedure: posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech 20(8):586–593. https://doi.org/10.1097/BSD.0b013e31803d3b16
Lowe TG, Lenke L, Betz R et al (2006) Distal junctional kyphosis of adolescent idiopathic thoracic curves following anterior or posterior instrumented fusion: incidence, risk factors, and prevention. Spine 31(3):299–302. https://doi.org/10.1097/01.brs.0000197221.23109.fc
Lundine K, Turner P, Johnson M (2012) Thoracic hyperkyphosis: assessment of the distal fusion level. Global Spine J 2(2):65–70. https://doi.org/10.1055/s-0032-1319771
Toombs C, Lonner B, Shah S et al (2018) Quality of life improvement following surgery in adolescent spinal deformity patients: a comparison between Scheuermann kyphosis and adolescent idiopathic scoliosis. Spine Deform 6(6):676–683. https://doi.org/10.1016/j.jspd.2018.04.009
Petcharaporn M, Pawelek J, Bastrom T, Lonner B, Newton PO (2007) The relationship between thoracic hyperkyphosis and the scoliosis research society outcomes instrument. Spine 32(20):2226–2231. https://doi.org/10.1097/BRS.0b013e31814b1bef
Gong Y, Yuan L, He M et al (2019) Comparison between stable sagittal vertebra and first lordotic vertebra instrumentation for prevention of distal junctional kyphosis in Scheuermann disease: systematic review and meta-analysis. Clin Spine Surg 32(8):330–336. https://doi.org/10.1097/BSD.0000000000000792
Sardar ZM, Ames RJ, Lenke L (2019) Scheuermann’s kyphosis: diagnosis, management, and selecting fusion levels. J Am Acad Orthop Surg 27(10):e462–e472. https://doi.org/10.5435/JAAOS-D-17-00748
Kim HJ, Nemani V, Boachie-Adjei O et al (2017) Distal fusion level selection in Scheuermann’s kyphosis: a comparison of lordotic disc segment versus the sagittal stable vertebrae. Global Spine J 7(3):254–259. https://doi.org/10.1177/2192568217699183
Chang KW, Cheng CW, Chen HC, Chang KI, Chen TC (2008) Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine 33(13):1470–1477. https://doi.org/10.1097/BRS.0b013e3181753bcd
Lonner BS, Newton P, Betz R et al (2007) Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine 32(24):2644–2652. https://doi.org/10.1097/BRS.0b013e31815a5238
Koptan WM, Elmiligui YH, Elsebaie HB (2009) All pedicle screw instrumentation for Scheuermann’s kyphosis correction: is it worth it? Spine J 9(4):296–302. https://doi.org/10.1016/j.spinee.2008.05.011
Acknowledgements
This work was supported by the National Natural Science Foundation of China (NSFC) (No. 82072518), the Nanjing Medical Science and Technique Development Foundation (No. QRX17126) funds and Jiangsu Provincial Key Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author’s declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, Y., Hu, Z., Zhang, L. et al. Selection of the optimal distal fusion level for Scheuermann kyphosis with different curve patterns: when can we stop above the sagittal stable vertebra?. Eur Spine J 31, 1710–1718 (2022). https://doi.org/10.1007/s00586-021-07039-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-07039-0