Abstract
Objective
To compare radiologically balloon kyphoplasty (BKP) and vertebral compression fracture (VCF) expansion and corroborate with a finite element (FE) analysis. The principle of BKP is to stabilize VCF by restoring vertebral body anatomy using bone expansion and cement filling. More recently, vertebral body stenting (VBS) has been developed to reduce the loss of vertebral height observed after balloon deflation.
Methods
A retrospective, monocentric and continuous study of 60 non-osteoporotic fractures of the thoracolumbar junction treated by vertebral bone expansion was carried out over three years. The main endpoint was radiological correction of vertebral kyphosis (VK) at 3 months. The other studied parameters were vertebral height, index of Farcy, index of Beck, cement leakages and their location.
A FE model was developed to analyze effects linked to the stent during cement injection, specifically throughout the risk of cement leakage evaluation.
Results
After three months, average reduction of VK was 4.73° ± 4.8° after BKP, and 4.63° ± 2.7° after VBS. There was no difference between the two techniques, but cement leakage was significantly greater with BKP (41.7%) than with VBS (4.2%). FE analysis showed substantial changes of the cement flow orientation in the presence of a stent.
Conclusion
BKP and VBS offer comparable expansion with no added value of VBS in non-osteoporotic VCF reduction. VBS technique appears to prevent cement leakage due to its mesh architecture hindering the leaking process. In counterpart, such balloon expansion is likely to require higher pressure to deploy the stent. This could be an important parameter to take into account in young patients with high bone density.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thoracolumbar vertebral compression fractures (VCFs) affecting approximately 5 million people worldwide (2–3 million in the USA and 2 million in Europe) can dramatically affect patient quality of life, leading to neurological deficit, sagittal kyphosis and imbalance [1]. New percutaneous techniques offer early recovery by minimizing surgical invasiveness [2]. They are based on vertebral expansion aimed at providing vertebral body reconstruction using either a balloon without stenting (balloon kyphoplasty/BKP) or an inflatable stent deployed by an underlying balloon (vertebral body stenting/VBS).
BKP, which is derived from vertebroplasty, has the capacity to restore vertebral height by combining external reduction of the traumatic kyphosis [3], obtained by intraoperative patient positioning, and internal reduction, which is due to balloon expansion of the collapsed vertebral body. Additional cement injected at the level of the fracture through pedicular catheterization is aimed at reinforcing the anterior column after reduction [4]. BKP was originally described in management of tumoral lesions and has become a treatment of choice in the field of osteoporotic VCF [5]. More recently, indications were extended to non-osteoporotic VCF [6]. This technique has shown some limitations, including substantial loss of correction between balloon deflation and cement injection [4, 6]. This limitation has supported the development of vertebral stentoplasty: In 2010, Rotter et al. [7] described a new method using the VBS system (Synthes GmbH Oberdorf, Switzerland). The idea was first to deploy a stent within the fracture using a coupled balloon and subsequently to keep the stent in place during cement injection.
Several biomechanical works have explored these techniques. In silico modeling [8] and finite element (FE) simulation have attempted to assess the risk of leakage, with cement stress distribution depending on catheter positioning and injected volume [9]. While the VCF management is more widely accepted to be a conservative treatment [10], BKP indication is becoming larger to avoid post-traumatic kyphosis and/or when conservative management is not tolerated or has failed. Until now, BKP and VBS expansion in a non-osteoporotic VCF population has never been compared in human study [11, 12]. BONEXP is a retrospective radiological study conducted on 60 consecutive patients treated by either BKP or VBS for acute VCF. The main aim of the current comparative study was to investigate whether VBS technique is advantageous compared to BKP in reduction of fracture. We hypothesis that stenting would provide benefit compared to BKP. We further investigated the anatomical distribution and clinical incidence of cement leaks and adjacent disk behavior in both VBS and BKP procedures. We then developed a FE model assessing the mechanical influence of additional physical stenting on cement polymerization, flow and leakage.
Materials and methods
Clinical study
The trial was retrospective, monocentric and involved two continuous cohorts with an inclusion period of 3 years.
-
(1)
Inclusion criteria
Patients presenting with osteoporotic-like fractures, neurological complications, multilevel degenerative disk disease or requiring an additional treatment were not considered for this study. Included patients were all operated under general anesthesia in one center by the same specialized spine surgeon, an expert in the relevant vertebral expansion techniques [6, 13]. Pre-and postoperative neurological examinations were collected and analyzed. Because of the angular correction losses described in the literature with phosphocalcic cement [14], acrylic cements were used in all cases. The cements were both high-viscosity PMMA (Bone Cement V—Zimmer Biomet company, Warsaw, IN, USA—for BKP and Vertecem V+—DePuy Synthes company, Raynham, MA, USA—for VBS).
-
(2)
Noninclusion criteria
Woman older than 60 years and patients presenting with osteoporotic-looking fractures (from the classification of Genant [15]), objective radiological criteria for rupture of the posterior ligament complex, neurological complications during management, multistage discopathy or requiring additional treatment (e.g., corset or osteosynthesis) were not included. Magerl type A.3.3 fractures with fragmentation or inter-fragmentary gap considered too large [≥ score 7 of the load sharing classification (16)] and Magerl type A.2.2 split fractures were also considered as noninclusion criteria.
-
(3)
Radiological analysis and measurement parameters
Radiological analysis was performed with Horizon Rad Station™ software (McKesson company, San Francisco, CA, USA) following spine X-rays. The patients were radiologically evaluated preoperatively and postoperatively, after 1 day (D1) and 90 days (D90) of clinical follow-ups, in particular to analyze the potential disk degeneration associated or not with the VCF [16, 17]. Fractures were described according to Magerl et al. [18] and McCormack et al. [19] classifications on initial 3D CT scan. Measurement of the different indexes [20] focused on fracture reduction was carried out by two independent observatories and is detailed in Fig. 1. Occurrence of cement leakage was systematically sought out. Radiological behavior of the adjacent disks was assessed on the load-bearing postoperative images at 3 months.
-
(4)
Ethical considerations
This retrospective evaluation was approved by the French National Commission on Informatics and Liberty and conducted in accordance with good clinical practice. All procedures in this study were implemented in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
-
(5)
Statistical analysis
Statistical analysis was performed using R 2.15 software (R Foundation for Statistical Computing). Shapiro–Wilk test was used to check the hypothesis of normality distribution of our variables. The student t test was used to compare the quantitative variables. Difference was considered to be significant for p < 0.05.
FE Model
A FE model was developed using generic and simplified vertebrae geometry based on the literature [8]. FE analysis of cement injection was carried out using SolidWorks software (Dassault Systèmes Corporation, Waltham, MA, USA). Cavities corresponding to the volume created by balloon expansion were modeled with or without stent (Fig. 2). The fracture was modeled by a gap corresponding to a separation of the vertebral body (cancellous and cortical bones) allowing the fluid to be disseminated in the sagittal and/or frontal directions. Stent and vertebra fragments were considered as rigid bodies (with young modulus of 1200 MPa and 100 MPa, respectively, for cortical bone and cancellous bone [21]), and the fluid volume was meshed with 19,800 elements. Flow behavior was simulated by injecting a fluid at a constant injection rate of 5 mL/min in both models and retaining viscosity of 20 kPa.s, corresponding to the viscosity of PMMA 10 min after mixing [22]. This numerical approach was validated by a comparison from an experimental model of flow of high-viscosity cement in a cavity with similar geometry [23]. To validate this comparison with numerical results, the experimental flow was observed by optical analysis with a CCD camera and cement injection.
Results
Study population
From the 60 consecutive initially included patients, 48 were monitored (Table 1), while seven were treated in another hospital and five did not come back for checkup). Twenty-four patients in BKP (11 women, 45.8 [24.6–61.8] years) and 24 in VBS (12 women, 48.7 [28.0–63.0] years) were analyzed. Fractures were located at T12 (5 BKP, 7 VBS), L1 (15 BKP, 12 VBS) and L2 (4 BKP, 5 VBS) and were classified as follows: Magerl A1 (11 BKP, 3 VBS), A2 (2 VBS) and A3 (13 BKP, 19 VBS).
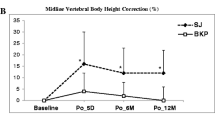
Radiological results
VK significantly increase (Table 1) in the overall population (p = 0.00029). In terms of gain of correction, no significant difference between BKP and VBS was found post-operatively, neither after 1 day (D1) nor after 90 days (D90). The Sagittal Index of Farcy (SIF) significantly increased in the general population, without any difference between the two groups (p = 0.3902). The values of disk height index (DHI), reported in Table 2, showed a nonsignificant tendency of the upper superior disk to collapse in time, indifferently between the two groups. No significant difference was found between them for upper discal angulation (DA) and the lower DA (Table 2).
We observed a significant gain of height of the anterior vertebral wall, of the index of Beck and of the index of collapse for the two groups. There was no significant difference between BKP and VBS in any of the measurements (Table 3).
Leakages
Figure 3 shows distribution of observed leakages in the BKP and VBS cohorts. The overall rate of leakages on the targeted population was 23%, and it was significantly higher in the BKP group (41.7% for BKP group vs. 4.2% for VBS group—p = 0.0023). Cement leakages were concentrated at the anterior wall, toward the superior or inferior endplates or the lateral part of the vertebra but never toward the posterior wall or the spinal canal. No clinical complication [24] due to a leakage was reported, and all patients were asymptomatic on neurological examination.
A thorough study of the disks in which intradiscal cement leakage was observed did not indicate any significant loss of the DHI loss when compared to patients without leakage (Table 4). However, a trend toward the increased loss of discal lordosis (DA) was observed (p = 0.0579).
Specific analysis of the preoperative CT scans of the vertebrae with leakages did not show any relationship between the fracture morphological parameters of the fractures (Magerl et al. [18] and McCormack et al. [19] classifications) and leakage occurrence.
Modeling
Figure 4 shows the velocity fields simulated during cement injection into the cavities created by balloon expansion. Velocity maps highlight a change in cement kinematics in the presence of a stent (Fig. 4a,b). The velocity profiles (Fig. 4c) show a clear decrease in fluid lateral diffusion and an increase in the longitudinal axis of the stent.
Discussion
Fracture reduction
Our radiological study shows a significant correction of 4.7° of the VK in accordance with the data of the literature ranging from 4.5° to 7.4° [12, 25] for the BKP group. The gain in correction is, according to the series, slightly inferior to those observed in the literature, but our population was characterized by non-osteoporotic fractures with inferior initial VK. The correction of the VK in percentage (44%) is similar to the data reported by Berlemann et al. [26] (47.7%, comparative data summarized in Table 5). For the VBS group, we observed a significant correction of 4.6° of the VK in accordance with the literature [11, 12, 27] (3.2° to 7.3°, Table 5). In this study, we were not able to highlight any significant difference between the two methods as regards restoration of the anatomy of the vertebral body (VK, Index of Beck, Index of collapse, SIF) in a non-osteoporotic patient population. These results match those of Werner et al. [12] who, in 100 osteoporotic fractures, did not observe any difference in terms of correction of VK with 4.5° ± 3.6° for the BKP versus 4,7° ± 4,2° for the VBS.
Interestingly, several biomechanical studies have shown a significant decrease in the loss of reduction due to addition of metallic stent [7]. For Rotter et al.[7] in a cadaveric study, loss of height occurs during balloon removal and is significantly greater in BKP (12%) than in VBS (4%). A minor gain in anterior height occurs with BKP compared to VBS with VK correction of 1.9° versus 4°, respectively. This study measured fracture reduction after bone expansion, while applying a substantial load on the vertebral endplates (force of 110 N) deduced from live measurements of intradiscal pressure on volunteers, standing up during daily routine activities [28]. Therefore, for this cadaveric study, while the role of the stent appears to be decisive in maintaining a reduction under external vertical compression, one should remember that a live surgery is performed on a lying patient, under prone position, using expansion to create a cavity without having to endure the compressive influence of the verticality on the vertebra.
In practice, we have noted that the intraoperative lordosis provided by patient positioning is part of fracture reduction strategy and can influence the quality of reduction. Voggenreiter et al. [25] demonstrated the impact of patient positioning. The works by Teyssédou et al. [6] corroborate the importance of the installation in prone position as a mean of optimizing fracture reduction. Finally, even though a significant decrease in the height of the vertebral body and a VK increase during balloon deflation both constitute substantial limitations of the BKP technique, this should nonetheless be pointed out that while the fracture reduction initially achieved by BKP might be superior without stenting, secondary loss of correction during balloon deflation using BKP annihilates this effect. This should explain the lack of difference in radiological fracture reduction between the two groups. The lack of added value for VBS in fracture reduction compared to BKP could be due to more limited possibilities of expansion of the balloon, when it is surrounded by a premounted stent. Indeed, for osteoporotic patients, balloon expansion requires higher pressures with than without a stent, a finding confirmed by Werner et al. [12]. Paradoxically, the balloon inflation rate provided by VBS is more limited in the range of available working pressure than BKP (440PSI for VBS versus 700PSI for BKP). This could be a major parameter for young patients with high bone density.
Cement leakage
In the BKP group, a sizable rate of leakage (41.7%) is observed, which is in accordance with the rates of leakage ranging from 10.6% [29] to 51% [30] found in the literature. In the VBS group, the rate of leakage is 4.2%, much lower than the rate in the literature, which generally ranges from 10% [27] to 30% [12]. It is interesting to note that the only leakage observed in the VBS group is not lateral but anterior. The anatomical distribution of cement leakage (preferentially anterolateral and intradiscal, never posterior) is in line with the lack of clinical consequences documented at 3-month clinical follow-up. In accordance with these results, radiological evaluation of the adjacent disks after surgery did not objectify any difference between the two groups. This study underlines the tendencies of the upper disk to lose height in time and of the lower disk to compensate for residual traumatic kyphosis, a finding that corresponds to the results of Teyssédou et al. [13].
Study limitations and FE analysis
The main limitations of this study include the number of patients, potential interindividual fracture variability and the nonrandomized design of this comparative study. One could expect a sequence effect due to a change in technique used for VCF treatment (moving in 2014 from exclusive BKP, which was considered as a gold standard procedure, to VBS, which was previously unavailable in France). Bone densitometry analysis was not conducted on the patients. Selective inclusion criteria, as regards the non-osteoporotic character of the fracture, requirement of a single-level fracture and intervention of a single operator, considerably reduced our population. A systematic MRI could not be performed for the included patients, and the potential disk degeneration was evaluated from radiographic analysis [16, 17].
To address these clinical limitations and to differentiate the role of the cement from the potential added value of the stent in leakage occurrence, we built a numerical model to simulate injection of cement into a cavity in the presence or absence of a stent.
FE analysis, using a strictly comparable cement and fracture model, confirms that the difference in rate of leakage between BKP and VBS corresponds to the properties of the metallic stent. Stentoplasty appears to function as a rheological brake preventing leakages. FE simulation clearly slows down the flow in radial directions, which corresponds to classical properties of mesh architecture, thereby limiting lateral leakage. FE analysis also confirms that stentoplasty promotes flow in the axial direction that may lead to anterior leakage. This numerical approach was preliminarily validated by a comparison with experiments on a simplified model and by using optical methods [23]. However, numerical results of the present study should be corroborated in future works by personalized adaptation of the volumes to be filled and shaping of the stent to be deployed within the cavity. Previous work on demonstration models has shown that the shape, positioning and volume of the cavity to be filled are important parameters in leakage risk analysis [8].
Conclusion
Kyphoplasty and stentoplasty are effective treatments for vertebral fracture reduction of the non-osteoporotic subject, with an equivalent quality in reduction. There is no added value of VBS compared to BKP in fracture reduction, although a difference in the incidence of asymptomatic leakage has been highlighted in this study. FE flow modeling provides substantial information to enhance our understanding of this phenomenon. The capacity of VBS to prevent leakage might be due to the mesh architecture created by stent addition, which may hinder the process of biomechanical leaking. This new architecture might potentially mitigate the mechanical expansion of the balloon due to higher pressure requirements, especially in cases of high bone density. However, BKP may initiate a more efficient expansion of the fractured vertebra, but it cannot prevent a loss of correction due to balloon deflation. A more ambitious randomized controlled trial could be carried out to clinically compare the rate of disk leakage, injection pressure and their repercussions on disks/patient outcomes in the long term.
References
Kraemer WJ, Schemitsch EH, Lever J et al (1996) Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma 10:541–544
Oppenheimer JH, DeCastro I, McDonnell DE (2009) Minimally invasive spine technology and minimally invasive spine surgery: a historical review. Neurosurg Focus 27:E9
Freslon M, Bouaka D, Coipeau P et al (2008) Thoracolumbar fractures. Rev Chir Orthop Reparatrice Appar Mot 94:S22–35
Oner FC, Dhert WJ, Verlaan J-J (2005) Less invasive anterior column reconstruction in thoracolumbar fractures. Injury 36:S82–S89
Bornemann R, Koch EMW, Wollny M, Pflugmacher R (2014) Treatment options for vertebral fractures an overview of different philosophies and techniques for vertebral augmentation. Eur J Orthop Surg Traumatol 24:131–143
Teyssédou S, Saget M, Prébet R et al (2012) Evaluation of percutaneous surgery in the treatment of thoracolumbar fractures. Preliminary results of a prospective study on 65 patients. Orthop Traumatol Surg Res 98:39–47
Rotter R, Martin H, Fuerderer S et al (2010) Vertebral body stenting: a new method for vertebral augmentation versus kyphoplasty. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 19:916–923. https://doi.org/10.1007/s00586-010-1341-x
Bou-Francis A, Soyka RPW, Ferguson SJ et al (2015) Novel methodology for assessing biomaterial–biofluid interaction in cancellous bone. J Mech Behav Biomed Mater 46:158–167
Tsouknidas A, Savvakis S, Asaniotis Y et al (2013) The effect of kyphoplasty parameters on the dynamic load transfer within the lumbar spine considering the response of a bio-realistic spine segment. Clin Biomech 28:949–955
Fritzell P, Ohlin A, Borgström F (2011) Cost-effectiveness of balloon kyphoplasty versus standard medical treatment in patients with osteoporotic vertebral compression fracture: a Swedish multicenter randomized controlled trial with 2-year follow-up. Spine 36:2243–2251
Hartmann F, Griese M, Dietz S-O et al (2015) Two-year results of vertebral body stenting for the treatment of traumatic incomplete burst fractures. Minim Invasive Ther Allied Technol MITAT Off J Soc Minim Invasive Ther 24:161–166. https://doi.org/10.3109/13645706.2014.962546
Werner CML, Osterhoff G, Schlickeiser J et al (2013) Vertebral body stenting versus kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a randomized trial. J Bone Jt Surg Am 95:577–584. https://doi.org/10.2106/JBJS.L.00024
Teyssédou S, Saget M, Gayet LE et al (2016) Radiologic study of disc behavior following compression fracture of the thoracolumbar hinge managed by kyphoplasty: a 52-case series. Orthop Traumatol Surg Res 102:61–65
Maestretti G, Cremer C, Otten P, Jakob RP (2007) Prospective study of standalone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J 16:601–610
Genant HK, Wu CY, Van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Benneker LM, Heini PF, Anderson SE et al (2005) Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration. Eur Spine J 14:27–35
Jarman JP, Arpinar VE, Baruah D et al (2015) Intervertebral disc height loss demonstrates the threshold of major pathological changes during degeneration. Eur Spine J 24:1944–1950
Magerl F, Aebi M, Gertzbein SD et al (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 3:184–201
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine 19:1741–1744
Ulmar B, Brunner A, Gühring M et al (2010) Inter-and intraobserver reliability of the vertebral, local and segmental kyphosis in 120 traumatic lumbar and thoracic burst fractures: evaluation in lateral X-rays and sagittal computed tomographies. Eur Spine J 19:558–566
Alizadeh M, Kadir MRA, Fadhli MM et al (2013) The use of X-shaped cross-link in posterior spinal constructs improves stability in thoracolumbar burst fracture: A finite element analysis. J Orthop Res 31:1447–1454
Baroud G, Crookshank M, Bohner M (2006) High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine 31:2562–2568
Aubert K, Vendeuvre T, Lanel A, et al (2018) Kyphoplasty vs Stentoplasty: FE analysis of the risk of cement leakage. 8th World Congress of Biomechanics, Dublin, Ireland.
Yeom JS, Kim WJ, Choy WS et al (2003) Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br 85:83–89
Voggenreiter G (2005) Balloon kyphoplasty is effective in deformity correction of osteoporotic vertebral compression fractures. Spine 30:2806–2812
Berlemann U, Franz T, Orler R, Heini PF (2004) Kyphoplasty for treatment of osteoporotic vertebral fractures: a prospective non-randomized study. Eur Spine J 13:496–501
Klezl Z, Majeed H, Bommireddy R, John J (2011) Early results after vertebral body stenting for fractures of the anterior column of the thoracolumbar spine. Injury 42:1038–1042. https://doi.org/10.1016/j.injury.2011.04.006
Sato K, Kikuchi S, Yonezawa T (1999) In vivo intradiscal pressure measurement in healthy individuals and in patients with ongoing back problems. Spine 24:2468
Majd ME, Farley S, Holt RT (2005) Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J 5:244–255
Garnier L, Tonetti J, Bodin A et al (2012) Kyphoplasty versus vertebroplasty in osteoporotic thoracolumbar spine fractures. Short-term retrospective review of a multicentre cohort of 127 consecutive patients. Orthop Traumatol Surg Res 98:S112–S119. https://doi.org/10.1016/j.otsr.2012.03.018
Acknowledgements
The authors wish to thank Jeffrey Arsham, an American translator, for rereading and correction of the original English-language manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Vendeuvre is consultant for companies Medtronic (Dublin, Ireland), Safe Orthopaedics (Paris, France), Spineart (Geneva, Switzerland), and he has received previously research grants from company Medtronic for other research works. P. Rigoard is consultant for companies Medtronic (Dublin, Ireland), Boston Scientific (Malborough, MA, USA), ABBOTT (Chicago, IL, U.S.), and he has received previously research grants from company Medtronic for other research works. P. Pries is consultant for company Spineart (Geneva, Switzerland). S. Teyssédou is consultant for companies Medtronic (Dublin, Ireland) and Safe Orthopaedics (Paris, France). A. Germaneau is consultant for company Medtronic (Dublin, Ireland).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vendeuvre, T., Brossard, P., Pic, JB. et al. Vertebral balloon kyphoplasty versus vertebral body stenting in non-osteoporotic vertebral compression fractures at the thoracolumbar junction: a comparative radiological study and finite element analysis (BONEXP study). Eur Spine J 30, 3089–3098 (2021). https://doi.org/10.1007/s00586-021-06785-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06785-5