Abstract
Purpose
As more patients undergo lumbar spine surgery, novel interventions may improve physical and mental health outcomes. Few studies summarize the benefit of cognitive behavioral therapy (CBT) among lumbar spine surgery patients. This study collects randomized control trial data to investigate the influence of CBT on patient reported outcomes among lumbar spine surgery patients.
Methods
Our study used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses and a medical library expert assisted in searching PubMed/MEDLINE, Scopus, CINAHL, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, PsycINFO, and Google Scholar. We calculated standardized mean differences (SMD) to evaluate the effect size of CBT versus control groups with a sensitivity analysis.
Results
Our meta-analysis included seven studies with a total of 531 patients. The majority of included studies evaluated lumbar fusion, with preoperative CBT performed by physiotherapists. The largest effects were observed for overall quality of life (SMD = 0.55 [95% CI 0.05, 1.05], p < 0.001, I2 = 86.7%) and psychological outcomes (SMD = 0.61 [95% CI 0.28, 0.94], p < 0.001, I2 = 89.7%) though disability and pain outcomes also favored CBT intervention. Included studies demonstrated low overall bias but large heterogeneity. Sensitivity analysis demonstrated negligible study design differences and revealed moderators including CBT session frequency and final follow-up duration (p < 0.001).
Conclusion
Compared to usual care or alternative therapy control arms, CBT delivered the most improvement with overall quality of life and psychological outcomes. Among appropriately selected patients, CBT could improve perioperative disability, pain, quality of life, and psychological health following lumbar spine surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although numerous lower back pain investigations have established benefits of psychological interventions on various outcomes [1,2,3,4], the incremental benefit of cognitive behavioral therapy (CBT) among patients undergoing lumbar spine surgery remains unclear. Lumbar spine surgery is increasingly common and aims to alleviate chronic low back and radicular pain [5,6,7,8]. Despite the efficacy of many spine surgery procedures, postoperative recovery can be suboptimal, and patients may complain of unrelenting pain or poor functionality [9, 10]. Patient reports of minimal improvement and various complications are associated with reoperation rates as high as 23% at 8–10 years following lumbar decompression [11].
To improve surgical outcomes, there is a push toward optimizing modifiable risk factors through prehabilitation [12, 13]. This approach is thought to have potential advantages including shorter recovery times, less postoperative pain, greater independence, fewer complications, and reduced costs [14,15,16,17,18]. Prehabilitation includes improving preoperative levels of physical activity, anxiety reduction, and nutrition optimization [12], and it may improve presurgical beliefs, such as kinesophobia [19], catastrophizing [20], and fear avoidance. The aforementioned metrics have been observed to correlate with inferior outcomes following lumbar surgery [21,22,23,24,25,26,27]. CBT can target these beliefs to help patients succeed after surgery. The purpose of CBT is provide support to patients experiencing feelings of distress by teaching coping mechanisms [28]. CBT is a “problem-oriented” therapy that aims to teach patients cognitive reframing techniques to confront current distress [28]. CBT has demonstrated efficacy in treating depression [29, 30], generalized anxiety disorder, panic disorder, pain, and post-traumatic stress disorder [30].
Clinicians have started exploring CBT’s utility in primary care and in surgery. CBT has shown efficacy as a preoperative intervention for patients undergoing bariatric surgery [31, 32], cardiac surgery [33], and lumbar surgery [10]. Several randomized control trials (RCTs) have investigated pre- and postoperative CBT among lumbar spine surgical candidates. Results of these RCTs are varied, and no summary of these findings is available. The purpose of this study is to evaluate the effect of CBT on patient-reported outcome (PRO) improvement following lumbar spine surgery.
Methods
General study design
Each RCT was classified as comparing CBT outcomes to protocol therapeutic alternatives (PTA) or versus usual conventional (UC) pre- and postoperative care. PTAs involved specific interventions including education or exercises focused on improving outcomes following surgery. We evaluated pre- and postoperatively collected outcome instruments that were measured at baseline before beginning the intervention of interest, as well as short- and long-term postoperative time points. To preserve comparability to other CBT-focused systematic reviews, short-term time points were selected in the range of 2–3 months postoperatively. We collected the final outcome assessment in each study as our long-term outcome measurement. We assessed PROs in terms of five outcome categories: disability, back pain, leg pain, quality of life, and psychological outcomes. These outcomes were based on a variety of specific outcome measurement tools utilized among the included studies at the specified time points.
Search strategy and information resources
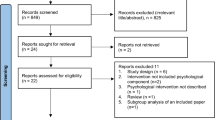
To gather relevant randomized studies with a reproducible study design, we used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA, Fig. 1). We consulted with a medical library and information sciences expert to conduct our search. Our reproducible search strategy was refined and recorded (“Appendix 1” in ESM). We searched the following seven databases in December 2019: PubMed/MEDLINE, Scopus, CINAHL, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, PsycINFO, and Google Scholar.
Study selection
Studies were selected based on their evaluation of a clinical impact of CBT on lumbar spine surgery outcomes. While descriptions of CBT can be heterogeneous [34], we defined CBT as an active psychologically informed intervention delivered by a trained therapist to identify and alter a patient’s maladaptive thoughts and behaviors [35]. Articles were included if they had the following characteristics: (1) if they were RCTs, (2) if patients underwent lumbar spine surgery, (3) if they included CBT interventions (pre- or postoperatively), and (4) if they contained PROs. The search was completed with both controlled vocabulary (i.e., MeSH terms) and keywords in the title or abstract. Studies were excluded if no English translation was available, if the article existed solely as a study protocol, if CBT was not conducted with a health professional, or if the study was only published in abstract form. We did not place restrictions on the publication date, geography, or participant age.
Data extraction and study quality assessment
We used Covidence (Melbourne, Australia) to synchronize our study assessment and evaluation. Duplicates were removed based on titles, abstracts, or matching identifiers. Each study was assessed by title and abstract by two independent reviewers (JMP, MSP). Full texts were then screened and inputted into a standardized form. We gathered the following information: demographics, surgical and psychological interventions (type, duration, timing, and provider), number of CBT sessions, and PROs (such as Oswestry Disability Index [ODI], Tampa Scale for Kinesiophobia [TSK], the Pain Catastrophizing Scale [PCS], and the European Quality of Life 5 Dimensions Questionnaire [EQ-5D]). To assess risk of bias (RoB), two reviewers used the Cochrane Back Review Group (CBRG) criteria, which evaluates selection bias, performance bias, detection bias, attrition bias, reporting bias, and all other biases [36]. Reviewers gave each category a rating of “low,” “high,” or “unclear.” When reviewers did not agree, a second review was conducted until consensus was reached.
Synthesis and analysis
Statistical analysis was performed with Stata SE 16.1 (College Station, TX, USA). The purpose of data synthesis was to numerically estimate the possible effect of CBT on spine surgery outcomes (disability, back pain, leg pain, quality of life, and psychological assessments). Secondary aims included exploring heterogeneity between studies and conducting sensitivity analysis. Standard deviations were collected and, if absent, were calculated [37, 38]. Forest plots visually depicted effect size, confidence intervals, and the effect of study heterogeneity. I2 statistics were used to describe the variability of effect size estimates, and previously established I2 statistic numerical cutoffs for heterogeneity estimation were used: Up to 40% heterogeneity may have been unimportant; 30–60% moderate heterogeneity; 50–90% substantial heterogeneity; and 75–100% considerable heterogeneity [39]. I2 statistics were compared with a Chi-squared test, and statistical significance was evaluated based on the associated p value (p < 0.005).
Our primary effect was the standardized mean difference (SMD) of CBT arms compared to control arms (e.g., PTA or UC) for all outcomes. Effect size was examined at three time points: preintervention baseline, postoperative short-term, and long-term. We used a random effects model with Cohen’s d estimators for our meta-analyses. Our outcome subgroup analysis was conducted according to five outcome categories: disability, back pain, leg pain, quality of life, and psychological assessment instruments. An outcome needed to be reported by at least three studies to be assessed in the meta-analysis. When necessary, outcome instrument scales were reversed by taking the mean score and subtracting from the maximum.
Sensitivity analysis was conducted by comparing the difference of effect size between the two groups of studies, i.e., those that assessed CBT vs PTA as compared to those that investigated CBT versus UC. A meta-regression assessed the influence of moderators on heterogeneity. Moderators that were assessed were the postoperative duration until final assessment, duration of CBT, number of CBT sessions, and instrument category.
Results
Systematic review
In total, our search returned 366 articles. After 125 duplicates were removed, 241 articles were screened by two independent reviewers, and 29 were selected for a full-text review (Fig. 1). The eleven studies eligible for qualitative analysis were conducted between 2003 and 2019 and included 735 lumbar spine surgery patients (Table 1). Of the eleven studies, seven evaluated lumbar fusion, three analyzed lumbar disk surgery, and one investigated laminectomy procedures. The primary intervention, CBT, was utilized preoperatively in four of the eleven studies. Postoperatively, ten of the eleven studies conducted some form of CBT. The total number of CBT sessions differed substantially, ranging from 3 to 18 sessions (Table 2). CBT sessions were completed in groups and individually in person, with the exception of one computer-based CBT study. Practitioner type varied, with the most frequent provider being physiotherapists (7 studies), followed by multidisciplinary teams (3 studies) (Table 2). The most frequently investigated PROs were disability (82%, ODI), pain (55%, visual analog scale), quality of life (55%, EQ-5D, 55% Short Form-36), pain catastrophizing (45%, Pain Catastrophizing Scale), and fear of movement (45%, TSK). PROs demonstrated improvement with CBT intervention (vs. control) in six of eleven studies (Table 3).
Quality assessment
Study population sample sizes ranged from 86 to 130, with an average age ranging from 42.8 to 58.4 years. Reporting styles and quality ranged considerably, with over one-third of all quality assessment (37.6%) ratings were either “poor” or “unclear.” Further analysis of risk of bias, assessment revealed that 91% (n = 10) of the included studies carried a low risk of bias and 9% (n = 1) carried a unclear risk of bias due to inadequate generation of a randomized sequence. In terms of risk of bias due to inadequate concealment of allocations prior to assignment, 100% of the included studies carried a low risk of selection bias. Performance bias due to inadequate blinding of participants and personnel carries the highest risk with 91% (n = 10) of studies carrying a high risk and only 9% (n = 1) carrying a low risk. Risk of detection bias due to inadequate blinding of outcome assessors was variable with 54.5% (n = 6) carrying a low risk, 9% (n = 1) carrying an unclear risk, and 45.5% (n = 4) carrying a high risk. Review of the included studies also demonstrated a more favorable risk of attrition bias with 64% (n = 7) demonstrating a low risk and 36% (n = 4) with an unclear risk of attrition bias due to handling of incomplete outcome data. Reporting bias due to selective outcome reporting had 91% (n = 10) of studies carrying a low risk and 9% (n = 1) with an unclear risk. Lastly, 27.3% (n = 3) of studies carried a low risk, 54.5% (n = 6) carried an unclear risk, and 18.2% (n = 2) carried a low risk of bias due to other sources. The most common bias category to incur a “high” risk rating was “blinding of participants and personnel.” Seven studies had two or more categories with a “high” risk of bias. A detailed summary of study bias is shown in Fig. 2.
On second review, four of the 11 studies originally included were removed due to a high risk of bias. Three of the removed studies reported results from the same RCT [40,41,42]. The investigators disclosed that treatment integrity within this RCT was likely compromised due to “issues” with adherence to study protocol [40]. The fourth study excluded was removed because it evaluated an computer-automated CBT application [43].
Meta-analysis
A total of seven studies from the previous eleven were included in the meta-analysis with 531 patients. Five compared CBT to UC and two compared PTA. The SMD improved from baseline measurements during both short-term and long-term evaluations for all five outcome categories (e.g., disability, back pain, leg pain, quality of life, and psychological) for PTA and CCG groups (Table 4). Forest plots of all long-term outcome categories indicated effect sizes that favored CBT in comparison with control groups (Figs. 3, 4).
All studies included in the meta-analysis reported at least one instrument for disability, back pain, quality of life, and psychological. Only one study did not report leg pain. Four psychological outcomes were reported with a high enough frequency (n ≥ 3) to be compared in further subgroup analysis. Psychological subgroups included catastrophizing, fear of movement, global mental health, and self-efficacy. At the short-term follow-up, the majority of studies reported outcome difference effects favoring CBT over control groups (small: 20% [n = 7], moderate: 6% [n = 2], large: 34% [n = 12]). At long-term follow-up, the number of outcomes reflecting effect sizes favoring CBT increased (small: 31% [n = 11], moderate: 23% [n = 8], large: 20% [n = 7]).
At short-term follow-up, while all outcomes favored CBT, disability (SMD = − 0.73 [95% CI − 1.46, 0.01], p < 0.001, I2 = 93.5%) and back pain (SMD = − 0.42 [95% CI − 0.98, 0.14], p < 0.001, I2 = 89.5%) had the largest effect sizes for outcome differences. At the long-term follow-up, psychological health outcomes (SMD = 0.61 [95% CI 95% CI 0.28, 0.94], p < 0.001, I2 = 89.7%) and overall quality of life (SMD = 0.55 [95% CI 0.05, 1.05], p < 0.001, I2 = 86.7%) outcome differences were most suggestive of a statistically significant effect size. The largest effect sizes within the psychological outcome subgroup analysis favoring CBT were observed for differences in fear of movement (SMD = 0.67 [95% CI 0.02, 1.32], p < 0.001, I2 = 91.7%) and self-efficacy (SMD = 0.27 [95% CI 0.02, 0.52], p < 0.001, I2 = 13.2%).
Comparing CBT versus PTA versus UC
Our analysis of the two study designs (e.g., CBT vs. PTA and CBT vs. UC) revealed that both designs favored CBT interventions for all assessed outcome groups (Table 4). In particular, CBT demonstrated the largest effect compared to UC for disability at the short-term time point (SMD = − 1.05 [95% CI − 2.15, 0.05], I2 = 95.01). The largest effect of CBT compared to PTA was demonstrated for back pain at the short-term time point (SMD = − 0.54 [95% CI − 1.41, 0.34], I2 = 86.72). At the long-term time point, CBT demonstrated its largest effect compared to UC for back pain (SMD = − 0.87 [95% CI − 2.45, 0.71], I2 = 97.48), whereas, compared to PTA, the largest effect by CBT was observed for disability (SMD = − 0.39 [95% CI − 0.68, − 0.10], I2 = 0.00). Only leg pain could not be assessed among PTA studies due to insufficient reporting.
When assessing the long-term follow-up for CBT versus UC studies, considerable heterogeneity was observed for disability (I2 = 95.80), back pain (I2 = 97.48), leg pain (I2 = 94.13), and psychological outcomes (global mental health, fear of movement, and catastrophizing) (I2 = 93.82; all p < 0.001, all). For long-term follow-up of CBT versus PTA studies, heterogeneity among studies was assessed as unimportant. When assessing all studies included in the meta-analysis, considerable heterogeneity was observed among disability (I2 = 92.75), back pain (I2 = 95.80), leg pain (I2 = 91.47), psychological outcomes overall (I2 = 89.71), and within the global mental health, fear of movement, and catastrophizing subgroups (p < 0.001, all).
Sensitivity analysis
When incorporating our study design comparison into a sensitivity analysis, our analysis revealed no significant differences among subgroups for disability, back pain, leg pain, quality of life or overall psychological outcomes (Fig. 3). Among the psychological subgroups, the PTA versus UC subgroups were only observed to have a significant group difference for global mental health (p < 0.001, Fig. 4). When analyzing all outcomes as a part of a meta-regression, the only two statistically significant moderators were the frequency of CBT sessions and months until final follow-up (p < 0.001).
Discussion
At the time of our search, this is the only study that summarizes RCT findings regarding the effect of CBT on outcomes following lumbar spine surgery. The results suggest that, when combined with lumbar spine surgery, CBT is associated with a clinically significant improvement in postsurgical outcomes as compared to UC or PTA. Pooled effect of our meta-analysis indicated that of all included RCT outcomes (n = 34), the majority demonstrated significant effect sizes favoring CBT interventions at both short-term (62% [n = 21]) and long-term (76% [n = 26]) intervals. While the average final follow-up time period of the studies varied from 6 months to 3 years following surgery, our meta-analysis suggests that the effects of CBT are sustained over time.
Within our meta-analysis, there was considerable variation regarding the type, interval, and frequency of outcome reporting. All seven studies reported disability with ODI. Back pain was also reported by seven studies and was variously measured among studies using VAS back, low back pain rating scale (LBPRS), back pain inventory (BPI), and the numerical rating scale (NRS). Leg pain was reported by six of the seven studies in our meta-analysis and all studies reported outcomes analogous to their back-pain counterparts (i.e., studies utilizing VAS back to report back pain used VAS Leg to report leg pain). While each study reported quality of life outcomes, all were unique (e.g., EQ-5D VAS, EQ-5D Index, SF-12, Patient-reported functioning, and SF-36). Psychological outcomes were reported with the most variability. Even among category subgroups, reported outcomes differed (e.g., global mental health, self-efficacy, catastrophizing, pain avoidance, etc.).
Although each investigation used validated outcomes, overall quality might have been improved with adherence to current RCT literature guidance. For example, the initiative on Methods, Measurement, and Pain Assessment in Clinical Trials guidelines recommends specific validated outcomes to assess global areas including pain, physical functionality, emotional functionality, etc. [44, 45]. While three of the RCTs included in the meta-analysis mentioned the recruitment protocols adhering to the Consolidated Standards of Reporting Trials guidelines, heterogeneity might have been reduced further with better adherence to these guidelines [46].
Relation to other literature and strengths
The results of this study are similar to previous studies that have demonstrated improvement of PROs after CBT intervention [47, 48]. While previous meta-analyses have investigated CBT in relation to chronic back pain [49,50,51], our study is the first to specifically analyze the efficacy of CBT interventions on PROs in the setting of lumbar spine surgery. Furthermore, this meta-analysis only reviewed RCTs that were prescreened to evaluate bias using the CBRG criteria. Although the reviewed studies utilized differing CBT methodologies, most sessions were led by physiotherapists, which may have controlled for a number of potential confounders (provider type, training, experience level, etc.). Similar PRO investigations also allowed for comparative improvement among treatment and control groups.
There was substantial heterogeneity with regard to the implementation of CBT in each study. Among eleven articles in the systematic review, four included preoperative CBT and all of the articles made use of postoperative CBT. The overall number of sessions varied from as few as three sessions to 18 sessions. Session lengths varied between studies and within each protocol, and ranged from 30-min to 3 h. Settings of CBT ranged from in person to over the phone and one-on-one sessions with a therapist to group therapy with multiple therapists. Finally, the overall treatment duration ranged from 4 to 12 weeks. With such a heterogeneous pool of CBT protocols, it is challenging to assess which treatment variables were most influential. Our sensitivity and meta-analysis revealed that frequency of CBT sessions was a statistically significant moderator for overall outcome effect size. These findings are generally aligned with current research, though less heterogeneity between studies may have allowed for a greater number of variable comparisons.
In general, research has demonstrated that increased frequencies of psychotherapy sessions can result in greater symptom improvement [52,53,54]. Among patients with depression, a meta-analysis found that symptoms of depression were inversely proportional to the number of CBT sessions per week [55]. In current mental healthcare practice, CBT is typically held once a week. However, the original CBT manual recommends beginning with two sessions per week [35]. When looking at the studies in this meta-analysis, only one study conducted biweekly CBT sessions, and interestingly, this study demonstrated the greatest overall PRO improvement effects [56]. Our results suggest CBT’s utility as an evidence-based treatment for depression may also be applied to surgical candidates. Furthermore, this may indicate a similarity between the core issues typically addressed by CBT and those associated with poor postsurgical outcomes.
The modes of CBT delivery can have numerous implications on outcome effect. CBT can be administered one-on-one or in group settings. Both can have potential advantages and disadvantages [57]. One-on-one therapy is ideal when both patient and provider are supportive and therapeutically aligned [58]. Particularly in the context of therapist availability and insurance policy limits, the resource-intensive nature of one-on-one therapy can hinder the application. None of the assessed RCTs utilized psychiatrists for individual sessions. With customized training, however, providers of differing backgrounds can administer CBT [59]. While having more providers qualified to administer CBT could improve access to care, varied technical training might also contribute to an array of CBT methodologies and limit outcome analysis.
Moreover, the impact of therapist experience on CBT outcomes is both nuanced and controversial. Although therapist experience level is often considered to influence the effect of CBT on anxiety, depression, and pain, several studies have revealed that less experienced therapists can still achieve meaningful clinical results [60, 61]. Others have observed that more years of general CBT clinical experience has a significant influence on lessening patient anxiety or depressive symptoms [62,63,64].
Group therapy is both appealing financially and importantly addresses the social isolation that many patients feel in the perioperative setting [57]. On functional magnetic resonance imaging, for example, feelings of social isolation have been associated with the same brain regions that activate during physical pain experiences [65]. Stigma imposed by both the public and the self that the individual may be socially undesirable or unacceptable may be a barrier to participation in group therapy [66]. One therapeutic possibility could be restructuring preoperative group therapy to include education and realistic expectations of postoperative rehabilitation. This could facilitate group therapy motifs while potentially reframing the purpose of the sessions to diminish the stigma associated with a “group therapy” session. The social interactions fostered during group CBT sessions have helped people gain comfort with a common experience and focus on aspects of life outside of their pain experience [67].
This meta-analysis and the studies reviewed had several strengths and limitations. Our review expands on research regarding the influence of CBT on lower back pain by examining a surgical population. This study included an information science expert to assemble a reproducible study search string, incorporated multidisciplinary input, adhered to the PRISMA guidelines, assessed RoB, and conducted a meta-analysis on clinically relevant outcomes in RCTs. The investigations we assessed should be commended for adhering to a sequence generation protocol, strong allocation concealment, and low-risk selective outcome reporting. Another strength is that they assessed patient samples using an intent-to-treat methodology.
Limitations
Although CBT appears to be beneficial, this is only one approach to psychotherapy. One limitation is that our search focused on CBT and did not include other potentially useful therapy mediums such as operant behavioral therapy, biofeedback, mindfulness, or meditation. Additionally, it is important to consider how to maximize CBT effectiveness and cost utility. Although it would have been helpful to evaluate the effect of CBT during the preoperative time period compared to the postoperative time period, neither of the CBT versus PTA investigations utilized preoperative CBT. This limited our ability to discern whether a difference in effects occurred due to the PTA study design or the lack of preoperative CBT. Further, since none of the included studies examined preoperatively administered CBT without subsequent postoperative CBT interventions, it is difficult to assess the independent contributions of preoperative vs postoperative CBT on improvements in PROs.
While our study focused on lumbar spine surgery, outcomes including disability, pain, quality of life, and psychological measures have complex perioperative determinants. Given the numerous surgical variables that could be related to these outcomes, quality may have been added if the RCTs reported perioperative characteristics including surgical levels, operative duration, blood loss, complications, surgical history, or comorbidities. Without this information, the ability of our investigation to control for the effects of these characteristics on outcomes between groups and/or studies was limited. For example, if study groups differed significantly on the basis of comorbidities, these might present a significant confounding effect. Other limitations may have stemmed from the lack of therapist heterogeneity and short, non-specific CBT training regimens. This may limit the generalizability of the results to CBT interventions facilitated by other types of practitioners. To some extent, all of the studies reviewed utilized physiotherapists to administer CBT and only two of the studies included clinical psychologists. None of the investigations attempted to discuss potential advantages associated with therapist training.
Conclusion
Our meta-analysis indicates that CBT arms had improved lumbar spine surgery outcomes as compared to UC or PTA. Additionally, CBT session frequency may be associated with CBT efficacy. Overall, the quality of the literature is high with a number of published RCTs and generally low risk of bias, although the available studies regarding CBT in lumbar spine patients are relatively heterogeneous. While we could not determine whether pre- or postoperative CBT is more beneficial, the majority of the RCTs in our meta-analysis utilized some combination. Our observations suggest that both pre- and postoperative CBT approach may be effective and expand on the benefits of CBT in association with lumbar spine health. Among appropriately selected patients, use of pre- and postoperative CBT, alone or in combination, could become an important asset to optimize patients before surgery to improve disability, pain, quality of life, and mental health.
Data availability statement
All data generated or analyzed during this study are included in this published article.
References
Bono CM, Dougherty P, Rahmathulla G, et al (2020) Medical and psychological treatment section. In: Scott Kreiner D, Matz P (eds) Evidence-based clinical guidelines for multidisciplinary spine care: diagnosis and treatment of low back pain. North American Spine Society, Burr Ridge
Smeets RJEM, Vlaeyen JWS, Hidding A, Kester ADM, van der Heijden GJMG, van Geel ACM, Knottnerus JA (2006) Active rehabilitation for chronic low back pain: cognitive-behavioral, physical, or both? First direct post-treatment results from a randomized controlled trial [ISRCTN22714229]. BMC Musculoskelet Disord 7:5. https://doi.org/10.1186/1471-2474-7-5
Pincus T, Anwar S, McCracken LM, McGregor A, Graham L, Collinson M, McBeth J, Watson P, Morley S, Henderson J, Farrin AJ (2015) Delivering an optimised behavioural intervention (OBI) to people with low back pain with high psychological risk; results and lessons learnt from a feasibility randomised controlled trial of contextual cognitive behavioural therapy (CCBT) vs. physiotherapy. BMC Musculoskelet Disord 16:147. https://doi.org/10.1186/s12891-015-0594-2
Linden M, Scherbe S, Cicholas B (2014) Randomized controlled trial on the effectiveness of cognitive behavior group therapy in chronic back pain patients. J Back Musculoskelet Rehabil 27:563–568. https://doi.org/10.3233/BMR-140518
Dhillon KS (2016) Spinal fusion for chronic low back pain: a “magic bullet” or wishful thinking? Malays Orthop J 10:61–68
Yaszemski MJ (2006) United States trends in lumbar fusion surgery for degenerative conditions. Yearbook Orthoped 2006:256–257
Harris IA, Dao ATT (2009) Trends of spinal fusion surgery in Australia: 1997 to 2006. ANZ J Surg 79:783–788. https://doi.org/10.1111/j.1445-2197.2009.05095.x
Strömqvist B, Fritzell P, Hägg O, Jönsson B (2009) SWESPINE, the Swedish Spine Register: The 2009 Report. Swedish Society of Spinal Surgeons, Falun
Jonsson E, Olafsson G, Fritzell P, Hägg O, Borgström F (2017) A profile of low back pain: treatment and costs associated with patients referred to orthopedic specialists in Sweden. Spine 42:1302–1310. https://doi.org/10.1097/BRS.0000000000002089
Archer KR, Devin CJ, Vanston SW, Koyama T, Phillips SE, Mathis SL, George SZ, McGirt MJ, Spengler DM, Aaronson OS, Cheng JS, Wegener ST (2016) Cognitive-behavioral-based physical therapy for patients with chronic pain undergoing lumbar spine surgery: a randomized controlled trial. J Pain 17:76–89. https://doi.org/10.1016/j.jpain.2015.09.013
Lurie JD, Tosteson TD, Tosteson A, Abdu WA, Zhao W, Morgan TS, Weinstein JN (2015) Long-term outcomes of lumbar spinal stenosis: eight-year results of the spine patient outcomes research trial (SPORT). Spine 40:63–76. https://doi.org/10.1097/BRS.0000000000000731
Le Roy B, Selvy M, Slim K (2016) The concept of prehabilitation: What the surgeon needs to know? J Visc Surg 153:109–112. https://doi.org/10.1016/j.jviscsurg.2016.01.001
Lundberg M, Archer KR, Larsson C, Rydwik E (2019) Prehabilitation: the Emperor’s new clothes or a new arena for physical therapists? Phys Ther 99:127–130. https://doi.org/10.1093/ptj/pzy133
Ditmyer MM, Topp R, Pifer M (2002) Prehabilitation in preparation for orthopaedic surgery. Orthop Nurs 21:43–51. https://doi.org/10.1097/00006416-200209000-00008
Wright S, Wiechula R, McLiesh P (2016) The effectiveness of prehabilitation for adults having elective surgery: a systematic review protocol. JBI Database System Rev Implement Rep 14: 78–92. https://doi.org/10.11124/jbisrir-2016-2460
Delgado-López PD, Rodríguez-Salazar A, Castilla-Díez JM (2019) “Prehabilitation” in degenerative spine surgery: a literature review. Neurocirugia 30:124–132. https://doi.org/10.1016/j.neucir.2018.11.008
Gometz A, Maislen D, Youtz C, Kary E, Gometz EL, Sobotka S, Choudhri TF (2018) The Effectiveness of prehabilitation (Prehab) in both functional and economic outcomes following spinal surgery: a systematic review. Cureus 10:e2675. https://doi.org/10.7759/cureus.2675
Nielsen PR, Jørgensen LD, Dahl B, Pedersen T, Tønnesen H (2010) Prehabilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil 24:137–148. https://doi.org/10.1177/0269215509347432
Lundberg MKE, Styf J, Carlsson SG. A psychometric evaluation of the Tampa Scale for Kinesiophobia—from a physiotherapeutic perspective. Physiother Theory Pract 20:121–133. https://doi.org/10.1080/09593980490453002
Abbott AD, Tyni-Lenné R, Hedlund R (2011) Leg pain and psychological variables predict outcome 2–3 years after lumbar fusion surgery. Eur Spine J 20:1626–1634. https://doi.org/10.1007/s00586-011-1709-6
Mannion AF, Elfering A, Staerkle R, Junge A, Grob D, Dvorak J, Jacobshagen N, Semmer NK, Boos N (2007) Predictors of multidimensional outcome after spinal surgery. Eur Spine J 16:777–786. https://doi.org/10.1007/s00586-006-0255-0
Archer KR, Wegener ST, Seebach C, Song Y, Skolasky RL, Thornton C, Khanna AJ, Riley LH (2011) The effect of fear of movement beliefs on pain and disability after surgery for lumbar and cervical degenerative conditions. Spine 36:1554–1562. https://doi.org/10.1097/BRS.0b013e3181f8c6f4
Archer KR, Phelps KD, Seebach CL, Song Y, Riley LH III, Wegener ST (2012) Comparative study of short forms of the Tampa Scale for Kinesiophobia: fear of movement in a surgical spine population. Arch Phys Med Rehabil 93:1460–1462. https://doi.org/10.1016/j.apmr.2012.03.024
Archer KR, Seebach CL, Mathis SL, Riley LH III, Wegener ST (2014) Early postoperative fear of movement predicts pain, disability, and physical health six months after spinal surgery for degenerative conditions. Spine J 14:759–767. https://doi.org/10.1016/j.spinee.2013.06.087
den Boer JJ, Oostendorp RA, Beems T, Munneke M, Evers AW (2006) Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioral factors. Pain 123:45–52. https://doi.org/10.1016/j.pain.2006.02.008
Hasenbring MI, Plaas H, Fischbein B, Willburger R (2006) The relationship between activity and pain in patients 6 months after lumbar disc surgery: do pain-related coping modes act as moderator variables? Eur J Pain 10:701–701. https://doi.org/10.1016/j.ejpain.2005.11.004
Seebach CL, Kirkhart M, Lating JM, Wegener ST, Song Y, Riley LH 3rd, Archer KR (2012) Examining the role of positive and negative affect in recovery from spine surgery. Pain 153:518–525. https://doi.org/10.1016/j.pain.2011.10.012
Fenn K, Byrne M (2013) The key principles of cognitive behavioural therapy. InnovAiT 6:579–585. https://doi.org/10.1177/1755738012471029
Lynch D, Laws KR, McKenna PJ (2010) Cognitive behavioural therapy for major psychiatric disorder: does it really work? A meta-analytical review of well-controlled trials. Psychol Med 40:9–24. https://doi.org/10.1017/S003329170900590X
Butler AC, Chapman JE, Forman EM, Beck AT (2006) The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev 26:17–31. https://doi.org/10.1016/j.cpr.2005.07.003
Gade H, Friborg O, Rosenvinge JH, Småstuen MC, Hjelmesæth J (2015) The impact of a preoperative cognitive behavioural therapy (CBT) on dysfunctional eating behaviours, affective symptoms and body weight 1 year after bariatric surgery: a randomised controlled trial. Obes Surg 25:2112–2119. https://doi.org/10.1007/s11695-015-1673-z
Paul L, van Rongen S, van Hoeken D, Deen M, Klaassen R, Biter LU, Hoek HW, van der Heiden C (2015) Does cognitive behavioral therapy strengthen the effect of bariatric surgery for obesity? Design and methods of a randomized and controlled study. Contemp Clin Trials 42:252–256. https://doi.org/10.1016/j.cct.2015.04.001
Hwang B, Eastwood J-A, McGuire A, Chen B, Cross-Bodán R, Doering LV (2015) Cognitive behavioral therapy in depressed cardiac surgery patients: role of ejection fraction. J Cardiovasc Nurs 30:319–324. https://doi.org/10.1097/JCN.0000000000000155
David D, Cristea I, Hofmann SG (2018) Why cognitive behavioral therapy is the current gold standard of psychotherapy. Front Psychiatry 9:4. https://doi.org/10.3389/fpsyt.2018.00004
Beck AT (1979) Cognitive therapy of depression. Guilford Press, New York
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC, Cochrane Bias Methods Group, Cochrane Statistical Methods Group (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/https://doi.org/10.1136/bmj.d5928
Higgins JPT, Li T, Deeks JJ (2019) Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (eds) Cochrane handbook for systematic reviews of interventions, 2nd edn. Wiley, Chichester, pp 143–176
Luo D, Wan X, Liu J, Tong T (2018) Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res 27:1785–1805. https://doi.org/10.1177/0962280216669183
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2019) Cochrane handbook for systematic reviews of interventions, 2nd edn. Wiley, Chichester
Ostelo RW, de Vet HC, Vlaeyen JW, Kerckhoffs MR, Berfelo WM, Wolters PM, van den Brandt PA (2003) Behavioral graded activity following first-time lumbar disc surgery: 1-year results of a randomized clinical trial. Spine 28:1757–1765. https://doi.org/10.1097/01.brs.0000083317.62258.e6
Ostelo RW, Goossens ME, de Vet HC, van den Brandt PA (2004) Economic evaluation of a behavioral-graded activity program compared to physical therapy for patients following lumbar disc surgery. Spine 29:615–622. https://doi.org/10.1097/01.brs.0000115130.42394.0b
Ostelo RW, de Vet HC, Berfelo MW, Kerckhoffs MR, Vlaeyen JW, Wolters PM, van den Brandt PA (2003) Effectiveness of behavioral graded activity after first-time lumbar disc surgery: short term results of a randomized controlled trial. Eur Spine J 12:637–644. https://doi.org/10.1007/s00586-003-0560-9
Strøm J, Nielsen CV, Jørgensen LB, Andersen NT, Laursen M (2018) A web-based platform to accommodate symptoms of anxiety and depression by featuring social interaction and animated information in patients undergoing lumbar spine fusion: a randomized clinical trial. Spine J. https://doi.org/10.1016/j.spinee.2018.11.011
Dworkin RH, Turk DC, Farrar JT et al (2005) Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 113:9–19. https://doi.org/10.1016/j.pain.2004.09.012
Dworkin RH, Turk DC, Wyrwich KW et al (2008) Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain 9:105–121. https://doi.org/10.1016/j.jpain.2007.09.005
Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (2012) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg 10:28–55. https://doi.org/10.1016/j.ijsu.2011.10.001
Nicholls JL, Azam MA, Burns LC, Englesakis M, Sutherland AM, Weinrib AZ, Katz J, Clarke H (2018) Psychological treatments for the management of postsurgical pain: a systematic review of randomized controlled trials. Patient Relat Outcome Meas 9:49–64. https://doi.org/10.2147/PROM.S121251
Archer KR, Motzny N, Abraham CM, Yaffe D, Seebach CL, Devin CJ, Spengler DM, McGirt MJ, Aaronson OS, Cheng JS, Wegener ST (2013) Cognitive-behavioral-based physical therapy to improve surgical spine outcomes: a case series. Phys Ther 93:1130–1139. https://doi.org/10.2522/ptj.20120426
Richmond H, Hall AM, Copsey B, Hansen Z, Williamson E, Hoxey-Thomas N, Cooper Z, Lamb SE (2015) The effectiveness of cognitive behavioural treatment for non-specific low back pain: a systematic review and meta-analysis. PLoS ONE 10:e0134192. https://doi.org/10.1371/journal.pone.0134192
Hoffman BM, Papas RK, Chatkoff DK, Kerns RD (2007) Meta-analysis of psychological interventions for chronic low back pain. Health Psychol 26:1–9. https://doi.org/10.1037/0278-6133.26.1.1
Henschke N, Ostelo RW, van Tulder MW, Vlaeyen JWS, Morley S, Assendelft WJJ, Main CJ (2010) Behavioural treatment for chronic low-back pain. Cochr Database System Rev. https://doi.org/10.1002/14651858.cd002014.pub3
Abramowitz JS, Foa EB, Franklin ME (2003) Exposure and ritual prevention for obsessive-compulsive disorder: effects of intensive versus twice-weekly sessions. J Consult Clin Psychol 71:394–398. https://doi.org/10.1037/0022-006x.71.2.394
Herbert JD, Rheingold AA, Gaudiano BA, Myers VH (2004) Standard versus extended cognitive behavior therapy for social anxiety disorder: a randomized-controlled trial. Behav Cogn Psychother 32:131–147. https://doi.org/10.1017/S1352465804001171
Reese RJ, Toland MD, Hopkins NB (2011) Replicating and extending the good-enough level model of change: considering session frequency. Psychother Res 21:608–619. https://doi.org/10.1080/10503307.2011.598580
Cuijpers P, Huibers M, Ebert DD, Koole SL, Andersson G (2013) How much psychotherapy is needed to treat depression? A metaregression analysis. J Affect Disord 149:1–13. https://doi.org/10.1016/j.jad.2013.02.030
Monticone M, Ferrante S, Teli M, Rocca B, Foti C, Lovi A, Brayda Bruno M (2014) Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J 23:87–95. https://doi.org/10.1007/s00586-013-2889-z
Hanscom DA, Brox JI, Bunnage R (2015) Defining the role of cognitive behavioral therapy in treating chronic low back pain: an overview. Glob Spine J 5:496–504. https://doi.org/10.1055/s-0035-1567836
Lim J-A, Choi S-H, Lee WJ et al (2018) Cognitive-behavioral therapy for patients with chronic pain: implications of gender differences in empathy. Medicine 97:e10867. https://doi.org/10.1097/MD.0000000000010867
Magidson JF, Weisberg RB (2014) Implementing cognitive behavioral therapy in specialty medical settings. Cogn Behav Pract 24:367–371. https://doi.org/10.1016/j.cbpra.2014.08.003
Hiltunen AJ, Kocys E, Perrin-Wallqvist R (2013) Effectiveness of cognitive behavioral therapy: An evaluation of therapies provided by trainees at a university psychotherapy training center. Psych J 2:101–112. https://doi.org/10.1002/pchj.23
Öst L-G, Karlstedt A, Widén S (2012) The effects of cognitive behavior therapy delivered by students in a psychologist training program: an effectiveness study. Behav Ther 43:160–173. https://doi.org/10.1016/j.beth.2011.05.001
Podell JL, Kendall PC, Gosch EA, Compton SN, March JS, Albano A-M, Rynn MA, Walkup JT, Sherrill JT, Ginsburg GS, Keeton CP, Birmaher B, Piacentini JC (2013) Therapist factors and outcomes in CBT for anxiety in youth. Prof Psychol Res Pr 44:89–98. https://doi.org/10.1037/a0031700
Huppert JD, Bufka LF, Barlow DH, Gorman JM, Shear MK, Woods SW (2001) Therapists, therapist variables, and cognitive-behavioral therapy outcome in a multicenter trial for panic disorder. J Consult Clin Psychol 69:747–755. https://doi.org/10.1037/0022-006X.69.5.747
James IA, Blackburn IM, Milne DL, Reichfelt FK (2001) Moderators of trainee therapists’ competence in cognitive therapy. Br J Clin Psychol 40:131–141. https://doi.org/10.1348/014466501163580
Eisenberger NI, Lieberman MD, Williams KD (2003) Does rejection hurt? An FMRI study of social exclusion. Science 302:290–292. https://doi.org/10.1126/science.1089134
Shechtman Z, Vogel D, Maman N (2010) Seeking psychological help: a comparison of individual and group treatment. Psychother Res 20:30–36
Lamb SE, Mistry D, Lall R, Hansen Z, Evans D, Withers EJ, Underwood MR (2012) Group cognitive behavioural interventions for low back pain in primary care: extended follow-up of the Back Skills Training Trial (ISRCTN54717854). Pain 153:494–501. https://doi.org/10.1016/j.pain.2011.11.016
Funding
No funds were received in support of this work. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Parrish, J.M., Jenkins, N.W., Parrish, M.S. et al. The influence of cognitive behavioral therapy on lumbar spine surgery outcomes: a systematic review and meta-analysis. Eur Spine J 30, 1365–1379 (2021). https://doi.org/10.1007/s00586-021-06747-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-021-06747-x