Abstract
Purpose
To identify age-related changes and the relationship between upper and lower cervical sagittal alignment and the range of motion (ROM).
Methods
A total of 600 asymptomatic volunteers were enrolled. There were 50 males and 50 females in each decade of life between the third and the eighth. The O–C2 angle and the C2–7 angle were measured using the neutral radiographs of the cervical spine. ROM was assessed by measuring the difference in alignment in the neutral, flexion, and extension positions.
Results
The mean O–C2 angle in the neutral position was 14.0° lordotic. The mean ROM of the O–C2 angle was 23.1°. The mean C2–7 angle in the neutral position was 14.3° lordotic. The mean ROM of the C2–7 angle was 56.0°. The O–C2 angle was 16.1° in the third decade and gradually decreased to 11.4° in the eighth decade. There were no significant age-related changes in the ROM of the O–C2 angle. The C2–7 angle was 7.2° in the third decade and gradually increased to 20.8° in the eighth decade, and the ROM gradually decreased with increasing age. Significant negative correlation was observed between O–C2 angle and C2–7 angle.
Conclusion
The O–C2 angle gradually decreased and the C2–7 angle increased with age. The ROM of the O–C2 angle did not change, but the ROM of the C2–7 angle decreased with age. The upper and lower cervical spine showed different age-related changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With aging, changes in the cervical spine gradually increase and lead to cervical degenerative disease, such as cervical spondylosis and disk herniation. In the aging population, the proportion of patients with cervical degenerative disease can increase. Cervical corrective surgery aims to maintain normal cervical alignment. The radiological parameters of the sagittal balance of the thoracic and lumbar spine are well defined [1,2,3]. However, only few studies have assessed the sagittal balance of the cervical spine; age-related changes in cervical sagittal alignment have rarely been evaluated.
Some studies have shown the importance of local cervical sagittal alignment affecting the other parameters of global sagittal alignment [4, 5]. In addition, cervical sagittal imbalance has been considered a predictor of the poor outcomes of cervical decompression surgery [6, 7]. Furthermore, increasing cervical lordosis has been found to be correlated to neck disability index score [8]. Based on the abovementioned information, the radiographic standard values for cervical alignment parameters are extremely important clinically. The normative values of cervical alignment differ between males and females and change with age. However, few studies investigating cervical sagittal alignment, particularly upper cervical alignment, have included a large cohort with an even age and gender distribution.
The current study aimed to investigate the standard values for the normal alignment and range of motion (ROM) of the upper and lower cervical spine in males and females in each decade of life between the third (20s) and the eighth (70s). Moreover, age-related changes and the relationship between the alignment of the upper and lower cervical spine were evaluated using the radiographic data of 600 healthy individuals.
Materials and methods
This study was approved by the institutional review board of our institution. In total, 600 asymptomatic Japanese volunteers (300 males and 300 females) provided informed consent and participated in this study. The exclusion criteria were individuals with a history of brain or spinal surgery, symptoms related to sensory or motor disorders (such as numbness, clumsiness, motor weakness, and gait disturbance), or severe neck pain. Pregnant women and individuals presented with symptoms after a motor vehicle accident or received worker’s compensation were also excluded. Among the volunteers, 50 males and 50 females were recruited for each decade of life between the third and the eighth.
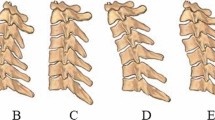
All individuals underwent lateral radiography of the neck while in the neutral, flexion, and extension positions. The film–tube distance was set at 1.5 m. Lateral X-ray images were obtained while the individuals were standing and in a straightforward position. Flexion and extension radiography were performed with the neck in maximum flexion and extension position. The O–C2 and C2–7 angles were measured using these images (Fig. 1). Flexion and extension ROMs were calculated by subtracting the value of the angle in the neutral position from those in the flexion and extension positions. The total ROM was calculated by adding the flexion and extension ROMs. The O–C2 angle was defined as the angle between the McGregor line [9] and the inferior aspect of the axis, and the C2–7 angle as the angle between the inferior aspect of the axis and vertebral body C7. All images were transferred to the computer as DICOM data. Each parameter was measured by experienced radiation technologists using an imaging software (Osiris4; Icestar Media Ltd., Essex, the UK). The intra-observer and inter-observer variations of the O–C2 angle and C2–7 angle were estimated using the reliability statistics by intraclass correlation coefficient (ICC) from the values of the angles of 60 subjects measured by two independent observers (TI and HK), and the mean intra- and the inter-observer ICCs were 0.96 and 0.92 in O–C2 angles, 0.98 and 0.98 in C2–7 angles, respectively.
BellCurve for Excel (Social Survey Research Information Co., Ltd.) was used for statistical analysis. All values were expressed as mean ± standard deviation. The Mann–Whitney U test was used to analyze the differences between the male and female groups. The Jonckheere–Terpstra test was utilized to evaluate the trends of the age-related changes in O–C2 and C2–7 angles. The Pearson correlation coefficient was used to examine the correlations between the O–C2 angle and C2–7 angle. A p value < 0.05 was considered statistically significant.
Results
The mean O–C2 angle of all individuals was 13.9° ± 7.79° (13.7° ± 7.7° in males, 14.1° ± 7.7° in females), and the mean total ROM of O–C2 angle (O–C2 ROM) was 23.1° ± 8.4° (22.3° ± 8.2° in males, 23.8° ± 8.6° in females) (Table 1). The flexion and extension O-C2 ROMs are depicted in Table 1. The mean flexion O–C2 ROM was significantly higher in females than in males. However, the mean O–C2 angle and the total O–C2 ROM did not significantly differ between males and females.
The mean C2–7 angle of all individuals was 14.3° ± 12.7° (15.7° ± 12.7° in males, 12.8° ± 9.12° in females), and the mean total ROM of C2–7 angle (C2–7 ROM) was 56.0° ± 16.40° (52.7° ± 15.8° in males, 59.4° ± 16.4° in females) (Table 1). The flexion and extension C2–7 ROMs are depicted in Table 1. The mean total C2–7 angle was significantly higher in males than in females, and females had a significantly higher total and extension C2–7 ROMs than males.
Age-related changes in measured angles are shown in Table 2. The O–C2 angle decreased significantly with age in both males and females (p < 0.05) (Fig. 2). However, no significant differences were observed between males and females in terms of the measured angles in any decade of life. Meanwhile, the total O-C2 ROM did not change significantly with age (Table 3, Fig. 2), and no significant differences were observed between males and females in terms of the total O–C2 ROM in any decade of life. The C2–7 angle increased significantly with age (p < 0.05) (Table 2, Fig. 3), and a significant difference was noted in the angle between males and females only at the third decade of life. The total C2–7 ROM significantly decreased with age (p < 0.05) (Table 4, Fig. 3). In almost all decades, except for the fourth, significant differences were observed between males and females.
The correlation coefficients between the O–C2 and C2–7 angles were r = − 0.41 (p < 0.01) in all individuals, r = − 0.37 (p < 0.01) in males, and r = − 0.44 (p < 0.01) in females (Fig. 4). A significant correlation was observed between the O–C2 and C2–7 angle.
Discussion
Only few studies have assessed the normative values for the upper cervical spine and the relationship between the upper and lower cervical spine. Nojiri et al. [10] have investigated the normative values and the age-related changes in the upper and lower cervical spine. They found that both the O–C2 and C2–7 angles changed significantly with aging and that there was a negative correlation between the angles of the upper and lower cervical spine. This finding is similar to our results. Although their study included 313 asymptomatic volunteers, the number of participants for each decade varied. In addition, they did not investigate the ROM of the upper and lower cervical spine. This study first investigated the normative values for alignment, ROM of the upper and lower cervical spine, and age-related changes in 600 healthy individuals (50 males and 50 females) in each decade of life between the third and eighth.
Previous studies about cervical alignment focused on lower alignment, including the C2–7 angle. Therefore, only few studies assessed the upper cervical spine. However, Hardacker et al. [11] have reported that the largest percentage of cervical lordosis is localized at the C1–2 segment (32.2° ± 7.0°) and that the lordosis at the C2–7 segment was only 9.6°. Several studies [12, 13] have assessed the loss of lower cervical lordosis in the occiput–C2 fusions, with excessive hyperlordosis observed at the occiput–C2 fusions. Thus, the upper cervical alignment is extremely critical in total cervical alignment.
Matsunaga et al. [14] have investigated 240 healthy volunteers (120 males and 120 females), and results showed that the O–C2 angle gradually decreased after the fifth decade of life. Yukawa et al. [15] have reported that the C2–7 angle gradually increased, whereas the total ROMs gradually decreased with age in over 1200 asymptomatic participants. Our report supports these results. That is, this study showed that the O–C2 angle decreased, whereas the C2–7 angle increased with age (Figs. 2, 3). In addition, the O-C2 ROM did not change. However, the C2–7 ROM decreased with age (Figs. 2, 3). The parameters of the upper and lower cervical spine had opposing changes. Several studies [2, 16, 17] have reported that thoracic kyphosis increased significantly with age. Therefore, compensatory lordotic changes may be observed in the cervical spine. However, these age-related changes were only observed in the lower cervical spine, and the upper cervical spine was not affected by these changes. The flexion O–C2 ROM and the extension C2–7 ROM were higher in females than in males, suggesting that cervical mobility was higher in females than in males. Furthermore, a possible explanation for this difference between upper and lower cervical ROMs is that C2–7 angles in females were lower and O–C2 angles in females were slightly higher than in males, resulting in more extension mobility in lower cervical spine and flexion mobility in upper cervical spine.
Lee et al. [18] have reported that the thoracic inlet angle is strongly correlated to the T1 slope, and significant correlation coefficients were observed between the T1 slope and C2–7 angle; the C2–7 angle and O–C2 angle; and the O–C2 angle and cranial offset. This correlation was expressed as a linear chain linking the parameters of T1 to the cranium. In the current study, a weak but statistically significant negative correlation was observed between the O–C2 and C2–7 angles (Fig. 4). These results indicate that the O–C2 angle may be affected by the age-related changes and gradual increases in C2–7 angle with age.
Several studies about the C2–7 ROM have shown that it decreases with increasing age [1, 3, 15, 19]. Degenerative changes in the facet joints, intervertebral disks, and back muscles were involved in the decrease in C2–7 ROM. Meanwhile, the number of studies about the ROM of the O–C2 angle is extremely low. In the current study, these angles did not change with age. The degenerative changes did not affect the O–C2 ROM, unlike the C2–7 ROM.
This study had several limitations. First, this study only used the data of Japanese volunteers. In addition, we have no information about their occupations, which may affect cervical alignment. However, the dataset generated in our study was large enough for most evaluations. Second, this study included only asymptomatic subjects, raising possibility that ROMs and lordotic angles may be overestimated due to the lack of neck pain, especially in elderly patients. However, we could describe the true parameters that did not affected by pain. Third, the parameters of global sagittal alignment, including that of the thoracic spine, were not evaluated. Because only asymptomatic healthy volunteers were included in this study, whole-spine radiography was difficult to perform. Nevertheless, the results of the current study can be used as baseline data for the sagittal balance and ROMs of the upper and lower cervical spine in various clinical conditions.
Conclusion
The normal alignment and ROM values of the upper and lower cervical spine were obtained using the radiographic data of 600 asymptomatic participants. The O–C2 angle decreased, whereas the C2–7 angle increased with age. The ROMs of the O–C2 angle did not change. However, that of the C2–7 angle decreased with age. Thus, a significant correlation exists between the O–C2 angle and C2–7 angle.
References
Ferlic D (1962) The range of motion of the “normal” cervical spine. Bull Johns Hopkins Hosp 110:59–65
Fon GT, Pitt MJ, Thies AC Jr (1980) Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol 134:979–983. https://doi.org/10.2214/ajr.134.5.979
Lind B, Sihlbom H, Nordwall A, Malchau H (1989) Normal range of motion of the cervical spine. Arch Phys Med Rehabil 70:692–695
Lee SH, Son ES, Seo EM, Suk KS, Kim KT (2015) Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J 15:705–712. https://doi.org/10.1016/j.spinee.2013.06.059
Alijani B, Rasoulian J (2020) The sagittal balance of the cervical spine: radiographic analysis of interdependence between the occipitocervical and spinopelvic alignment. Asian Spine J. https://doi.org/10.31616/asj.2019.0165
Sakai K, Yoshii T, Hirai T, Arai Y, Torigoe I, Tomori M, Sato H, Okawa A (2016) Cervical sagittal imbalance is a predictor of kyphotic deformity after laminoplasty in cervical spondylotic myelopathy patients without preoperative kyphotic alignment. Spine (Phila Pa 1976) 41:299–305. https://doi.org/10.1097/brs.0000000000001206
Kim TH, Lee SY, Kim YC, Park MS, Kim SW (2013) T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 38:E992–E997. https://doi.org/10.1097/brs.0b013e3182972e1b
Iyer S, Nemani VM, Nguyen J, Elysee J, Burapachaisri A, Ames CP, Kim HJ (2016) Impact of cervical sagittal alignment parameters on neck disability. Spine (Phila Pa 1976) 41:371–377. https://doi.org/10.1097/brs.0000000000001221
Mc GM (1948) The significance of certain measurements of the skull in the diagnosis of basilar impression. Br J Radiol 21:171–181. https://doi.org/10.1259/0007-1285-21-244-171
Nojiri K, Matsumoto M, Chiba K, Maruiwa H, Nakamura M, Nishizawa T, Toyama Y (2003) Relationship between alignment of upper and lower cervical spine in asymptomatic individuals. J Neurosurg 99:80–83. https://doi.org/10.3171/spi.2003.99.1.0080
Hardacker JW, Shuford RF, Capicotto PN, Pryor PW (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 22:1472–1480 ;discussion 1480
Yoshida G, Kamiya M, Yoshihara H, Kanemura T, Kato F, Yukawa Y, Ito K, Matsuyama Y, Sakai Y (2010) Subaxial sagittal alignment and adjacent-segment degeneration after atlantoaxial fixation performed using C-1 lateral mass and C-2 pedicle screws or transarticular screws. J Neurosurg Spine 13:443–450. https://doi.org/10.3171/2010.4.SPINE09662
Yoshimoto H, Ito M, Abumi K, Kotani Y, Shono Y, Takada T, Minami A (2004) A retrospective radiographic analysis of subaxial sagittal alignment after posterior C1–C2 fusion. Spine (Phila Pa 1976) 29:175–181. https://doi.org/10.1097/01.brs.0000107225.97653.ca
Matsunaga S, Onishi T, Sakou T (2001) Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976) 26:161–165
Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T (2012) Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: radiographic data from over 1,200 asymptomatic subjects. Eur Spine J 21:1492–1498. https://doi.org/10.1007/s00586-012-2167-5
Oe S, Togawa D, Nakai K, Yamada T, Arima H, Banno T, Yasuda T, Kobayasi S, Yamato Y, Hasegawa T, Yoshida G, Matsuyama Y (2015) The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine (Phila Pa 1976) 40:1487–1494. https://doi.org/10.1097/brs.0000000000001071
Yoshida G, Yasuda T, Togawa D, Hasegawa T, Yamato Y, Kobayashi S, Arima H, Hoshino H, Matsuyama Y (2014) Craniopelvic alignment in elderly asymptomatic individuals: analysis of 671 cranial centers of gravity. Spine (Phila Pa 1976) 39:1121–1127. https://doi.org/10.1097/brs.0000000000000360
Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES (2012) The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech 25:E41–E47. https://doi.org/10.1097/BSD.0b013e3182396301
Gore DR, Sepic SB, Gardner GM (1986) Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 11:521–524
Funding
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Informed consent
The Institutional Review Board in our institution approved this study, and written informed consent was obtained from each patient before study participation or surgery.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Inoue, T., Ito, K., Ando, K. et al. Age-related changes in upper and lower cervical alignment and range of motion: normative data of 600 asymptomatic individuals. Eur Spine J 29, 2378–2383 (2020). https://doi.org/10.1007/s00586-020-06547-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-020-06547-9