Abstract
Purpose
CT myelography has been used since 1976 to diagnose neural compression in the axial skeleton. With the advent of routine MRI, its role in accurately diagnosing neural compression has been questioned as its normal appearances are not defined in the study. In this study, we examine a series of CT myelograms to define the normal appearances of the neural elements of the spine.
Methods
The CT myelograms of patients with unilateral symptoms were examined by four independent physicians. The lateral extent of contrast was examined and recorded. Concordance between the recorded extents was assessed using kappa scores.
Results
Thirty-six scans were reviewed. Kappa analysis shows that there is a fair agreement in the lateral extent of contrast at L1, L3 and L4. At L2 and L5, agreement is slight.
Conclusion
The interpretation of CT myelography shows significant interobserver variability. As a result, the usefulness of this diagnostic tool can be questioned, and if misinterpreted, it could lead to questionable diagnoses and inadvertently erroneous management if used in isolation.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Computed tomographic myelography (CTM) has been used since 1976 to investigate the morphology of the spinal neurological structures [1]. Despite the prevalence of magnetic resonance imaging (MRI), CTM has been used to demonstrate neural compression due to herniated nucleus pulposus (HNP) and central, lateral recess, subarticular or foraminal stenosis. Assessments of the technique show that it has a sensitivity of between 57 and 92% for HNP and 62% in nerve root compression [2,3,4,5,6].
With the increasing availability and capabilities of MRI, CTM has fallen into increasing disuse. Several studies have shown that MRI is more sensitive in detecting neural compression and obligatory dural puncture and ionising radiation is not required, meaning that MRI is thought to be safer [2, 7, 8]. However, with increasing use of instrumentation CTM remains available in the investigation of spinal pathology. The technique has found use in post-operative scans because of its reduced vulnerability to distortion caused by instrumentation, when dynamic stenosis is suspected where standing myelograms can emphasises mobile segments and where MRI is contraindicated [8,9,10].
Despite its potential uses, there is a paucity of information regarding the interpretation of a normal CTM. In the absence of a definition of normal appearances, it is impossible to define abnormal findings and consequently to plan treatment using imaging studies. There is, as yet, no definition of the normal appearances of the neural structures seen on CTM, and so, its clinical utility could be considered limited. In this case series, we seek to define whether the normal appearances of the nerve roots on a lumbar CT myelogram can be defined.
Method
The study was carried out in a single tertiary referral centre in the UK for both orthopaedic care and neurosurgical spinal care. Using the search function of the picture archiving and communication system (PACS, Synapse, Fujifilm, Bedford, UK), all adult (aged ≥ 18 years) patients who underwent CTM between 1 July 2011 and 2 February 2018 were identified.
The clinical information recorded in the investigation request was scrutinised to establish the patient’s symptoms and clinical findings, and patients were included only if they had undergone a CTM to investigate only unilateral lumbar radiculopathy. We considered that if the contralateral side of the patient was asymptomatic, it should be considered anatomically normal. Patients who had undergone any previous spinal surgery, had any bilateral symptoms at any lumbar level, were investigated for central canal stenosis or had no coronal images available were excluded from the analysis.
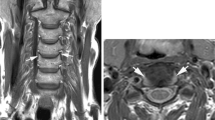
The coronal sequences of myelogram images of each of the patients included were reviewed. The lateral extent of contrast relative to the L1, L2, L3, L4 and L5 pedicle was measured on the side of the spine identified as asymptomatic by the clinical records.
Four investigators reviewed the images (a consultant spinal surgeon, a consultant musculoskeletal radiologist, a senior trainee in orthopaedic spinal surgery and a foundation year-one doctor). Data were recorded on a spreadsheet (Microsoft Excel, Seattle, USA). No collusion between reviewers was permitted. The lateral extent of the contrast was recorded as zone 1–4 using the schematic shown in Fig. 1.
The completed data set was analysed using a kappa score to assess for the concordance between the data recorded by each reviewer.
Results
One hundred and sixty-eight adult patients underwent CTM between 1 July 2011 and 2 February 2018. Ninety-six patients underwent investigation for bilateral symptoms or central canal stenosis. Three patients had insufficient images to assess the lumbar spine. Of the remaining 69 cases, 33 had undergone previous spinal surgery, leaving 36 suitable for inclusion into the analysis (Fig. 2). The frequency of the lateral extent of the contrast as assessed by each investigator is evident in Fig. 3.
Each reviewer’s assessment of the lateral extent of contrast spread was compared to each of the other investigators through unweighted kappa analysis. The results are shown in Table 1. The majority of kappa scores showed slight or fair agreement between reviewers, with B and D (senior trainee in orthopaedic spinal surgery and FY1 doctor) showing the highest degree of agreement.
The combined kappa analysis shows that slight agreement between all reviewers was achieved at L2 and L5. Fair agreement was observed at the remaining levels (Table 2).
Discussion
CTM remains in use in the evaluation of spinal pathology where MRI is not practical. The results shown here suggest that there is poor agreement in the interpretation of results. As a consequence, it may well be that patients are receiving inappropriate management based on misleading clinical decisions. Using the definitions published by Landis and Koch in 1977, our results show that there is fair agreement in the lateral extent of contrast at L1, L3 and L4 [11]. At L2 and L5, the agreement is slight. At higher resolution, it is evident that there is very little agreement between each of the individual reviewers (Table 1). The individual kappa values suggest that there may be development in individual skills of interpreting images as experience progresses, though we noted that the seniormost investigators both of whom examine the outputs of CTM regularly showed low agreement in their assessments. An alternative, and perhaps more likely, explanation given the lack of agreement between senior specialists is that the images are challenging to interpret, and as such, it is reasonable to assume that different treatments would be offered by clinicians with different degrees of experience for similar clinical pictures as a result, with consequent differing outcomes. As a result, it is difficult to consistently describe what should be considered as normal CTM findings throughout the lumbar spine in the adult population with sufficient accuracy to make robust treatment decisions.
MRI has become the gold standard for evaluating neural compression within the spine. Clearly, in some cases these are not practical or possible because of a range of possible reasons, including pacemaker implantation, the presence of surgical clips or claustrophobia. As a result, we need to have an option for advanced imaging that does not rely on high-strength magnetic fields. To date, CT has been the only option available, with CTM being a development of the standard protocol in an effort to better identify the compressive lesion. Unfortunately, despite the case for its use, CTM is not free from complications. The procedure requires technical skill to perform and unavoidably involves inserting both a needle and contrast into the dura. As a result of its invasive nature, significant complications have been identified in up to 10–15% of patients, where post-procedure headaches, meningitis and infection have been described [9].
Further to the safety aspects of CTM, its accuracy has been questioned. Analyses have shown that CTM underestimates root compression in up to 38% of patients where compression was confirmed intraoperatively, and Penning showed that 22/62 scans showed no abnormality despite cervical radicular symptoms [5, 12].
These studies, combined with our new data showing that image interpretation is difficult and unreliable, show that the utility of CTM may well be very limited to select patients where surgeons have a clear equipoise in their planning, rather than confirming an existing strategy. In a development of CTM, dynamic CTM has become a technique established to evaluate cerebrospinal fluid leak, and there is now some evidence that this specific technique adds to the diagnostic yield of MRI and influences surgical planning [13, 14]. In this study, we examined only static CTM studies, and future work should include dynamic studies in their analysis. Interpretation of CTM is generally understood to be challenging; however, this is the first investigation that quantifies both this and the clinically relevant variation in image assessment.
Conclusion
Although CTM has a use in modern surgical practice through its use where MRI is contraindicated or when the spine has been heavily instrumented, its interpretation shows that there are variability in the anatomy of the dura and significant interobserver variability in image interpretation. As a result, the usefulness of this diagnostic tool can be questioned, and if misinterpreted, it could lead to questionable diagnoses and inadvertently erroneous management if used in isolation. We suggest that a study examining the role of CTM in central stenosis, extra-foraminal or far lateral neural compression could identify a use for this technique in these specific pathologies.
References
Di Chiro G, Schellinger D (1976) Computed tomography of spinal cord after lumbar intrathecal introduction of metrizamide (computer-assisted myelography). Radiology 120:101–104. https://doi.org/10.1148/120.1.101
Kim JH, van Rijn RM, van Tulder MW, Koes BW, de Boer MR, Ginai AZ, Ostelo R, van der Windt D, Verhagen AP (2018) Diagnostic accuracy of diagnostic imaging for lumbar disc herniation in adults with low back pain or sciatica is unknown; a systematic review. Chiropr Man Ther 26:37. https://doi.org/10.1186/s12998-018-0207-x
Jackson RP, Becker GJ, Jacobs RR, Montesano PX, Cooper BR, McManus GE (1989) The neuroradiographic diagnosis of lumbar herniated nucleus pulposus: I. A comparison of computed tomography (CT), myelography, CT-myelography, discography, and CT-discography. Spine (Phila Pa 1976) 14:1356–1361
Gillstrom P, Ericsson K, Hindmarsh T (1986) A comparison of computed tomography and myelography in the diagnosis of lumbar disc herniation. Arch Orthop Trauma Surg 106:12–14
Bartynski WS, Lin L (2003) Lumbar root compression in the lateral recess: MR imaging, conventional myelography, and CT myelography comparison with surgical confirmation. AJNR Am J Neuroradiol 24:348–360
Bischoff RJ, Rodriguez RP, Gupta K, Righi A, Dalton JE, Whitecloud TS (1993) A comparison of computed tomography-myelography, magnetic resonance imaging, and myelography in the diagnosis of herniated nucleus pulposus and spinal stenosis. J Spinal Disord 6:289–295
Jackson RP, Cain JE Jr, Jacobs RR, Cooper BR, McManus GE (1989) The neuroradiographic diagnosis of lumbar herniated nucleus pulposus: II. A comparison of computed tomography (CT), myelography, CT-myelography, and magnetic resonance imaging. Spine (Phila Pa 1976) 14:1362–1367
Fortin JD, Wheeler MT (2004) Imaging in lumbar spinal stenosis. Pain Phys 7:133–139
Kretzschmar K (1998) Degenerative diseases of the spine. The role of myelography and myelo-CT. Eur J Radiol 27:229–234
Ozdoba C, Gralla J, Rieke A, Binggeli R, Schroth G (2011) Myelography in the age of mri: why we do it, and how we do it. Radiol Res Pract 2011:329017. https://doi.org/10.1155/2011/329017
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Penning L, Wilmink JT (1986) Specificity of CT myelographic findings in cervical nerve root symptoms. Neurosurg Rev 9:99–101
Amrhein TJ, Kranz PG (2019) Spontaneous intracranial hypotension: imaging in diagnosis and treatment. Radiol Clin North Am 57:439–451. https://doi.org/10.1016/j.rcl.2018.10.004
McKay G, Torrie PA, Bertram W, Landham P, Morris S, Hutchinson J, Watura R, Harding I (2017) Myelography in the assessment of degenerative lumbar scoliosis and its influence on surgical management. Korean J Spine 14:133–138. https://doi.org/10.14245/kjs.2017.14.4.133
Acknowledgements
Thanks go to Adrian Sayers for his invaluable assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Brett Rocos, David R S Evans, Brathaban Rajayogeswaran and M. John Hutchinson declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rocos, B., Evans, D.R.S., Rajayogeswaran, B. et al. The normal appearance of CT myelograms. Eur Spine J 29, 1087–1091 (2020). https://doi.org/10.1007/s00586-019-06287-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06287-5