Abstract
Purpose
This systematic review and meta-analysis of all available evidence was performed to assess the safety and efficacy of surgery for lumbar stenosis and spondylolisthesis in patients 80 years or older versus those younger than 80 years.
Methods
A search of the literature was conducted in PubMed/MEDLINE, EMBASE and the Cochrane Collaboration Library. Relevant studies comparing the clinical outcomes of lumbar surgery in octogenarians and younger patients were selected according to the eligibility criteria. The predefined endpoints were extracted and meta-analysed from the identified studies.
Results
Data from 16 observational studies including 374,197 patients were included in the final analysis. The pooled data revealed that patients 80 years or older had a significantly higher incidence of overall complication, mortality, readmission and longer length of hospital stay than younger patients. There was a similar improvement in the clinical symptoms (Oswestry Disability Index and pain) of patients in the two groups. No significant differences in overall wound complication, reoperation rate, operative time and intraoperative blood loss were found between the groups.
Conclusions
Our results revealed that the clinical improvement in pain and disability did not significantly differ according to age, although the patients aged 80 years or older had increased incidences of mortality and complication than younger patients. Age alone is not a contraindication for lumbar surgery in very old patients. A careful preoperative evaluation, proper patient selection and appropriate surgical approach are important to achieve successful surgical outcomes.
Graphic abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With advances in public health and continued medical progress, the elderly has been a fast-growing segment of the population in industrialized countries [1]. This will lead to a proportional increase in age-related diseases such as lumbar disc herniation, stenosis and spondylolisthesis. Degenerative changes in the lumbar spine can cause chronic low back pain and sensory and motor deficits in the lower extremities, often leading to limitations in the activities of daily living [2]. When conservative treatment fails to ameliorate the patient’s symptoms, surgical decompression is the recommended method [3]. With increased ageing of the population, many elderly wish to maintain functional status, a situation that has contributed to a greater need for spinal surgery as an option to improve the quality of life [4]. The number of surgical procedures performed in the elderly with degenerative lumbar disease, particularly spinal fusion procedures, has increased massively in the past decade [5].
However, the elderly population, especially those older than 80 years, are more likely to have a higher comorbidity and osteoporosis burden, often with multiple systems involved [6]. The complexity of the health status may increase the risks of complications, poor functional outcomes and mortality after surgery in patients aged 80 years and older [7]. When surgery is performed on an octogenarian patient, the risks and benefits have to be evaluated. However, the benefits and safety of lumbar surgery in octogenarian patients remain controversial [8]. To date, no meta-analysis has specifically addressed the effect that patient age has on outcomes after surgery for lumbar stenosis and spondylolisthesis. Therefore, to address this issue, a meta-analysis regarding the post-operative outcomes after lumbar spinal surgery in octogenarians and younger patients with lumbar stenosis or spondylolisthesis was performed to assess whether surgery is as safe and effective in patients 80 years or older as it is among younger patients.
Materials and methods
Literature search strategy
Our meta-analysis was executed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement and was registered at International Prospective Register of Systematic Reviews (registration number CRD42018103777).
A systematic computerized literature search was conducted using PubMed/MEDLINE, EMBASE and the Cochrane Collaboration Library from their dates of inception to July 2019. To achieve maximum sensitivity of the search strategy and identify all studies, the following search terms were used in several logical combinations: “octogenarians”, “elderly”, “aged, 80 and over”, “lumbar stenosis”, “lumbar spondylolisthesis”, “surgical procedures, operative”, “spinal fusion”, “arthrodesis”, “decompression, surgical” and “laminectomy”. The details of the search strategy are listed in Supplemental Table 1. The reference lists of all included articles and reviews were also searched to identify additional relevant publications.
Inclusion criteria
Two reviewers (H.F.L. and S.Y.L.) screened the search results independently. Discrepancies between reviewers were resolved by discussion and consensus. Eligible comparative studies that compared surgical outcomes among octogenarians and younger patients who underwent surgery for lumbar spinal stenosis or spondylolisthesis were included in the current systematic review. Other inclusion criteria included the following: (1) the study included age group specifications (or obtainable from the presented data); (2) the study showed at least one of the desirable outcome measures and matched their population groups; and (3) each group comprised at least 15 patients. All publications were limited to human subjects and were written in English.
Exclusion criteria
The following criteria were used to exclude studies: (1) studies without any comparison between octogenarians and younger patients; (2) minimally invasive spine surgery, such as microscopic surgery, microendoscopic surgery, or percutaneous surgery; (3) incomplete data or unclear distinction between the two different age groups; and (4) abstracts, conference presentations, editorials, case reports, review articles, biomechanical studies, animal experiments and cadaveric studies.
Data extraction and assessment of study quality
Two investigators (H.F.L. and S.Y.L.) extracted the data independently and cross-checked them mutually. A database was created from the selected studies with the following data: author, country, study design, publication year, patients (age, sex, diagnosis and number of included patients), surgical information, complication, mortality, reoperation, readmission, hospital stay, operative time, blood loss, numerical rating scale (NRS), visual analogue score (VAS), Low Back Pain Bothersomeness Scale (LBPBS) and Oswestry Disability Index (ODI).
The quality of comparative observational studies was assessed using the Newcastle–Ottawa Scale (NOS) [9], as recommended by the Cochrane Non-Randomized Studies Methods Working Group. The quality of selected studies was assessed according to the selection quality, comparability and exposure. The maximum score was 9, and a high-quality study was defined as a total score of 6 to 9. Two reviewers (H.F.L. and S.Y.L.) independently evaluated the selected studies. Inconsistencies in assessment were resolved by consensus.
Statistical analysis
Statistical analyses were conducted using Review Manager (RevMan) Version 5.3 software (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Analysis was performed using the random effects models to account for differences in the study methodology, patient characteristics and surgical practice. The Mantel–Haenszel random effects model was used for dichotomous variables calculating the odds ratio (OR) between groups. The inverse variance random effects model was applied for continuous variables calculating the mean difference between groups. The weighted mean difference (WMD) was applied to analyse continuous variables if the outcome measurements in all studies were conducted on the same scale. Otherwise, the standardized mean difference (SMD) was used. Both were reported with 95% confidence intervals (CI), and P < 0.05 was considered statistically significant. The heterogeneity between studies was estimated using Chi-square-based Q statistics (significant at P < 0.1) and I2 test. I2 > 50% was considered as substantial heterogeneity. Sensitivity analysis was performed to check the robustness of the meta-analysis findings by the leave-one-out approach. Publication bias was assessed by the Egger’s tests and funnel plot, which were carried out in STATA 14.0 (StataCorp LP, College Station, TX, USA).
Results
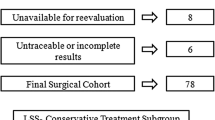
A flow diagram of the detailed search process used is shown in Fig. 1. The literature search yielded 1986 unique articles. A further screening of titles and abstracts was conducted, and 69 studies were considered potentially relevant to our review. According to the inclusion criteria, 16 comparative observational studies were identified in this study, of which four were prospective cohort studies [10,11,12,13] and 12 were retrospective cohort studies [5, 8, 14,15,16,17,18,19,20,21,22,23].
The total number of patients was 374,197, comprising 36,084 octogenarians and 338,113 younger patients. The mean age ranged from 82.2 to 83 years in the octogenarian group compared with 59.5 to 75 years in the younger group (six studies). Patients with lumbar stenosis alone or combined with lumbar spondylolisthesis were included in the present analysis. Surgical procedures included lumbar laminectomy, laminotomy, discectomy, posterolateral lumbar fusion (PLF), posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF) or anterior lumbar interbody fusion (ALIF). The NOS scores in 16 studies were in the range from 6 to 9. Therefore, they were considered high methodological quality. The baseline characteristics and NOS scores of the included articles are presented in Table 1.
Quantitative data synthesis
Patient characteristics and preoperative health status
The pooled data of the preoperative characteristics and comorbidities are presented in Table 2. Patients aged younger than 80 years had significantly more smokers (OR 0.24; P = 0.008) and a higher comorbidity rate for diabetes mellitus (OR 0.91; P < 0.001). There was a significantly larger BMI in younger patients (WMD: − 1.82; P = 0.008). As expected, patients older than 80 years showed significantly higher comorbidity rates for hypertension (OR 2.45; P < 0.001), chronic pulmonary disease (OR 1.13; P < 0.001) and congestive heart failure (OR 1.95; P < 0.001). The fragile physical condition was also reflected by a higher American Society of Anesthesiologists score (ASA ≥ 3). Octogenarian patients were nearly threefold more likely to have an ASA score ≥ 3 than the younger group (OR 2.97; P < 0.001).
Post-operative complications
Eleven studies adequately reported post-operative complications. The overall complication rate (intraoperative and post-operative complications) for the octogenarians was 12.6% compared with 10.0% for the younger patients. The overall complication rate was significantly increased in octogenarian patients (OR 1.53; 95% CI 1.42, 1.64; I2 = 40%; P < 0.00001) (Fig. 2). We also assessed the complications of specific surgical procedures. Three studies in which the surgical approach was decompression alone reported overall complications. There was a significantly higher overall complication rate in octogenarians than in younger patients (9.3% vs 5.0%; OR 1.63; 95% CI 1.12, 2.38; I2 = 0%; P = 0.01). Four studies in which the surgical approach was decompression plus fusion reported overall complications. Octogenarians also showed a significantly higher overall complication rate than younger patients (15.8% vs 10.0%; OR 1.69; 95% CI 1.38, 2.09; I2 = 47%; P < 0.00001) (Fig. 3).
Eleven studies reported wound complications, including haematoma, haemorrhage, wound disruption, wound infection and nonhealing surgical wounds. The overall wound complication rates were the same (2.1%) in both groups. No significant difference was found between octogenarians and younger patients (OR 1.09; 95% CI 0.98, 1.21; I2 = 0%; P = 0.10) (Fig. 2).
Regarding the main complication types, octogenarian patients were more likely to develop urinary tract infection (OR 2.51; 95% CI 1.67, 3.77; I2 = 53%; P < 0.0001), pneumonia (OR 1.68; 95% CI 1.51, 1.87; I2 = 0%; P < 0.00001), deep venous thrombosis (OR 1.61; 95% CI 1.42, 1.84; I2 = 0%; P < 0.00001), pulmonary embolism (OR 1.40; 95% CI 1.17, 1.66; I2 = 0%; P = 0.0002), myocardial infarction (OR 2.41; 95% CI 1.22, 4.76; I2 = 39%; P = 0.01) and dural tear (OR 1.63; 95% CI 1.04, 2.56; I2 = 0%; P = 0.03) than younger patients (Figs. 4 and 5). However, the rates of wound infection (OR 1.12; 95% CI 0.99, 1.26; I2 = 0%; P = 0.07), wound haematoma (OR 1.56; 95% CI 0.31, 7.85; I2 = 0%; P = 0.59) and nerve injury (OR 1.95; 95% CI 0.31, 12.13; I2 = 0%; P = 0.47) were similar between the groups (Fig. 5).
Mortality, reoperation and readmission
In total, 11 of the 16 studies reported the incidences of in-hospital and 90-day post-operative mortality among octogenarian patients versus younger patients. The difference in the mortality rate was statistically significant, showing that the mortality in octogenarians was three times higher than that in younger patients (0.61% vs 0.17%; OR 3.28; 95% CI 2.54, 4.25; I2 = 46%; P < 0.00001) (Fig. 6).
The readmission outcome was reported in three studies. There was a significantly higher readmission rate in octogenarians than in younger patients (10.8% vs 6.9%; OR 1.46; 95% CI 1.26, 1.68; I2 = 10%; P < 0.00001) (Fig. 6). Four studies reported the reoperation outcome. No significant difference was found between the groups (OR 0.45; 95% CI 0.19, 1.04; I2 = 0%; P = 0.06) (Fig. 6).
Functional outcomes
The data regarding ODI improvement scores were available in three studies. No significant difference was found between octogenarian and younger patients (WMD: − 1.54; 95% CI − 4.10, 1.02; I2 = 0%; P = 0.24) (Fig. 7). Pain scores were assessed based on the VAS, NRS or LBPBS scores. Back pain improvement scores were reported in three studies. No significant difference was found between the two groups (SMD: 0.03; 95% CI − 0.11, 0.17; I2 = 0%; P = 0.71) (Fig. 8). Three studies had sufficient data to extract leg pain improvement scores. Improvement scores were also similar between the two groups (SMD: 0.08; 95% CI − 0.07, 0.24; I2 = 0%; P = 0.29) (Fig. 8).
Other perioperative outcomes
Hospital stay was reported in six studies. There was a significantly longer hospital stay in octogenarians than in younger patients (WMD: 0.48; 95% CI 0.36, 0.60; I2 = 56%; P < 0.00001) (Fig. 7). The data regarding the operative time were available in four studies, and intraoperative blood loss was available in three studies. There were no significant differences in the operative time (WMD: 1.57; 95% CI − 9.37, 12.52; I2 = 43%; P = 0.78) and blood loss (WMD: − 9.25; 95% CI − 104.61, 86.11; I2 = 0%; P = 0.85) between the two groups (Fig. 7).
Sensitivity analysis and publication bias
Sensitivity analysis was performed by serially omitting an individual study and pooling the remaining studies. The sensitivity analysis results showed little change in the pooled ORs and did not alter the overall results of the analysis, suggesting the high stability of the meta-analysis (Supplemental Figs. 1–5). Publication bias was assessed for the overall complication, wound complication, mortality, reoperation, readmission, ODI improvement, back pain improvement, leg pain improvement, hospital stay, operative time and blood loss. All Egger’s P values were greater than 0.1, indicating the absence of publication bias. All of the Egger’s p values and funnel plots are shown in Supplemental Figs. 6–16.
Discussion
As the proportion of octogenarian patients with lumbar stenosis increases, surgeons are often faced with clinical decision-making regarding treatment with insufficient evidence. Octogenarians are frequently associated with comorbidities and a poor health status; thus, they represent a population with uncertain benefits and the risks of treatment [24, 25]. The increasing number of published literature on the treatment outcome of lumbar surgery in octogenarian patients has posed conflicting evidence [10,11,12,13, 26,27,28,29]. The present study is the first meta-analysis to evaluate the difference between patients 80 years or older and patients younger than 80 years with respect to preoperative characteristics and post-operative outcomes after lumbar surgery, which included 36,084 octogenarians and 338,113 younger patients from 16 published studies. With our synthesis of the current data available, the pooled analysis revealed the following: (1) octogenarian patients have a significantly higher incidence of overall complication, mortality, readmission and longer hospital stay than younger patients; (2) the available literature showed similar improvement in the clinical symptoms (ODI and pain) of patients in the two groups; (3) no significant differences in the overall wound complication, reoperation rate, operative time and intraoperative blood loss was found between the two groups.
Complications following surgery in general are a major concern among elderly patients [26, 30]. It is not surprising that octogenarians are associated with more complications than younger patients because, compared with younger patients, octogenarians were more likely to have fragile physical conditions [31]. This study confirmed that octogenarian patients have more significant concomitant diseases, as reflected by higher ASA scores (ASA ≥ 3). Our meta-analysis showed that the overall complication in octogenarians was 1.5 times higher than that in younger patients from 11 included studies. It is worth noting that only two studies showed a significant difference in concomitant diseases between the two groups [13, 22]. Their results showed that the overall complication rate was similar between the two groups. Therefore, the higher complication rate in octogenarian patients in our meta-analysis was mainly due to the other nine studies, in which octogenarian patients had more significant concomitant diseases than the younger patients, indicating that medical comorbidities and a poor functional status, rather than age alone, contribute to the increased complication in patients aged 80 years or older. Furthermore, we evaluated the complications of specific surgical procedures. Patients aged 80 years or older had a higher complication rate than those younger than 80 years old, regardless of decompression alone or decompression plus fusion. This study also confirmed that fusion is associated with greater complications than decompression alone in octogenarian patients (15.8% vs 9.3%).
As in the case of overall complication, the mortality in octogenarians was three times higher than that in younger patients on pooled analysis of the data from the 11 studies included in this review. When analysing the data of each included study, the preoperative comorbidities were significantly greater among octogenarian patients in 10 of 11 studies. Thus, a sufficient preoperative assessment and a subsequent reasonable choice for lumbar decompression surgery in elderly patients seem to be important to reduce or avoid complication and mortality [17]. Moreover, clinical frailty stratification is helpful to improve patient selection, planning surgical procedures and predicting the risk of complication or death in the elderly. Li et al. [27], in 2008, performed a retrospective cohort study observing complications and mortality after lumbar decompression surgery in the elderly and quantified the overall complication or mortality rate stratified by age and comorbidities. They found that the complication and mortality rates increased within each age group with increasing numbers of comorbidities. For example, the overall complication and mortality rates in patients aged 65 to 84 years with three comorbidities were greater than the complication and mortality rate in patients 85 years or older with no comorbidities. Similarly, complications in patients aged 45 to 64 years with three comorbidities were similar to those in patients aged 65 to 84 years with no comorbidities.
Previous studies have evaluated the effect of age on the functional outcome of surgery for lumbar stenosis [4, 7]. Galiano et al. [7] studied the preoperative and follow-up outcomes in 23 patients older than 80 years who underwent decompression surgery for lumbar stenosis. There was no comparison group. The data revealed that significant improvements in the ODI and VAS from baseline measurements. Pain scores and disability measured by the ODI, also being our main outcome parameters, were reported in four studies [11,12,13, 19]. The present review demonstrated similar clinical improvement in the pain scores and ODI between patients aged older than 80 years and those aged younger than 80 years. Our results indicated that surgery for lumbar stenosis or spondylolisthesis could provide comparable improvement in disability and adequate pain relief for patients aged older than 80 years. However, with such limited available studies (four studies), solid conclusions on the functional outcomes between the two groups cannot be drawn. Furthermore, there may be confounding baseline variables that differed between octogenarians and younger patients, such as comorbidities and the severity of stenosis. Octogenarians who were offered surgery may represent well-selected octogenarians and have a better baseline health than their peers.
Thus, there needs to be further evaluation of a surgical indication among octogenarians with lumbar stenosis or spondylolisthesis. It is clear that conservative treatment must be helpful, but patients who do not respond favourably need surgery. There is growing evidence that surgical decompression offers an advantage over nonsurgical treatment for older patients with persistent severe symptoms [32]. In a multicentre prospective study, Rihn et al. [12] revealed that operative treatment of lumbar degenerative disease offers a significant benefit over conservative treatment in the octogenarian population. There is no widely accepted consensus on the indication for the surgical treatment of degenerative lumbar pathologies. Two randomized controlled trials by Forsth et al. [33] and Ghogawala et al. [34] have been published comparing simple decompression to decompression plus fusion, but they drew contradictory conclusions. Forsth et al. [33] reported that there was no strong evidence to support the use of fusion in patients with lumbar stenosis, even in patients with degenerative spondylolisthesis. Fusion surgery does not result in better clinical results than decompression alone. However, Ghogawala et al. [34] found that patients with lumbar stenosis and stable degenerative spondylolisthesis who underwent fusion have better clinical results and lower rates of reoperation than those who underwent decompression alone. The indications and optimal therapy to this issue in the octogenarian population remain unanswered. Although operative treatment may be safely used in selected octogenarians, patient comorbidities, osteoporosis and the surgical method should be considered when deciding to perform spinal surgery in the elderly population. Drazin et al. [35] and Lagman et al. [18] found that decompression plus fusion results in a higher rate of complications than decompression surgery alone in octogenarians. Our study also confirmed previous findings. It is not surprising because the fusion procedure requires extensive dissection of spinal tissues and a longer operation time and often involves placement of implants. Additionally, several authors have reported that older patients with more comorbidities were associated with more complications [17, 27]. Based on the current literature, in the absence of evidence showing better pain or function improvement with fusion surgery for lumbar stenosis in patients aged 80 years and older, decompression alone appears to be safe and effective. For physically well octogenarians who also have lumbar spondylolisthesis or associated spinal instability, decompression plus fusion may lead to a satisfactory clinical outcome.
Strengths and limitations
This is the first meta-analysis with a large sample size to investigate the difference in the preoperative characteristics and post-operative outcomes between octogenarians and younger patients after surgery for lumbar stenosis or spondylolisthesis. There was minimal to moderate heterogeneity (I2 < 50%) in evaluating most of the outcome variables included in our study, thus suggesting that these outcomes are fairly consistent and approximate the true effect size. Perfect homogeneity (I2 = 0%) was observed for wound complication, reoperation, ODI improvement scores, pain improvement scores and intraoperative blood loss. Additionally, single-elimination sensitivity analysis was performed, and it did not alter the overall results of the analysis, suggesting the high stability of the meta-analysis.
This study has several limitations. First, because these studies were comparative observational studies, they are at risk of selection bias. Heterogeneity in the patient population, unbalanced cohort sizes and surgical procedures may have limited its power to detect differences between cohorts. Second, the increased frequency of preoperative concomitant diseases, commonly observed in octogenarian patients, potentially introduce a significant selection bias when comparing the post-operative outcomes with younger patients without similar health status. Third, this study mixed decompression alone and decompression plus fusion as surgical procedures to evaluate the clinical outcomes in patients 80 years or older. Limited by the current literature, we could not evaluate other clinical outcomes of the specific surgical procedure between two different age groups, except for the overall complication. Fourth, the follow-up period was not reported in eight studies, which may affect the reliability of the available literature.
Conclusion
In the present systematic review and meta-analysis, octogenarian patients with lumbar stenosis or spondylolisthesis have a significantly higher incidence of overall complication, mortality, readmission and longer hospital stay than younger patients after surgery. The available literature showed that clinical improvement in pain and disability after lumbar surgery in octogenarian patients were comparable to those in patients aged younger than 80 years. No significant differences in the overall wound complication, reoperation rate, operative time and intraoperative blood loss were detected. Based on the current evidence, we recommend that age alone is not a contraindication for lumbar surgery in very old patients. A careful preoperative evaluation, proper patient selection and appropriate surgical approach are important to achieve successful surgical outcomes.
References
Fehlings MG, Tetreault L, Nater A, Choma T, Harrop J, Mroz T, Santaguida C, Smith JS (2015) The aging of the global population: the changing epidemiology of disease and spinal disorders. Neurosurgery 77(Suppl 1):S1–S5
Phan K, Mobbs RJ (2016) Minimally invasive versus open laminectomy for lumbar stenosis: a systematic review and meta-analysis. Spine (Phila Pa 1976) 41(2):E91–E100
Dijkerman M, Overdevest G, Moojen W, Vleggeert-Lankamp C (2018) Decompression with or without concomitant fusion in lumbar stenosis due to degenerative spondylolisthesis: a systematic review. Eur Spine J 27(7):1629–1643
Shabat S, Arinzon Z, Folman Y, Leitner J, David R, Pevzner E, Gepstein R, Ilya P, Shuval I (2008) Long-term outcome of decompressive surgery for lumbar spinal stenosis in octogenarians. Eur Spine J 17(2):193–198
Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG (2010) Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 303(13):1259–1265
Nagashima H, Dokai T, Hashiguchi H, Ishii H, Kameyama Y, Katae Y, Morio Y, Morishita T, Murata M, Nanjo Y (2011) Clinical features and surgical outcomes of cervical spondylotic myelopathy in patients aged 80 years or older: a multi-center retrospective study. Eur Spine J 20(2):240
Galiano K, Obwegeser AA, Gabl MV, Bauer R, Twerdy K (2005) Long-term outcome of laminectomy for spinal stenosis in octogenarians. Spine (Phila Pa 1976) 30(3):332–335
Lieber BA, Chiang V, Prabhu AV, Agarwal N, Henry JK, Lin D, Kazemi N, Tabbosha M (2016) Postoperative complications for elderly patients after single-level lumbar fusions for spondylolisthesis. World Neurosurg 91:149–153
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Deyo RA, Hickam D, Duckart JP, Piedra M (2013) Complications following surgery for lumbar stenosis in a veteran population. Spine (Phila Pa 1976) 38(19):1695
Giannadakis C, Solheim O, Jakola AS, Nordseth T, Gulati AM, Nerland US, Nygaard ØP, Solberg TK, Gulati S (2016) Surgery for lumbar spinal stenosis in individuals aged 80 and older: a multicenter observational study. J Am Geriatr Soc 64(10):2011–2018
Rihn JA, Hilibrand AS, Zhao W, Lurie JD, Vaccaro AR, Albert TJ, Weinstein J (2015) Effectiveness of surgery for lumbar stenosis and degenerative spondylolisthesis in the octogenarian population: analysis of the Spine Patient Outcomes Research Trial (SPORT) data. J Bone Joint Surg Am 97(3):177
Ulrich NH, Kleinstück F, Woernle CM, Antoniadis A, Winklhofer S, Burgstaller JM, Farshad M, Oberle J, Porchet F, Min K (2015) Clinical outcome in lumbar decompression surgery for spinal canal stenosis in the aged population: a prospective Swiss multicenter cohort study. Spine (Phila Pa 1976) 40(6):415–422
Ciol MA, Deyo RA, Howell E, Kreif S (1996) An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc 44(3):285–290
Hayashi K, Matsumura A, Konishi S, Kato M, Namikawa T, Nakamura H (2016) Clinical outcomes of posterior lumbar interbody fusion for patients 80 years of age and older with lumbar degenerative disease: minimum 2 years’ follow-up. Glob Spine J 6(7):665–672
Jansson K-Å, Blomqvist P, Granath F, Nemeth G (2003) Spinal stenosis surgery in Sweden 1987–1999. Eur Spine J 12(5):535–541
Kalanithi PS, Patil CG, Boakye M (2009) National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976) 34(18):1963–1969
Lagman C, Ugiliweneza B, Boakye M, Drazin D (2017) Spine surgery outcomes in elderly patients versus general adult patients in the United States: a MarketScan analysis. World Neurosurg 103:780–788
Liao J-C, Chen W-J (2018) Surgical outcomes in the elderly with degenerative spondylolisthesis: comparative study between patients over 80 years of age and under 80 years—a gender-, diagnosis-, and surgical method-matched two-cohort analyses. Spine J 18(5):734–739
Machado GC, Maher CG, Ferreira PH, Harris IA, Deyo RA, McKay D, Li Q, Ferreira ML (2017) Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine (Phila Pa 1976) 42(22):1737–1743
Murphy ME, Gilder H, Maloney PR, McCutcheon BA, Rinaldo L, Shepherd D, Kerezoudis P, Ubl DS, Crowson CS, Krauss WE (2017) Lumbar decompression in the elderly: increased age as a risk factor for complications and nonhome discharge. J Neurosurg Spine 26(3):353–362
Nanjo Y, Nagashima H, Dokai T, Hamamoto Y, Hashiguchi H, Ishii H, Kameyama Y, Morio Y, Murata M, Tanida A (2013) Clinical features and surgical outcomes of lumbar spinal stenosis in patients aged 80 years or older: a multi-center retrospective study. Arch Orthop Trauma Surg 133(9):1243–1248
Puvanesarajah V, Jain A, Shimer AL, Li X, Singla A, Shen F, Hassanzadeh H (2017) Complications and mortality following 1 to 2 level lumbar fusion surgery in patients above 80 years of age. Spine (Phila Pa 1976) 42(6):437–441
Battié MC, Jones CA, Schopflocher DP, Hu RW (2012) Health-related quality of life and comorbidities associated with lumbar spinal stenosis. Spine J 12(3):189–195
Sciubba DM, Scheer JK, Yurter A, Smith JS, Lafage V, Klineberg E, Gupta M, Eastlack R, Mundis GM, Protopsaltis TS (2016) Patients with spinal deformity over the age of 75: a retrospective analysis of operative versus non-operative management. Eur Spine J 25(8):2433–2441
Rothenfluh DA, Koenig M, Stokes OM, Behrbalk E, Boszczyk BM (2014) Access-related complications in anterior lumbar surgery in patients over 60 years of age. Eur Spine J 23(Suppl 1):S86–S92
Li G, Patil CG, Lad SP, Ho C, Tian W, Boakye M (2008) Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine (Phila Pa 1976) 33(11):1250–1255
Sobottke R, Herren C, Siewe J, Mannion AF, Roder C, Aghayev E (2017) Predictors of improvement in quality of life and pain relief in lumbar spinal stenosis relative to patient age: a study based on the Spine Tango registry. Eur Spine J 26(2):462–472
Costa F, Ortolina A, Tomei M, Cardia A, Zekay E, Fornari M (2013) Instrumented fusion surgery in elderly patients (over 75 years old): clinical and radiological results in a series of 53 patients. Eur Spine J 22(Suppl 6):S910–S913
Antoniadis A, Ulrich NH, Schmid S, Farshad M, Min K (2017) Decompression surgery for lumbar spinal canal stenosis in octogenarians; a single center experience of 121 consecutive patients. Br J Neurosurg 31(1):67–71
Raffo CS, Lauerman WC (2006) Predicting morbidity and mortality of lumbar spine arthrodesis in patients in their ninth decade. Spine (Phila Pa 1976) 31(1):99–103
Shamji MF, Mroz T, Hsu W, Chutkan N (2015) Management of degenerative lumbar spinal stenosis in the elderly. Neurosurgery 77(suppl_1):S68–S74
Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, Öhagen P, Michaëlsson K, Sandén B (2016) A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Engl J Med 374(15):1413–1423
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374(15):1424–1434
Drazin D, Lagman C, Bhargava S, Nuño M, Kim TT, Johnson JP (2017) National trends following decompression, discectomy, and fusion in octogenarians and nonagenarians. Acta Neurochir 159(3):517–525
Funding
The study had no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liang, H., Lu, S., Jiang, D. et al. Clinical outcomes of lumbar spinal surgery in patients 80 years or older with lumbar stenosis or spondylolisthesis: a systematic review and meta-analysis. Eur Spine J 29, 2129–2142 (2020). https://doi.org/10.1007/s00586-019-06261-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-06261-1