Abstract
Purpose
To delineate the changes in functional outcomes of surgically treated U-shaped sacral fractures.
Methods
Forty-one patients with U-shaped sacral fractures were followed for a mean of 4.1 years after surgery. Impairment of lower extremities was assessed via a modified Gibbons score. Urinary function was assessed with a structured interview and residual urine volume. Sexual and bowel functions, as well as patient-reported health, were evaluated using a structured interview, and pain was evaluated with the visual analog scale. Comparisons of data at different time points were conducted with a mixed model, and Z-scores of the SF-36 questionnaire were calculated.
Results
Forty patients reported pain at 1 year and demonstrated no change at 2 years (p = 0.24). Thirty-six of 39 eligible patients had neurological deficits involving the lower extremities at baseline and demonstrated improvement at 1 year (p = 0.0002) but not between years 1 and 2 (p = 0.47). Twenty-three of 38 eligible patients had impaired bladder function, and 13 of 35 eligible patients had impaired bowel function at 3 months. Urinary function was worse at 2 years than at 1 year (p = 0.02). Sexual dysfunction was common, and patient-reported health was significantly worse than that of the normal population.
Conclusions
Neurological function in the lower extremities of patients with U-shaped sacral fractures improved after surgery; however, bowel and sexual functions did not change, and urinary function deteriorated over time. The majority of impairments appear to be permanent if still present at 1 year after surgery.
Graphical abstract
These slides can be retrieved under Electronic Supplementary Material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
U-shaped sacral fractures result from high-energy trauma with an axial load through the sacrum and are characterized by multiplanar instability of the lumbopelvis. Hallmarks include vertical and transverse fracture lines that form a U-, H-, T-, or Y-shaped pattern (comprising four variations in U-shaped sacral fractures) (Supplementary Figure 1) [1]. The relationship between the proximal and distal sacral fragments has been classified by Roy-Camille and revised by others (Fig. 1a–f) [2,3,4]. U-shaped sacral fractures frequently cause neurological deficits due to center canal occlusion (Fig. 2a) and intraforaminal osseous fragments (Fig. 2b) [5]. Because U-shaped sacral fractures are highly unstable, without surgical treatment, nonunion (Fig. 3a, b) and malunion (Fig. 3c, d) of the fractures may develop and result in progressive neurological dysfunction [5]. Furthermore, patients with U-shaped sacral fractures are often polytraumatized, and thus, an operative intervention that permits early mobilization may reduce mortality and improve the quality of life [6].
Images showing the modified Roy-Camille classification, with type I as a flexion fracture without translational displacement (a); type IIa as a flexion fracture with partial posterior displacement of the upper fragment (b); type IIb as a flexion fracture with complete posteroinferior displacement of the upper fragment (c); type IIIa as an extension fracture with partial anterior displacement of the upper fragment (d); type IIIa as an extension fracture with complete anteroinferior displacement of the upper fragment (e); and type IV as a complete comminution of the upper sacrum (f). The locations of transverse fracture are indicated by the white arrows
U-shaped sacral fractures are rare, and the patient population documented in the literature is small [5, 7,8,9]; consequently, little information is available on the detailed functional outcomes of these injuries after surgical treatment, such as neurological sequelae, voiding, bowel and sexual functions, residual pain, and patient-reported health [5, 7]. Therefore, the aim of this study was to delineate the changes in the functional outcomes of surgically treated U-shaped sacral fractures by analyzing the functional outcomes at different time points.
Materials and methods
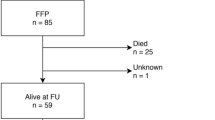
Between December 2005 and November 2015, 49 consecutive patients with U-shaped sacral fractures were admitted to our trauma center and diagnosed through pelvic radiographs (anteroposterior (AP), inlet, and outlet projections), CT scans, and, if available, an additional three-dimensional reconstruction. Five patients were excluded because of nonoperative treatment, two patients were excluded because of an insufficient duration of follow-up, and one patient was lost to follow-up. No patients were excluded because of low-energy insufficiency fractures or osteoporotic fractures. The remaining 41 patients were available for a mean follow-up of 4.1 years (range 2–10 years) (Table 1) (Supplementary Table 1). Written informed consent was obtained from all participants and was approved by the institutional review board of our institution.
Function assessment
All patients were independently examined by 2 physicians who were not involved in the initial treatment, and all patients underwent a structured interview to address neurological function as described below. The clinical assessment focused on only lumbar and sacral nerve root injuries. At follow-up, patient-reported health was measured by the 36-item Short-Form Health Survey (SF-36) [10], and pain was measured by the visual analog scale (VAS) [7]. Problems associated with sexual function were assessed with the Female Sexual Function Index (FSFI) in female patients and the International Index of Erectile Function-5 (IIEF-5) questionnaire in male patients based on the sexual activity during the previous 4 weeks [11, 12].
A modified Gibbons score was applied to specifically assess neurological deficits in the lower extremities as follows [13]: grade I, normal; grade II, sensory changes only; grade III, combined sensory and motor deficits; and grade IV, complete loss of neurological function.
Bladder dysfunction was assessed by a questionnaire concerning hesitation, urgency, frequency, and incontinence [13]. In addition, bladder dysfunction was graded according to the postmicturition volume as assessed by ultrasound within 10 min after bladder emptying as follows: grade I, normal (same as before injury); grade II, slightly changed voiding pattern with less than 50 mL of residual urine; grade III, significantly changed voiding pattern with more than 50 mL of residual urine or with incontinence; and grade IV, no volitional voiding.
Bowel function was graded according to the questionnaire as follows [13]: grade I, normal (same as before injury); grade II, change in frequency or need for laxatives; and grade III, incontinence and/or need for enemas or even colostomy.
Surgical management
Surgical management was based on fracture stability, neurological status, and medical condition (Table 2). Bilateral less invasive lumbopelvic fixation was conducted in patients with a displacement less than 1 cm and no neurological symptoms [14, 15], whereas patients with noticeably displaced fractures or radiological signs of neurological injuries on a CT scan and/or magnetic resonance imaging (MRI) underwent open reduction and decompression [16, 17]. Briefly, with the patient lying prone, a midline incision was made from L4 to S4. After exposure of the lumbar transverse processes, sacral ala, and posterior superior iliac spines (PSISs), pedicle screws were placed into the L4 and/or L5 pedicles and both iliac bones under fluoroscopic control. Direct decompression was achieved through laminectomy (expanded as necessary to decompress the dural sac) and foraminotomy (to decompress the sacral roots to their foraminal exit). Consequently, the nerve roots maintained a loose status during reduction. Reduction and fixation were performed according to the method described by Schildhauer et al. [18]. All patients received deep vein thrombosis prophylaxis in addition to perioperative antibiotics.
Statistical analysis
GraphPad Prism 5 (GraphPad Software, Inc., La Jolla, CA) and SAS (SAS institute Inc., North Carolina, USA) were used for statistical analyses. The mixed model, which incorporates a time variable, was used to compare follow-up data at different time points. Z-scores of all eight domains of the SF-36 questionnaire were calculated using age- and sex-adjusted norm-based scores for the general Chinese population in mainland China [19]. p < 0.05 was considered statistically significant.
Results
Baseline characteristics of the injury
All 41 patients were treated with internal fixation (Fig. 4a–d); of these patients, 37 (90%) were treated with direct decompression (Table 3) (Supplementary Table 1). Thirty-one of 41 (76%) patients suffered severe associated injuries. Four patients presented fractures to the skull combined with an epidural hematoma and/or subdural hematoma. Thoracic injuries consisted of rib fractures and/or sternal fractures (N = 5), pneumothorax (N = 1), hemopneumothorax (N = 2), and lung contusion (N = 2). Two patients suffered a spleen laceration, and one patient suffered a bladder laceration. Four patients showed fractures of the upper extremities, including humeral fractures (N = 2) and radial and/or ulnar fractures (N = 2). Seven patients had an acetabular fracture. Eleven patients showed fractures of the lower extremities, including femoral fractures (N = 4), tibial and/or fibular fractures (N = 4), and calcaneal fractures (N = 7, with 2 bilateral). Thirty-nine patients suffered pubic fractures, of which fifteen were bilateral. The remaining two patients had pubic symphysis diastasis.
A 29-year-old female with a U-shaped sacral fracture. Preoperative three-dimensional reconstruction CT scan of the AP view (a) and posteroanterior (PA) view (b). AP pelvic radiograph (c) showing that the multiplanar fracture has been fixed by lumbopelvic fixation. AP pelvic radiograph showing that the fracture was healed at 2 years after surgery (d)
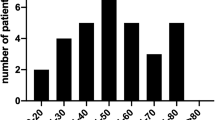
In some of the patients, a poor general condition precluded an early comprehensive assessment. However, during a secondary survey in the course of the hospital stay, all patients underwent complete neurological evaluation, and the results were regarded as baseline characteristics. Thirty-six of 39 (92%) eligible patients had neurological deficits in the lower extremities (Fig. 5) (Supplementary Table 2). In 28 patients, the neurological deficits in the lower extremities could be ascribed to an injury to the sacrum (Table 2). Bladder and bowel functions were assessed at 3 months, as those assessments were not feasible at the time of injury. Twenty-three of 38 (61%) eligible patients had impaired bladder function (Fig. 6), and 13 of 35 (37%) eligible patients had impaired bowel function (Fig. 7). All but 2 patients demonstrated fracture union on a CT scan at 6 months; however, subsequent CT scans at 9 months revealed that the fractures of those 2 patients had healed.
Results at the 1-year follow-up
Comparison of the baseline and 1-year follow-up data revealed that neurological function in the lower extremity remained unchanged in 25 (64%) patients and deteriorated in 1 (3%) patient. However, in 13 (33%) patients, neurological function in the lower extremity improved. The overall improvement was statistically significant (p = 0.0002) (Fig. 5). Twenty-seven of 39 (69%) patients were ambulant without walking aids. However, six patients were unable to run because of pain or decreased muscle strength.
Comparison of the 1-year follow-up data to the 3-month follow-up data showed that out of 38 eligible patients, 24 (63%) patients exhibited unchanged bladder function. Bladder function was fully recovered in five (13%) patients, and one (3%) patient who initially had grade IV function improved to grade III function. Eight (21%) patients suffered bladder function deterioration (Fig. 6). However, the changes were not statistically significant (p = 0.83).
Twenty-three (66%) patients had unchanged bowel function at the 1-year follow-up compared to the 3-month follow-up. One (3%) out of four patients with grade III function improved to grade II function, and six (17%) out of nine patients with grade II function were completely recovered at the 1-year follow-up. Six (17%) patients with initially normal bowel function deteriorated to grade II function (Fig. 7). However, the changes were not statistically significant (p = 0.78).
Thirty-five of 41 (85%) patients were sexually active, but only 22 patients (15 male, 7 female) completed the IIEF-5 or FSFI questionnaire. Two female patients reported sexual dysfunction associated with decreased lubrication and altered self-image (Fig. 8). Nine male patients reported a different degree of erectile dysfunction (IIEF-5 < 22) (Fig. 8) (Supplementary Table 3). All but one (40/41) patient reported pain on the VAS, with an average VAS score of 4.9 (range 1–8). The overall patient-reported health scores were significantly lower than those of the normal population (Fig. 9), except in the GH (general health) and MH (mental health) domains (Fig. 9) (Supplementary Table 4). However, eight patients were able to return to school or the workplace 1 year after the operation.
Z-scores of all eight domains of the SF-36 questionnaire for the 1-year and 2-year follow-ups (N = 36). The 0-line represents the age- and sex-adjusted norm-based scores for the general Chinese population in mainland China. The number by the outliers represents the corresponding patient. PF physical functioning, RP role physical, BP bodily pain, GH general health, VT vitality, SF social functioning, RE role emotional, MH mental health
Results at the 2-year follow-up
All patients, except one, reported pain at 1 year and demonstrated no statistically significant change at 2 years (p = 0.24). Neurological function in the lower extremity was improved at 2 years compared to baseline (p < 0.0001); however, the changes between the 1- and 2-year time points were not statistically significant (p = 0.47) (Fig. 5). Urinary function had deteriorated at 2 years compared to that at 1 year (p = 0.02) or that at 3 months (p = 0.04) (Fig. 6). The alterations in bowel function (Fig. 7), sexual function (Fig. 8), pain, and patient-reported health (Fig. 9) were not statistically significant.
Discussion
Because of the relative heterogeneity and rarity of U-shaped sacral fractures, little evidence is available for the development of a standardized treatment. In recent years, operative treatment has been reported to facilitate early mobilization and potentially improve the quality of life [1]. For this reason, we included only surgically treated patients in this study. The applied fixation methods have similar biomechanical properties and are capable of providing multiplanar stability, which allows early full weight bearing postoperatively. In addition, all surgeries were performed by the senior author, and nearly all patients were treated with direct decompression. Therefore, the management methods we adopted were relatively homogeneous.
Clinical examination alone is insufficient to determine the status of urinary bladder function [20]; thus, we evaluated the residual urine volume, as it can be objectively and practically measured with ultrasound. The urodynamic test was not adopted because it was not initially available at our trauma center. We also applied a modified Gibbons score to evaluate neurological function in the lower extremities [13]. Although the Gibbons score fails to effectively distinguish partial from complete neurological recovery, better substitutions are currently not available.
The majority of patients had neurological deficits in the lower extremities at baseline but achieved a statistically significant improvement at 1 year, which may indicate a positive effect of fracture stabilization and decompression. The improvements between the 1- and 2-year follow-ups were not statistically significant, indicating the poor rewiring ability of the impaired nervous system [21]. Notably, in accordance with a previous study [13], urinary function deteriorated in 9 patients between the 1- and 2-year follow-ups. Because 5 of the patients had incomplete bladder emptying at 1 year, the secondary deterioration may have been due to bladder distention. However, the cause of deterioration in 4 patients with previously normal bladder function may have been the frequently delayed urination caused by decreased mobility, as 3 of those patients had impaired neurological function in the lower extremities, and 1 patient was disabled. We observed that a considerable portion of patients showed bowel dysfunction. The causes of bowel dysfunction are assumed to be multifactorial, and future studies are needed to elucidate the connection between bowel dysfunction and sacral fractures [22].
The interpretation of neurological prognosis remains controversial, as some studies have shown partial or even complete neurological recovery without decompression [23]. The variation in neurological recovery may reflect the different types of nerve lesions acquired at the time of injury [24]. However, confirmation of the type of nerve lesion at the time of injury was not feasible. In our experience, because neurological injuries are largely irreversible and the time window of neurological treatment is small, internal fixation and decompression are beneficial to patients at high risk of neurological impairment if the general condition of the patient permits those procedures.
Chronic pain following injury was common in the present study, indicating that pain management is important. Because all fractures of the sacrum were radiologically united, other factors clearly contributed to the pain. Although posttraumatic kyphotic spine deformity may have been a contributor to lumbosacral pain, a previous study showed that kyphotic angulation is not correlated with VAS pain [7]; thus, further studies are required to determine the mechanism of residual lumbosacral pain. Lumbosacral pain during intercourse may contribute to sexual dysfunction, as the 11 (11/22) patients who reported sexual dysfunction had a high mean VAS score of 5.8 points. Further analysis of the psychosocial aspects of sexual dysfunction was beyond the scope of this study.
Sabiston subdivided the sacral transverse fractures into upper (S1/S2–S2/S3) and lower (S3/S4–S4/S5) segment fractures at the level of the sacroiliac joint and reported that only 1 in 11 patients who sustained lower segment fractures developed a neurological deficit; meanwhile, 5 of 5 patients with upper segment fractures developed neurological deficits [25]. In this study, 33 of 35 patients who sustained upper segment fractures developed a neurological deficit. Interestingly, 5 of 6 patients who sustained lower segment fractures also developed a neurological deficit, and notably, 3 of these 6 patients had a concomitant lumbar fracture.
Limitations
Due to the retrospective design, the subclass of neurological statuses for all patients could not be determined at all time points. Therefore, the patients eligible for subclass comparison were usually fewer than 41. In addition, no neurophysiological tests were used to objectively document the nerve injury, as these tests were not feasible in the trauma setting. Another limitation is that the contribution of the sacral fracture to the functional outcome may be difficult to interpret because of the associated injuries, particularly thoracolumbar spine fractures.
Conclusions
Although all the sacral fractures were united at follow-up, impairments of lower extremity, urinary bladder, bowel, and sexual function remained common at 1 year or even 2 years after injury. The overall neurological function in the lower extremities significantly improved, as most of the patients were able to ambulate without walking aids. However, the majority of impairments appeared to be permanent if still present at 1 year after surgery, and urinary function can even deteriorate over time. Furthermore, data on the overall patient-reported health indicated that U-shaped sacral fractures can cause both physiological and psychological damages. Although the overall outcome remains poor, we recommend surgical management when indicated, as it can restore spinopelvic stability, allowing early full weight bearing and potentially improving the quality of life. However, future studies comparing operative versus nonoperative treatment are required to further validate these results.
References
Kaye ID, Yoon RS, Stickney W, Snavely J, Vaccaro AR, Liporace FA (2018) Treatment of spinopelvic dissociation: a critical analysis review. JBJS Rev 6(1):e7. https://doi.org/10.2106/jbjs.rvw.16.00119
Strange-Vognsen HH, Lebech A (1991) An unusual type of fracture in the upper sacrum. J Orthop Trauma 5(2):200–203
Roy-Camille R, Saillant G, Gagna G, Mazel C (1985) Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine (Phila Pa 1976) 10(9):838–845
Lindahl J, Makinen TJ, Koskinen SK, Soderlund T (2014) Factors associated with outcome of spinopelvic dissociation treated with lumbopelvic fixation. Injury 45(12):1914–1920. https://doi.org/10.1016/j.injury.2014.09.003
Gribnau AJ, van Hensbroek PB, Haverlag R, Ponsen KJ, Been HD, Goslings JC (2009) U-shaped sacral fractures: surgical treatment and quality of life. Injury 40(10):1040–1048. https://doi.org/10.1016/j.injury.2008.11.027
Yi C, Hak DJ (2012) Traumatic spinopelvic dissociation or U-shaped sacral fracture: a review of the literature. Injury 43(4):402–408. https://doi.org/10.1016/j.injury.2010.12.011
Adelved A, Totterman A, Glott T, Hellund JC, Madsen JE, Roise O (2016) Long-term functional outcome after traumatic lumbosacral dissociation. A retrospective case series of 13 patients. Injury 47(7):1562–1568. https://doi.org/10.1016/j.injury.2016.04.006
Markel DC, Raskas DS, Graziano GP (1993) A case of traumatic spino-pelvic dissociation. J Orthop Trauma 7(6):562–566
Vresilovic EJ, Mehta S, Placide R, Milam RAT (2005) Traumatic spondylopelvic dissociation. A report of two cases. J Bone Joint Surg Am 87(5):1098–1103. https://doi.org/10.2106/jbjs.d.01925
Lam CL, Tse EY, Gandek B, Fong DY (2005) The SF-36 summary scales were valid, reliable, and equivalent in a Chinese population. J Clin Epidemiol 58(8):815–822. https://doi.org/10.1016/j.jclinepi.2004.12.008
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Pena BM (1999) Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 11(6):319–326
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’Agostino R Jr. (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26(2):191–208. https://doi.org/10.1080/009262300278597
Adelved A, Totterman A, Glott T, Madsen JE, Roise O (2012) Functional outcome 10 years after surgical treatment of displaced sacral fractures. Spine (Phila Pa 1976) 37(16):E1009–E1016. https://doi.org/10.1097/brs.0b013e31823a0d83
Keel MJ, Benneker LM, Siebenrock KA, Bastian JD (2011) Less invasive lumbopelvic stabilization of posterior pelvic ring instability: technique and preliminary results. J Trauma 71(3):E62–E70. https://doi.org/10.1097/TA.0b013e3182092e66
Taguchi T, Kawai S, Kaneko K, Yugue D (1999) Operative management of displaced fractures of the sacrum. J Orthop Sci 4(5):347–352
Kulkarni MV, McArdle CB, Kopanicky D, Miner M, Cotler HB, Lee KF, Harris JH (1987) Acute spinal cord injury: MR imaging at 1.5 T. Radiology 164(3):837–843. https://doi.org/10.1148/radiology.164.3.3615885
Wintermark M, Mouhsine E, Theumann N, Mordasini P, van Melle G, Leyvraz PF, Schnyder P (2003) Thoracolumbar spine fractures in patients who have sustained severe trauma: depiction with multi-detector row CT. Radiology 227(3):681–689. https://doi.org/10.1148/radiol.2273020592
Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML Jr., Chapman JR (2006) Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma 20(7):447–457
Rui W, Cheng W, Ma XQ, Zhao YF, Yan XY, Jia H (2011) Health-related quality of life in Chinese people: a population-based survey of five cities in China. Scand J Public Health 39(4):410–418. https://doi.org/10.1177/1403494810395817
Wyndaele JJ (1997) Correlation between clinical neurological data and urodynamic function in spinal cord injured patients. Spinal Cord 35(4):213–216
Ramer LM, Ramer MS, Bradbury EJ (2014) Restoring function after spinal cord injury: towards clinical translation of experimental strategies. Lancet Neurol 13(12):1241–1256. https://doi.org/10.1016/s1474-4422(14)70144-9
Siebler JC, Hasley BP, Mormino MA (2010) Functional outcomes of Denis zone III sacral fractures treated nonoperatively. J Orthop Trauma 24(5):297–302. https://doi.org/10.1097/BOT.0b013e3181ccb645
Nork SE, Jones CB, Harding SP, Mirza SK, Routt ML Jr. (2001) Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 15(4):238–246
Huittinen VM (1972) Lumbosacral nerve injury in fracture of the pelvis. A postmortem radiographic and patho-anatomical study. Acta Chir Scand Suppl 429:3–43
Sabiston CP, Wing PC (1986) Sacral fractures: classification and neurologic implications. J Trauma 26(12):1113–1115
Acknowledgements
The authors are grateful to Yin Li for assisting in statistical analysis and outcome interpretation. Yin Li is from State Key Laboratory of Environmental Health, School of Public Health, Tongji Medical College, Huazhong University of Science and Technology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest in the submission of this manuscript.
Informed consent
Written informed consent was obtained from all participants and was approved by the Institutional Review Board of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Images showing the variations in U-shaped sacral fractures, including the U-shaped (a), H-shaped (b), T-shaped (c), and Y-shaped (d) pattern (TIFF 9089 kb)
Rights and permissions
About this article
Cite this article
He, L., Yi, C., Hak, D.J. et al. Functional outcome of surgically treated U-shaped sacral fractures: experience from 41 cases. Eur Spine J 28, 1146–1155 (2019). https://doi.org/10.1007/s00586-019-05900-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-019-05900-x