Abstract
Purpose
Pyogenic spondylodiscitis (PS) is a potentially life-threatening infection burdened by high morbidity rates. Despite the rising incidence, the proper management of PS is still controversial. Aim of this study was to describe the clinical features of PS and to evaluate the prognostic factors and the long-term outcomes of a large population of patients.
Methods
207 cases of PS treated from 2008 to 2016 with a 2-year follow-up were enrolled. Clinical data from each patient were recorded. The primary outcome was the rate of healing without residual disability. Secondary outcomes included length of stay, healing from infection, death, relapse, and residual disability. Binomial logistic regression and multivariate analysis were used to evaluate prognostic factors.
Results
Median diagnostic delay was 30 days and the rate of onset neurological impairment was 23.6%. Microbiological diagnosis was established in 155 patients (74.3%) and the median duration of total antibiotic therapy was 148 days. Orthopedic treatment was conservative for 124 patients and surgical in 47 cases. Complete healing without disability was achieved in 142 patients (77.6%). Statistically confirmed negative prognostic factors were: negative microbiological culture, neurologic impairment at diagnosis and underlying endocarditis (p ≤ 0.05). Healing from infection rate was 90.9%, while residual disabilities occurred in 23.5%. Observed mortality rate was 7.8%.
Conclusion
The microbiological diagnosis is the main predictive factor for successful treatment. Early diagnosis and multidisciplinary management are also needed to identify underlying aggressive conditions and to avoid neurological complications associated with poorer long-term outcomes. Despite high healing rates, PS may lead to major disabilities still representing a difficult challenge.
Graphical abstract
These slides can be retrieved under Electronic Supplementary material.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pyogenic spondylodiscitis (PS) is a non-specific and acute or subacute infection involving intervertebral disks and adjacent vertebral bodies.
PS predominantly occurs in elderly and chronically debilitated patients aged over 50 years with peak prevalence between 50 and 70 years [1,2,3]. PS is more common among male patients with a male to female ratio of 1.6–2.0:1 which further increases in elderly populations [1, 2, 4]. Previous studies estimated the annual incidence of PS ranging from 0.5 to 2.4 cases per 100,000 inhabitants in Europe [1, 5, 6]. However, more recent studies reported an alarming increase of incidence in the last 20 years. A Danish nation-wide study, conducted over the last 14 years, showed that annual incidence of PS increased from 2.2 to 5.8/100,000 inhabitants [7]. Akiyama et al. reported an increase of incidence of approximately 140% in Japan [8]. Similar findings were confirmed by Lora-Tomayo et al. on a Spanish population [9]. This epidemiological trend is likely due to the higher diagnostic efficacy obtained with the spread of MRI and to an increased number of persons at risk. Aging population and longer life expectancy for chronically debilitated and immunosuppressed patients led to an increased number of high-risk individuals, while the spread of invasive and minimally invasive diagnostic or surgical procedures exposed more patients to iatrogenic infections.
Pathogenesis
PS is in most cases a hematogenous infection where arterial or, less frequently, venous septic emboli from distant infectious foci may occlude the terminal arterioles of vertebral end-plates causing ischemia and infected osteonecrosis. The development of PS by direct inoculation may follow spinal surgery, epidural procedures and lumbar puncture with a reported prevalence up to 18.8% [10]. Through the osteonecrosis, the infection can lead to biomechanical instability and epidural abscesses causing neurological impairment in about 1/3 of all cases [4, 11].
Clinical challenges
PS is still burdened by high morbidity rates even though mortality significantly dropped from the first case series published by Kulowski in 1936 [12]. Early diagnosis is still a challenge because of the non-specific clinical onset of PS which is frequently confused with more prevalent degenerative diseases. Indeed, average diagnostic delay from symptoms onset still ranges from 30 to 90 days [2, 3]. Guidelines for the pharmacological therapy have been published by the Infectious Diseases Society of America (IDSA) in 2015 [13]. On the other hand, there are only few proposals of standard algorithms for orthopedic treatment [14].
Understanding the clinical features of PS is necessary to achieve an early diagnosis. However, there are only few studies conducted on large populations and the available clinical data are controversial. Few authors have evaluated the long-term outcomes and few data are available on prognostic factors and residual disabilities. Aim of this study was to describe the clinical features of PS in a large population of patients and to evaluate the prognostic factors and the long-term outcomes of treatment strategies.
Materials and methods
An observational, monocentric, cohort study was performed. All consecutive cases of PS treated in a 1100-bed university hospital over a 9-year period (2008–2016) with a 2-year follow-up were enrolled. With a multidisciplinary approach, both spine surgeons and infectious diseases specialists were involved in the care and follow-up of all patients. Records from each patient were collected using an electronic database. Diagnostic approach included clinical history and physical examination, serum C-reactive protein (CRP) levels, white blood cells count (WBC), and full spine contrast-enhanced MRI (or CT when contraindicated). Suspected or confirmed non-pyogenic spondylodiscitis (e.g. tubercular and brucellar infections) were excluded. Serial blood cultures were collected from all patients, even if afebrile, at the admission and just after every invasive procedure. CT-guided biopsy was performed when blood cultures were negative while surgical biopsy was used as third line technique. Patients were matched according to a clinical-radiological classification: PS without biomechanical instability nor neurological impairment or epidural abscess (type A), PS with significant bone destruction and/or biomechanical instability without acute neurological impairment or epidural abscess (type B), and PS with epidural abscess and/or acute neurological impairment (type C) [14].
All patients received initial intravenous antibiotic therapy, followed by oral course until clinical improvement and normalization of laboratory and radiological markers of infection. Patients without microbiological diagnosis received empiric broad-spectrum antibiotic therapy and underwent closer monitoring. Conservative orthopedic treatment consisted of immobilization with rigid orthosis (i.e. hard cervical collar or thoraco-lumbar rigid brace molded on plaster cast) until complete infection healing. Open surgical treatment was performed when decompression of neurological structures, spine instrumentation, or debridement of necrotic tissues were required. Minimally invasive percutaneous screw-rod instrumentation was used as an alternative to orthosis in patients with single-level thoraco-lumbar PS and high functional demands. Surgical fixation was always performed avoiding instrumentation of infected vertebrae.
Follow-up visits were performed at 1, 3, 6, 12 and 24 months from diagnosis and consisted of physical examination, serial CRP and WBC. When appropriate, also MRI was performed. Patients were also asked to fill in Visual Analogic Scale (VAS) questionnaire at each visit.
Outcome measures
The primary outcome of the study was the rate of healing without residual disability at 24 months from diagnosis, defined as resolution of onset symptoms together with the normalization of WBC and CRP values and absence of radiological signs of active infection. Secondary outcomes included length of stay, healing from infection, death, relapse, and residual disability. Residual disability was defined as persistence of neurological impairment or chronic spinal pain. Healing from infection was defined as resolution of laboratory and radiological signs of infection with or without residual disability at 24 months from diagnosis.
Statistical analysis
IBM SPSS Statistics, version 22 (IBM, Armonk, NY, USA) was used for statistical analysis. Data are expressed as median and interquartile range for continuous variables and as number with percentage for categorical variables. Binomial logistic regression and multivariable analysis were used to evaluate prognostic factors and p values of 0.05 or less were considered significant.
Results
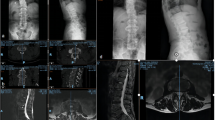
A total of 207 patients (134 men and 73 women) treated in our university hospital were enrolled. The median age was 67 years (IQR 56.00–74.00). The median time from symptom onset to diagnosis was 30 days (IQR 15.00–63.00) (Table 1). Most common symptoms at onset were spinal pain (193 patients, 93%) and fever (126 patients, 64.6%). Radiating pain (84 patients, 43.8%) and weight loss (54 patients, 30.7%) were referred less frequently. Neurologic impairment at diagnosis occurred in 47 patients (23.5%) (Fig. 1). Leukocytosis, defined as WBC > 10,000/mm3, occurred in 73 patients (35.8%) while high CRP, defined as CRP > 5 mg/l, occurred in 161 patients (92.5%), with a median CRP level at onset of 45 mg/l (IQR 13.77–98.47) (Fig. 1). Lumbar spine was the most commonly affected tract (143 patients, 70.1%) with peaks at L3–L5 levels. Multiple levels involvement was observed in 53 patients (26.1%).
The most common underlying medical conditions were cardiovascular diseases (70 patients, 37.6%), diabetes mellitus (58 patients, 32.0%), malignancies (45 patients, 24.2%), and chronic renal failure (27 patients, 14.9%) (Table 1). Twenty-six patients (14.6%) were on steroid therapy, while 10 patients (5.7%) were intravenous drug abusers. A diagnosis of post-surgery PS was established in 48 patients (23.4%) (Table 1).
Microbiological diagnosis was established in 155 patients (74.3%). Observed sensitivities of blood culture, CT-guided biopsy and surgical biopsy were, respectively, 55.5, 44.1 and 59.6%. Staphylococcus aureus was the most commonly isolated microorganism (58 patients, 28.7%) and in 10/58 patients (17.2%) the isolate was methicillin-resistant (MRSA). Other microorganisms were: coagulase-negative staphylococci (35 patients, 17.3%), streptococci (27 patients, 13.4%), Gram-negative bacilli (26 patients, 12.9%), enterococci (9 patients, 4.5%), Candida albicans (2 patients, 1.0%) (Table 2). Polymicrobial infections were observed in 10 patients (5.0%). Endocarditis was diagnosed in 22 patients (11.7%).
Observed sensitivities of full spine contrast-enhanced MRI and CT were 98.2 and 77.2%, respectively. Instability or deformity were observed in 31 patients (19%), vertebral fracture in 57 patients (33.1%), paravertebral abscess in 120 patients (67.8), epidural abscess in 90 patients (50.8%) and intramuscular abscess in 44 patients (25.1%). Sixty-eight cases (32.9%) were classified as type A PS, 43 cases (20.8%) were classified as type B PS, and 96 cases (46.4%) as type C PS (Table 3).
As for the orthopedic treatment, 124 patients (60.5%) were treated conservatively, with a high compliance to orthosis in 66.7%. Surgical treatment was required in 47 cases (27.4%): minimally invasive posterior percutaneous stabilization was performed in 6 patients (3.5%), open decompression alone in 27 patients (15.7%), and combined open decompression and stabilization in 13 patients (7.6%). Posterior approach alone was used in 80.5% of surgical cases and a combined anterior–posterior approach was performed in the remaining cases (Table 3). 4 patients underwent procedure-related complications, however, none of them reported permanent damages.
The median duration of total antibiotic therapy was 148 days (IQR 100–201), with a median length of intravenous antibiotic therapy of 35 days (IQR 24–46) and a median length of oral antibiotic therapy of 127 days (IQR 84–174) (Table 4). Glycopeptide + beta-lactam was the most commonly intravenous regimen (24.2%), followed by glycopeptide + fluoroquinolone (17.8%), glycopeptide monotherapy (17.8%) and beta-lactam monotherapy (17.8%). Fluoroquinolones were the most used oral antibiotics (62.7%) and the most commonly oral regimens were quinolone monotherapy (24.6%), quinolone + rifampin (11.9%), beta-lactam monotherapy (10.3%), quinolone + tetracycline (10.3%) (Table 4). An oral combination therapy of two or more antibiotics was used in 55.6% of cases. Median CRP levels significantly decreased across time points with median levels at 6 months below the threshold (Fig. 2).
Complete healing without disability at 24 months from diagnosis was achieved in 142 patients (77.6%) (Table 5). Negative prognostic factors related to complete healing were: neurological impairment at onset (OR 0.40; 95% CI 0.18–0.90; p = 0.02), epidural abscess at diagnosis (OR 0.43; 95% CI 0.20–0.92; p = 0.03), underlying endocarditis (OR 0.34; 95% CI 0.12–1.00; p = 0.05), negative microbiological culture (OR 0.41; 95% CI 0.19–0.87; p = 0.02) and type C PS (OR 0.72; 95% CI 0.57–0.92; p = 0.01). Multivariate analysis confirmed statistical significance for negative microbiological culture (AOR 0.26; 95% CI 0.10–0.65; p = 0.004), neurologic impairment at diagnosis (AOR 0.40; 95% CI 0.13–1.17; p = 0.009) and underlying endocarditis (AOR 0.25; CI 95% 0.06–0.98; p = 0.04) (Table 6).
Healing from infection at 24 months from diagnosis with or without residual disability occurred in 169 patients (90.9%). Eleven relapses of PS (5.7%) were observed during follow-up. Residual disability persisted in 44 patients (23.5%): chronic back pain in 32 patients (17.1%), paraparesis in 7 patients (3.7%) and paraplegia in 5 patients (2.7%). The median length of stay was 45 days (IQR 26–63). Death occurred in 15 cases with a mortality rate of 7.8% (Table 5).
Self-reported VAS scores significantly decreased across time points with slower recovery for type C cases (Fig. 3).
Self-reported Visual Analog Scale (VAS) scores are shown at diagnosis and at 1, 3, 6, 12, and 24 months post-diagnosis. VAS scores significantly decreased across time points in overall population and in all groups of our classification, showing the efficacy of different treatments in controlling pain. Patients affected by more aggressive PS (type C) showed a slower recovery
Discussion
PS is an uncommon but potentially life-threatening disease and severe disabling complications can occur. Therefore, our analysis of one of the largest populations of PS in literature can be useful to suggest the correct approach and management of this condition.
As part of a non-specific clinical onset, spinal pain is the most common presenting symptom. Clinically suspecting an infectious etiology is difficult in this condition. In fact, fever and leukocytosis occur only in a half and a third of cases, respectively. Neurological impairment at diagnosis, such as sensory or motor deficits and medullary signs, always require further investigation with MRI that help in earlier diagnosis [2]. CRP seems to be the most sensitive laboratory test. Although its low specificity, Jean et al. found that a CRP value over 63 mg/l was significantly associated with shorter diagnostic delay [15]. Therefore, the association of spinal pain and high value-CRP could increase the suspicion of PS and lead to an early diagnosis.
Contrast-enhanced MRI is the most sensitive technique for the diagnosis of PS, especially in the acute phase [16, 17]. However, since radiographic evidence of ongoing inflammation may persist for months to years in patients without clinical implications, caution should be used in interpreting follow-up MRI for the assessment of therapeutic response, to avoid unnecessary extended treatment [13]. Plain and dynamic X-rays and CT scans may be helpful in the evaluation of osteonecrosis extension and segmental stability. According to radiological criteria such as bone destruction, biomechanical instability, epidural abscess and clinical evaluation of acute neurological impairment, we previously provided a useful classification with a standard surgical treatment algorithm [14]. Although we do not routinely use fluorodeoxyglucose-positron emission tomography (FDG-PET/CT), this technique can be useful in the differential diagnosis between infective and severe degenerative processes [18].
Microbiological culture is a cornerstone for the diagnosis and treatment of PS. We observed that negative microbiological culture is the most significant negative prognostic factor. Hopkinson et al. showed that if no causative organism was found, the outcome was poorer and longer courses of antibiotics were required [5]. Blood culture had a good sensitivity, even higher than that of CT-leaded biopsy. To enhance the diagnostic power, we suggest to perform blood culture even if the patient is afebrile and after every invasive procedure.
The optimal total duration of antibiotic treatment is a controversial topic. There is only a single published randomized trial that showed that 6 weeks of antibiotic treatment is non-inferior to 12 weeks in patients with PS [19]. However, this study excluded patients with negative microbiological cultures thus probably affecting the results. The optimal duration of antibiotic treatment was evaluated by Park et al. on patients with haematogenous PS at low and high risk of recurrence [20]. Authors concluded that prolonged antibiotic therapy (≥ 8 weeks) should be prescribed for patients with risk factors of recurrence (i.e. MRSA infection, end-stage renal disease, and undrained abscesses) [20]. However, Roblot et al. performed a retrospective study to compare the risk of relapse according to the duration of antibiotic therapy (≤ 6 weeks versus > 6 weeks) without finding significant differences [21]. In a similar study by Grados et al. instead, the risk of relapse was higher when antibiotic treatment was shorter than 12 weeks [22].
As for the orthopaedic treatment, there are no guidelines for the conservative and surgical treatments of PS. The clinical-radiological classification we used can be very useful to guide the spine surgeons facing this pathology in a multidisciplinary management. When there are no neurological deficits and no significant instability, PS can be managed without surgical intervention. Lumbar epidural abscess may be approached with a conservative treatment only if there is no evidence for cauda equina or conus dysfunction [11, 23]. Immobilization is necessary to preserve spinal stability until ankylosis occurs. However, spontaneous ankylosis requires 6–24 months and may not take place at all [23]. In our population, percutaneous posterior screw-rod instrumentation bridging the infected level has been used in a limited number of cases as minimally invasive alternative to prolonged bracing for single-level thoraco-lumbar PS, especially for high functional-demanding patients. In a previous study, we reported faster recovery and improved quality of life associated with this minimally invasive treatment [24]. Residual chronic back pain, observed in 17.1% of our patients, is mostly due to non-surgically treated patients with post-infection kyphosis or pseudoarthrosis. When acute neurological impairment or severe kyphosis occur (defined as type C PS in our classification), open surgical approach is mandatory. Decompression and spinal stabilization should be performed as soon as possible and in the same procedure if neurological impairment exists. On the contrary, if instability and pain are present in a patient without neurological impairment, the correction of deformity through surgical instrumentation may be delayed until infection has been cleared. Debridement and arthrodesis without instrumentation may be sufficient in cases without instability, combined with bed rest and bracing [13, 23]. Anterior surgical approach is most often used when aggressive debridement and anterior column reconstruction are required. The remaining cases have been successfully treated with a posterior approach alone. Among 47 patients with acute neurological impairment at diagnosis, reverse of neurological deficits was achieved in 35 cases (74.5%).
The choice of appropriate surgical approaches and instrumentation is still a matter of controversy, including the possibility to instrument the infected vertebrae. The low relapses rate we observed seems to confirm our choice to avoid infected levels in surgical stabilization. Moreover, new minimally invasive techniques and new instrumentations have been recently proposed even if few clinical results are available [25].
In this setting of uncertainty, it seems to be essential to identify all forms of PS that can be more difficult to treat and that may deserve longer antibiotic course or more aggressive surgical treatments. Our analysis of possible prognostic factors can be helpful in this way. We found that neurological impairment and/or epidural abscess at onset (defined as type C PS in our classification), underlying endocarditis, and especially negative microbiological culture were negative prognostic factors for a complete healing without disability at 24 months from diagnosis. Therefore, the high rate of PS without microbiological etiology in our study population (25%) could partially justify the long duration of total antibiotic treatment that we reported. However, the rates of relapse and mortality we reported (5.7 and 7.8%) are among the lowest in the literature [3,4,5].
Our study had several limitations. First, as with all retrospective studies, some patients were lost to follow-up. Another potential limitation was the monocenter design of the study which did not allow to standardize our diagnostic and therapeutic algorithms to other clinical centers with different patient populations. Further studies, especially clinical trials, are needed to focus on topics such as the role of FDG-PET/CT in the diagnosis of PS, the real value of MRI in the follow-up, the role of oral combination therapy during the maintenance phase and the optimal duration of total antibiotic treatment in culture-negative PS. More clinical data are also needed to define the correct timing of surgical treatment and the indications for new techniques.
References
Grammatico L, Baron S, Rusch E, Lepage B, Surer N, Desenclos JC, Besnier JM (2008) Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2003. Epidemiol Infect 136:653–660. https://doi.org/10.1017/s0950268807008850
Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis A (2009) Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. Semin Arthritis Rheum 39:10–17. https://doi.org/10.1016/j.semarthrit.2008.03.002
Fantoni M, Trecarichi EM, Rossi B, Mazzotta V, Di Giacomo G, Nasto LA, Di Meco E, Pola E (2012) Epidemiological and clinical features of pyogenic spondylodiscitis. Eur Rev Med Pharmacol Sci 16(Suppl 2):2–7
Skaf GS, Domloj NT, Fehlings MG, Bouclaous CH, Sabbagh AS, Kanafani ZA, Kanj SS (2010) Pyogenic spondylodiscitis: an overview. J Infect Public Health 3:5–16. https://doi.org/10.1016/j.jiph.2010.01.001
Hopkinson N, Patel K (2016) Clinical features of septic discitis in the UK: a retrospective case ascertainment study and review of management recommendations. Rheumatol Int 36:1319–1326. https://doi.org/10.1007/s00296-016-3532-1
Krogsgaard MR, Wagn P, Bengtsson J (1998) Epidemiology of acute vertebral osteomyelitis in Denmark: 137 cases in Denmark 1978–1982, compared to cases reported to the National Patient Register 1991–1993. Acta Orthop Scand 69:513–517. https://doi.org/10.3109/17453679808997789
Kehrer M, Pedersen C, Jensen TG, Lassen AT (2014) Increasing incidence of pyogenic spondylodiscitis: a 14-year population-based study. J Infect 68:313–320. https://doi.org/10.1016/j.jinf.2013.11.011
Akiyama T, Chikuda H, Yasunaga H, Horiguchi H, Fushimi K, Saita K (2013) Incidence and risk factors for mortality of vertebral osteomyelitis: a retrospective analysis using the Japanese diagnosis procedure combination database. BMJ Open 3:e002412. https://doi.org/10.1136/bmjopen-2012-002412
Lora-Tamayo J, Euba G, Narváez JA, Murillo O, Verdaguer R, Sobrino B, Narváez J, Nolla JM, Ariza J (2011) Changing trends in the epidemiology of pyogenic vertebral osteomyelitis: the impact of cases with no microbiologic diagnosis. Semin Arthritis Rheum 41:247–255. https://doi.org/10.1016/j.semarthrit.2011.04.002
Nasto LA, Colangelo D, Rossi B, Fantoni M, Pola E (2012) Post-operative spondylodiscitis. Eur Rev Med Pharmacol Sci 16(Suppl 2):50–57
Duarte RM, Vaccaro AR (2013) Spinal infection: state of the art and management algorithm. Eur Spine J 22:2787–2799. https://doi.org/10.1007/s00586-013-2850-1
Kulowski J (1936) The Orr treatment of pyogenic osteomyelitis. Ann Surg 103:613–624
Berbari EF, Kanj SS, Kowalski TJ, Darouiche RO, Widmer AF, Schmitt SK, Hendershot EF, Holtom PD, Huddleston PM 3rd, Petermann GW, Osmon DR (2015) Infectious Diseases Society of America. 2015 Infectious Diseases Society of America (IDSA) Clinical Practice Guidelines for the Diagnosis and Treatment of Native Vertebral Osteomyelitis in Adults. Clin Infect Dis 61:e26–e46. https://doi.org/10.1093/cid/civ482
Pola E, Autore G, Formica VM, Pambianco V, Colangelo D, Cauda R, Fantoni M (2017) New classification for the treatment of pyogenic spondylodiscitis: validation study on a population of 250 patients with a follow-up of 2 years. Eur Spine J 26(Suppl 4):479–488. https://doi.org/10.1007/s00586-017-5043-5
Jean M, Irisson JO, Gras G, Bouchand F, Simo D, Duran C, Perronne C, Mulleman D, Bernard L, Dinh A (2017) Diagnostic delay of pyogenic vertebral osteomyelitis and its associated factors. Scand J Rheumatol 46:64–68. https://doi.org/10.3109/03009742.2016.1158314
Leone A, Dell’Atti C, Magarelli N, Colelli P, Balanika A, Casale R, Bonomo L (2012) Imaging of spondylodiscitis. Eur Rev Med Pharmacol Sci 16(Suppl 2):8–19
Ramadani N, Dedushi K, Kabashi S, Mucaj S (2017) Radiologic Diagnosis of Spondylodiscitis, Role of Magnetic Resonance. Acta Inform Med 25:54–57. https://doi.org/10.5455/aim.2017.25.54-57
Lee IS, Lee JS, Kim SJ, Jun S, Suh KT (2009) Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography imaging in pyogenic and tuberculous spondylitis: preliminary study. J Comput Assist Tomogr 33:587–592. https://doi.org/10.1097/RCT.0b013e318187fef8
Bernard L, Dinh A, Ghout I, Simo D, Zeller V, Issartel B, Le Moing V, Belmatoug N, Lesprit P, Bru JP, Therby A, Bouhour D, Dénes E, Debard A, Chirouze C, Fèvre K, Dupon M, Aegerter P, Mulleman D (2015) Duration of Treatment for Spondylodiscitis (DTS) study group (2015) Antibiotic treatment for 6 weeks versus 12 weeks in patients with pyogenic vertebral osteomyelitis: an open-label, non-inferiority, randomised, controlled trial. Lancet 385:875–882. https://doi.org/10.1016/S0140-6736(14)61233-2
Park KH, Cho OH, Lee JH, Park JS, Ryu KN, Park SY, Lee YM, Chong YP, Kim SH, Lee SO, Choi SH, Bae IG, Kim YS, Woo JH, Lee MS (2016) Optimal duration of antibiotic therapy in patients with hematogenous vertebral osteomyelitis at low risk and high risk of recurrence. Clin Infect Dis 62:1262–1269. https://doi.org/10.1093/cid/ciw098
Roblot F, Besnier JM, Juhel L, Vidal C, Ragot S, Bastides F, Le Moal G, Godet C, Mulleman D, Azaïs I, Becq-Giraudon B, Choutet P (2007) Optimal duration of antibiotic therapy in vertebral osteomyelitis. Semin Arthritis Rheum 36:269–277
Grados F, Lescure FX, Senneville E, Flipo RM, Schmit JL, Fardellone P (2007) Suggestions for managing pyogenic (non-tuberculous) discitis in adults. Joint Bone Spine 74:133–139
Pola E, Logroscino CA, Gentiempo M, Colangelo D, Mazzotta V, Di Meco E, Fantoni M (2014) Medical and surgical treatment of pyogenic spondylodiscitis. Eur Rev Med Pharmacol Sci 16(Suppl 2):35–49
Nasto LA, Colangelo D, Mazzotta V, Di Meco E, Neri V, Nasto RA, Fantoni M, Pola E (2014) Is posterior percutaneous screw-rod instrumentation a safe and effective alternative approach to TLSO rigid bracing for single-level pyogenic spondylodiscitis? Results of a retrospective cohort analysis. Spine J 14:1139–1146. https://doi.org/10.1016/j.spinee.2013.07.479
Turel MK, Kerolus M, Deutsch H (2017) The role of minimally invasive spine surgery in the management of pyogenic spinal discitis. J Craniovertebr Junction Spine 8:39–43. https://doi.org/10.4103/0974-8237.199873
Acknowledgements
The authors declare that they received no grants or funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pola, E., Taccari, F., Autore, G. et al. Multidisciplinary management of pyogenic spondylodiscitis: epidemiological and clinical features, prognostic factors and long-term outcomes in 207 patients. Eur Spine J 27 (Suppl 2), 229–236 (2018). https://doi.org/10.1007/s00586-018-5598-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-018-5598-9