Abstract
Purpose
To determine the incidence of pseudarthrosis at the osteotomy site after three-column spinal osteotomies (3-COs) with posterior column reconstruction.
Methods
82 consecutive adult 3-COs (66 patients) with a minimum of 2-year follow-up were retrospectively reviewed. All cases underwent posterior 3-COs with two-rod constructs. The inferior facets of the proximal level were reduced to the superior facets of the distal level. If that was not possible, a structural piece of bone graft either from the local resection or a local rib was slotted in the posterior column defect to re-establish continual structural posterior bone across the lateral margins of the resection. No interbody cages were used at the level of the osteotomy.
Results
There were 34 thoracic osteotomies, 47 lumbar osteotomies and one sacral osteotomy with a mean follow-up of 52 (24–126) months. All cases underwent posterior column reconstructions described above and the addition of interbody support or additional posterior rods was not performed for fusion at the osteotomy level. Among them, 29 patients underwent one or more revision surgeries. There were three definite cases of pseudarthrosis at the osteotomy site (4%). Six revisions were also performed for pseudarthrosis at other levels.
Conclusion
Restoration of the structural integrity of the posterior column in three-column posterior-based osteotomies was associated with > 95% fusion rate at the level of the osteotomy. Pseudarthrosis at other levels was the second most common reason for revision following adjacent segment disease in the long-term follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal osteotomies are the surgical technique of choice when correcting rigid and severe deformities [1, 2]. Relatively high rates of pseudarthrosis at the level of the osteotomy have been described as a complication following three-column spinal osteotomies (3-COs). Within adult spinal deformity correction, the rate of pseudarthrosis at the site of the 3-CO ranges from 0 to 56.3% [3,4,5,6,7,8,9,10,11,12]. This may be partly due to the differences in the surgical technique and surgical diagnosis. The resection of the posterior column to achieve the required decompression often leaves a posterior column defect, leading to pseudarthrosis and implant failure [5] even with the use of cages or other forms of interbody support [3, 5,6,7,8, 10,11,12,13,14].
The aim of this paper is to determine the incidence and potential causes of pseudarthrosis at the osteotomy site in patients undergoing 3-COs. It is hypothesized that re-establishing the integrity of the posterior column at the region of the osteotomy is a key factor in promoting local fusion.
Materials and methods
Patient selection
Following Research Ethics Board approval, 66 consecutive adult patients who underwent spinal fusion with posterior 3-COs between 2001 and 2012 were identified. Two observers not involved in patient care independently reviewed all medical records. All patients were followed for a minimum of 2 years or displayed obvious implant failure at the site of the osteotomy prior to the 2-year mark. Inclusion criteria were patients who had one or more single level pedicle subtraction osteotomy (PSO), offset PSO or partial body resection with no anterior column support. Vertebral column resections (VCR) of one or more levels requiring anterior column support were not included in this review.
Demographics
Demographic data collected included age, gender, time to maximum follow-up, smoking status and surgical diagnosis. Surgical diagnosis included degenerative and congenital kyphoscoliosis, degenerative, congenital, post-traumatic and Scheurmann’s kyphosis, ankylosing spondylitis, proximal junctional kyphosis (PJK), idiopathic and congenital scoliosis and flat back deformity.
Surgical technique
The surgical technique for PSO has been described previously in the literature [15]. Pedicle screw-based construct was used for all cases, and screws were placed in the adjacent levels to the osteotomy site whenever possible for better control of reduction. PSOs (Schwab type 3) were performed for primarily sagittal plane deformities, transdiscal PSOs (Schwab type 4) were performed for post-traumatic deformities, offset PSOs for primarily sagittal plane with some coronal deformity and partial VCRs (offset PSO with partial resection of anterior body) for combined deformities with a significant coronal component [2]. After completion of the osteotomy, the osteotomy was closed by approximating the inferior facets of the proximal level to the superior facet of the distal level (Fig. 1). If bone-to-bone contact could not be achieved, then a structural bone graft obtained from the local area of resection (large pieces of spinous process, pedicle/body fragments) or from rib harvested locally (for thoracic level osteotomies) was used to bridge the gap across the lateral margins of resection (Fig. 2). The decorticated structural bone graft was placed after the rods were secured in position and press fitted into similarly decorticated host bone slotted between the distal end of the remaining inferior facet (proximal level) and the proximal margin of the distal pedicle, with the graft placed ventral to the rod. Compression of the adjacent screws was performed to further secure the press-fit graft. No interbody cages or other forms of anterior support were used at the level of the osteotomy. No fusion adjuncts or biologics were utilized. In all cases, a single posterior 5.5 mm rod was placed on each side.
Artist rendering completed bone resection a for a pedicle subtraction osteotomy demonstrating preservation of the inferior facet of the proximal level and superior facet of the distal level. Following closure of the osteotomy (b), a new facet joint is created by reduction of the inferior facet of the proximal level to the superior facet of the distal level, maintaining integrity of the posterior column
Three cases demonstrating structural restoration of the posterior column following closure of the osteotomies. Posterior column defect a created by lumbar osteotomy through a solid fusion mass is closed b with bone on bone contact of the posterior column. c A thoracic osteotomy partially closed on one side and reinforced with a structural rib graft, which is press-fit between the rod and the posterior column. d The final construct prior to closure with the morselized local bone graft that was placed in a bone mill spread along the fusion bed. e The defect created following a lower thoracic osteotomy. After closure of the osteotomy (f), direct bone on bone contact is achieved on one side with a small gap on the near side. A local rib is fashioned and partially seated g into the defect. Following impaction of the rib graft into the defect and compression of the graft in position (h), a solid posterior column is re-established
Intra-operative and post-operative data
Intra-operative and post-operative data were collected from electronic patient records and the operative note. Information collected included the number, and level and type of 3-COs performed. Short- and long-term complications were recorded.
Radiographic analysis
The follow-up radiological examinations were reviewed to identify pseudarthrosis both at the level of the osteotomy and at other vertebral levels. The criteria to identify pseudarthrosis has been described in the literature and include signs of instrumentation loosening or failure, radiological or clinical progression of deformity, loss of disc height in serial post-op radiographs and motion on dynamic radiographs and at revision surgery [16]. All cases of suspected pseudarthrosis underwent CT scans to assess the fusion.
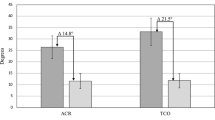
Outcome measure and statistical analysis
Scoliosis Research Society (SRS)-24 or SRS-30 questionnaires were provided at baseline and at the final follow-up. For comparisons between pre- and post-operative outcomes, paired Student’s t test was used. All statistical analyses were performed using IBM SPSS Statistics software version 19.0 (SPSS, Inc., Chicago, IL, USA), and P values < 0.05 were considered to be statistically significant.
Results
66 consecutive patients underwent a total of 82 3-COs with posterior column reconstruction (Table 1). There were 21 males and 45 females with a mean age of 51.7 years (19–77) at the time of surgery. Ten patients were active smokers (15%). Among patients with kyphoscoliosis, 20 patients were diagnosed with degenerative kyphoscoliosis and 1 with congenital kyphoscoliosis. Among patients with kyphosis, seven were diagnosed with degenerative kyphosis, six with post-traumatic kyphosis, four with Scheuermann’s kyphosis, four with ankylosing spondylitis, three with PJK and two cases of congenital kyphosis. Among patients with scoliosis, there were eight cases of idiopathic scoliosis and five cases of congenital scoliosis. Six patients presented with flat back deformity. 74 PSOs and 8 partial vertebrectomies were performed. There were 34 thoracic osteotomies (Fig. 3), 47 lumbar osteotomies (Fig. 4) and one sacral osteotomy. The mean duration of follow-up was 52.8 months (range 24–126 for fused patients). Mean sagittal balance (C7-SVA) was significantly improved from 68.4 to 22.3 mm (P < 0.001), and mean coronal balance (C7-CSVL) was changed from 25.4 to 21.8 mm (P = 0.32). Summary of SRS scores is shown in Table 2. All domain scores and the total score showed significant post-operative improvements. There were a total of 42 post-operative complications and 29 patients underwent one or more revision surgeries (Table 3).
Long cassette posteroanterior (a) and lateral (b) of a 19-year-old woman treated with a T2–L2 fusion (c, d) with a pedicle subtraction osteotomy at T8. Coronal CT scan at 1 week (e) and a repeat coronal (f) and sagittal (g) CT at 27 months show a solid posterior fusion across the level of the osteotomy (white arrow) and throughout the construct (h)
Pseudarthrosis at the osteotomy site
There were three definitive pseudarthrosis at the osteotomy site (4%) that were later revised. Two of these patients were active smokers. One was a 48-year-old female, who underwent a T4-pelvis instrumented fusion with an L3 PSO for ankylosing spondylitis (AS). She required a revision fusion at 14 months post-operatively. Imaging at the latest follow-up (57 months) shows a solid fusion and she has not required further revision (Fig. 5). The second patient was a 68-year-old female with a previous L2–S1 fusion for degenerative deformity and was treated with an L2 PSO and T5–S1 posterior instrumented fusion for proximal junction failure. She sustained a rod fracture and pseudarthrosis at the site of the osteotomy and underwent revision surgery at 15 months with good result. The third patient was a 67-year-old male who underwent three corrective surgeries for degenerative kyphoscoliosis including L1 PSO. Subsequently, he fractured the unilateral rod at the osteotomy site 32 months after the first procedure. Revision surgery was performed with posterior column reconstruction by another structural bone graft and smoking cessation was encouraged. Solid bone fusion was obtained with the optimal clinical outcome at 2 years.
X-rays of pre-operative (a, b), post-operative (c, d) and following pseudarthrosis (e, f) of a patient with pseudarthrosis and bilateral broken rods at the site of osteotomy (L3). At 14 months post-operatively, the patient underwent revision and fusion. Imaging at the latest follow-up (57 months) shows a solid construct (g, h)
Other complications
Six patients (9%) had pseudarthrosis not associated with the osteotomy site. There were 11 cases of PJK, 6 cases of incomplete correction, 4 neurologic complications, 3 adjacent level fractures, 2 asymptomatic broken rods with no pseudarthrosis on CT and 2 cases of infection. There were three cases of instrumentation complications due to painful or loose hardware.
Discussion
The results of this series demonstrate a fusion rate of 96.3% at the osteotomy site in patients undergoing posterior-only spinal fusion surgery with a single level partial body 3-CO. All cases had structural bone, either local or harvested from a local rib, placed across the posterior column bridging or supplementing the host bone in the region of the facet joints. The three cases with pseudarthrosis at the osteotomy site were following pedicle subtraction osteotomy in smokers. The rate of pseudarthrosis at other sites was 9%. No anterior column support or bone graft adjuncts were used in these cases. All cases had posterior constructs with two rods.
Pseudarthrosis at the osteotomy site is one of the potentially avoidable events by surgical technique among the various complications encountered in osteotomy cases. Our results demonstrate that re-establishing the structural integrity of the posterior column through direct bone-to-bone contact or with the addition of local structural bone graft leads to excellent fusion rates at the site of the osteotomy (Fig. 2). Our surgical technique emphasizes the importance of establishing good lateral bone-to-bone contact, similar to a previously published series [3]. We did not use cross-links in the latter half of this study, since higher rates of pseudarthrosis were noted at the site of cross-links. Other authors have similarly shown a pseudarthrosis rate of up to 69% at the site of cross-links [17].
A posterior-only approach with a focus on re-establishing bone-to-bone contact has been successful in previous series [3, 6,7,8]. This was established in the current series by limiting the lateral posterior resection to include the complete posterior elements at the level of the osteotomy only. Closure of the osteotomy would create a new ‘facet joint’ comprising the inferior facet of the level proximal to the superior facet of the level distal to the osteotomy. If this was not possible, local structural bone was added to maintain or supplement the structural integrity of the posterior column. Bridwell et al. first described the technique of ensuring lateral bone-to-bone contact during osteotomy closure and reported a pseudarthrosis rate at the osteotomy site of 1.5% [3]. Ikenaga et al. utilized morselized local bone chips as a graft at the site of the PSO. In 67 patients undergoing PSO, they recorded no pseudarthrosis at the site of the osteotomy [6]. In a small cohort of patients undergoing a modified VCR (n = 13), Wang et al. used harvested iliac bone sticks when rod compression alone was unable to restore the posterior column. They had no recorded pseudarthrosis at the osteotomy site at the last follow-up [8]. Our series is the first to demonstrate the effectiveness of a localized structural bone graft to promote fusion in a posterior-only approach for both PSO and partial vertebrectomies.
Some authors have suggested that the addition of anterior column support or staging with anterior plating improves sagittal balance [5, 13]. In the present case series, we did not have any cases that necessitated staged anterior procedures. When the posterior environment for bone union is severely impaired (e.g., scar formation after multiple revision surgeries, post-radiation and massive congenital/iatrogenic bone loss), anterior fusion could be an important option. However, correcting the sagittal balance through the osteotomy offloads the anterior column in the lumbar spine, directing the force through the posterior column. Anterior column support in these settings will not protect the posterior column, especially if there is a structural defect in the posterior column, which is common following the decompression required for these osteotomies. Posterior reconstruction with or without bone graft enables the structural continuity of bone that allows load sharing on the posterior side of the spinal axis. Smith et al. analyzed the incidence of pseudarthrosis in the form of symptomatic rod fractures following posterior-only fusion and posterior fusion with anterior support. They demonstrated that the majority of the patients (56%) who underwent anterior column support had a symptomatic rod fracture [12]. Similarly, a review of 35 patients by Yang et al., in which all patients received anterior column support, reported a rod fracture rate of 14.3% [5]. Hyun et al. reported a rod fracture rate of 7.7% at the osteotomy site in their series of 13 patients [10]. All major published series using anterior column support following three-column osteotomies showed a higher incidence of pseudarthrosis at the site of three-column osteotomy [5, 10, 12, 13]. This may be explained by the decompression required to place the interbody device [i.e., transforaminal lumbar interbody fusion (TLIF)] which further compromises the integrity of the posterior column. With a restored sagittal alignment following the osteotomy, the gravity line is directed through the posterior column and not the anterior column. This leads to compressive forces through the posterior column, leaving the interbody device in the anterior column unable to load share the construct [16]. An anteriorly placed interbody support that avoids disruption of the posterior column may have less of a negative impact.
Multiple rods placed around the osteotomy site have also been described to prevent early rod fracture. In a finite element model, Luca et al. demonstrated up to a 50% reduction of the stress on the spinal fixators at the level of the osteotomy [18]. While this technique may prevent rod breakage, it leaves very little room for fusion, and delayed infection at this site or rod fracture at the sites of the connectors may be seen in long-term follow-up [16, 18, 19]. Comorbidities, such as smoking and osteoporosis, play a role in the development of pseudarthrosis [20, 21]. All three patients who had pseudarthrosis at the osteotomy site in the current series received lumbar PSO and were active smokers. While all patients were educated pre-operatively on the importance of smoking cessation in the success of these surgeries, we were surprised at the high percentage of our patients that continued to smoke despite undergoing these major procedures. We feel this contributed to our high revision rate in this series. Given the small number of pseudarthrosis cases in our cohort, we found it unfeasible to run any risk factor analyses. However, the smoking rate in pseudarthrosis patients was extremely high (5 out of 9 patients). Ongoing work on bone turnover markers may shed further light into the etiology of pseudarthrosis [22].
A shortcoming of this study is the use of historical controls to compare our data. Since this was a single surgeon series, the procedures were performed in a consistent manner, which did not offer a control group. Another weakness is the heterogeneity of the study population and the osteotomy procedures (PSO, VCR and their modifications). While we feel that re-establishing the structural integrity of the posterior column is key to achieving fusion at the level of the osteotomy, other factors such as sagittal alignment, smoking and comorbidities (i.e., obesity and osteoporosis) could have contributed to the pseudarthrosis rate as well. While we have been able to decrease the incidence of pseudarthrosis at the osteotomy site, our series highlights the high rate of complications associated with three column osteotomies. As a result, we have shifted our practice to perform more posterior column osteotomies when the anterior column is mobile and when adequate correction can be achieved through these less complex osteotomies.
Conclusion
Re-establishing the structural integrity of the posterior column following 3-COs contributed to a greater than 95% fusion rate at the level of the osteotomy in this series. This was achieved with direct bone-to-bone closure of the osteotomy or with the addition of local structural bone if a posterior column gap persisted after osteotomy closure. No adjuvant graft material, biologics or anterior column support was utilized at the level of the osteotomy. These results are much better than those observed in other series using anterior column cages. These results demonstrate the importance of a structurally stable posterior column in the successful fusion at the osteotomy site of partial body 3-COs.
References
Gill JB, Levin A, Burd T et al (2008) Corrective osteotomies in spine surgery. J Bone Jt Surg Am 90:2509–2520
Schwab F, Blondel B, Chay E et al (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74:112–120 (discussion 120)
Bridwell KH, Lewis SJ, Edwards C et al (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 28:2093–2101. doi:10.1097/01.BRS.0000090891.60232.70
Suk SI, Chung ER, Lee SM et al (2005) Posterior vertebral column resection in fixed lumbosacral deformity. Spine (Phila Pa 1976) 30:E703–E710
Yang BP, Ondra SL, Chen LA et al (2006) Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine 5:9–17. doi:10.3171/spi.2006.5.1.9
Ikenaga M, Shikata J, Takemoto M et al (2007) Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine 6:330–336. doi:10.3171/spi.2007.6.4.8
Kim YJ, Bridwell KH, Lenke LG et al (2007) Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine (Phila Pa 1976) 32:2189–2197. doi:10.1097/BRS.0b013e31814b8371
Wang Y, Zhang Y, Zhang X et al (2008) A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J 17:361–372. doi:10.1007/s00586-007-0566-9
O’Shaughnessy BA, Kuklo TR, Hsieh PC et al (2009) Thoracic pedicle subtraction osteotomy for fixed sagittal spinal deformity. Spine (Phila Pa 1976) 34:2893–2899. doi:10.1097/BRS.0b013e3181c40bf2
Hyun SJ, Rhim SC (2010) Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc 47:95–101. doi:10.3340/jkns.2010.47.2.95
Kim KT, Lee SH, Suk KS et al (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine (Phila Pa 1976) 37:1667–1675. doi:10.1097/BRS.0b013e3182552fd0
Smith JS, Shaffrey CI, Ames CP et al (2012) Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 71:862–867. doi:10.1227/NEU.0b013e3182672aab
Saer Iii EH, Winter RB, Lonstein JE (1990) Long scoliosis fusion to the sacrum in adults with nonparalytic scoliosis: an improved method. Spine 15:650–653
Auerbach JD, Lenke LG, Bridwell KH et al (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine 37:1198–1210
Bridwell KH, Lewis SJ, Lenke LG et al (2003) Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Jt Surg Am 85:454–463
Gupta M, Henry JK, Schwab F et al (2016) Reducing rod breakage and pseudarthrosis in pedicle subtraction osteotomy: the importance of rod number and configuration in 264 patients with 2-year follow-up. Glob Spine J 6:0036. doi:10.1055/s-0036-1582911
Kim YJ, Bridwell KH, Lenke LG et al (2005) Pseudarthrosis in primary fusions for adult idiopathic scoliosis: incidence, risk factors, and outcome analysis. Spine 30:468–474
Luca A, Ottardi C, Sasso M et al (2017) Instrumentation failure following pedicle subtraction osteotomy: the role of rod material, diameter, and multi-rod constructs. Eur Spine J 26:764–770. doi:10.1007/s00586-016-4859-8
Palumbo MA, Shah KN, Eberson CP et al (2015) Outrigger rod technique for supplemental support of posterior spinal arthrodesis. Spine J 15:1409–1414
Brown CW, Orme TJ, Richardson HD (1986) The rate of pseudarthrosis (surgical nonunion) in patients who are smokers and patients who are nonsmokers: a comparison study. Spine 11:942–943
Calori GM, Albisetti W, Agus A et al (2007) Risk factors contributing to fracture non-unions. Injury 38:S11–S18
Inose H, Yamada T, Mulati M et al (2016) Bone turnover markers as a new predicting factor for non-union after spinal fusion surgery. Spine. doi:10.1097/BRS.0000000000001995
Acknowledgements
REB approval was granted prior to start of the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SJL: consulting for Stryker and Medtronic; receives payment for lectures and travel for meetings from Medtronic, Stryker and AO. He is a stockholder in Augmedics and Thompson Surgical. CM: nothing to disclose. AMG: nothing to disclose. SK: nothing to disclose. SGK: nothing to disclose. NDL: nothing to disclose. SPM: nothing to disclose. DP: nothing to disclose. JC: nothing to disclose.
Source of funding
None of the authors received financial support in relation to this manuscript.
Rights and permissions
About this article
Cite this article
Lewis, S.J., Mohanty, C., Gazendam, A.M. et al. Posterior column reconstruction improves fusion rates at the level of osteotomy in three-column posterior-based osteotomies. Eur Spine J 27, 636–643 (2018). https://doi.org/10.1007/s00586-017-5299-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5299-9