Abstract
Purpose
The purpose of this study was to compare patient-reported outcomes (PROs), morbidity, and costs of TLIF vs PLF to determine whether one treatment was superior in the setting of single-level degenerative spondylolisthesis.
Methods
Patients undergoing TLIF or PLF for single-level spondylolisthesis were included for retrospective analysis. EQ-5D, ODI, SF-12 MCS/PCS, NRS-BP/LP scores were collected at baseline and 24 months after surgery. 90-day post-operative complications, revision surgery rates, and satisfaction scores were also collected. Two-year resource use was multiplied by unit costs based on Medicare payment amounts (direct cost). Patient and caregiver workday losses were multiplied by the self-reported gross-of-tax wage rate (indirect cost). Total cost was used to assess mean total 2-year cost per QALYs gained after surgery.
Results
62 and 37 patients underwent TLIF and PLF, respectively. Patients in the PLF group were older (p < 0.01). No significant differences were seen in baseline or 24-month PROs between the two groups. There was a significant improvement in all PROs from baseline to 24 months after surgery (p < 0.001). Both groups had similar rates of 90-day complications, revision surgery, satisfaction, and similar gain in QALYs and cost per QALYs gained. There was no significant difference in 24-month direct, indirect, and total cost.
Conclusions
Overall costs and health care utilization were similar in both the groups. Both TLIF and PLF for single-level degenerative spondylolisthesis provide improvement in disability, pain, quality of life, and general health.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the setting of degenerative spondylolisthesis, lumbar fusion may lead to improved patient-reported outcomes compared with decompression alone [1, 2]. The use of interbody fusion (IBF) devices as adjuncts has drastically increased over time [3, 4]. In 2010, an estimated 83% of all lumbar fusions for degenerative spondylolisthesis incorporated interbody fusion [5]. Rationale for the use of the IBF in the setting of degenerative spondylolisthesis includes increased disc height with indirect decompression, reduction of slippage, more favorable fusion environment compared to the posterior lateral gutters, and load sharing with posterior instrumentation [6,7,8,9]. However, the translation to clinical benefits has yet to be adequately demonstrated.
Controversy exists due to conflicting studies that have questioned the benefits of IBF. A recent meta-analysis by McAnany et al. demonstrated that there were no differences in fusion rates, operative time, estimated blood loss, Oswestry Disability Index (ODI), SF-36 Physical Component Score (SF-36 PCS), Visual Analog Scale (VAS), or complication rates between PLF and IBF in degenerative spondylolisthesis while patients undergoing IBF had greater length of hospital stay [10]. Another recent systematic review by Baker et al. suggests that patients with instability may benefit most from IBF [11]. Furthermore, while the addition of an interbody fusion may increase surgical costs, financial burden is not well defined in the literature with some studies presenting conflicting evidence about the effect on long-term cost compared to PLF alone [8, 12].
Few studies have assessed whether interbody fusion provides improved outcomes while using transforaminal lumbar interbody fusion (TLIF) as their sole method of IBF. The purpose of this study was to compare patient-reported outcomes (PROs), morbidity, direct and indirect healthcare costs of TLIF vs PLF. We sought to analyze whether the addition of TLIF led to superior patient-reported outcomes compared to PLF alone in the setting of single-level lumbar degenerative spondylolisthesis.
Materials and methods
A retrospective analysis of prospectively collected data between 2010 and 2013 was performed from a single institution. An approval for the study and wavier of informed consent was obtained from the institutional review board (IRB) for all the patients entered into the registry. The inclusion criteria for the study were: (1) patients age >18 years; (2) presenting with leg and/or back pain; (3) correlative imaging findings for the diagnosis of degenerative spondylolisthesis; and (4) failure of multimodal non-operative measures over 3 months or patients with progressive neurological deficit. The exclusion criteria were: (1) diagnosis of spinal tumor, trauma, or infection; (2) degenerative spine diagnosis other than spondylolisthesis; (3) multi-level spine disease; (4) any extra-spinal cause of back or leg pain; and (5) patients who were unwilling or unable to participate in the follow-up questionnaires.
Patients undergoing either TLIF or PLF for single-level degenerative spondylolisthesis of the lumbar spine were analyzed. In the TLIF cohort, interbody fusion was performed as an adjunct to posterolateral fusion with pedicle screw fixation. The decision to perform a TLIF was at the discretion of the treating surgeon. Patients operated on by six surgeons were entered into the registry. All surgeons are fellowship-trained spine surgeons with varying level of seniority. The treating surgeons diagnosed patients based on clinical examination and correlative imaging findings.
Patient demographics including age, body mass index (BMI), duration and amount preoperative opioid use, smoking status, duration of symptoms, employment status, comorbidities (diabetes, hypertension, coronary artery disease, myocardial infarction, preoperative anticoagulation, congestive heart failure, chronic obstructive pulmonary disease, and osteoporosis), clinical presentation, operative variables (intra-operative estimated blood loss, length of surgery, length of hospital stay, graft type), and post-operative morbidity (complications, readmission, discharge destination, and revision surgery) were reviewed through electronic medical records. Zung Self-Rating Depression Scale (ZDS) of >33 was used to dichotomize patients into depressed and non-depressed groups [13, 14]. Modified Somatic Perception Questionnaire MSPQ of >12 was used to dichotomize patients into anxious and non-anxious groups [15]. The following validated PROs were recorded at baseline and 24 months after surgery: (1) back-related disability: Oswestry Disability Index (ODI) [16]; (2) numeric rating scale (NRS) pain scores for back pain and leg pain [17]; (3) quality of life: EuroQol-5D (EQ-5D) [18]; (4) general health: Short-form-12 item health surgery (SF-12), Physical component score (PCS) and Mental component score (MCS) [19]; (5) satisfaction: North American Spine Society (NASS) satisfaction questionnaire [20].
Clinically significant improvement in disability (ODI), pain (NRS-BP and LP) and quality of life (EQ-5D) were defined using the concept of minimum clinically important difference (MCID). The MCID represents a critical threshold, compared with the baseline, which is considered a clinically meaningful improvement to the patient. The MCID compares the change in score for a PRO following the intervention to another externally validated measure of outcomes such as perceived improvement or satisfaction following the procedure in question [21, 22]. Previously published MCID values for the ODI (14.9), NRS-BP (2.1) and NRS-LP (2.8) scores, and the EQ-5D (0.46) were used to dichotomize the patient groups based on whether MCID was achieved [23].
Cost data
Total 2-year costs included those associated with the inpatient hospital stay (hospital cost), surgeons’ professional fees, and 2-year post-discharge health care utilization. All costs were calculated based on Medicare national payment amounts. A unit multiplier was used to standardize and eliminate any geographic variations. Such calculations have been reported previously [24,25,26]. The hospital costs were derived based on the diagnosis-related group (DRG). Surgeons’ professional fees were derived based on current procedural terminology (CPT) codes. Post-discharge resource utilization was derived from CPT codes assigned for patient self-reported resource utilization. Low back-related outpatient visits to surgeons, other physicians, chiropractors, physical and occupational therapists, and acupuncturists were captured. Diagnostic tests including radiographs, CT scans, MR imaging, and electromyography were tracked. Pre- and post-operative devices utilized (braces, canes, and walkers), epidural steroid injections, emergency department visits, back-specific medications [non-steroidal anti-inflammatory drugs (NSAIDs), oral steroids, narcotics, muscle relaxants, and antidepressants], and inpatient or outpatient rehabilitation resources were assessed. The costs associated with readmissions to our institution during the 90-day global period were also recorded.
Indirect costs included patient or family member workday losses and cost of a caregiver, if this was needed. Loss of work days were estimated by assessing the productivity losses due to spine-related problems such as missed workdays for those employed outside the home. Patient income loss is calculated for the patients that were pre-operatively employed and did not retire up to 2 years after surgery. Costs for missed days of unpaid caregivers were estimated based on average gross wages plus non-health benefits. Using the standard human capital approach, costs were estimated by multiplying the change in hours worked by the gross-of-tax wage rate (gross income before taxes are deducted) based on wages reported by patients at study entry. All the indirect costs were estimated based on 2012 median patient and family income rates. Such calculations for indirect costs have been previously validated [24, 25, 27,28,29,30].
Statistical analysis
Mean (standard deviation) and median (range) for continuous variables and frequency for categorical variables were computed. Student’s t test and Mann–Whitney U test was used for continuous data. Nominal data was compared via Chi-squared test. Quality-adjusted life years were calculated from the EQ-5D with US valuation. 1- and 2-year spine-related medical resource utilization, missed work, and health state values (QALYs, calculated from the EQ-5D with US valuation using time-weighted area under the curve approach) were assessed. QALYs at 1- and 2-year are presented as mean and 95% CI. Mean total 1- and 2-year cost per QALYs gained after surgery was assessed for TLIF vs. PLF groups. Total cost (direct + indirect) was used to assess mean total 2-year cost per QALY gained for TLIF vs. PLF surgery. For indirect costs, the average indirect costs for all patients were calculated. A p value <0.05 was considered statistically significant. Analysis was performed using SPSS version 20 (IBM Inc, Chicago, IL, USA).
Results
A total of 62 patients underwent TLIF and 37 patients underwent PLF. Table 1 illustrates the preoperative characteristics of the patients in the study. There was a significant difference seen in age with older patients belonging to the PLF cohort [58.7 (31.5–75.9) vs. 65.8 (29.7–83.7) p = 0.006]. No significant differences were seen with regards to duration of symptoms, duration of pre-operative opioid use, BMI, co-morbidities, or employment status. EBL, length of surgery, length of hospital stay, and discharge destination also showed no statistical difference.
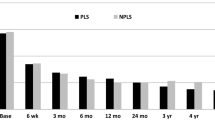
No significant differences were seen in PROs at baseline or 24 month between the two groups (Table 2). There was a significant improvement in all PROs from baseline to 24 months after surgery (p < 0.001). Patients in the TLIF cohort compared to PLF had significantly higher improvement in general physical health (SF-12 PCS: 12.3 ± 12.1 vs. 6.1 ± 14.1, p = 0.03) and back pain (NRS-BP: 3.6 ± 3.2 vs. 2.3 ± 2.7, p = 0.04). Both groups had similar rates of 90-day complications [6.5% (n = 4) vs. 13.5% (n = 5), p = 0.237], 90-day readmissions [3.2% (n = 2) vs. 2.7% (n = 1), p = 0.687], and revision surgery within the 2-year post-operative period [8.1% (n = 5) vs. 10.8% (n = 4), p = 0.724]. The patients undergoing TLIF had higher rate of return to work (RTW) within 90 days, however, the difference did not reach statistical significance. (82.7 vs. 66.7%, p = 0.202). There were no differences in the frequency of patients achieving satisfaction at 2 years post-operatively [NASS 1 and 2: 84% (n = 52) vs. 81% (n = 30), p = 0.82].
The total 2-year costs associated with TLIF was $34,708 ($23,931–$64,700, 95% CI) which was similar to the total cost associated with PLF $34,977 ($24,675–$69,844), (p = 0.901). There was no significant difference in 24-month direct [$29,648 ($17,296–$47,639) vs. $31,554 ($24,675–$67,536), (p = 0.204)] and indirect costs [$5059 ($3398–$6719) vs. $3423 ($1523–$5323), (p = 0.19)] between TLIF and PLF cohorts. There was a significant difference in terms of surgeon’s professional fee [$3068 ($2949–$3187) vs. $2784 ($2604–$2965), p = 0.010] with costs being higher in the TLIF group (Table 3). Both the groups had similar post-discharge resource utilization, except with regards to frequency of MRI scans, which was higher in the PLF group [19.3% (n = 12) vs. 40.5% (n = 15), p = 0.022] (Table 4).
Both groups had significant gain in QALY from 1 year (TLIF: 0.26, PLF 0.32) to 2 years (TLIF: 0.43, PLF 0.50), p = 0.01. The TLIF group had 0.43 QALYs gained at 2 years and the PLF group had 0.50 QALYs gained (p = 0.604). The cost per QALYs gained at 2 years was $80,716 per QALY gained in the TLIF group vs. $69,954 per QALY gained in the PLF group (p = 0.21) (Table 5).
Discussion
The purpose of this study was to compare PROs, morbidity, and cost-effectiveness of TLIF and PLF in patients with single-level lumbar degenerative spondylolisthesis. Both groups had similar demographics and comorbidities except that patients who underwent PLF were significantly older compared to those who underwent TLIF. No significant differences in improvement were seen among the two groups with regards to EQ-5D, ODI, SF-12 MCS, or NRS-LP. Furthermore, satisfaction and 90-day morbidity following surgery were also similar between the two groups. However, patients undergoing TLIF had significantly greater improvement in general physical health (SF-12 PCS) and back pain (NRS-BP) scores at 2 years compared to the PLF group (Table 6).
A previous meta-analysis by McAnany et al. demonstrated that there were no differences in fusion rates and PROs between patients undergoing IBF vs. PLF; however, the patients undergoing PLF were noted to have significantly shorter length of stay [10]. This meta-analysis included five separate studies all of which analyzed the benefits of the IBF vs. PLF for degenerative spondylolisthesis. One of the more notable studies included in this analysis was performed by Høy et al. who performed a randomized clinical trial examining the benefits of TLIF vs. PLF [31]. Their most recent follow-up data, with an impressive mean follow-up of 8.6 years, demonstrated no significant differences in ODI, SF-36, Dallas pain questionnaire (DPQ), or low back pain questionnaire (LBRS), or RTW [32]. However, this study included patients with multiple etiologies of back pain and was not unique to those with the diagnosis of degenerative spondylolisthesis. In their original study, they confirmed that their results were not powered for subgroup analysis [31]. Furthermore, McAnany et al. concluded that removal of the Høy study resulted in a loss of statistical significance in favor of PLF for length of stay in their meta-analysis [10]. In our study, there were no differences in the LOS between the two groups. Similarly, there were no significant differences in the direct cost and total cost at 2 years after TLIF and PLF surgery. There were no differences in the QALYs gained or cost per QALY gained 2 years after surgery. These results indicate that at 24 months there was no significant increase in financial burden when TLIF was added to PLF. Bydon et al. in their retrospective review demonstrated increased rates of pseudoarthrosis and reoperation in PLF vs. patients undergoing IBF with greater than 2-year follow-up [8]. This suggests that TLIF may potentially be a more durable procedure than PLF alone and cost-effectiveness may shift in favor of TLIF due to increased rates of pseudoarthrosis and reoperation with PLF when assessed with longer follow-up than 24 months.
As demonstrated in our study, patients undergoing TLIF had higher improvement in general physical health and back pain compared to PLF. While this difference may potentially have been associated by the type of procedure performed, it may also have been impacted by the significant difference in age. Patients in the TLIF cohort were on average younger than those in the PLF group which may be the reasoning for greater improvement in physical health and back pain. Overall costs as well as other outcomes were otherwise similar between the two cohorts; however, it is difficult to determine whether the addition of TLIF provides greater clinical benefit. Ha et al. in their study noted patients undergoing IBF only had significant differences in improvement in ODI and VAS compared to patients undergoing PLF when patients were noted to have dynamic degenerative spondylolisthesis [33]. The addition of an interbody fusion may provide more benefit over PLF alone primarily in patients with dynamic instability, the importance of which has been previously indicated in the literature [11, 34, 35].
Multiple previous studies have reported the benefits of IBF for patients with degenerative spondylolisthesis yet only a few studies incorporate methods using TLIF as the sole method of IBF. First described by Harms and Jeszensky, the TLIF is a modification to the posterior lumbar interbody fusion (PLIF) procedure using a more lateral approach through the vertebral foramen to access the disc space reducing some of the risks and limitations associated with PLIF such as increased retraction of the thecal sac and neural elements [36]. A few comparative studies have shown that TLIF affords outcomes similar to PLIF and have even shown TLIF to be associated with less complications [37, 38]. Therefore, studies that have previously included both TLIF and PLIF treatments into a single cohort may have unintentionally introduced bias into their studies. It is critical that individual IBF methods are distinguished in any comparative study to truly assess whether one method is superior to PLF alone given that each IBF method may have statistically different outcomes. Outside of our study, Fujimori et al. provided one of the few studies that have made the distinction of using only TLIF as their method for IBF in the setting of degenerative spondylolisthesis [39]. In their retrospective cohort study, they determined that patients with TLIF had significantly greater improvement in back pain, leg pain, reduction of slippage, and post-operative disk height compared to those with PLF alone. We uniformly compared TLIF only to PLF instead of including multiple IBFs for a single disease process eliminating possible bias from heterogeneity.
There are limitations to our study that need to be addressed. First, the number of patients in each TLIF and PLF sub-groups were low. We were able to provide two-year post-operative outcomes, which is a major strength of the study; however, this unfortunately diminished our sample sizes. There was also a significant difference with regards to age between the two cohorts which limits our ability to interpret the results. This is a single institution study and the inpatient costs were derived based on the DRG. The DRG-based hospital cost will not reflect the accurate cost based on the type of implant or biologics used. The decision to perform TLIF vs PLF was at the surgeon’s discretion, and was not standardized for this analysis. The diagnosis was also confirmed by the treating surgeon only. We were also not able to retrospectively assess which patients in our study had dynamic instability pre-operatively limiting our ability to further delineate whether this subgroup of patients may have been the most to benefit from the addition of TLIF. Furthermore, there is literature suggesting that a subset of patients with degenerative spondylolisthesis may benefit from decompression alone without the addition of instrumentation [40, 41]. However, this treatment option was not included in our study, therefore, we are only able to compare the effectiveness of TLIF to PLF rather than determine the most superior method to treat this disease. Ideally, future studies that prospectively assess outcomes of TLIF compared to PLF and decompression alone in degenerative spondylolisthesis while stratifying for disease characteristics such as dynamic instability may help further improve our understanding of which patients can benefit from the addition of TLIF.
Conclusion
Both TLIF and PLF for single-level degenerative spondylolisthesis provide improvement in disability, pain, quality of life, and general health. Overall costs and health care utilization are similar in both groups. Future, randomized studies prospectively assessing patients with degenerative spondylolisthesis in the setting of dynamic instability are needed to delineate which patients may potentially benefit the most from the addition of TLIF.
References
Herkowitz HN, Kurz LT (1991) Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Jt Surg Am 73:802–808
Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, Coumans JV, Harrington JF, Amin-Hanjani S, Schwartz JS, Sonntag VK, Barker FG 2nd, Benzel EC (2016) Laminectomy plus fusion versus laminectomy alone for lumbar spondylolisthesis. N Engl J Med 374:1424–1434. doi:10.1056/NEJMoa1508788
Kepler CK, Vaccaro AR, Hilibrand AS, Anderson DG, Rihn JA, Albert TJ, Radcliff KE (2014) National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine (Phila Pa 1976) 39:1584–1589. doi:10.1097/brs.0000000000000486
Pannell WC, Savin DD, Scott TP, Wang JC, Daubs MD (2015) Trends in the surgical treatment of lumbar spine disease in the United States. Spine J 15:1719–1727. doi:10.1016/j.spinee.2013.10.014
Norton RP, Bianco K, Klifto C, Errico TJ, Bendo JA (2015) Degenerative spondylolisthesis: an analysis of the nationwide inpatient sample database. Spine (Phila Pa 1976) 40:1219–1227. doi:10.1097/brs.0000000000000987
Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG (1997) Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 22:210–219 (discussion 219–220)
McAfee PC, DeVine JG, Chaput CD, Prybis BG, Fedder IL, Cunningham BW, Farrell DJ, Hess SJ, Vigna FE (2005) The indications for interbody fusion cages in the treatment of spondylolisthesis: analysis of 120 cases. Spine (Phila Pa 1976) 30:S60–S65
Bydon M, Macki M, Abt NB, Witham TF, Wolinsky JP, Gokaslan ZL, Bydon A, Sciubba DM (2015) The cost-effectiveness of interbody fusions versus posterolateral fusions in 137 patients with lumbar spondylolisthesis. Spine J 15:492–498. doi:10.1016/j.spinee.2014.10.007
Macki M, Bydon M, Weingart R, Sciubba D, Wolinsky JP, Gokaslan ZL, Bydon A, Witham T (2015) Posterolateral fusion with interbody for lumbar spondylolisthesis is associated with less repeat surgery than posterolateral fusion alone. Clin Neurol Neurosurg 138:117–123. doi:10.1016/j.clineuro.2015.08.014
McAnany SJ, Baird EO, Qureshi SA, Hecht AC, Heller JG, Anderson PA (2016) Posterolateral fusion versus interbody fusion for degenerative spondylolisthesis: a systematic review and meta-analysis. Spine (Phila Pa 1976). doi:10.1097/brs.0000000000001638
Baker JF, Errico TJ, Kim Y, Razi A (2017) Degenerative spondylolisthesis: contemporary review of the role of interbody fusion. Eur J Orthop Surg Traumatol 27:169–180. doi:10.1007/s00590-016-1885-5
Christensen A, Hoy K, Bunger C, Helmig P, Hansen ES, Andersen T, Sogaard R (2014) Transforaminal lumbar interbody fusion vs. posterolateral instrumented fusion: cost-utility evaluation alongside an RCT with a 2-year follow-up. Eur Spine J 23:1137–1143. doi:10.1007/s00586-014-3238-6
Lebow R, Parker SL, Adogwa O, Reig A, Cheng J, Bydon A, McGirt MJ (2012) Microdiscectomy improves pain-associated depression, somatic anxiety, and mental well-being in patients with herniated lumbar disc. Neurosurgery 70:306–311. doi:10.1227/NEU.0b013e3182302ec3 (discussion 311)
Main CJ, Wood PL, Hollis S, Spanswick CC, Waddell G (1992) The distress and risk assessment method. A simple patient classification to identify distress and evaluate the risk of poor outcome. Spine (Phila Pa 1976) 17:42–52
Main CJ (1983) The modified somatic perception questionnaire (MSPQ). J Psychosom Res 27:503–514
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25:2940–2952 (discussion 2952)
Langley GB, Sheppeard H (1985) The visual analogue scale: its use in pain measurement. Rheumatol Int 5:145–148
EuroQol (1990) A new facility for the measurement of health-related quality of life. Health Policy (Amst, Neth) 16:199–208
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Daltroy LH, Cats-Baril WL, Katz JN, Fossel AH, Liang MH (1996) The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine (Phila Pa 1976) 21:741–749
Parker SL, Godil SS, Shau DN, Mendenhall SK, McGirt MJ (2013) Assessment of the minimum clinically important difference in pain, disability, and quality of life after anterior cervical discectomy and fusion: clinical article. J Neurosurg Spine 18:154–160. doi:10.3171/2012.10.spine12312
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and pain scales. Spine J 8:968–974. doi:10.1016/j.spinee.2007.11.006
Parker SL, Adogwa O, Paul AR, Anderson WN, Aaronson O, Cheng JS, McGirt MJ (2011) Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 14:598–604. doi:10.3171/2010.12.spine10472
Parker SL, Fulchiero EC, Davis BJ, Adogwa O, Aaronson OS, Cheng JS, Devin CJ, McGirt MJ (2011) Cost-effectiveness of multilevel hemilaminectomy for lumbar stenosis-associated radiculopathy. Spine J 11:705–711. doi:10.1016/j.spinee.2011.04.024
Devin CJ, Chotai S, Parker SL, Tetreault L, Fehlings MG, McGirt MJ (2015) A cost-utility analysis of lumbar decompression with and without fusion for degenerative spine disease in the elderly. Neurosurgery 77(suppl 4):S116–S124. doi:10.1227/neu.0000000000000949
Chotai S, Sielatycki JA, Parker SL, Sivaganesan A, Kay HL, Stonko DP, Wick JB, McGirt MJ, Devin CJ (2016) Effect of obesity on cost per quality adjusted life years gained following anterior cervical discectomy and fusion in elective degenerative pathology. Spine J. doi:10.1016/j.spinee.2016.06.023
Bala MM, Riemsma RP, Nixon J, Kleijnen J (2008) Systematic review of the (cost-)effectiveness of spinal cord stimulation for people with failed back surgery syndrome. Clin J Pain 24:741–756. doi:10.1097/AJP.0b013e318179032a
Adogwa O, Parker SL, Shau DN, Mendenhall SK, Aaronson O, Cheng JS, Devin CJ, McGirt MJ (2012) Cost per quality-adjusted life year gained of revision neural decompression and instrumented fusion for same-level recurrent lumbar stenosis: defining the value of surgical intervention. J Neurosurg Spine 16:135–140. doi:10.3171/2011.9.spine11308
Adogwa O, Parker SL, Shau DN, Mendenhall SK, Devin CJ, Cheng JS, McGirt MJ (2012) Cost per quality-adjusted life year gained of laminectomy and extension of instrumented fusion for adjacent-segment disease: defining the value of surgical intervention. J Neurosurg Spine 16:141–146. doi:10.3171/2011.9.spine11419
Parker SL, Adogwa O, Bydon A, Cheng J, McGirt MJ (2012) Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg 78:178–184. doi:10.1016/j.wneu.2011.09.013
Hoy K, Bunger C, Niederman B, Helmig P, Hansen ES, Li H, Andersen T (2013) Transforaminal lumbar interbody fusion (TLIF) versus posterolateral instrumented fusion (PLF) in degenerative lumbar disorders: a randomized clinical trial with 2-year follow-up. Eur Spine J 22:2022–2029. doi:10.1007/s00586-013-2760-2
Hoy K, Truong K, Andersen T, Bunger C (2016) Addition of TLIF does not improve outcome over standard posterior instrumented fusion. 5–10 years long-term Follow-up: results from a RCT. Eur. Spine. doi:10.1007/s00586-016-4592-3
Ha KY, Na KH, Shin JH, Kim KW (2008) Comparison of posterolateral fusion with and without additional posterior lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Spinal Disord Tech 21:229–234. doi:10.1097/BSD.0b013e3180eaa202
Even JL, Chen AF, Lee JY (2014) Imaging characteristics of “dynamic” versus “static” spondylolisthesis: analysis using magnetic resonance imaging and flexion/extension films. Spine J 14:1965–1969. doi:10.1016/j.spinee.2013.11.057
Schroeder GD, Kepler CK, Kurd MF, Vaccaro AR, Hsu WK, Patel AA, Savage JW (2015) Rationale for the surgical treatment of lumbar degenerative spondylolisthesis. Spine (Phila Pa 1976) 40:E1161–E1166. doi:10.1097/brs.0000000000001116
Harms JG, Jeszenszky D (1998) Die posteriore, lumbale, interkorporelle fusion in unilateraler transforaminaler Technik. Oper Orthop Traumatol 10:90–102. doi:10.1007/s00064-006-0112-7
Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA (2001) Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976) 26:567–571
Yan DL, Pei FX, Li J, Soo CL (2008) Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J 17:1311–1316. doi:10.1007/s00586-008-0739-1
Fujimori T, Le H, Schairer WW, Berven SH, Qamirani E, Hu SS (2015) Does transforaminal lumbar interbody fusion have advantages over posterolateral lumbar fusion for degenerative spondylolisthesis? Global Spine J 5:102–109. doi:10.1055/s-0034-1396432
Kitchen WJ, Mohamed M, Bhojak M, Wilby M (2016) Neurogenic claudication secondary to degenerative spondylolisthesis: Is fusion always necessary? Br J Neurosurg 30:662–665. doi:10.1080/02688697.2016.1206181
Austevoll IM, Gjestad R, Brox JI, Solberg TK, Storheim K, Rekeland F, Hermansen E, Indrekvam K, Hellum C (2017) The effectiveness of decompression alone compared with additional fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a pragmatic comparative non-inferiority observational study from the Norwegian Registry for Spine Surgery. Eur Spine J 26:404–413. doi:10.1007/s00586-016-4683-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to disclose and no outside sources of funding were received for this study. This study was approved by the institutional review board (IRB). The manuscript submitted does not contain information about medical device(s)/drug(s).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, E., Chotai, S., Stonko, D. et al. A retrospective review comparing two-year patient-reported outcomes, costs, and healthcare resource utilization for TLIF vs. PLF for single-level degenerative spondylolisthesis. Eur Spine J 27, 661–669 (2018). https://doi.org/10.1007/s00586-017-5142-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5142-3