Abstract
Purpose
To conduct a meta-analysis to compare the clinical and radiological outcomes in single-level anterior cervical discectomy and fusion (ACDF) surgery for degenerative cervical disease performed by either single-level locking stand-alone cage (LSC) or anterior plate construct (APC).
Methods
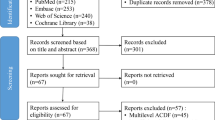
We performed a comprehensive database search of Medline, PubMed, EMBASE and Cochrane Database of Systematic Reviews according to PRISMA guidelines and identified six articles that satisfied our inclusion criteria. We excluded all non-English language articles and articles which did not directly compare LSC and APC. Only papers which focussed on single-level ACDF were included in the study.
Results
There were no significant differences in blood loss, clinical outcomes (JOA, VAS, NDI scores) or radiological outcomes (cervical lordosis, segmental Cobb angle, subsidence and fusion) between the two groups. Operative time was significantly shorter in the LSC group (MD 7.2 min, 95% CI 0.3–14.1, p = 0.04). APC was associated with a statistically significant increase in dysphagia in the follow-up period (OR 6.2, 95% CI 1.0–36.6, p = 0.05).
Conclusion
LSC and APC have similar clinical and radiological outcomes. Further blinded randomised trials are required to establish conclusive evidence in favour of LSC with regards to minimising post-operative dysphagia. We also encourage future studies to make use of formalised dysphagia outcome measures in reporting complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aim of anterior cervical discectomy and fusion (ACDF) in degenerative cervical spine disease is to improve patient symptoms, improve spine stability and restore lordosis, while avoiding complications.
Since the first description of ACDF by Smith and Robinson [1], there have been many advancements in surgical technique, as well as prosthesis options. More recently, there has been a rise in the use of the locking stand-alone cages (LSC), which does not require an anterior plate. LSCs developed with the aim of minimising soft tissue disruption anterior to the vertebrae and reducing the profile of the construct by avoiding an anterior plate [2, 3].
Figures 1 and 2 show examples of the APC and LSC, respectively.
Studies have focussed on the stability profile, outcomes and complications of LSC in contrast to the more traditional anterior plate construct (APC), which have suggested that LSCs have a lower risk of dysphagia as a complication than APCs, while maintaining similar clinical and radiographic outcomes [4–6]. Subsequently, LSCs have increased in popularity. This meta-analysis compares the clinical and radiographic outcomes as well as complication profile of single-level ACDF for degenerative cervical disease between APC and LSC.
Methods
Literature search strategy
Our study was conducted according to the PRISMA guidelines [7, 8]. Electronic databases were searched from the date of inception till 4 July 2016. The databases included Medline, PubMed, EMBASE and Cochrane Database of Systematic Reviews. In order to increase the sensitivity of our search, we combined the terms “zero-profile”, “integrated”, “self-locking”, “anchored”, “stand-alone” and “cervical” as either keywords or MeSH terms. The identified articles, as well as their references, were reviewed according to the selection criteria for consideration of inclusion in the study.
Selection criteria
The systematic review and meta-analysis included studies which adhered to the following inclusion criteria, of studies which: (1) compared patients which had stand-alone locking cages and those which had an anterior plate construct, (2) included patients that only had an operation on one cervical level, (3) included patients who had surgery for symptomatic degenerative spine disease, (4) reported one of the following outcome measures: operative time, blood loss, Visual Analogue Score (VAS), Japanese Orthopaedic Association (JOA) score, Neck Disability Index (NDI) score, fusion rate, subsidence, cervical lordosis, segmental Cobb angle and prevertebral thickness. Our exclusion criteria included patients that had a non-degenerative indication for ACDF such as trauma or tumour, as well as patients that had a multilevel fusion.
We also excluded conference papers, case reports, letters to the editor and abstracts. Only English language articles were included in the study. The LSC defined in the study included only those that had a profile that did not extend anteriorly to the vertebral end plate and a locking mechanism.
Data extraction and critical appraisal
Articles from the literature search were critically reviewed by two authors (MN, KP) with regard to suitability for inclusion in the study, according to the critical review checklist of the Dutch Cochrane Centre proposed by MOOSE [9].
Data were collected from article text, tables and graphs.
Statistical analysis
The odds ratio (OR) was used as a summary statistic. In the present study, both fixed- and random-effects models were tested. In the fixed-effects model, it was assumed that treatment effect in each study was the same, whereas in a random-effects model, it was assumed that there were variations between studies. χ 2 tests were used to study heterogeneity between trials. I 2 statistic was used to estimate the percentage of total variation across studies, owing to heterogeneity rather than chance, with values greater than 50% considered as substantial heterogeneity. I 2 can be calculated as: I 2 = 100% × (Q − df)/Q, with Q defined as Cochrane’s heterogeneity statistics and df defined as degree of freedom. If there was substantial heterogeneity, the possible clinical and methodological reasons for this were explored qualitatively. In the present meta-analysis, the results using the random-effects model were presented to take into account the possible clinical diversity and methodological variation between studies. Specific analyses considering confounding factors were not possible because raw data were not available. All p values were two-sided. Review Manager (version 5.3, Copenhagen, The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used for statistical analysis.
Results
Literature search
Electronic database searches yielded 3665 in PubMed, 2437 in EMBASE and 1940 in Medline. Screening of titles and abstracts yielded 44 articles which were subsequently assessed for suitability for inclusion in the study. Exclusion based on our criteria yielded six studies [4, 10–14] which were subsequently included in our quantitative analysis. Figure 3 shows the PRISMA flowchart for inclusion of articles. Assessment of the quality of articles included in the study according to the MOOSE criteria is described in Table 1. Study characteristics are described in Table 2.
Demographics
Our analysis included a total of 325 patients (158 APC and 167 LSC groups), which included a total of 143 females and 182 males. LSC constructs used in the studies included Zero-P (DePuy Synthes), PEEK Prevail (Medronic Sofamor Danek, Memphis, TN), as well as unspecified stand-alone cages involving a screw locking mechanism. A breakdown of mean ages of patients as well as follow-up times in each study is listed in Table 3.
Operative time
Four studies noted operative time for APC and LSC groups. Figure 4 shows the forest plot analysis for operative time. Mean operative time was greater for the APC group in three studies [10, 13, 14]. Overall, operative time was significantly greater in the APC group compared to the LSC group (MD 7.22 min, 95% CI 0.33–14.11, p = 0.04).
Blood loss
Data regarding blood loss during the operation were reported in four studies. Figure 5 describes this information in a forest plot. The APC group was noted to have a higher mean blood loss in all four studies [10, 12–14]. Overall, the APC group had a higher amount of blood loss compared to the LSC group (MD 16.79, 95% CI −1.77 to 35.36, p = 0.08).
Clinical outcome scores
Mean difference in post-operative JOA scores between APC and LSC groups was reported in one study [13] and was not significant (MD 0.20, 95% CI −1.0 to 0.60, p = 0.63). Post-operative NDI was reported in one study [13] and noted a non-significant mean difference between the two groups (MD 0.30, 95% CI −0.66 to 1.26, p = 0.54). Similarly, post-operative VAS was reported in one study [14], which found a non-significant mean difference between APC and LSC groups (MD 0.80, 95% CI −1.89 to 0.29, p = 0.15).
Radiological outcome
Forest plots detailing analysis of post-operative segmental Cobb angle and cervical lordosis are presented in Figs. 6 and 7, respectively.
Radiographic fusion was reported in four studies, with results varying from 83 to 100% at the final follow-up, and forest plot analysis is presented in Fig. 8. Meta-analysis showed an odds ratio of 0.45 (95% CI 0.10–2.07, p = 0.31) in favour of a LSC construct; however, this was not significant. There was no significant difference between the two groups in post-operative cervical lordosis (MD 1.40 degrees, 95% CI −0.34 to 3.13, p = 0.12) or post-operative segmental Cobb angle (MD 1.20, 95% CI −0.12 to 2.53, p = 0.07).
Complications
Subsidence was reported in three studies [4, 10, 11], with no significant difference noted between the two groups (OR 0.70, 95% CI 0.30–1.67, p = 0.42), and Fig. 9 details the forest plot analysis. None of the articles noted the incidence of preoperative dysphagia. Post-operative dysphagia was noted to be higher in the APC group (OR 1.77, 95% CI 0.74–4.25, p = 0.20). In the follow-up period, the APC group still had a higher incidence of dysphagia (OR 6.17, 95% CI 1.04–36.64, p = 0.05). Post-operative and follow-up dysphagia forest plots are described in Figs. 10 and 11, respectively.
Discussion
The literature includes three recent meta-analyses which compare anterior plate constructs with locking stand-alone cages [15–17]. While these meta-analyses also included patients who underwent multilevel instrumentation, our analysis focuses on patients who only had single-level ACDF.
Surgical measures
Our analysis found that operative time was statistically less in the LSC group, with a mean difference of 7.2 min. Blood loss was also noted to be lower in the LSC group, though the data had high heterogeneity (I 2 = 87%). Dong et al. [17] also found that LSC had a statistically significant shorter operation time and less blood loss. Shao et al. [15] noted no significant difference in operative time, however significant less blood loss LSC group. The decreased surgical time in the LSC group is likely due to the fact that less surgical exposure is required to insert the device. This in turn would contribute to a decreased amount of blood loss, due to less soft tissue structures being involved in dissection and exposure.
Clinical outcomes
All functional outcomes scores (VAS, NDI and JOA) were similar in both LSC and APC groups with no statistically significant difference in scores. This has been noted in previous meta-analyses [16, 17]. Clinical functional outcomes correspond to pain and neurological dysfunction. Both LSC and APC groups require total discectomy, and thus, both procedures would be equivalent in providing cervical decompression of neural structures and restoring intervertebral height. Therefore, it is understandable that both techniques impart a similar functional outcome for patients.
Radiological outcomes
The post-operative segmental Cobb angle was noted to be non-significantly increased in the APC group (MD 1.20°). The post-operative cervical lordosis was also increased in the APC group (MD 1.40), although this was not significant (p = 0.12). The Dong et al. [17] meta-analysis also noted a higher post-operative segmental Cobb in APC (MD −0.98, p < 0.01) and no significant difference in cervical lordosis. A study on interobserver reliability in the measurement of Cobb angle noted a standard deviation of up to 3.2° [18]. The mean differences noted between APC and LSC constructs, therefore, are unlikely to be clinically relevant.
Our analysis did not demonstrate a significant difference in fusion rates between the APC and LSC groups, which was also noted in previous meta-analyses [16, 17]. This finding links to previous biomechanical studies which note the similar ranges of motion and stability profiles in APC and LSC construct types [19–21], which would facilitate a similar degree of motion at the fusion site, and would therefore lead to similar fusion rates.
Complications
The Liu et al. [16] meta-analysis showed a statistically significant difference in subsidence rates, which was higher for LSC (risk difference 0.13, 95% CI 0–0.26). This was largely due to the inclusion of the Shi et al. [22] study, which studies non-contiguous ACDF, and showed a statistically significant higher subsidence rate in LSC patients compared with the APC group. Other studies in the Liu et al. analysis did not demonstrate a statistically significant difference [4, 10]. Our analysis showed no statistically significant difference in subsidence, and this correlates with the similar biomechanical properties of both construct types and similar fusion rates.
Dysphagia is a known complication of ACDF, of which the exact causal mechanism is unknown. Fountas et al. [3] in a review of 1015 patients undergoing ACDF cited an incidence of 9.5%, while Bazaz et al. [23] noted an incidence of 50% at one month after anterior spine surgery. Fountas noted that patients undergoing three-level fusion had a statistically significant higher incidence than those undergoing single- or two-level fusions, suggesting that iatrogenic irritation to soft tissues during surgical exposure is a contributing factor for dysphagia [3]. This is highlighted by the fact that less exposure of the anterior vertebrae is required to insert a LSC. A decreased incidence of dysphagia following instrumentation with small plate profiles [2] implies that plate design may have an effect on soft tissue structures. Previous meta-analyses have noted higher early post-operative and follow-up dysphagia in patients undergoing APC than LSC [15–17]. We also note the subjective nature of describing the symptom of dysphagia, as well as the lack of information regarding the effect that dysphagia has had for a patient. We encourage the use of scoring system for dysphagia in future studies, such as the commonly used Bazaz scoring method [23], which would provide a standardised reporting method for this complication.
Limitations
Our meta-analysis was restricted to the inclusion of only seven articles, which only included one randomised control trial. Furthermore, there were different functional outcome scores used by different articles, which overall resulted in even less articles being used for analysis. This limits the reliability of meta-regression. There was an inherent language bias, where non-English language articles were excluded. While most studies used the Zero-P (DePuy Synthes) prosthesis, there was no uniform homogeneity in prosthesis type or surgical technique. This may have an effect on biomechanical construct stiffness which in turn may influence radiographic and clinical outcomes. We also note the variability in length of follow-up of the studies, which impacts on the reporting of post-operative complications as well as functional outcome scores.
Conclusion
The LSC is equivalent to APC in single-level ACDF with regard to operative time, blood loss, functional outcomes and fusion rates. However, based on the available literature, post-operative dysphagia is noted to be higher in the APC group. Further RCTs are required to confirm our results. We also suggest uniformity in assessing post-operative dysphagia via a structured questionnaire.
References
Smith GW, Robinson RA (1958) The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Jt Surg Am 40A:607–624
Lee MJ, Bazaz R, Furey CG, Yoo J (2005) Influence of anterior cervical plate design on dysphagia: a 2-year prospective longitudinal follow-up study. J Spinal Disord Tech 18:406–409
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, Lee GP, Robinson JS Jr (2007) Anterior cervical discectomy and fusion associated complications. Spine 32:2310–2317
Lee YS, Kim YB, Park SW (2015) Does a zero-profile anchored cage offer additional stabilization as anterior cervical plate? Spine 40:E563–E570. doi:10.1097/brs.0000000000000864
Scholz M, Schleicher P, Pabst S, Kandziora F (2015) A zero-profile anchored spacer in multilevel cervical anterior interbody fusion: biomechanical comparison to established fixation techniques. Spine 40:E375–E380. doi:10.1097/brs.0000000000000768
Hoffstetter CP, Kesavabhotla K, Boockvar JA (2015) Zero-profile anchored spacer reduces rate of dysphagia compared with ACDF with anterior plating. J Spinal Disord Tech 28:E284–E290
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Phan K, Mobbs RJ (2015) Systematic reviews and meta-analyses in spine surgery, neurosurgery and orthopedics: guidelines for the surgeon scientist. J Spine Surg 1:19–27
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Nemoto O, Kitada A, Naitou S, Tachibana A, Ito Y, Fujikawa A (2015) Stand-alone anchored cage versus cage with plating for single-level anterior cervical discectomy and fusion: a prospective, randomized, controlled study with a 2-year follow-up. Eur J Orthop Surg Traumatol 25(Suppl 1):S127–S134. doi:10.1007/s00590-014-1547-4
Shin JS, Oh SH, Cho PG (2014) Surgical outcome of a zero-profile device comparing with stand-alone cage and anterior cervical plate with iliac bone graft in the anterior cervical discectomy and fusion. Korean J Spine 11:169–177. doi:10.14245/kjs.2014.11.3.169
Son DK, Son DW, Kim HS, Sung SK, Lee SW, Song GS (2014) Comparative study of clinical and radiological outcomes of a zero-profile device concerning reduced postoperative dysphagia after single level anterior cervical discectomy and fusion. J Korean Neurosurg Soc 56:103–107. doi:10.3340/jkns.2014.56.2.103
Wang Z, Zhu R, Yang H, Shen M, Wang G, Chen K, Gan M, Li M (2015) Zero-profile implant (Zero-p) versus plate cage Benezech implant (PCB) in the treatment of single-level cervical spondylotic myelopathy. BMC Musculoskelet Disord 16:290. doi:10.1186/s12891-015-0746-4
Tabaraee E, Ahn J, Bohl DD, Collins MJ, Massel DH, Aboushaala K, Singh K (2016) Comparison of surgical outcomes, narcotics utilization, and costs after an anterior cervical discectomy and fusion: stand-alone cage versus anterior plating. Clin Spine Surg. doi:10.1097/bsd.0000000000000341
Shao H, Chen J, Ru B, Yan F, Zhang J, Xu S, Huang Y (2015) Zero-profile implant versus conventional cage-plate implant in anterior cervical discectomy and fusion for the treatment of degenerative cervical spondylosis: a meta-analysis. J Orthop Surg Res 10:148. doi:10.1186/s13018-015-0290-9
Liu W, Hu L, Wang J, Liu M, Wang X (2015) Comparison of zero-profile anchored spacer versus plate-cage construct in treatment of cervical spondylosis with regard to clinical outcomes and incidence of major complications: a meta-analysis. Ther Clin Risk Manag 11:1437–1447. doi:10.2147/tcrm.s92511
Dong J, Lu M, Lu T, Liang B, Xu J, Zhou J, Lv H, Qin J, Cai X, Huang S, Li H, Wang D, He X (2015) Meta-analysis comparing zero-profile spacer and anterior plate in anterior cervical fusion. PLoS One 10:e0130223
Pruijs JE, Hageman MA, Keessen W, van der Meer R, van Wieringen JC (1994) Variation in Cobb angle measurements in scoliosis. Skelet Radiol 23:517–520
Scholz M, Reyes PM, Schleicher P, Sawa AG, Baek S, Kandziora F, Marciano FF, Crawford NR (2009) A new stand-alone cervical anterior interbody fusion device: biomechanical comparison with established anterior cervical fixation devices. Spine 34:156–160
Nayak AN, Stein MI, James CR, Gaskins 3rd RB, Cabezas AF, Adu-Lartey M, Castellvi AE, Santoni BG (2014) Biomechanical analysis of an interbody cage with three integrated cancellous lag screws in a two-level cervical spine fusion construct: an in vitro study. Spine J 14:3002–3010
Paik H, Kang DG, Lehman RA Jr, Cardoso MJ, Gaume RE, Ambati DV, Dmitriev AE (2014) Do stand-alone interbody spacers with integrated screws provide adequate segmental stability for multilevel cervical arthrodesis? Spine J 14:1740–1747
Shi S, Liu ZD, Li XF, Qian L, Zhong GB, Chen FJ (2015) Comparison of plate-cage construct and stand-alone anchored spacer in the surgical treatment of three-level cervical spondylotic myelopathy: a preliminary clinical study. Spine J 15:1973–1980. doi:10.1016/j.spinee.2015.04.024
Bazaz R, Lee MJ, Yoo JU (2002) Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine 27:2453–2458
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There was no funding for this research.
Rights and permissions
About this article
Cite this article
Nambiar, M., Phan, K., Cunningham, J.E. et al. Locking stand-alone cages versus anterior plate constructs in single-level fusion for degenerative cervical disease: a systematic review and meta-analysis. Eur Spine J 26, 2258–2266 (2017). https://doi.org/10.1007/s00586-017-5015-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-017-5015-9