Abstract
Purpose
Surgery for lumbar disc herniation (LDH) is most often elective, but intense pain may require more urgent, non-elective, treatment. It was hypothesized that non-elective treatment could be associated with a less favourable outcome than elective surgery. The aim of this study was to compare 1–2-year outcome after non-elective and elective surgery for treatment of para-median LDH using data from the Swedish Spine register (SweSpine).
Methods
Pre- and postoperative data were available for 301 non-elective and 2364 elective cases. Patient reported outcome measures (PROMs) were; Visual Analogue Scale (VAS) leg and back pain, Oswestry Disability Index (ODI), EuroQol five-Dimensions (EQ-5D) and patient satisfaction. Postoperative p values were adjusted for baseline differences.
Results
Preoperative mean (SD) in the non-elective and elective groups were for VAS leg pain 81 (22) and 65 (24), for VAS back pain 51 (33) and 45 (28), for ODI 66 (20) and 45 (17) and for EQ-5D 0.024 (0.35) and 0.31 (0.33), respectively, (p for all <0.001). Postoperative VAS leg pain was 23 (28) in the non-elective group and 20 (26) in the elective group (p = 0.19). Corresponding figures were for VAS back pain 25 (27) and 24 (27) (p = 0.69), ODI 19 (17) and 17 (17) (p = 0.052) and for EQ-5D 0.70 (0.28) and 0.73 (0.29) (p = 0.73). Patient satisfaction did not differ between the groups (p = 0.78).
Conclusions
Even if non-elective patients preoperatively had substantially more pain, higher disability and poorer quality of life than elective patients, postoperative differences were clinically small. Patient satisfaction did not differ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery for lumbar disc herniation (LDH) is the second most common spinal surgical procedure in Sweden, with a mean yearly incidence rate of 20–24 per 100,000 inhabitants [1–3]. The majority of these operations are elective procedures, but some are made non-electively, or acute, i.e. non-planned cases with severe symptoms, mostly admitted through the emergency department. Indications for surgery are persistent, severe leg pain, acute or progressive paresis or ‘cauda equina syndrome’ [4].
Waiting times for surgery varies [5]. Patients with severe pain, disability and neurological impact, eventually causing bed confinement, may not be able to wait for elective treatment and therefore require more urgent surgery. It was hypothesized that non-elective patients would have a less favourable outcome and be at risk for more complications in comparison to elective patients.
Hence, the aim here is to examine possible differences in outcome between the two groups after surgery for para-median lumbar disc herniation.
Materials and methods
This study is based on data from the SweSpine register [6]. The register was introduced in 1993 to obtain prospective data on outcome following spine surgery in Sweden and has since the start continually been developed. The SweSpine register is currently in use at 44 of 47 clinics performing spine surgery in Sweden [3]. The register consists of two parts, one filled in by the patient and one by the surgeon. The surgeon registers diagnosis, type of surgical procedure, length of hospitalization and any complications occurring during the in-patient stay. Since 2007 the surgeon indicates whether the patient was treated non-electively or as a planned, elective surgical procedure. In this study, patients treated through March 2011, were included.
Criteria for inclusion and exclusion
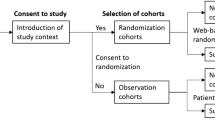
Criteria for inclusion were; first time back surgery, unilateral, para-median LDH, mono-segmental surgery and disc extirpation as the only surgical procedure. As patients with ‘cauda equina syndrome’ represent a group with a poorer outcome and are only treated with urgency (non-electively) [7], we strived to exclude those from the study. In the SweSpine registry there is no specific option for ‘cauda equina syndrome’ diagnosis. To address this question, patients with bilateral, or central LDH, were excluded [8]. In addition, in case ‘cauda equina syndrome’ had been noted as a text comment by the surgeon, the patient was excluded. Individuals with LDH on more than one level were also excluded, thought to have a less clear indication of surgery, and possibly a less favourable prognosis. For a flow chart of the study, see Fig. 1.
Outcomes
Following the recommendations of, amongst others, McCormick et al. [9] and the SweSpine registration concept, patient reported outcome measures (PROMs) were used. The primary four outcomes were; leg pain and back pain, measured by a 100 mm visual analogue scale (VAS) [10]; the Oswestry disability index (ODI), a questionnaire for rating back pain and function [11, 12] giving a score from 1 (best) to 100 (worst); EuroQol five-dimensions (EQ-5D), a form measuring quality of life in which an index between −0.59 (worst) and 1.00 (best) is possible, and represents the societal perspective on health. Swedish reference values have not been developed and the UK reference values are used in place [13].
As secondary outcome a question on patient’s satisfaction is used to evaluate the clinical importance of primary outcome. This question is formulated as follows: ‘Are you satisfied with the result of the surgery?’ and the three alternative answers were dichotomized into ‘satisfied’, versus ‘uncertain’ and ‘dissatisfied’.
Other patient reported data
The patient preoperatively reports data on anthropometrics, gender, duration of leg and back pain, smoking, and the prevalence of any co-morbidities heavily restricting the quality of life, such as heart disease, neurological disease, cancer and other disease affecting walking ability or causing pain.
Use of follow-up data
Primarily, PROMs from the 2-year follow-up were used in this study. If these were missing, 1-year PROMs were used instead as the results have been reported to be similar [6]. From the final study cohort of 2665 patients, 2-year follow-up data were collected for 2106 patients and 1-year data for 559 patients.
Complications
Any complications occurring during the in-patient stay are reported by the surgeon. At the 1-year follow-up the patients are also asked whether any complications occurred after surgery. The incidence of dural tears, root lesions, surgical site infections and thromboembolic incidents reported by the surgeon or patient in the two groups were compared. Reoperation on the same spinal segment and side for recurrent LDH, was noted by the surgeon and the number of patients with reoperations within 2 years after primary surgery was calculated.
Statistics
Descriptive data are presented as mean (SD) or number (%). The Chi-square test is used for comparison of categorical variables. Continuous variables are compared with the Student’s t test, Wilcoxon’s test for paired differences and in case of adjustment for co-variables, analysis of covariance (ANCOVA). Adjustments were made for BMI, the prevalence of any co-morbidity (‘yes’ or ‘no’), duration of preoperative leg pain and back pain (‘no pain’ or ‘<3 months’ vs ‘3 months or more’), as these co-variables showed significant differences at baseline between the two groups. In the analyses of postoperative VAS leg pain, VAS back pain, ODI and EQ-5D, adjustments were also made for the baseline level of the dependent variable. A p value of <0.05 was considered significant. SPSS version 22 was used for the statistical analysis.
Ethical approval
Ethical approval was obtained from the regional ethics board in Stockholm (number 2012/206-31/1).
Results
Baseline characteristics for the non-elective and elective groups are shown in Table 1. The non-elective group had a higher prevalence of serious co-morbidities and a shorter duration of leg and back pain than the elective group. The mean age was the same and the proportion of women and smokers did not differ between the groups. The non-elective patients spent more days in hospital before, as well as after surgery (Table 1). The co-variables correlated to a less successful outcome, in order of importance; preoperative high back pain, co-morbidity, duration of back pain, smoking, gender, preoperative high leg pain, BMI and duration of leg pain (data not shown).
Before surgery the non-elective group had higher mean VAS leg pain, VAS back pain, ODI-score and lower EQ-5D-index than the elective group, all clinically significant differences, except for VAS back pain (Table 2).
The elective and non-elective groups improved significantly in all outcome variables after surgery, both statistically (all p < 0.001) and clinically. The non-elective group improved significantly more (all p < 0.001), than did the elective group and the groups reached almost the same clinical results at follow-up (Table 2). The only statistically significant difference in the unadjusted analysis was seen for EQ-5D, which was lower in the non-elective group. In the initially adjusted analysis VAS leg pain, ODI and EQ-5D was significantly lower in the non-elective group, but these differences diminished and became non-significant after adjustment with the baseline level of the dependent variable. When adjusting, the changes of the scoring units were small without any clinical significance (data not shown). Among the patients answering the question on satisfaction, those satisfied after surgery were 236 out of 294 (80 %) in the non-elective group and 1822 out of 2320 (79 %) in the elective group (adjusted p = 0.78).
The frequency of dural tears, nerve root lesions, surgical site infections and thromboembolic incidents did not differ between the groups (Table 3). Reoperations for recurrent LDH were more frequent in the non-elective group (Table 3; adjusted p = 0.032).
Non-response analysis
The 566 non-responders without PROMs at follow-up were compared to the final study cohort of 2665 responders. The proportion of non-elective and elective patients did not differ between the groups (p = 0.90). The non-responders were in comparison with the responders in mean 3.9-year younger (p < 0.001), had a 0.4 kg/m2 lower mean BMI (p = 0.044), were smokers to a larger extent (26 vs 17 %; p < 0.001) and had more often back and leg pain of a duration longer than 3-month preoperatively (85 vs 80 %; p = 0.015 and 86 and 81 %; p = 0.039, respectively). The proportion of women did not differ significantly between the groups, nor did co-morbidities. Dividing the non-responders and responders into non-elective and elective subgroups, weakened, but did not change these significances substantially (data not shown).
Discussion
Not unexpectedly, the non-elective group had significantly more severe pain, dysfunction and lower quality of life, but shorter duration of pain, longer hospitalization pre- and postoperatively and a higher frequency of operations for recurrent LDH, than the elective group. These preoperative differences were in general notable, but the improvement (effect of treatment) after surgery was also clearly more notable in the non-elective group, resulting in an outcome 1–2 years after surgery without significant clinical differences. In addition the patient satisfaction with the surgery was identical in the two groups.
Non-elective patients had a shorter duration of both leg and back pain preoperatively. This may reflect the often more pronounced onset and higher degree of suffering and disability in this group, not possible to endure for an extended period of time. The longer duration of hospitalization for these patients, both pre- and postoperative, supports this assumption. A longer preoperative duration of pain has been reported to predict poorer outcome in several studies [14, 15]. In the current study duration of pain, particularly back pain, correlated to a less successful outcome. Even so, the elective group did not have a poorer outcome than did the non-elective, despite the longer duration of preoperative leg and back pain. This may be an effect of other compensating co-variables, i.e. initial level of pain, which was clearly higher in the non-elective group.
High preoperative level of pain has in a systematic review of eleven studies been reported to be a negative predictor of outcome [16]. Back or leg pain was not described specifically in this study. In the ‘SPORT’ study, a high level of initial back pain predicts less successful surgical outcomes, but also predicts higher reduction of pain in absolute figures (effect of treatment), than for patients with lower initial back pain [17], findings supported by our study.
As randomization is not possible in a study like this, adjustment of the groups, to lessen systematic bias, is of fundamental interest. How to adjust may be discussed at length, but is usually carried out by identifying important baseline variables that are not equal in the different study groups and adjust for these. In the current study both the unadjusted and the adjusted analyses of the postoperative PROM:s showed small or non-significant differences between the two groups, especially when also adjusting for baseline levels of the PROM:s (the model we recommend), indicating a remarkable potential of improvement in the non-elective group.
Obesity has a negative impact on outcome and complications following lumbar surgery for spinal stenosis as well as other surgical methods for the degenerative back, including disc herniation [18, 19]. The non-elective group in this study had a slightly higher mean BMI, but inclusion of BMI alone or in the multi-adjusted model made no significant difference to the outcome, nor did the variable co-morbidity (data not shown).
Complications are an important factor when interpreting the outcome after surgery and may be underreported or misinterpreted, i.e. failure of improvement is often reported as a complication. Four important complications are reported, self-assessed and/or surgeon reported data, which we believe can be reliably interpreted by the patient and/or surgeon. There is no reason to assume that there was a systematic bias in the reporting of complications between the groups. The rates were equal in both groups.
The reported rate of reoperations for recurrent LDH in other studies varies widely, mainly due to differences in definitions of reoperations and the time of reporting, but is predominantly between 5 and 10 % at 1 year [20–22]. Our study supports these figures, with 8 and 4 % (non-elective/elective, adj. p = 0.012), respectively, within a 2-year period after surgery. We report only ‘true’ (=same side and level) reoperations for recurrent LDH. Combined or other procedures including the primary operated level are always difficult to delimit from other indications for surgery. The higher rate of LDH among the non-elective patients may be explained by various factors. The literature has highlighted several risk factors; male gender, younger age and primary extrusions/protrusions [23, 24]. No such significance was found among these variables in this study. The type of herniation is not noted in the SweSpine register and cannot be assessed, but may be one explanation. Nor did we find any significant differences in time of occurrence for the reoperation between non-elective (mean 9.8 months) and elective patients (mean 9.3 months).
The non-elective group had marginally less favourable values at follow-up, statistically borderline significant or insignificant, depending on model of adjustment. However, the distinction between statistical and clinical significance must be considered. The differences between the non-elective and the elective groups are far smaller than what can be regarded as clinically relevant. Recommended minimal clinical important differences (MCID) are discussed extensively, but proposed approximate values are 15–20 for VAS pain, 10–12 for ODI [25, 26] and 0.17–0.30 for EQ-5D [27, 28].
The statistical methods can be argued and the use of parametric methods, though the outcome variables must basically be regarded as non-parametric, may be questioned. In alternative analyses the outcome data were dichotomized and logistic regression was used. The results were essentially identical. Dichotomization leads to unnecessary loss of statistical power and the here used methods were favoured. The number of patients in the groups is also rather substantial, minimizing unwanted effects of parametric methods. Even more complex statistics, like longitudinal mixed model regression and similar methods, could have been used, but as it would not have affected the outcome essentially we opted for simpler statistics.
There are some limitations. The SweSpine register does not specifically define non-elective and elective surgery and registration in SweSpine is at the discretion of the surgeon. However, in our opinion, the general interpretation of this question is very conform in Sweden, supported by the findings of longer hospitalization both pre- and postoperative and higher level of pain in the non-elective group, indicating that these were non-planned admissions.
The fact that follow-up is a mix of 1 and 2-year results may also be regarded as a limitation. At the 1-year follow-up, the response rate was 76 % and a comparison with the 2-year results showed almost equal data (not shown). Further, a Norwegian spine register study showed no significant difference between responders (78 %) and non-responders at 2-year follow-up for lumbar spine degenerative disorders [29], indicating that our results may well be representative of the whole group. Even though the follow-up rate was 82 % in this study, our analysis of non-responders showed preoperative differences in age, smoking status and pain duration preoperatively and it cannot be ruled out that this causes a slight bias.
We attempted to exclude patients with ‘cauda equina syndrome’, but it cannot be assured there were no such patients unintentionally included. If such patients have been included, these are very few and unlikely to substantially affect the outcome data and the interpretation of the study.
As for all registry studies, one limitation is the potential for unmeasured confounding. In this study adjustments have been made for commonly known baseline confounders, showing significant differences between the groups. These adjustments did not change the outcome substantially.
What is the reason initially such different groups may show this similar results at follow-up? Even the unadjusted analyses show nearly similar results (Table 2) as the adjusted analyses. It appears to reflect a true improvement in both groups, but greater in the non-elective, despite that higher pain level preoperatively, more co-morbidity and a marginally higher BMI, would indicate the opposite. One hypothesis may be that this reflects a high potential of recovery of the nerve fibres, even after severe mechanical impact and pain, provided there is no serious damage to the fibres [30–32].
Conclusion
Despite initially considerably higher levels of pain, disability, lower quality of life and postoperatively a higher rate of reoperations, the non-elective patients showed the same clinical outcome and satisfaction with the procedure at follow-up, as did the elective. There are likely to be many causes for this remarkable outcome, some may be found in neurophysiological healing mechanisms.
References
Jansson KA, Nemeth G, Granath F, Blomqvist P (2004) Surgery for herniation of a lumbar disc in Sweden between 1987 and 1999. An analysis of 27,576 operations. J Bone Joint Surg Br 86(6):841–847
Spangfort EV (1972) The lumbar disc herniation. A computer-aided analysis of 2504 operations. Acta Orthop Scand Suppl 142:1–95
Strömqvist BFP, Hägg O, Knutsson B, Sandén B (2014) Swespine, the Swedish spine register 2014 report. Available via The Swedish Spine Surgeon’s Society. Accessed 30 sept 2014
Weber H (1994) The natural history of disc herniation and the influence of intervention. Spine (Phila Pa 1976) 19(19):2234–2238 (discussion 2233)
Hurlbert RJ, Mobbs R, Teo C (2008) Access to spine care: a tale of two cities. Can J Neurol Sci 35(3):308–313
Stromqvist B, Fritzell P, Hagg O, Jonsson B, Sanden B, Swedish Society of Spinal S (2013) Swespine: the Swedish spine register : the 2012 report. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 22(4):953–974. doi:10.1007/s00586-013-2758-9
Chau AM, Xu LL, Pelzer NR, Gragnaniello C (2014) Timing of surgical intervention in cauda equina syndrome: a systematic critical review. World Neurosurg 81(3–4):640–650. doi:10.1016/j.wneu.2013.11.007
Gardner A, Gardner E, Morley T (2011) Cauda equina syndrome: a review of the current clinical and medico-legal position. Eur Spine J 20(5):690–697. doi:10.1007/s00586-010-1668-3
McCormick JD, Werner BC, Shimer AL (2013) Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg 21(2):99–107
Zanoli G, Stromqvist B, Jonsson B (2001) Visual analog scales for interpretation of back and leg pain intensity in patients operated for degenerative lumbar spine disorders. Spine (Phila Pa 1976) 26(21):2375–2380
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66(8):271–273
Fairbank JC, Pynsent PB (2000) The Oswestry disability index (Phila Pa 1976). Spine 25(22):2940–2952 (discussion 2952)
Burstrom K, Johannesson M, Diderichsen F (2001) Health-related quality of life by disease and socio-economic group in the general population in Sweden. Health Policy 55(1):51–69
Quon JA, Sobolev BG, Levy AR, Fisher CG, Bishop PB, Kopec JA, Dvorak MF, Schechter MT (2013) The effect of waiting time on pain intensity after elective surgical lumbar discectomy. Spine J Off J N Am Spine Soc 13(12):1736–1748. doi:10.1016/j.spinee.2013.05.038
Junge A, Dvorak J, Ahrens S (1995) Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine 20(4):460–468
den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW (2006) A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J 15(5):527–536. doi:10.1007/s00586-005-0910-x
Kerr D, Zhao W, Lurie JD (2015) What are long-term predictors of outcomes for lumbar disc herniation? A randomized and observational study. Clin Orthop Relat Res 473(6):1920–1930. doi:10.1007/s11999-014-3803-7
Knutsson B, Michaelsson K, Sanden B (2013) Obesity is associated with inferior results after surgery for lumbar spinal stenosis: a study of 2633 patients from the Swedish spine register. Spine (Phila Pa 1976) 38(5):435–441. doi:10.1097/BRS.0b013e318270b243
Buerba RA, Fu MC, Gruskay JA, Long WD 3rd, Grauer JN (2014) Obese class III patients at significantly greater risk of multiple complications after lumbar surgery: an analysis of 10,387 patients in the ACS NSQIP database. Spine J 14(9):2008–2018. doi:10.1016/j.spinee.2013.11.047
Golinvaux NS, Bohl DD, Basques BA, Yacob A, Grauer JN (2014) Comparison of the lumbar disc herniation patients randomized in SPORT to 6846 discectomy patients from NSQIP: demographics, perioperative variables, and complications correlate well. Spine J. doi:10.1016/j.spinee.2014.12.008
Ambrossi GL, McGirt MJ, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Long DM (2009) Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery 65(3):574–578. doi:10.1227/01.NEU.0000350224.36213.F9 (discussion 578)
Kim CH, Chung CK, Park CS, Choi B, Kim MJ, Park BJ (2013) Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nationwide cohort study. Spine (Phila Pa 1976) 38(7):581–590. doi:10.1097/BRS.0b013e318274f9a7
Suk KS, Lee HM, Moon SH, Kim NH (2001) Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976) 26(6):672–676
Aizawa T, Ozawa H, Kusakabe T, Nakamura T, Sekiguchi A, Takahashi A, Sasaji T, Tokunaga S, Chiba T, Morozumi N, Koizumi Y, Itoi E (2012) Reoperation for recurrent lumbar disc herniation: a study over a 20-year period in a Japanese population. J Orthop Sci 17(2):107–113. doi:10.1007/s00776-011-0184-6
Hagg O, Fritzell P, Nordwall A (2003) The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J 12(1):12–20 (discussion 21)
Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, Bouter LM, de Vet HC (2008) Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976) 33(1):90–94
Johnsen LG, Hellum C, Nygaard OP, Storheim K, Brox JI, Rossvoll I, Leivseth G, Grotle M (2013) Comparison of the SF6D, the EQ5D, and the oswestry disability index in patients with chronic low back pain and degenerative disc disease. BMC Musculoskelet Disord 14:148
Solberg T, Johnsen LG, Nygaard OP, Grotle M (2013) Can we define success criteria for lumbar disc surgery?: estimates for a substantial amount of improvement in core outcome measures. Acta Orthop 84(2):196–201. doi:10.3109/17453674.2013.786634
Solberg TK, Sorlie A, Sjaavik K, Nygaard OP, Ingebrigtsen T (2011) Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop 82(1):56–63. doi:10.3109/17453674.2010.548024
Abuduhadeer T (2004) Neuropathic pain intensity depends on the degree of peripheral nerve injury in the rat. J Nippon Med Sch 71(6):399–407
Huang C, Zou W, Lee K, Wang E, Zhu X, Guo Q (2012) Different symptoms of neuropathic pain can be induced by different degrees of compressive force on the C7 dorsal root of rats. Spine J 12(12):1154–1160
Chiang CY, Sheu ML, Cheng FC, Chen CJ, Su HL, Sheehan J, Pan HC (2014) Comprehensive analysis of neurobehavior associated with histomorphological alterations in a chronic constrictive nerve injury model through use of the CatWalk XT system. J Neurosurg 120(1):250–262. doi:10.3171/2013.9.JNS13353
Acknowledgments
The authors would like to acknowledge all the participating patients and surgeons in SweSpine, and Carina Blom at the SweSpine register for the help with data retrieval.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was financially supported by funds from the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet and the Karolinska Institutet research funds.
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Elkan, P., Sjövie Hasserius, J. & Gerdhem, P. Similar result after non-elective and elective surgery for lumbar disc herniation: an observational study based on the SweSpine register. Eur Spine J 25, 1460–1466 (2016). https://doi.org/10.1007/s00586-016-4419-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-016-4419-2