Abstract
Purpose
The cortical bone trajectory (CBT) is a novel lumbar pedicle screw trajectory. The aim of this study was to conduct a detailed morphometric measurement of the lumbosacral spine for CBT pedicle screw, using the inferior facet of the cephalad level as a bony landmark.
Methods
The three-dimensional computed tomography (3D-CT) scans of 86 adults who underwent examination of the lumbosacral spine were studied. The distances from the starting point to the inferior, lateral and medial border of the inferior facet of the cephalad level were measured. The angles formed between the screw trajectory and the sagittal plane, the superior endplate of the vertebral body and the posterior margin of the pars interarticularis were defined as the transverse angle (TA), cephalad angle 1 (CA1) and cephalad angle 2 (CA2), respectively.
Results
The distances from the inferior border of inferior facet to the starting point from L1 to S1 were 8.9, 6.3, 4.1, 2.9, 1.4 and 0 mm, respectively. The distances from the medial border of the inferior facet to the starting point from L1 to S1 were between 3 and 4 mm. TA from L1 to S1 was 9.0°, 9.6°, 11.3°, 13.5°, 15.5°, and 8.2°, respectively. CA1/CA2 from L1 to S1 was 26.7°/38.7°, 26.0°/38.7°, 26.9°/38.0°, 24.4°/37.2°, 22.9°/35.1° and 18.4°/47.8°, respectively. The maximum screw diameters from L1 to S1 were 4.8, 5.1, 6.1, 6.8, 7.8, and 6.1 mm, respectively. Twenty-five millimeter can serve as a safe maximum length of CBT pedicle screws.
Conclusions
The inferior facet of the cephalad level is an attractive bony landmark for establishing a starting point of CBT for minimally invasive spine surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of pedicle screws to achieve solid fixation has become increasingly common in instrumented lumbar spine fusion. The traditional method of pedicle screw insertion involves a transpedicular approach, which relies on screw engagement with cancellous bone in the pedicle and vertebral body. This method of pedicle screw fixation can become problematic especially in osteoporotic and elderly patients who are at a high risk for complications such as instrumentation failure [1, 2]. Various modifications to pedicle screw design and insertion techniques have been designed to address issues related to fixation strength [3–6].
In 2009, Santoni et al. introduced a novel method of pedicle screw insertion termed cortical bone trajectory (CBT) [7]. This new trajectory follows a caudocephalad path sagittally and a laterally directed path in the transverse plane, which increases cortical bone contact in the pedicle and vertebral body, compared to the traditional method. Biomechanical studies have demonstrated that the CBT technique achieves screw purchase and strength equivalent to or greater than the traditional method [7, 8].
There is a dearth of literature on CBT screw insertion techniques. Specifically, there is a limited amount of information on bony landmarks to establish a starting point for pedicle screw insertion or information on screw size and trajectory. The goal of this study was to conduct a detailed computed tomography (CT) scan-based assessment of cortical bone trajectory pedicle screw starting point, trajectory and screw diameter of lumbosacral spine segments.
Materials and methods
Between January 2014 and May 2014, all consecutive patients who had a CT scan of the chest, abdomen, pelvis and spine as part of an institutional protocol after a high-energy traumatic event were included in the study. Patients were excluded if they had a spine fracture, history of spine surgery, infection, tumor, deformity, or obvious hyperostosis of facet joint. 86 adults met the inclusion criteria. CT images were analyzed using three-dimensional reconstruction software (Centricity Enterprise Web Version 3.0; GE Healthcare, Barrington, Illinois). An institutional review board approval was obtained for this study.
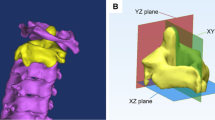
The junction of the inferior and medial border of the isthmic portion (smallest section) of the lumbar pedicle in the coronal plane was traced (Fig. 1) in the lumbar segments while the junction of the medial border of the sacral 1 (S1) pedicle and the inferior border of the L5 inferior facet was traced in the S1 segment. The starting point was defined to be the projective point on the vertebrae by this junction. The starting point is identified in Fig. 2 as SP. The distances from the starting point to the inferior, lateral and medial border of the inferior facet of the cephalad level were defined as DIAP, DLAP and DMAP, respectively (Fig. 2). The position of the starting point relative to inferior articular process at each level was calculated as a percentage using the formula: DMAP percentage = DMAP/(DMAP + DLAP) × 100 %. Measurements were also made for the distance from the starting point to the inferior border of the transverse process at all levels except S1 (DITP, Fig. 2).
Measurement of the location of the starting point. SP indicates the starting point (white circle), DITP the distance from the starting point to the inferior border of the transverse process, DIAP the distances from the starting point to inferior border of the inferior articular process at the upper level (black double-headed arrows), DMAP the distances from the starting point to the medial border of the inferior articular process at the upper level (black double-headed arrows), DLAP the distances from the starting point to the lateral border of the inferior articular process at the upper level (black double-headed arrows)
The trajectory of pedicle screws for the lumbar and S1 segments was determined in the axial and sagittal planes (Fig. 3). A line was drawn from starting point, aimed to the midpoint of the pedicle and abutting the lateral cortex of the vertebral body on the axial CT scan (white thick line, Fig. 3). The angle formed between this trajectory and the sagittal plane was defined as the transverse angle (TA) (Fig. 3). On the sagittal CT scan, a line was drawn from the starting point aimed to the midpoint of the pedicle and abutting the cortex of the superior endplate of the vertebral body. The angle formed between this trajectory and the superior endplate of the vertebral body was defined as the cephalad angle 1 (CA1, Fig. 3). Cephalad angle 2 (CA2, Fig. 3) was defined as the angle formed between the same trajectory on the sagittal plane and the posterior margin of the pars interarticularis. The maximum pedicle screw diameter and length of the lumbosacral segments were also measured on axial and sagittal CT scans (SD, TD, SL, TL, Fig. 3).
Measurement of the diameter, length, and directions of the CBT. Upper views the lumbar segments, and lower views the S-1 level. SD the maximum sagittal diameter (black double-headed arrows), TD the maximum transverse diameter (black double-headed arrows), SL the maximum sagittal length (white thick line), TL the maximum transverse length (white thick line), TA transverse angle was formed between the trajectory and the sagittal plane, CA1 cephalad angle 1 was formed between the trajectory and the superior endplate of the vertebral body in the sagittal plane, CA2 cephalad angle 2 was formed between the trajectory and the posterior margin of the vertebral plate in the sagittal plane
Results are presented as mean ± standard deviation (SD). One-way analysis of variance and the Tukey analysis were performed for statistical comparison, and significance was defined as p < 0.05. All statistical analyses were performed with SPSS (version 19, SPSS Statistics for Windows, Armonk, New York).
Results
Demographic data
Eighty-six adults, 48 males and 38 females, with a mean age of 59 years old (range 20–91) were evaluated (Table 1).
Starting point
The distances from the starting point to the inferior, lateral and medial border of the inferior articular process of the cephalad level are presented in Table 2. There was a statistically significant gradual decrease in the DIAP caudally from L1 to L5 in all pairs (p < 0.05). There was a statistically significant gradual increase in the DLAP caudally from L1 to S1. This difference was statistically significant in all pairs except L1 versus L2 (p = 0.56). The DMAP from L1 to S1 was between approximately 3–4 mm (the maximum was 4.1 ± 1.5 mm in L5, and the minimum was 3.2 ± 1.3 mm in S1). The DMAP percentages from L1 to S1 were 80.5 ± 36.5, 70.1 ± 31.2, 61.6 ± 22.7, 48.6 ± 17.9, 40.8 ± 16.0 and 29.3 ± 14.6 %, respectively. There was a tendency for a gradual decrease in DMAP percentages caudally from L1 to S1, which was statistically significant in all pairs except L1 versus L2, L2 versus L3 and L4 versus L5. When comparing patients of different age groups (<60 and ≥60 years of age), there were statistically significant differences in the DIAP from L2 to L5 (p < 0.05). However, no statistically significant differences were found in the DLAP, DMAP or the DMAP percentages between the age groups. The distances from the starting point to the inferior border of the transverse process from L1 to L5 were 1.1 ± 1.0, 1.4 ± 1.1, 1.7 ± 1.5, 1.4 ± 1.4, and 1.3 ± 1.4 mm, respectively. There was no statistically significant difference between all pairs except L1 versus L3 (p = 0.01).
Screw trajectory
From the starting point, the trajectory of the TA, CA1 and CA2 from L1 to S1 are presented in Table 3. The CA1 of lumbar segments was higher than those observed in S1 (lumbar segments; 22°–26°, S1; 18°, p < 0.05). Conversely, the CA2 of lumbar segments was lower than those observed in the S1 (lumbar segments; 35°–38°, S1; 47°, p < 0.05). The TA of lumbar segments was between 9° and 15°. There was a tendency for a gradual increase in the TA caudally from L1 to L5.
Screw diameter and length
The maximum screw diameter and length in the sagittal and transverse plane from L1 to S1 are presented in Table 3. There was no significant difference between all pairs in the maximum screw length in axial plane. However, the maximum screw length in the sagittal plane was longer in S1 compared to all lumbar segments (p < 0.05). The maximum screw diameter in the axial plane was much smaller than in the sagittal plane in each segment from L1 to S1, except for L5. The maximum screw diameter in the axial plane from L1 to S1 was 4.8, 5.1, 6.1, 6.8, 8.0, and 6.1 mm, respectively. There was a tendency for maximum screw diameter in the axial plane to gradually increase caudally from L1 to L5.
Discussion
CBT is a relatively new pedicle screw fixation technique. It was designed as a means of enhancing fixation strength at the pedicle screw–bone interface. The starting point is on the lateral aspect of the pars interarticularis and its trajectory follows a caudocephalad path sagittally and a laterally directed path in the transverse plane. This trajectory maximizes screw contact with dense cortical bone in the pedicle and vertebral body. Biomechanical studies have demonstrated that CBT screws have a 30 % increase in uniaxial yield pullout load relative to traditional pedicle screw trajectory [7]. Insertional torque, which has been correlated with screw stability, is noted to be 1.7 times higher in CBT compared to the traditional technique in in vivo analysis [9]. As a result, CBT pedicle screw technique is a valuable tool to maximize fixation strength in elderly or osteoporotic patients.
In this study, we conducted a detailed CT scan-based assessment of lumbosacral CBT pedicle screw starting point, trajectory, length and diameter. The inferior facet was used as a bony landmark for establishing a starting point on the pars interarticularis. This relatively medial starting point, compared to the traditional pedicle screw technique, obviates the need for tissue dissection and muscle disruption, which produces less tissue trauma and may decrease recovery time. In the sagittal plate, there was a tendency for the distance from the starting point to the inferior border of the inferior facet to decrease with cephalad to caudal progression (8.9 mm in L1 compared to 0 mm in S1). In the transverse plane, the distances from the starting point to the medial border of the inferior facet for all segments were between 3 and 4 mm. The value of 3–4 mm could be used as an important reference during surgery. When comparing patients of different age groups (<60 and ≥60 years of age), statistically significant differences were noted in the DIAP from L2 to L5. However, no statistically significant differences were found in the DLAP, DMAP or the DMAP percentages between the age groups. These findings are likely due to the decrease in the height of degenerated discs in the older age group, rather than to the degree of facet hyperostosis. In the lumbar segments, there was a tendency for the lateral-directed trajectory angles to increase with cephalad to caudal progression. However, the cephalad-directed trajectory angle ranges were relatively similar for all lumbar segments, which were 22°–26° and 35°–38° for CA1 and CA2, respectively. CA1 and CA2 are both viable options to use as a screw trajectory guide with the caveat that CA1 requires fluoroscopic imaging to visualize the superior endplate of the vertebral body. Since the starting point is on the lamina, CA2 may be more convenient to use than CA1 during surgery. Our measurements also demonstrated that the screw diameter seem to depend on the pedicle width, which was smaller than the pedicle height at all levels except at L5. The morphology of the pedicle, such as shape, width and height, has been shown to differ throughout the lumbosacral spine [10–12]. Alfonso et al. reported that the L5 vertebral body shape is hemispherical in the upper part of the pedicle and triangular in the lower part of the pedicle, which likely explains our finding [13]. Last, based on our measurements, 25 mm can serve as a safe value for the maximum length of pedicle screws from L1 to S1.
Recently, Matsukawa et al. published a morphometric measurement of CBT for the lumbar pedicle screw insertion [14]. In that study, the intersection of the junction of the center of the superior facet and 1 mm inferior to the inferior border of the transverse process was used as bony landmarks to establish a starting point. Adequate visualization of the transverse process requires soft tissue dissection that may contribute to access-related muscle trauma, which may affect recovery time. In addition, using the inferior facet instead of the superior facet serves as a better bony landmark for establishing a starting point because the inferior facet is in the vicinity of the screw insertion point and may minimize the risk of inadvertent facet capsule disruption. Despite the differences in bony landmarks for establishing a starting point, the results from this current study validate the results from the Matsukawa study as the lateral and cephalad angles reported in both studies were relatively similar. In addition, the results of our study showed that the distances from the starting point to the inferior border of the transverse process from L1 to L5 were all nearly 1.0 mm, which were again similar to the measurements reported by Matsukawa et al.
Despite the increased use of CBT screws in the lumbar spine, little has been reported on the technique in sacral spine. Due to the unique anatomy of the sacral foramen, the sacrum does not contain a true pedicle of cortical bone ring [15, 16]. Additionally, the sacrum mainly consists of cancellous bone, and the superior sacral endplate has a higher bone mineral density than other layers of the S1 body [17, 18]. It has been reported that the anterolateral part of the upper S1 body is the densest area of the sacral trabecular intersection [18, 19]. In a study by Matsukawa et al. on sacral CBT, the entry point was described as the junction of the center of the superior articular process of S1 and approximately 3 mm inferior to the most inferior border of the inferior articular process of L5 [20]. In our study, the starting point of S1 was the junction of the medial border of the S1 pedicle and the inferior border of the L5 inferior articular process, which is closer to the superior endplate and might be easier to visualize. The sacral CBT screw in our study was targeted to the superior-anterolateral part of the sacrum, which is the anatomically favorable region needed to obtain contact with dense bone.
In addition to the stronger fixation strength afforded by CBT pedicle screw, there are several other advantages of this technique. Mobbs et al. reported on successfully using CBT technique in trauma, tumor and degenerative pathologies [21]. Some of the proposed advantages mentioned are that the CBT technique can be used in the proximal aspect of a construct to avoid wide dissection of the mobile superior facet joint, which minimizes iatrogenic instability. In addition, the CBT technique reduces incision length and muscle dissection, thus minimizing approach-related trauma, which makes it an attractive option for minimally invasive spine surgery. Takata et al. reported successfully outcomes in patients with spondylolisthesis undergoing minimally invasive spine fusion with a hybrid construct of CBT pedicle screw at the cephalad level and traditional pedicle screw at the caudal level [22]. For obese patients, the CBT technique may also be a favorable option given the depth of soft tissue in the low back that may make it challenging to insert pedicle screws through the traditional transpedicular axis.
There are several potential drawbacks to the CBT technique. As with traditional pedicle screw placement, canal breach with pedicle screws poses a risk of neurologic injury although this has not been reported in patients undergoing spine fusion with the CBT technique. The cortical path of the CBT technique may actually prove to be advantageous in avoiding canal breach given the medial-to-lateral direction of the pedicle screw away from the neural elements. Exiting nerve root injuries are also possible during screw insertion from incorrect depth of screw penetration or incorrect screw trajectory. Pars fracture is also a theoretical risk of CBT technique given the location of the starting point. It has been recommended that a traditional pedicle screw should be placed if a pars fracture occurs while attempting to insert a CBT screw [21]. A thorough understanding of the spine anatomy and screw insertion technique is essential to decrease the risks of these complications. Last, another potential disadvantage of the CBT technique is difficulty with rod placement when used in a hybrid construct due to the fact that CBT pedicle screw heads may not line up in the para-sagittal plane with traditional pedicle screw heads [22, 23].
In this study, we present a detailed assessment of lumbosacral CBT pedicle screw starting point, trajectory, length and diameter using CT scan. The result of this study provides valuable technical information to spine surgeons hoping to add the CBT pedicle screw technique to their toolbox for options during spinal fusion.
References
Hu SS (1997) Internal fixation in the osteoporotic spine. Spine (Phila Pa 1976) 22(24 Suppl):43S–48S
Okuyama K, Sato K, Abe E, Inaba H, Shimada Y, Murai H (1993) Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine (Phila Pa 1976) 18(15):2240–2245
Matsukawa K, Yato Y, Hynes RA, Imabayashi H, Hosogane N, Yoshihara Y et al (2015) Comparison of pedicle screw fixation strength among different transpedicular trajectories: a finite element study. J Spinal Disord Tech [Epub ahead of print]
Yuan Q, Han X, Han X, He D, Liu B, Tian W (2014) Krag versus caudad trajectory technique for pedicle screw insertion in osteoporotic vertebrae: biomechanical comparison and analysis. Spine (Phila Pa 1976) 39(26B):B27–B35
Colmana M, Pondb J, Bachusc K, Lawrenced BD, Spikere WR, Brodkef DS (2014) Fenestrated screws augmented with PMMA increase the pull-out strength of sacral pedicle screws. J Spinal Disord Tech [Epub ahead of print]
Ueno M, Sakai R, Tanaka K, Inoue G, Uchida K, Imura T et al (2015) Should we use cortical bone screws for cortical bone trajectory? J Neurosurg Spine 22(4):416–421
Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA et al (2009) Cortical bone trajectory for lumbar pedicle screws. Spine J 9(5):366–373
Inceoglu S, Montgomery WH Jr, St Clair S, McLain RF (2011) Pedicle screw insertion angle and pullout strength: comparison of 2 proposed strategies. J Neurosurg Spine (Phila Pa 1976) 14(5):670–676
Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K (2014) In vivo analysis of insertional torque during pedicle screwing using cortical bone trajectory technique. Spine (Phila Pa 1976) 39(4):E240–E245
Sugisaki K, An HS, Espinoza Orías AA, Rhim R, Andersson GB, Inoue N (2009) In vivo three-dimensional morphometric analysis of the lumbar pedicle isthmus. Spine (Phila Pa 1976) 34(24):2599–2604
Su BW, Kim PD, Cha TD, Lee J, April EW, Weidenbaum M, Vaccaro AR (2009) An anatomical study of the mid-lateral pars relative to the pedicle footprint in the lower lumbar spine. Spine (Phila Pa 1976) 34(13):1355–1362
Li B, Jiang B, Fu Z, Zhang D, Wang T (2004) Accurate determination of isthmus of lumbar pedicle: a morphometric study using reformatted computed tomographic images. Spine (Phila Pa 1976) 29(21):2438–2444
Alfonso M, Palacio P, Bastarrika G, Villas C (2008) Does the shape of the L5 vertebral body depend on the height of CT slices in the pedicle? Evaluation of the shape of the L5 vertebral body with a multicut CT scan. Spine (Phila Pa 1976) 33(1):E1–E5
Matsukawa K, Yato Y, Nemoto O, Imabayashi H, Asazuma T, Nemoto K (2013) Morphometric measurement of cortical bone trajectory for lumbar pedicle screw insertion using computed tomography. J Spinal Disord Tech 26(6):E248–E253
Robertson PA, Plank LD (1999) Pedicle screw placement at the sacrum: anatomical characterization and limitations at S1. J Spinal Disord 12(3):227–233
Esses SI, Botsford DJ, Huler RJ, Rauschning W (1991) Surgical anatomy of the sacrum: a guide for rational screw fixation. Spine (Phila Pa 1976) 16(6 Suppl):S283–S288
Peretz AM, Hipp JA, Heggeness MH (1998) The internal bony architecture of the sacrum. Spine (Phila Pa 1976) 23(9):971–974
Zheng Y, Lu WW, Zhu Q, Qin L, Zhong S, Leong JC (2000) Variation in bone mineral density of the sacrum in young adults and its significance for sacral fixation. Spine (Phila Pa 1976) 25(3):353–357
Ebraheim N, Sabry FF, Nadim Y, Xu R, Yeasting RA (2000) Internal architecture of the sacrum in the elderly. An anatomic and radiographic study. Spine (Phila Pa 1976) 25(3):292–297
Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K (2014) Cortical bone trajectory for lumbosacral fixation: penetrating S-1 endplate screw technique: technical note. J Neurosurg Spine 21(2):203–209
Mobbs RJ (2013) The “medio-latero-superior trajectory technique”: an alternative cortical trajectory for pedicle fixation. Orthopaed Surg 5(1):56–59
Takata Y, Matsuura T, Higashino K, Sakai T, Mishiro T, Suzue N et al (2014) Hybrid technique of cortical bone trajectory and pedicle screwing for minimally invasive spine reconstruction surgery: a technical note. J Med Investig JMI 61(3–4):388–392
Rodriguez A, Neal MT, Liu A, Somasundaram A, Hsu W, Branch CL Jr (2014) Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurg Focus 36(3):E9
Acknowledgments
This work is in financially supported by the National Natural Science Foundation of China (NSFC) (81301670) and Specialized Research Fund for the Doctoral Program of Higher Education (SRFDP) (No. 20110101120122).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, H., Ajiboye, R.M., Shamie, A.N. et al. Morphometric measurement of the lumbosacral spine for minimally invasive cortical bone trajectory implant using computed tomography. Eur Spine J 25, 870–876 (2016). https://doi.org/10.1007/s00586-015-4224-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4224-3