Abstract
Purpose
A prospective, longitudinal cohort was studied to determine the incidence, consequences, and risk factors of major perioperative complications in patients with cerebral palsy (CP) treated with spinal fusion. There is a wide variety of data available on the complications of spine surgery; however, little exists on the perioperative complications in patients with CP.
Methods
A prospective multicenter dataset of consecutive patients with CP treated with spinal fusion was evaluated. All major perioperative complications were identified and stratified into categories: pulmonary, gastrointestinal, other medical, wound infection, neurological, instrumentation related, and unplanned staged surgery. Univariate and multivariate analyses were performed to identify various risk factors for major perioperative complications.
Results
127 patients were identified with a mean age of 14.3 ± 2.6 years. Overall, 39.4 % of the patients had a major perioperative complication. Occurrence of a complication [no complication (NC), yes complication (YC)] resulted in significantly increased intensive care unit (ICU) (NC = 3.2 days, YC = 7.8 days, p < 0.05) and hospital stays (NC = 7.7 days, YC = 15.6 days, p < 0.05). Variables associated with greater risk of a complication included: increased estimated blood loss (EBL) (p < 0.001), larger preoperative kyphosis (p = 0.05), staged procedures (p < 0.05), a lack of antifibrinolytic use (p < 0.05), and a trend toward lower body mass index (BMI) (p = 0.08). Multivariate regression analysis revealed an increased EBL as independently associated with a major perioperative complication (p < 0.05).
Conclusions
In this cohort of patients with CP who underwent spinal fusion, 39.4 % experienced a major perioperative complication, with pulmonary being the most common. The occurrence of a major perioperative complication lengthened both ICU and hospital stay. Risk factors for major perioperative complications included greater preoperative kyphosis, staged procedures, a lack of antifibrinolytic use, and increased EBL, with the latter being an independent predictor of a major perioperative complication.
Level of evidence
2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Scoliosis is the most common spinal abnormality in patients with cerebral palsy (CP), with an incidence ranging from 15 to 80 % [1–3]. There is a vast literature published on the surgical treatment of neuromuscular scoliosis in patients with CP [4–12], but few studies have documented the complications involved with those procedures [8, 12–21], with the majority including patients with CP as a subgroup of patients with neuromuscular scoliosis [16–21].
Based on the current literature, complications involving the treatment of neuromuscular scoliosis are common, with rates ranging from 44 to 62 % [16–18, 20, 21]. In 2007, Mohamad et al. [19] reported on 175 patients with neuromuscular scoliosis, 73.7 % of whom had CP. They found an overall perioperative complication rate of 33.1 % (58/175) and concluded that patients with a history of seizures or those who experienced increased intraoperative blood loss were more likely to experience complications [19]. To date, Tsirikos et al. [12] have published the largest study on complications in a series of 287 patients with CP treated with unit rod instrumentation, reporting an intraoperative complication rate of 10.8 % (38/287), an early postoperative (within 6 weeks) complication rate of 9.4 % (27/287), and a late postoperative complication rate of 10.1 % (29/287). However, this study was retrospective and did not report on the risk factors that may lead to major perioperative complications in the treatment of scoliosis in patients with CP.
The purpose of this study was to define the incidence of major perioperative complications in patients with CP treated with spinal fusion and determine its impact on the length of intensive care unit (ICU) and hospital stays. Furthermore, this study sought to identify the risk factors that may be associated with major perioperative complications in these patients.
Materials and methods
Institutional Review Board approval for the study was obtained locally from each contributing institution’s review board, and written and informed consent was obtained from each patient prior to preoperative data collection. The prospectively collected multicenter database of consecutive patients with CP treated with spinal fusion was queried to identify cases with at least 90 days of follow-up. From a total of 131 patients, the 127 patients with at least 90 days of follow-up were included.
Data collection forms were completed by the investigators at the preoperative, operative and postoperative visits. Clinical, radiographic, and intraoperative measurements were recorded. All major perioperative (within 90 days of surgery) complications as defined by Hod-Feins et al. [22] were identified by the treating physicians at the times of evaluation and stratified into categories including: pulmonary, gastrointestinal, other medical, wound infection, neurologic, instrumentation related, and unplanned staged surgery. The major pulmonary complications included were respiratory compromise requiring reintubation or prolonged intubation and pneumonia or significant pleural effusion requiring chest tube placement. Pulmonary complications including asymptomatic atelectasis, pulmonary contusions, or pleural effusion were not included. We excluded the aforementioned complications as there was variability among the sites in reporting these entities. However, any complication which necessitated an intervention, such as placement of a chest tube, was included. The major gastrointestinal complications included gastrointestinal bleeding, superior mesenteric artery syndrome, and pancreatitis. Gastrointestinal complications including constipation, elevated liver enzymes or bilirubin, nausea, or vomiting were not included. The major “other” medical complications included postoperative coagulopathy or acute hemodynamic instability requiring resuscitation with inotropic support. The major neurologic complications included any motor or sensory complications or changes in bladder continence. Infections and instrumentation-related complications were only considered major complications if they required a reoperation. Unplanned second surgery included those patients in whom the first attempt was aborted.
Univariate and multivariate analyses were performed on a variety of possible risk factors for major perioperative complications including: age, gender, body mass index (BMI), gross motor function classification system level, ambulatory status, seizure status, use of divalproex sodium (Depakote), preoperative major coronal Cobb angle, preoperative kyphosis (T2–T12), preoperative pelvic obliquity, fusion to the pelvis, preoperative albumin, preoperative white blood cell count (WBC), preoperative total protein, antifibrinolytic use, estimated blood loss (EBL), operative time, surgical approach, and staged procedures.
Statistical analysis was performed using the SPSS 12.0.2 statistical package (SPSS Inc., Chicago, IL). All results were reported as means plus or minus standard deviation (SD) with a significance level of 0.05 and a confidence interval of 95 %.
Results
Patient demographics (Table 1)
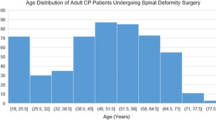
A total of 127 patients with CP treated with spinal fusion were identified with a mean age of 14.3 ± 2.6 years. 58.3 % (74/127) of the patients were male. The mean preoperative radiographic measurements were: major coronal Cobb angle 80.9° ± 27.4°, minor coronal Cobb angle 35.6° ± 16.8°, major coronal curve percent flexibility 36.0 ± 16.9 %, minor coronal curve percent flexibility 29.1 ± 22.5 %, kyphosis (T2–T12) 43.1° ± 23.1°, lordosis (T12 to top of sacrum) −38.4° ± 33.6°, sagittal balance (C7 to sacrum) 1.6 ± 6.9 cm, and pelvic obliquity 63.1° ± 14.9°. Eleven patients had staged procedures.
Major perioperative complications (Table 2)
Overall, there were 87 major perioperative complications in 50 patients for a major perioperative complication rate of 39.4 % (50/127). The major perioperative complications occurred at the following rates: Pulmonary 29.9 % (38/127), gastrointestinal 18.9 % (24/127), other medical (coagulopathy and severe hypotension) 11.8 % (15/127), wound infection 4.7 % (6/127), instrumentation related 1.6 % (2/127), unplanned staged surgery 0.8 % (1/127), and neurologic 0.8 % (1/127).
Of the pulmonary complications, five patients required reintubation for respiratory failure, seven patients required prolonged intubation, three patients required CT placement for effusion, and two patients required tracheostomy. In addition, 73.7 % (28/38) of these patients had a past medical history significant for asthma, pneumonia, or aspiration. Of the gastrointestinal complications, 22 patients had pancreatitis, one patient experienced ischemic colitis requiring bowel resection, and one patient experienced Clostridium difficile colitis. We hypothesize that the cause of pancreatitis is multifactorial and includes lengthy time in the prone position, blood loss, and potential stretching of the vascular supply after deformity correction. Thirteen patients had an acute hypotensive event requiring support for hemodynamic instability. There was one patient who died from cardiorespiratory failure. Two patients experienced severe intraoperative coagulopathy. Regarding wound infection complications, five patients required reoperation for deep wound infections, and one patient had an incision and drainage for a suspected deep wound infection. Of the instrumentation-related complications, one patient experienced proximal junctional kyphosis requiring a reoperation, and the other required revision surgery for prominent instrumentation with removal of the superior aspect of the unit rod and application of a cross-connector. One patient had the primary attempt at correction halted prior to completion after experiencing excessive blood loss; the patient had an unplanned second procedure 4 days later. One patient experienced a neurologic complication involving a nerve root injury resulting in neuropathy to the right upper leg.
Occurrence of a complication [no complication (NC), yes complication (YC)] resulted in a significantly increased ICU (NC = 3.2 days, YC = 7.8 days, p < 0.05) and hospital stay (NC = 7.7 days, YC = 15.6 days, p < 0.05).
Risk factors (Table 3)
Univariate analysis revealed the following as risk factors associated with major perioperative complications: increased EBL (p < 0.001), larger preoperative kyphosis (p = 0.05), staged procedures (p < 0.05), a lack of antifibrinolytic use (p < 0.05), and a trend toward lower BMI (p = 0.08). Multivariate regression analysis revealed increased EBL as an independent predictor of a major perioperative complication (p < 0.05).
Discussion
Several studies have documented the incidence of complications in patients with CP treated with spinal fusion. In this study, the incidence of a major perioperative complication was 39.4 %, with pulmonary being the most common category. The occurrence of a major perioperative complication significantly increased ICU and hospital length of stay. Risk factors for major perioperative complications included greater preoperative kyphosis, staged procedures, a lack of antifibrinolytic use, and increased EBL, with the latter being an independent predictor of a major perioperative complication.
Lonstein et al. [13] reported a 58 % rate for early complications (complications that occurred intraoperatively or during the hospital stay), and a 47 % rate for late complications (complications that occurred after discharge) in 93 patients with CP treated with the Luque–Galveston method. These values were higher than the 39.4 % rate of major perioperative complications in the current study because they included all complications rather than just the major perioperative complications (as defined by Hod-Feins et al. [22]) that we reported. Mohamad et al. [19] and Lonstein et al. [13] noted that respiratory complications were the most common complication in patients with neuromuscular scoliosis (mostly pneumonia and atelectasis). Previous studies have shown that respiratory diseases may be the most common cause of death in patients with CP [23–29]. The current study found that the majority (29.9 %) of major perioperative complications were pulmonary, and that 73 % of the pulmonary complications were for respiratory failure. In addition, 73.7 % (28/38) of the patients with major perioperative pulmonary complications had a past medical history significant for asthma, pneumonia, or aspiration. This leads the authors to suggest that a thorough evaluation of the respiratory medical history (pneumonia, aspiration, or asthma) is necessary before proceeding with surgery in this cohort of patients. Some reasons for the high incidence of pulmonary issues may include the preexisting spine deformity impacting pulmonary volume and the fact that many of these patients are sitters and thus do not push their pulmonary capacity. Preoperative pulmonary optimization, whenever possible, may be most important in those patients identified preoperatively to have the most significant dysfunction.
Based on the Kaplan–Meier survival analysis, Tsirikos et al. [30] concluded that 68 % of patients with CP who have spinal instrumentation are expected to survive at least 11 years, with the most predictive determinant for survival rate being the number of days the patient had to spend after surgery in the ICU. Our study showed that there was a significant increase in both ICU and hospital length of stay in patients with CP who experienced major perioperative complications. This corresponds with Lonstein et al. [13] who also found a statistically significant increase in hospital length of stay associated with early infections. As a result, it is important for surgeons to try to minimize major perioperative complications in this patient population not only because these complications have an immediate impact on hospital and ICU length of stay, but because they may have a greater long-term impact on patient mortality. Longer follow-up time of the current study would be necessary to show this correlation.
In 2003, Tsirikos et al. [30] suggested that there was a weak relationship with kyphosis >90° decreasing survival rates in patients with CP undergoing spinal fusion. Our study showed a similar relationship with preoperative kyphosis (T2–T12) being a risk factor for major perioperative complications in patients of the same subset.
In a different study, Tsirikos et al. [31] compared one-stage versus two-stage anteroposterior spinal fusion in patients with CP and found a higher rate of intraoperative blood loss, longer surgery times, and increased complications in the group that received single-stage anteroposterior spinal fusions. Our study showed different results, with univariate analysis revealing staged procedures as a risk factor for a major perioperative complication in patients with CP treated with spinal fusion. This was also supported by Ferguson et al. [32] who showed fewer complications in patients with neuromuscular scoliosis treated with a single-stage anteroposterior procedure compared to a two-stage anteroposterior procedure. This was supported by our study that showed 54.5 % (6/11) of the patients with staged procedures sustained major perioperative pulmonary complications (one of those patients also had pancreatitis, and one required a reoperation for an infection). Of the remaining five patients, one required an unplanned staged procedure due to increased blood loss leading to hypotension, one had pancreatitis, and the other three did not have any major perioperative complications.
In 1992, Kalen et al. [33] suggested that the best predictor for postoperative complications in children with CP who undergo spinal surgery is their degree of neurologic disability, along with associated medical problems and a curve >70°.
The current study also revealed that the lack of antifibrinolytic use and increased estimated blood loss as risk factors for major perioperative complications in patients with CP treated with spinal fusion. There are studies that suggest that increased blood loss may lead to complications, mainly infections, in scoliosis surgery [34–37], but none have reported this finding in patients with CP. Our data did not show a relationship between increased estimated blood loss and higher rates of infection, but this is most likely due to the small number of complications in the study.
As would be expected, patients with CP undergoing spinal fusion sustain very different complications when compared to other pediatric cohorts, such as patients with adolescent idiopathic scoliosis. Utilizing the Morbidity and Mortality database from the Scoliosis Research Society [38], we found an overall complication rate of 5.7 %, which was substantially lower than the 39.4 % in our current series. In addition, the most common complication in their cohort of patients with posterior instrumentation and fusion for AIS was wound infection, whereas ours was pulmonary.
In conclusion, in this cohort of patients with CP who underwent spinal fusion, 39.4 % experienced a major perioperative complication, with pulmonary being the most common. The occurrence of a major perioperative complication lengthened both ICU and hospital stay. Risk factors for major perioperative complications included greater preoperative kyphosis, staged procedures, a lack of antifibrinolytic use, and increased EBL, with the latter being an independent predictor of a major perioperative complication.
References
Samilson RL, Bechard R (1973) Scoliosis in cerebral palsy: incidence, distribution of curve patterns, natural history and thoughts on etiology. Curr Pract Orthop Surg 5:183–205
Balmer GA, MacEwen GD (1970) The incidence and treatment of scoliosis in cerebral palsy. J Bone Joint Surg Br 52(1):134–137
Persson-Bunke M, Hagglund G, Lauge-Pedersen H, Wagner P, Westbom L (2012) Scoliosis in a total population of children with cerebral palsy. Spine (Phila Pa 1976) 37(12):E708–E713. doi:10.1097/BRS.0b013e318246a962
Rinsky LA (1990) Surgery of spinal deformity in cerebral palsy. Twelve years in the evolution of scoliosis management. Clin Orthop Relat Res 253:100–109
Boachie-Adjei O, Lonstein JE, Winter RB, Koop S, vanden Brink K, Denis F (1989) Management of neuromuscular spinal deformities with Luque segmental instrumentation. J Bone Joint Surg Am 71(4):548–562
Tsirikos AI, Mains E (2012) Surgical correction of spinal deformity in patients with cerebral palsy using pedicle screw instrumentation. J Spinal Disord Tech 25(7):401–408
Tsirikos AI (2010) Development and treatment of spinal deformity in patients with cerebral palsy. Indian J Orthop 44(2):148–158
Sponseller PD, Shah SA, Abel MF, Sucato D, Newton PO, Shufflebarger H, Lenke LG, Letko L, Betz R, Marks M, Bastrom T, Harms Study Group (2009) Scoliosis surgery in cerebral palsy: differences between unit rod and custom rods. Spine (Phila Pa 1976) 34(8):840–844. doi:10.1097/BRS.0b013e31819487b7
Teli MG, Cinnella P, Vincitorio F, Lovi A, Grava G, Brayda-Bruno M (2006) Spinal fusion with Cotrel-Dubousset instrumentation for neuropathic scoliosis in patients with cerebral palsy. Spine (Phila Pa 1976) 31(14):E441–E447. doi:10.1097/01.brs.0000221986.07992.fb
Bulman WA, Dormans JP, Ecker ML, Drummond DS (1996) Posterior spinal fusion for scoliosis in patients with cerebral palsy: a comparison of Luque rod and unit rod instrumentation. J Pediatr Orthop 16(3):314–323
Swank SM, Cohen DS, Brown JC (1989) Spine fusion in cerebral palsy with L-rod segmental spinal instrumentation. A comparison of single and two-stage combined approach with Zielke instrumentation. Spine (Phila Pa 1976) 14(7):750–759
Tsirikos AI, Lipton G, Chang WN, Dabney KW, Miller F (2008) Surgical correction of scoliosis in pediatric patients with cerebral palsy using the unit rod instrumentation. Spine (Phila Pa 1976) 33(10):1133–1140
Lonstein JE, Koop SE, Novachek TF, Perra JH (2012) Results and complications after spinal fusion for neuromuscular scoliosis in cerebral palsy and static encephalopathy using Luque Galveston instrumentation: experience in 93 patients. Spine (Phila Pa 1976) 37(7):583–591. doi:10.1097/BRS.0b013e318225ebd5
Jevsevar DS, Karlin LI (1993) The relationship between preoperative nutritional status and complications after an operation for scoliosis in patients who have cerebral palsy. J Bone Joint Surg Am 75(6):880–884
Szoke G, Lipton G, Miller F, Dabney K (1998) Wound infection after spinal fusion in children with cerebral palsy. J Pediatr Orthop 18(6):727–733
Edwards BT, Zura R, Bertrand S, Leonard S, Pellett J (2003) Treatment of neuromuscular scoliosis with posterior spinal fusion using the Galveston technique: a retrospective review and results of 62 patients. J Long Term Eff Med Implant 13(6):437–444
Benson ER, Thomson JD, Smith BG, Banta JV (1998) Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine (Phila Pa 1976) 23(21):2308–2317
Teli M, Elsebaie H, Biant L, Noordeen H (2005) Neuromuscular scoliosis treated by segmental third-generation instrumented spinal fusion. J Spinal Disord Tech 18(5):430–438
Mohamad F, Parent S, Pawelek J, Marks M, Bastrom T, Faro F, Newton P (2007) Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 27(4):392–397
Reames DL, Smith JS, Fu KM, Polly DW Jr, Ames CP, Berven SH, Perra JH, Glassman SD, McCarthy RE, Knapp RD Jr, Heary R, Shaffrey CI, Scoliosis Research Society Morbidity and Mortality Committee (2011) Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine (Phila Pa 1976) 36(18):1484–1491. doi:10.1097/BRS.0b013e3181f3a326
Master DL, Son-Hing JP, Poe-Kochert C, Armstrong DG, Thompson GH (2011) Risk factors for major complications after surgery for neuromuscular scoliosis. Spine (Phila Pa 1976) 36(7):564–571. doi:10.1097/BRS.0b013e3181e193e9
Hod-Feins R, Abu-Kishk I, Eshel G, Barr Y, Anekstein Y, Mirovsky Y (2007) Risk factors affecting the immediate postoperative course in pediatric scoliosis surgery. Spine (Phila Pa 1976) 32(21):2355–2360. doi:10.1097/BRS.0b013e3181558393
Strauss DJ, Shavelle RM, Anderson TW (1998) Life expectancy of children with cerebral palsy. Pediatr Neurol 18(2):143–149
Crichton JU, MacKinnon M, White CP (1995) The life expectancy of persons with cerebral palsy. Dev Med Child Neurol 37(7):567–576
Evans PM, Evans SJ, Alberman E (1990) Cerebral palsy: why we must plan for survival. Arch Dis Child 65(12):1329–1333
Hutton JL, Cooke T, Pharoah PO (1994) Life expectancy in children with cerebral palsy. BMJ 309(6952):431–435
Hutton JL, Colver AF, Mackie PC (2000) Effect of severity of disability on survival in northeast England cerebral palsy cohort. Arch Dis Child 83(6):468–474
Chaney RH, Eyman RK, Miller CR (1979) Comparison of respiratory mortality in the profoundly mentally retarded and in the less retarded. J Ment Defic Res 23(1):1–7
Anderson TW (1997) Life expectancy in cerebral palsy. Lancet 349:283–284
Tsirikos AI, Chang WN, Dabney KW, Miller F, Glutting J (2003) Life expectancy in pediatric patients with cerebral palsy and neuromuscular scoliosis who underwent spinal fusion. Dev Med Child Neurol 45(10):677–682
Tsirikos AI, Chang WN, Dabney KW, Miller F (2003) Comparison of one-stage versus two-stage anteroposterior spinal fusion in pediatric patients with cerebral palsy and neuromuscular scoliosis. Spine (Phila Pa 1976) 28(12):1300–1305
Ferguson RL, Hansen MM, Nicholas DA, Allen BL Jr (1996) Same-day versus staged anterior-posterior spinal surgery in a neuromuscular population: the evaluation of medical complications. J Pediatr Orthop 16(3):293–303
Kalen V, Conklin MM, Sherman FC (1992) Untreated scoliosis in severe cerebral palsy. J Pediatr Orthop 12(3):337–340
Gerometta A, Rodriguez Olaverri JC, Bitan F (2012) Infections in spinal instrumentation. Int Orthop 36(2):457–464
Koutsoumbelis S, Hughes AP, Girardi FP, Cammisa FP Jr, Finerty EA, Nguyen JT, Gausden E, Sama AA (2011) Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am 93(17):1627–1633. doi:10.2106/JBJS.J.00039
Watanabe M, Sakai D, Matsuyama D, Yamamoto Y, Sato M, Mochida J (2010) Risk factors for surgical site infection following spine surgery: efficacy of intraoperative saline irrigation. J Neurosurg Spine 12(5):540–546. doi:10.3171/2009.11.SPINE09308
Pull Ter Gunne AF, Cohen DB (2009) Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 34(13):1422–1428
Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, Perra JH, Shaffrey CI (2006) Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 31(3):345–349
Acknowledgments
This study was supported by a research grant from DePuy Synthes Spine to the Setting Scoliosis Straight Foundation for the Harms Study Group. Dr. Belin’s fellowship was supported by a grant from the Orthopaedic Research and Education Foundation.
Conflict of interest
Research supported by a grant from the Setting Scoliosis Straight Foundation for the Harms Study Group
Informed consent
IRB approval for the study was obtained locally from each contributing institution’s review board, and consent was obtained from each patient prior to data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samdani, A.F., Belin, E.J., Bennett, J.T. et al. Major perioperative complications after spine surgery in patients with cerebral palsy: assessment of risk factors. Eur Spine J 25, 795–800 (2016). https://doi.org/10.1007/s00586-015-4054-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-4054-3