Abstract
Purpose
To explore the relationship between cervical spine and the global spine alignment and to postulate the hypotheses that a lordotic alignment of cervical spine is not the only standard to identify asymptomatic subjects, and the degenerative modification of cervical curves depends primarily on their spinal-pelvic alignment.
Methods
A cohort of 120 cases of Chinese asymptomatic subjects and a cohort of 121 cases of Chinese cervical spondylotic patients were recruited prospectively from 2011 to 2012. Roussouly Classification was utilized to categorize all subjects and patients according to their thoracic spine, lumbar spine and pelvic alignment. The cervical alignments were evaluated as lordosis, straight, sigmoid or kyphosis. Through the lateral X-ray images of neutral cervical and global spine, a number of parameters were measured and analyzed, including pelvic incidence, pelvic tilt, sacral slope, thoracic kyphosis (TK), lumbar lordosis, global cervical angles (angles between two lines parallel with posterior walls of C2 and C7), practical cervical angles (the addition of different cervical end plate angles from C3 to C7, and inter-vertebral angles from C23 to C67), T1 slope, spinal sacral angles (SSA), Hip to C7/Hip to Sacrum and C0–C2 angle.
Results
The percentages of cervical lordosis were 28.3 % and 36.4 % in asymptomatic and spondylotic group, respectively. The cervical spine alignments correlated with Roussouly types of global spine alignment in both asymptomatic and cervical spondylotic group (P < 0.001). And there were significant differences between Roussouly Type 2 and 4, Type 3 and 4, Type 1 and 3 in cervical angles in spondylotic group (P < 0.05). In the comparison of the two cohorts, significant differences were found in both general and practical cervical angles in Roussouly Type 4 (P = 0.00 and 0.01, respectively), and there were significant differences in inter-vertebral angle in Roussouly Type 2 at C4–5 and C5–6 levels (P = 0.04 and 0.04, respectively), and in Roussouly Type 3 at C6–7 level (P = 0.01). The SSA showed significant difference between Roussouly Type 2 and 4 in asymptomatic subjects (P = 0.00), and between Type 1 and 3, 1 and 4, 2 and 3, 2 and 4 in cervical spondylotic patients (P = 0.01, 0.02, 0.00 and 0.01, respectively). The T1 slope was significantly different among Roussouly types (P = 0.04) with its largest value in Type 1 in cervical spondylotic group. There are significant differences in C0–C2 angles in all Roussouly types (P = 0.01, 0.02, 0.00 and 0.01, respectively), as well as in the ratio of Hip to C7/hip to sacrum in Type 2 (P = 0.01), and Type 3 (P = 0.00) in the comparison of the two cohorts. The multiple linear regression of all parameters showed both general and practical cervical angles were significantly related to TK, C0–C2 and T1 slope (P = 0.01, 0.00 and 0.00, respectively).
Conclusion
The cervical alignment correlates with their global spine and pelvic curves. And lordosis is not the only presentation in asymptomatic subjects. The degenerative modification of cervical disc angles was the compensation of global spine degeneration for horizontal gaze. Cervical angles are influenced by their TK angles, occipital-C2 joint and the tilt of T1 vertebral body. The occipital-C2 joint has a compensating mechanism in all Roussouly types in cervical spondylosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical lordosis forms naturally as the infant begins to raise his or her head, and its modification correlates with age. Cervical curvature has been thought to be the secondary curve counterbalancing to the primary curve of the thoracic and sacral spine [1, 2]. On the other hand, a kyphosis was regarded as a pathological alignment in the recognition of cervical spine [3].
However, the correlation between the physiological alignment and clinical symptoms was still controversial because segmental kyphotic curve had been detected in asymptomatic subjects [1]. Lee et al. [4] reported 60.2 % (109/131) asymptomatic subjects had hypolordotic cervical spine, including approximately 40 % in kyphosis. Radiographic surveys of asymptomatic persons had found an incidence of “straight” or “kyphotic” cervical spines ranging from 7 to 40 % [5, 6].
So far, the reasons for the variation of cervical spine curves are still unknown. The authentic cervical alignment could probably correlate with the global spine curves. The interaction between thoracic, lumbar spine and pelvis has been well documented in publications during the past decade [7, 8]. However, it is rare to see reports on the relationship between cervical spine and global spino-pelvic curvature. Therefore, we prospectively observed the morphological characteristics of the cervical spine in 120 asymptomatic subjects and 121 cervical spondylotic patients and analyzed the relationship between cervical alignment and spino-pelvic parameters in both groups. We hypothesized that the cervical spine alignments are various according to their global spine sagittal curves.
Materials and methods
A cohort of 120 asymptomatic subjects (including 63 males and 57 females, average age 23.2 ± 6.3 years old) and a cohort of 121 cervical spondylotic cases (including 80 males and 41 females, average age 53.3 ± 10.6 years old) were recruited prospectively from November 2011 to December 2012,Footnote 1 both of which were Chinese. All cervical spondylotic cases were operated with either anterior cervical discectomy/corporectomy with bone fusion or posterior laminoplasty. The asymptomatic ones were free of current or historical symptoms suggestive of spinal or orthopedic diseases and were excluded if they had obvious radiographic abnormality such as scoliosis, spondylolisthesis, spondylolysis, Scheumann disease, leg discrepancy, etc. The distribution of the degenerative levels was showed as L23 2 levels, L34 3 levels, L45 3 levels, L5S1 2 levels. The cervical spondylotic patients were only suffering cervical disease but free from chronic back pain, deformity or other significant orthopedic diseases. Abnormal radiographic signs as asymptomatic ones presented were also ruled out. The distribution of degenerative levels was presented as L12 40 levels, L23 22 levels, L34 60 levels, L45 112 levels, L5S1 118 levels.
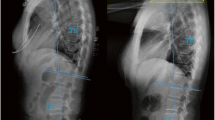
All pre-operative full-length and cervical lateral X-rays of the spine were taken in Peking University Third Hospital, Beijing, China. Patients stood in an erect comfortable position with their hands placed on supports and gaze horizontally to reduce any inaccuracy caused by head motion (Fig. 1) and exposures were taken from the base of the skull to the proximal femora in the left to right lateral plane. The distance from the radiographic source to the film was maintained at 180 cm for all exposures and the edges of the radiographic film were square in respect to the horizontal and vertical axes. The films were digitized with a commercially available optical scanner (XR 650, GE, USA). A custom computer application (PACS, GE Electrics) was used to measure the angles and distances. The global radiological parameters included the pelvic incidence (PI, the angle subtended by the line drawn from the hip axis to the center of upper sacral end plate and the line perpendicular to upper sacral end plate) [9], sacral slope (SS, the angle subtended by the horizontal line and upper sacral end plate) [9], pelvic tilt (PT, the angle subtended by the vertical line and the line drawn from HA to the center of upper sacral end plate) [9], spinal–sacral angles (SSA, sacral end plate and the line from the center of C7 vertebral body to the center of upper sacral end plate) [10], ratio of Hip to C7/Hip to sacrum (horizontal distance from the center of upper sacral end plate to C7 plumb line divided by horizontal distance from the center of upper sacral end plate to HA) [11], C0–C2 angle (the angle between McGregor line and the inferior surface of the axis) [12], T1 slope angle between a horizontal line and the superior end plate of (T1) [13], lumbar lordosis (LL, the angle subtended by the superior end plates of L1 and S1) [9], thoracic kyphosis (TK, the angle subtended by the superior end plate of T4 and inferior end plate of T12) [9] (Fig. 2). All values were measured three times and the average results were obtained.
a Pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), thoracic kyphosis (TK), lumbar lordosis (LL). b Spinal sacral angles, c hip to C7/Hip to sacrum, d T1 slope, e C0–C2 angle. a pelvic incidence (PI) is defined as the angle subtended by the line drawn from the hip axis (HA, center of the line connecting the center of each femoral heads) to the center of upper sacral end plate and the line perpendicular to upper sacral end plate. Pelvic tilt (PT) is defined as the angle subtended by the vertical line and the line drawn from HA to the center of upper sacral end plate. Sacral slope (SS) is defined as the angle subtended by the horizontal line and upper sacral end plate. Thoracic kyphosis (TK) is defined as the angle subtended by the lines drawn along the superior end plate of T4 and inferior end plate of T12. Lumbar lordosis (LL) is defined as the angle subtended by line drawn along the superior end plates of L1 and S1. b Spinal sacral angles (SSA): sacral end plate and the line from the center of C7 vertebral body to the center of upper sacral end plate. c Hip to C7/Hip to sacrum: horizontal distance from the center of upper sacral end plate to C7 plumb line (drawn from the center of C7 vertebral body). divided by horizontal distance from the center of upper sacral end plate to HA. d T1 slope is defined as the angle between a horizontal line and the superior end plate of T1. e C0–C2 angle is defined as the angle between McGregor line (a line passing through the postero-superior aspect of the hard palate and the most caudal point on the midline occipital curve) and the inferior surface of the axis
The relative inclinations of lines passing through the superior and inferior end plate of vertebral bodies from C2 to C7 were recorded, which provided a measurement for angles of end plates and discs (Fig. 3a). And local measurement involved cervical end plate angles (from C3 to C7), the inter-vertebral angles (from C23 to C67), global cervical angle (two lines parallel with posterior walls of C2 and C7, Fig. 3b), practical cervical angle (the addition of each end plate angle from C3 to C7, and each inter-vertebral angle from C23 to C67).
We categorized the cervical sagittal alignment into four types: lordosis, straight, sigmoid and kyphosis [14] (Fig. 4). Two diagonal lines were drawn after constructing four contour tangents for each body. Each connects two corners of the vertebra, where adjacent contour tangents intersect. The intersection of these two lines is the vertebral centroid. Line AB was constructed to connect midpoint A on the inferior surface of C2 and midpoint B on the superior surface of C7. The alignment is then determined from the position of the centroids relative to line AB. The four types of the cervical sagittal alignment are therefore defined as follows. Lordosis: all centroids are anterior to AB and the apex distance is more than 2 mm; Straight: the distance between line AB and each centroid is less than 2 mm; Sigmoid: some centroids are anterior to and some posterior to line AB and the distance between AB and at least one centroid is more than 2 mm; Kyphosis: all the centroids are posterior to line AB and the distance between at least one centroid and the AB is 2 mm or more (Fig. 5).
The degenerative changes of disc space narrowing, end-plate sclerosis, and anterior and posterior osteophyte formation were recorded for each cervical disc space.
All subjects in the two cohorts were categorized with Roussouly Morphological Classification [8] according to their PI, SS, PT, thoracic and lumbar alignments. To avoid the intra-observer bias, all radiographs were reviewed by two senior spine surgeons, respectively. If they disagreed, a third one was invited to make a final decision.
The data were analyzed with SPSS 15.0 software (SPSS Inc, Chicago, IL, USA). Statistical significance was set at 0.05. An adaptation of Kolmogorov–Smirnov test was applied to test for normally distributed data. Descriptive statistics in the form of mean ± SD for all spine parameters were provided for all patients. The relationships were assessed with Chi square test. The one-way ANOVA test, Student t tests or Mann–Whitney U test for independent samples were also utilized to evaluate the parameters among different groups. The multiple logistic regression was utilized to analyze dominant determinant among different independent.
Results
The inter-observer correlation in classifying the cervical spine sagittal alignment and Roussouly Sagittal Classification were 0.95 and 0.97, respectively.
Comparison in cervical alignments and Roussouly Classifications in both cohorts
Significant differences were found between the cervical alignments of different Roussouly types in both asymptomatic subjects and cervical spondylotic patients (Tables 1, 2, P < 0.001). In asymptomatic subjects, the percentages of cervical lordosis in Roussouly Type 1 and 4 were 60 and 62.5 %, respectively, and straight cervical alignment accounted for 64.3 % in Roussouly Type 3. Meanwhile, the lordotic alignment took up 56.5 and 88.2 % in Roussouly Type 1 and 4, respectively, and straight ones reached 50 and 58.2 % in Type 2 and 3, respectively, in cervical spondylotic patients. There is no correlation between cervical alignment and the value of PI both in asymptomatic and spondylotic cohorts (P > 0.05). There were significant differences in T1 slope and TK between lordotic and kyphotic alignments (29.6 ± 6.2° versus 20.6 ± 6.4°, P = 0.00; 28.0 ± 8.4° versus 19.7 ± 6.5°, P = 0.00), and between straight and kyphotic alignments (26.3 ± 6.3° versus 20.6 ± 6.3°, P = 0.01; 27.2 ± 6.1° versus 19.7 ± 6.5°, P = 0.00) in asymptomatic cohort. Moreover, significant differences were found in T1 slope and TK between lordotic and straight cervical alignments (27.2 ± 7.8° versus 22.4 ± 7.4°, P = 0.04; 35.9 ± 10.1° versus 29.7 ± 8.5°, P = 0.01) in spondylotic patients.
Comparison of cervical angles between Roussouly classifications in both cohorts
In the cervical spondylotic group, there were significant differences between Roussouly Type 2 and 4, Type 3 and 4 in both Global and Practical cervical angles (Table 3, P = 0.01, 0.00, 0.01 and 0.00, respectively), and also between Type 1 and 3 in Global cervical angles (Table 3, P = 0.04). However, no such significant differences were found in asymptomatic group (P > 0.05). Comparing asymptomatic group and cervical spondylotic group, significant differences were found in both general cervical angles (12.0 ± 5.9° versus 20.8 ± 7.8°, P = 0.00) and practical cervical angles (13.7 ± 12.9° versus 23.5 ± 9.2°, P = 0.01) in Roussouly Type 4.
The intervertebral disc angles in asymptomatic subjects and degenerative levels in spondylotic patients are shown in Table 4. The angle in C56 showed significant difference between Roussouly Type 2 and Type 4 (Table 4, P = 0.04). The distribution of degenerative levels at C45 was significantly different among various Roussouly types with 16 cases in Type 1, 18 cases in Type 2, 28 cases in Type 3 and three cases in Type 4 (Table 4, P = 0.04). In the comparison of asymptomatic subjects and spondylotic patients, there was significant difference at C4–5 level [−0.5° (−6.7°, 11.8°) versus 1.6° (−6.1°, 7.3°), P = 0.04], at C5–6 level [0.5° (−6.6°, 9.2°) versus 2.1° (−0.5, 10.5), P = 0.04] in Roussouly Type 2 and at C6–7 level [3.0° (−0.6°, 11.8°) versus 1.1° (−3.0°, 12.2°), P = 0.01] in Roussouly Type 3.
Comparisons of other parameters in both cohorts
The value of SSA between Roussouly Type 2 and 4 in asymptomatic group showed significant difference (128.6 ± 5.9° versus 135.9 ± 8.2°, P = 0.00). Moreover, in cervical spondylotic group, the values of SSA were statistically different between Type 1 and 3, 1 and 4, 2 and 3, 2 and 4 (Table 5, P = 0.01, 0.02, 0.00 and 0.01, respectively), and the values of T1 slope were different among all Types (Table 5, P = 0.04) with the largest one in Type 1.
In the comparison of parameters between asymptomatic group and cervical spondylotic group, significant differences were found in C0–C2 angles in all Roussouly types (Table 6, P = 0.01, 0.02, 0.00 and 0.01, respectively), and in the ratio of Hip to C7/hip to sacrum in Type 2 [3.0 (−5.7, 12.2) versus 1.4 (−6.6, 7.0), P = 0.01], and Type 3 [2.4 (−7.4, 10.4) versus 1.4 (−1.0, 11.2), P = 0.00].
Multiple linear regression of all the parameters showed that both general and practical cervical angles were significantly related to the thoracic kyphosis, C0–C2 and T1 slope. (Table 7a, b, P = 0.01, 0.00 and 0.00, respectively).
Discussion
The cervical alignments and angles in the two cohorts
It has been well accepted that cervical lordosis is a physiological posture in asymptomatic subjects. However, our results showed that only 28.3 % (34/120) of the cervical alignments maintained lordosis. Radiographic surveys of asymptomatic persons have found an incidence of “straight” or “kyphotic” cervical spines ranging from 7 to 40 % [2, 3]. The percentage of hypolordosis or kyphosis in cervical spine alignment could even be 60.2 % in asymptomatic adolescents, and a decrease of cervical lordosis would happen after the age of 17 years [4]. But for the cervical spondylotic patients, few changes have been found except for an 8.1 % increase of lordosis (from 28.3 to 36.4 %) and a 10 % decrease of kyphosis (from 21.7 to 10.7 %).
Minor modifications of both general and practical angles in cervical spondylotic patients were identified from asymptomatic subjects. Gore el al. reported an average general cervical angle around 15° at the age of 20–25 years, an average around 24° at the age of 50–55 years in healthy volunteers [1]. In our research, in Roussouly Type 1 and 4, the cervical angles increased in cervical spondylotic patients, with statistical significance in Type 4. However, in Roussouly Type 2 and 3, there was a decrease in general cervical angles but a slight increase in practical cervical angles for spondylotic patients compared to asymptomatic subjects. This result might suggest that increasing angles in the discs between C23 and C67 could compensate their slight loss in general angles. And these explanations were supported by the comparisons in intervertebral angles at C45 and C56 in Type 2, and at C67 in Type 3 between asymptomatic subjects and cervical spondylotic patients. And we thought the degeneration of discs might aggravate the variance in cervical angles among types as was shown in Type 1 and 4 compared to Type 2 and 3 in cervical spondylotic patients.
Possible mechanisms of cervical alignment in different Roussouly types
We thought the distribution and modification of the cervical spine might be attributed to their different sagittal spino-pelvic alignments. Moreover, degenerative modification may also follow the characteristic of cervical curve. Boyle et al. reported that the mass of head was balanced over the reciprocal primary and secondary curves of the spine. The consequence of an accentuated thoracic curvature is mirrored in the cervical region with compensatory adjustments to head posture required to preserve forward gaze [6]. In different Roussouly types, the distribution of cervical alignment was varied probably due to its original modification of sagittal curves in spine-pelvic connecting mechanism. The application of Roussouly Classification for degenerative cases was still controversial, since it was designed for asymptomatic ones. However, its influence still needs to be considered because individual’s value of PI is stable after adolescence.
In Roussouly Type 1 asymptomatic subjects, a large curve of thoraco-lumbar kyphosis accompanies a small lumbar lordosis in the global sagittal spine. Therefore, the C7 plumbline would migrate posteriorly so that the subjects could gaze horizontally, with their heads elevated. And the cervical lordosis compensates the thoraco-lumbar alignment. The lordotic alignment accounted for 60 % in this type, while only 30 % were the straight alignment. Moreover, a similar distribution was found in spondylotic group in spite of its global spine degeneration. A decrease of SSA and similar T1 slope reflected the process of global spine degeneration. However, such a process can be compensated mainly by the increase of angles in C0–C2, even by a minor increase in the general and practical cervical angles. Hence, an increase in cervical lordotic and straight curves was probably the result of a global spine re-alignment occurring to prevent imbalance in patients with cervical spondylosis, Nevertheless, the T1 slope and distribution of cervical alignment were similar in both cohorts in Type 1, which may be due to their smaller PI and thoraco-lumbar kyphosis. Meanwhile, we found that the larger intervertebral angles were more liable to degenerate. With the modification of inner mechanical environment in intervertebral discs, the space below the apex of cervical lordosis, like at C5–6 and at C6–7, of which the overall degeneration rate was 64 %, would be influenced by the shear forces of disc–end plate interface. However, would this mechanism also work in Type 2?
In Roussouly Type 2 asymptomatic subjects, their smallest angles in thoracic kyphosis (TK) and lumbar lordosis form a “flat back”. And the cervical spine inherits the same character as an extension of global spine alignment derived from pelvis, transferring the vertical forces cranially and became straight in general. Therefore, the number of straight and kyphotic alignments increased by 38.1 and 31 %, respectively compared with Type 1. The results also showed, for the cervical spondylotic patients, there was a higher percentage of straight alignment (from 38.1 to 50 %) and lower of kyphotic alignment (from 31 to 15.4 %) than those for asymptomatic subjects, which could be deemed as a demand of horizontal gazing while global spine degeneration was forming. The significant declines of SSA and Hip to C7/hip to sacrum reflect the global spine degeneration. However, T1 slope seems to maintain intact between asymptomatic and spondylotic subjects. Therefore, the cervical spine has to increase the angles of lordosis to keep gazing horizontally. The significant increase of intervertebral angles in C45 and C56 in spondylotic cohorts explained its slight increase of practical cervical angles. Moreover, the largest increase of C0–C2 angle was thought to compensate the global cervical alignment that rarely changed in cervical spondylotic patients compared to other types. Which force play the fundamental role in such degeneration, shear force or vertical force? Roussouly et al. reported that the vertical weight force decides the degeneration in thoracic and lumbar spine in Type 2 due to its smaller PI value. According to the disc angles in asymptomatic subjects and degenerative levels in spondylotic patients, the degeneration distributed evenly among cervical levels, which is different from the distribution in Type 1. Therefore, the vertical forces are likely to lead to the degeneration.
In Roussouly Type 3, a well-balanced global spine alignment in thoracic and lumbar curves does not need a lordotic cervical curve for physiological (horizontal) gaze. Hence, the percentage of kyphosis ones reached 26.2 %. To some extent, the degeneration of cervical spine in Type 3 is similar to Type 2 due to their straight spinal alignment in general. The similar distribution of degenerative levels supported our deduction. Whereas considering the decrease of straight cervical alignment from 64.3 % in asymptomatic subjects to 58.2 % in patients with cervical spondylosis, the bio-mechanism of the two types seems different. The significant decrease of C67 and the most common degenerative levels in C45 among types could explain such a phenomenon. Furthermore, the percentage of lordosis increased from 9.5 % in asymptomatic subjects to 18.2 % in cervical spondylotic patients, which could be associated with the increase of practical cervical angles. A decrease of Hip to C7/hip to sacrum and T1 slope represent the general degeneration of the spine, which might demand a larger cervical lordosis to compensate to horizontal gaze in daily life. Consequently, the C0–C2 angle plays a role in such a process.
In Roussouly Type 4, the lordotic alignment was the majority in both asymptomatic subjects and cervical spondylotic patients, no matter the global spine degeneration occurred or not. Moreover, the percentage of the lordotic alignment in patients with cervical spondylosis reached 88.2 % compared with 62.5 % in asymptomatic ones. And hypolordosis, including kyphosis, straight and sigmoid, was rare, which suggests the larger curves they have in lumbar lordosis and TK, the larger lordosis they need in cervical spine in spite of the degenerating in global spine. The degeneration levels concentrated at C56 and C67, occupying 85 %, which was similar to Type 1, suggesting their similar mechanism during degeneration. The cervical angles still increased significantly in spondylotic cohort even with an increase in C0–C2 angle, which proposes a trend in aging process. And similar SSA value in this type suggests that there should be a larger range of self-adjustment of the gravity line above the pelvis without any version in degeneration.
The relationship between cervical angles and other parameters
The results of Logistic Regression, both the general and practical cervical angles correlated with TK positively, with T1 slope positively and with C0–C2 angles negatively. Matsunaga et al. [12] reported that C0–C2 angles in healthy volunteers were around 22° in women and 16° in men at the age of 30s, and decreased gradually in people more than 40 years in both sexes. However, the C0–C2 angles in our spondylotic cohort had a tendency of increasing and correlated negatively with cervical angles, which suggest that an increase of C0–C2 might accompany a decrease of cervical angles. This was supported in General angles in Type 2 and 3. Therefore, the general cervical angles could only be a rough predictor rather than a precise one, like the practical angle, in the assessment of alignment. As for the T1 slope, Knott et al. [13] reported that the T1 slope had the strongest correlation with the global spine balance and patients had at least 10 cm of positive sagittal imbalance with its value larger than 25° and a negative sagittal balance with its value less than 13°. In our cohort, the cervical spondylotic patients were still in well balance despite their values beyond the upper limits. The significant differences in T1 slope among lordotic, straight and kyphotic alignments in asymptomatic cohort suggest a strong capability of adjustment in intervertebral discs for these curves. However, with the disc degeneration, kyphotic alignment is likely to increase the tilt of the T1 vertebral body to maintain their horizontal gazing. Nevertheless, the degree of modification in straight alignments was lower than that in kyphotic ones. And all these modifications are accompanied by their variations of TK. As far as the TK is concerned, it is reported that cervical lordosis correlates with TK and lumbar lordosis; it increases slightly with age [4]. Our research found that the cervical angles were related to thoracic angles, but not with the lumbar angles, which was contrary to the previous researches [15]. Besides, the values of SSA were similar to those in asymptomatic subjects, as an average of 130.4° among those under 30 years; and 131.7° in their 50s and 127.9° in their 60s [16]. As is well known, the positive values of Hip to C7/hip to sacrum implied that the center of C7 vertebral body always located behind both the hip axis and sacrum, which was considered as a balanced spino-pelvic relationship [16]. In our research, decreased values, especially in Roussouly Type 2 and 3 in spondylotic cohort, were found, which suggested that the C7 vertebral body approached sacrum in vertical axis. However, no complaint of back pain was found. This phenomenon reminded us that the cervical pathology was usually accompanied by the global spine degeneration, but rarely influenced the sacro-pelvic morphology [17].
In summary, we conclude the cervical alignment is more liable to be influenced by the local parameters as an independent degenerative disease but is seldom influenced by the global spinal degeneration.
As for the limitation of this article, the lack of longitudinal research is a problem that we could not avoid. Moreover, the clinical follow-up of the modification in cervical spine is summarized in our coming publication with a minimum 2-year observation.
Notes
Consent was obtained from each subject or patient with the approval from Peking University Third Hospital Institutional Review Board.
References
Gore DR, Sepic SB, Gardner GM (1986) Roentgenographic findings of the cervical spine in asymptomatic people. Spine 11:521–524
Kasai T, Ikata T, Katoh S et al (1996) Growth of the cervical spine with special reference to its lordosis and mobility. Spine 21(18):2067–2073
Harrison DD, Troyanovich SJ, Harrison DE et al (1996) A normal sagittal spinal configuration: a desirable clinical outcome. J Manipulative Physiol Ther 19:398–405
Lee CS, Noh H, Lee DH et al (2012) Analysis of sagittal spinal alignment in 181 asymptomatic children. J Spinal Disord Tech 25(8):E259–E263
Hardacker JW, Shuford RF, Capicotto PN et al (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 22:1472–1480
Boyle J, Milne N, Singer K (2002) Influence of age on cervicothoracic spinal curvature: an ex vivo radiographic surgery. Clin Biomech 17:361–371
Mac-Thiong JM, Labelle H, Charlebois M (2003) Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 28(13):1404–1409
Roussouly P, Gollogly S, Berthonnaud E et al (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30(3):346–353
Legaye J, Duval-Beaupere G, Hecquet J et al (1998) Pelvic incidence: a fundamental parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2):99–103
Roussouly P, Gollogly S, Noseda O et al (2006) The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line. A radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 31(11):E320–E325
Barrey C, Jund J, Noseda O et al (2007) Sagittal balance of the pelvis-spine complex and lumbar degenerative disease. A comparative study about 85 cases. Eur Spine J 16(9):1459–1467
Matsunaga S, Onishi T, Sakou T (2001) Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine 26(2):161–165
Knott PT, Mardjetko SM, Techy F (2010) The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J 10:994–998
Ohara A, Miyamoto K, Naganwa T et al (2006) Reliabilities of and correlations among five standard methods of assessing the sagittal alignment of the cervical spine. Spine 31(22):2585–2591
Park MS, Moon SH, Lee HM et al (2013) The effect of age on cervical sagittal alignment normative data on 100 asymptomatic subjects. Spine 38(8):E458–E463
Mac-Thiong J.M., Roussouly P, Berthonnaud E et al (2010) Sagittal parameters of global spinal balance normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adult. Spine 35(22):E1193–1198
Gore DR (2001) Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine 26(22):2463–2466
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, M., Zhao, WK., Li, M. et al. Analysis of cervical and global spine alignment under Roussouly sagittal classification in Chinese cervical spondylotic patients and asymptomatic subjects. Eur Spine J 24, 1265–1273 (2015). https://doi.org/10.1007/s00586-015-3832-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-015-3832-2