Abstract
This review provides a comprehensive exploration of factors contributing to sudden death (SD) in ruminants, focusing on cattle, sheep, and goats. The definition of unexpected death varies based on the farming system. In intensive systems, constant surveillance enables rapid detection of diseases, while in extensive systems, irregular checks may result in finding animals dead after a prolonged illness. SD syndrome definitions vary; some involve clear clinical signs, while others consider acute death in apparently healthy animals. Various infectious causes of SD are discussed, including enterotoxemia, hemorrhagic bowel syndrome, caudal vena cava thrombosis, and respiratory diseases. The review also covers nutritional disorders like acidosis, hypomagnesemia, and vitamin deficiencies. Poisoning, both from inappropriate drug use and toxic plants, is examined, as well as accidents and trauma, parasitism, stress, and miscellaneous causes such as aortic aneurysm rupture, congenital defects, and snakebites. Differential diagnosis is emphasized, and the importance of post-mortem examinations in understanding the cause of unexpected deaths is highlighted. The paper offers a detailed overview of the complex factors contributing to SD in ruminants, emphasizing the need for thorough investigations and necropsy examinations to identify the specific cause in each case.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The definition of unexpected death in ruminants varies depending on the individual approach and farming system type. In intensive industrial systems (such as dairy herds and feedlots), animals are under constant surveillance, which enables rapid detection of even peracute diseases. However, in extensive sedentary and transhumance systems, routine herd controls are irregular and infrequent, resulting in animals being found dead after a long period of illness, which may involve sub-acute or even chronic diseases that culminate in the perception of SD. The definition of SD syndrome remains ambiguous among authors, certain involve cases of animals that showed more or less obvious clinical signs before death (Lincoln 2012; Plumlee 2003) while others only consider an acute death of an animal apparently in good health (Anscombe 2016; Kelly 2003).
Studies of ruminant pathology suggest that the most common causes of SD are acute infectious diseases, digestive disorders, and nutritional deficiencies, but a number of cases of SD have been attributed to fatal poisonings, accidents, and certain parasitic agents.
This review aims to explore various factors that may contribute to SD in cattle, sheep, and goats. The paper highlights diseases that can manifest with clinical symptoms and their associated signs and etiopathogenesis. Additionally, particular attention is paid to the role of necropsy diagnosis in identifying the cause of SD in ruminants.
Causes of sudden death in ruminants
Infectious etiology
Enterotoxemia
The term “enterotoxemia” was initially used to describe diseases caused by certain strains of Clostridium perfringens (Simpson et al. 2018). Enterotoxemia can be acute or peracute, and is a well-recognized cause of SD in what was otherwise considered to be very healthy animals (Lebrun et al. 2010). Recent investigations have reported that C. perfringens toxinotypes (A, B, C, D, and E) produce lethal toxins that can cause SD in ruminants (Fahimeh et al. 2018; Redondo et al. 2013; Simpson et al. 2018). Clostridia pathogen strains induce syndromes that can be classified as enteric, neurotoxic, and histotoxic (Santos et al. 2019). However, animals can die from enterotoxemia due to a single disorder or a combination of several syndromes (Simpson et al. 2018; Uzal et al. 2014). Toxemia is induced by the systemic spread of toxins in blood and to tissues, leading to intravascular hemolysis and capillary damage, as well as hepatic necrosis and cardiac effects (Lebrun et al. 2010; Uzal and Songer 2008). Furthermore, several other strains of the histotoxic Clostridium genus are involved in SD syndrome in cattle and sheep (Abbott 2018). Infections with histotoxic clostridia occur when wounds are contaminated with spores or vegetative forms; however, toxemia occurs when the toxins enter the bloodstream, resulting in shock and death (Junior et al. 2020). SD with severe hemorrhagic jejunitis and hemorrhagic intestinal contents observed at postmortem inspection is suggestive of clostridial enterotoxemia. Additionally, rapid putrefaction of the abdominal viscera with gas and putrid odor is characteristic of clostridial enterotoxemia (Lebrun et al. 2010). However, clinical, epidemiological, necropsy, and histological findings are essential for the accurate diagnosis of clostridial SD (Santos et al. 2019).
Hemorrhagic bowel syndrome (HBS), also known as jejunal hematoma syndrome, primarily occurs in adult cattle, with most clinical cases reported in dairy cows (Abutarbush and Radostits 2005; Kalender et al. 2007). HBS is an acute enteric disease that often occurs within the first 3 to 4 months of the lactation period (Underwood et al. 2015). The underlying causes are not well-known, but the most commonly discussed potential cause is infection with C. perfringens type A (Adaska et al. 2014; Simpson et al. 2018). Thus, it has been proposed that linked alpha and beta2 toxins may have a role in the occurrence of the disease; further, the implication of certain mycotoxins in the appearance in HBS has been reported (Mamak and Börkü 2019). Healthy cows affected by HBS can be found dead without prodromal signs. During necropsies, notable lesions include intestinal hemorrhage and ulceration (Kalender et al. 2007).
Caudal vena cava thrombosis (CVCT)
The most frequent cause of vena cava thrombosis in cattle is liver abscess rupture (Schild et al. 2017). Abscesses form in the liver due to the dissemination of bacteria from the rumen secondary to inflammation in the ruminal wall (Motta et al. 2016). Bacteria from the abscess can travel to the vena cava, causing septic thrombosis, and from there, septic emboli dislodge and are carried to and lodge in the pulmonary capillaries (Miller and Gal 2017). As a result, acute death occurs after a septic shock with evident hemoptysis after episodes of acute pulmonary hemorrhage (Motta et al. 2016). As well as a large septic thrombus may cause enough direct pulmonary infarction or a septic myocarditis leading to heart failure (Peek and Divers 2018). The most frequent pathogens isolated from liver abscesses are Fusobacterium necrophorum and Trueperella (Arcanobacterium) Pyogenes pyogenes (Motta et al. 2016; Nagaraja and Lechtenberg 2007).
Though, emboli may come from inflammatory processes such as deep digital sepsis, mastitis, or metritis and result in CVCT (Braun 2008; Schild et al. 2017); also, this process has been reported in acute rupture of reticuloperitonitis abscess (Gerspach et al. 2011). The diagnosis of CVCT requires careful necropsy when SD results and, in general, affected animals have appeared completely healthy before death (Peek and Divers 2018).
Infectious respiratory diseases
Glock and Degroot (1998) estimated that respiratory disease accounted for 47% of SDs in ruminants, highlighting its importance. Shipping fever complex, a type of acute pneumonia, is the most prevalent cause of SD (Glock and DeGroot 1998; Peek and Divers 2018). Pasteurella multocida and Mannheimia haemolytica are two common pathogens associated with pneumonia and septicemia in all ruminants, causing pasteurellosis; a bacterial disease characterized by bronchopneumonia, septicemia, and SD (Underwood et al. 2015). Mannheimia haemolytica, formerly known as Pasteurella haemolytica A1, is particularly associated with SD in sheep (Gilmour 1980) and can also cause septicemia in young lambs and kids (Brogden et al. 1998). Moreover, high mortality rates have been reported in cattle with acute pneumonia caused by Bibersteinia trehalosi (Cortese et al. 2012).
Histophilus spp. has also been associated with respiratory disease in sheep and goats, with death being typically the first sign of Histophilus somni pneumonia. Death can result from septicemia and thromboembolic meningoencephalitis (Underwood et al. 2015). Additionally, the acute form of bovine respiratory syncytial virus (BRSV) infection has been reported as responsible for SD in severe cases (Scott et al. 2011). Bovine herpesvirus 5 (BoHV-5) is frequently associated with neurological disease and SD in young calves within 18 h of infection course (Lunardi et al. 2009). In goat herds, Mycoplasma mycoides subspecies capri or Mycoplasma mycoides subspecies mycoides has been found to cause high mortality rates (Debien et al. 2013).
Other infectious etiologies
Bacillus anthracis is the causative agent of anthrax or splenic fever. Sudden unexplained death is most commonly seen in grazing herbivore in contaminated vegetation or soil by Bacillus anthracis spores (Rao et al. 2019). Affected animals have nasal, oral, and anal or vulva hemorrhage (dark blood) and a few cases are ataxic in terminal septicemia (Abbott 2018; Blowey and Weaver 2011; Fasanella et al. 2010). Heartwater (cowdriosis) is one the most important tick-borne diseases of domestic ruminants in southern Africa, and it is caused by Cowdria ruminantium (Van de Pypekamp and Prozesky 1987). Fulminating fever in an apparently healthy animal is the main symptom, followed by paroxysmal convulsions, respiratory difficulties, and rapid collapse; however, it is often fatal and both goat and sheep may die suddenly (Van de Pypekamp and Prozesky 1987; Yunker 1996). Coliforms seem to be responsible for anaphylactic shock and SD (Andrews et al. 2008; Owens et al. 1998). Coliform septicemia is a disease that affects cattle, goats, and lambs and can cause SD in lambs under the age of 10 days (Pohl et al. 1993). Peracute toxic coliform mastitis, which occurs during the peripartum period or early lactation, can occasionally cause cow death, and many deaths related to endotoxic mastitis are likely due to disseminated intravascular coagulation (DIC) (Stalberger and Kersting 1988). In newborns, toxemia associated with particular pathogens, especially E. coli, are important causes of SD (Radostits et al. 2006). Listeria monocytogenes is the most common cause of bacterial infection affecting the central nervous system. Goats appear to be more sensitive to this infection than cattle or sheep, and neonatal listeriosis can lead to SD in 2- to 4-day-old calves (Blowey and Weaver 2011; Debien et al. 2013).
Foot-and-mouth disease (FMD), caused by an RNA Picornavirus of the genus Aphthovirus, is a highly contagious disease that is difficult to diagnose in sheep due to its subacute form. In very young animals, the virus can infect the myocardium, leading to SD (Ryan et al. 2008).
Malignant catarrhal fever is a severe disease caused by bovine herpesvirus 6 (BoHV-6) that mostly affects cattle and can lead to SD (Stanitznig and Wittek 2018; Underwood et al. 2015).
Nutritionals disorders
Acute and peracute acidosis
Acute and peracute acidosis have been associated with high-concentrate feeding regimes and production diseases such as SD in feedlot steers (Andersen 2003). SD usually occurs near the end of finishing without any signs of disease (Wilson et al. 1975). According to a study by Malafaia et al. (2016), a high level of lactate (9.13 mmol/L blood) in fattening cattle is considered dangerous as it can cause systemic metabolic acidosis (Malafaia et al. 2016). Endotoxemia is also considered an important factor in follow-on systemic metabolic acidosis leading to SD (Andersen 2003).
Red gut
Red gut is a fatal intestinal accident that can rapidly lead to death in weaned lambs and adult sheep, this condition may mostly occur in lush pastures (Abbott 2018); usually, lucerne (Barrell et al. 1989); white clover and ryegrass (Gumbrell 1997).
High intake of digestible forage leads to a reduction in rumenoreticulum and an increase in intestinal mass, which becomes mobile. Accidental twisting of the intestines occurs as a result of this mobility, leading to obstruction of the mesenteric blood vessels, causing death from shock (Barrell et al. 1989; Gumbrell 1997). Autopsy reveals an intense reddened or dark red intestinal mass, often displaced in the anterior abdominal cavity (Gumbrell 1997).
Hypomagnesemia
Hypomagnesemia is one of the differential diagnoses that should be considered in SD in cattle and sheep (Doncel et al. 2021). It is a biochemical disorder characterized by low serum magnesium (< 0.7 mmol/L) (Chevalier et al. 2012). The risk of hypomagnesemia increases when the diet is low in Mg and high in K, primarily in fast-growing lush grasses (Doncel et al. 2019). Clinical signs may be absent, and abrupt high mortality rates on pasture may be observed (Doncel et al. 2019). Like many metabolic disorders, hypomagnesemia can cause seizures responsible for SD in calves (Chevalier et al. 2012) and a certain diagnosis is only possible after biochemical investigation (Doncel et al. 2021).
Vitamin E and selenium deficits
Selenium deficiency, also known as white muscle disease, is often associated with a lack of vitamin E and can cause paresis and SD, particularly in neonatal ruminants (Underwood et al. 2015). Calves are often born dead or die shortly after birth due to a congenital deficiency form (Davis and Myburgh 2016). Abbott (2018) stated that selenium deficiency can cause cardiac myopathy syndrome, which is liable to SD (Abbott 2018).
Vitamin B1 deficiency
Vitamin B1 deficiency can cause polioencephalomalacia (PEM) in ruminants; the disease can be peracute and lead to death (Jean-Blain and de Oliveira 1994). Animals are at risk when their diet contains thiaminases or when their feed or water is high in sulfates (Underwood et al. 2015). Major clinical signs of the disease in young dairy calves include incoordination, convulsions, and head retraction (Karapinar et al. 2010).
Poisoning
Toxic plants
While there are only a few poisonous plants that cause SD without predictive signs (King 1983), several plants can produce poisoning severe enough to cause death within 12 h (Burrows and Tyrl 1989). Certain cardiotoxic poisonous plants have been associated with the consumption of many species of the genera Palicourea, Arrabidaea and Amorimia, Pseudocalymma, Elegans, Nerium Oleander (Lima et al. 2019; Soares et al. 2011), and Gossypol (Plumlee 2003). Nitrate/nitrite poisoning, followed by gossypol, oleander, and pyrrolizidine alkaloids, accounted for most plant-associated poisonings (Varga and Puschner 2012). Poisonous plant consumption is one of the most common causes of SD in African livestock, according to Anaeto et al. (2009), with cyanogenic plants and yew being the most rapidly lethal (Anaeto et al. 2009; Burrows and Tyrl 1989). Traditional medicine can also lead to inappropriate dosing of herbal medicines, such as C. occidentalis (Nalule et al. 2011). Sorghums are among the most dangerous crops, as cyanide can be released during chewing and in the rumen or abomasum, leading to rapid intoxication (Burrows and Tyrl 1989). The entire oleander plant, whether fresh or dried, is poisonous, and just five to ten leaves can be fatal to adult cattle (Ceci et al. 2020) within 2–8 h (Varga and Puschner 2012). Gossypol intoxication causes myocardial necrosis in young ruminants. The cardiotoxic effects are gradual destruction of the heart muscle and interference with the conduction system (Plumlee 2003). However, it should be noted that poisoning by plants rich in cyanogenic glycosides can cause disorders similar to certain fatal nervous diseases (KAzI TAnI 2014), which can make diagnosis problematic. Ingestion of large amounts of oxalis causes severe hypocalcemia, central nervous system depression, and death from cardiovascular collapse (Mohammedi et al. 2014).
Monofluoroacetate (MFA) is a deadly toxic component of some plants and causes SD in livestock; of these, Amorimia pubiflora, which contains high concentration of AMF and cause fatal poisoning at all vegetative stages (Lima et al. 2019).
Nitrate poisoning is a serious problem only in ruminants. Plants that accumulate nitrates, such as sorghum, can cause SD (Burrows and Tyrl 1989). Similarly, cabbage plants and fertilizers are potential sources of nitrates (Scott et al. 2011). White sweet clover and yellow sweet clover produce the hemorrhagic syndrome (Burrows and Tyrl 1989). Nitrite is responsible for tissue anoxia by converting hemoglobin to methemoglobin (Scott et al. 2011; Varga and Puschner 2012). Further, non-protein nitrogen (NPN) (e.g., urea) induces ammonia toxicosis, with a rapid onset of clinical signs and SD (Peek and Divers 2018). The peracute death of lambs from ammonia poisoning may erroneously suggest clostridial enterotoxemia (Plumlee 2003).
Taxus baccata (European yew) causes SD from acute cardiac arrest and diagnosis is based on the detection of alkaloids in the liver, urine, or blood (Cortinovis and Caloni 2015).
Conium maculatum (hemlock) is one of the most toxic members of the plant kingdom and Hemlock alkaloids cause central nervous system depression in livestock (Vetter 2004).
Agricultural chemicals
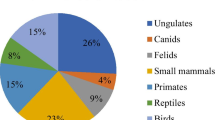
Chemicals such as insecticides, herbicides, and rodenticides can also be toxic to animals (Delano et al. 2002). According to Caloni et al. (2018), pesticides were the leading cause of poisoning in Europe from 2010 to 2016 in most species (Caloni et al. 2018). Among ruminants, cattle are the species most frequently exposed to poisoning due to their undemanding feeding behavior (Cowan and Blakley 2016).
Metalloids
Sulfur poisoning in ruminants can cause polioencephalomalacia (PEM), which is characterized by brain damage (De Sant’Ana and Barros 2010). PEM is primarily caused by a thiamine deficiency, as mentioned earlier. Acute arsenic toxicosis occurs when livestock have access to old and waste materials containing arsenic, often in combination with chromium or lead and the primary clinical outcome is SD (Bertin et al. 2013).
Cattle are more susceptible to lead poisoning than other ruminant species (Caloni et al. 2018). Neurological dysfunction and respiratory failure can lead to death within 24 h (Cowan and Blakley 2016). When the clinical signs are overlooked lead poisoning can result in SD and cattle may be found down or dead-on pasture (Bates and Payne 2017). Excessive exposure to copper can lead to high mortality, with death occurring within 12 to 72 h. Acute clinical signs of copper overdose include diarrhea and central nervous system disorders, shortness of breath, and depression (Varga and Puschner 2012). In rare cases, water intoxication has been reported in sheep, leading to acute deaths resulting from the consumption of large quantities of water after several days of deprivation (Abd-Elrahman et al. 2020).
Accident and trauma
Mortality due to trauma and accidents can be high in calves and young stock in beef cattle (Mõtus et al. 2017). Generally, sheep handling is safe; however in certain practices, such as shearing, accidental wounding resulting in lethal outcomes has been reported (Irandoust et al. 2013). A rupture of the small intestine can lead to rapid deterioration and often manifests itself in SD, similar situation is observed in newborn calves trampled by adult animals. Alike, a rectal laceration can result in SD from an abrupt rectal touch; a tear in the thickness of the rectal mucosa can result in fatal septic peritonitis within 24 h (Peek and Divers 2018). During investigations, veterinarians should not exclude the possibility of criminal intent, especially following suspicious death cases (Archibald and Smith 1965).
Bloat
Bloat is a common cause of SD in cattle due to physical obstruction by a foreign object in the alimentary body or esophagus. Gas is trapped in the rumen, causing acute free-gas bloat. Bloat occurs as well in pastured beef cattle and feedlot cattle, due to the production of a large amount of stable foam (Galyean and Rivera 2003; Radostits et al. 2006). When the bloat becomes severe enough, death is likely caused by suffocation when the distended rumen pushes against the diaphragm and stops breathing (Majak et al. 2003).
Traumatic reticuloperitonitis
Hardware disease is primarily a disease of cattle and is rarely seen in smaller ruminants (Underwood et al. 2015). SD can occur due to heart failure (Buczinski et al. 2010) or by fatal hemorrhage when metal wire migrates and punctures the heart coronary vessels or other large vessels like the reticular vein (Radostits et al. 2006).
Perforated abomasal ulcer
SD may occur in dairy cattle with perforated abomasal ulcer and death usually occurs in 48–96 h from shock and dehydration (Andrews et al. 2008; Radostits et al. 2006).
Electrical injuries
The accidental contact with electrical currents can cause instantaneous death in grazing animals. This is due to the disruption of neural regulatory impulses or heart failure (Schulze et al. 2016). Dead animals may be found with fresh food in their mouth and scorch marks of burned hair on their coat, especially the legs (Blowey and Weaver 2011).
Inhalation pneumonia
The major cause of pulmonary aspiration in cattle is the inhalation of foreign material into the larynx and then the lower airway. The aspiration of a significant amount of liquid or solid material can lead to instant death due to mechanical asphyxiation (Shakespeare 2012). Inhalation pneumonia may also result following hypocalcaemia, especially if the cow becomes cast, during general anesthesia, and after the faulty administration of drenches (Scott et al. 2011).
Parasitism
Haemonchus contortus is sometimes associated with SD in sheep, particularly in cases of hyperacute haemonchosis, which is due to a heavy Haemonchus species infection (20,000–30,000 worms) (Besier et al. 2016; Gebresilassie and Afera Tadele 2015). Clinical signs of acute disease are anemia, dark-colored feces, edema “bottle jaw,” and weakness (Besier et al. 2016; Roeber et al. 2013). Acute visceral cysticercosis mainly affects lambs and goat kids and can cause SD without premonitory signs. It has been very sporadically cited in calves (Koutsoumpas et al. 2013). Echinococcus spp. is the causal agent of hydatid cysts, the rupturing of the cysts can result in pulmonary artery embolism and SD due to massive giant pulmonary artery embolism (Bayaroğullari et al. 2013). In young calves during the first month of their lives, a hyper infestation with Strongyloides papillosus worms can be fatal (Kváč and Vítovec 2007). Dictyocaulus viviparus is a lungworm that can be responsible for SD in severely affected growing cattle under severe challenge. In feedlot steers, death can occur suddenly in animals without exhibiting signs of clinical illness (Scott et al. 2011). Cysts containing Fascioloides magna found in the liver and lung can liberate flukes that involve fatal pulmonary hemorrhage (Wobeser and Schumann 2014).
SDs caused by trypanosomiasis have been reported in small ruminants. An acute hemorrhagic syndrome has also been seen sporadically in cattle infected with some isolates of T. vivax, mostly in East Africa, the syndrome can be rapidly fatal (Spickler 2018). SD may also occur with Babesia bovis and Babesia bigeminia infection in cattle (Underwood et al. 2015).
Stress
In newborn calves, the threat of mortality increases following difficult parturition and adverse climatic conditions. In cold environments, hypothermia often occurs and may cause the death of weaker calves (Roland et al. 2016; Vermorel et al. 1983). According to Cox et al. (2016), heat stress is not only specific to young animals; significant cold- and heat-related increases in dairy cattle mortality have been observed. Farm animals, such as cattle, are known to suffer from temperature extremes (Cox et al. 2016). For some authors, high on-farm mortality is seen as a potential indicator of poor cow welfare (Sarjokari et al. 2018). Moreover, Vitali et al. (2015) established a link between cow age, temperature, and death (Vitali et al. 2015). Older dairy cows (5 to 8 years) are at high risk of death following exposure to long heat waves (> 11 days), likely with a high humidity index (Vitali et al. 2015).
SD is likely caused by severe stress during the transport of animals over long distances, in poor conditions or high stocking densities in pens, and a diet that is high in grain and low in fiber (Malafaia et al. 2016). Severe stress conditions can cause SD in lambs, even without diarrhea (King 1983).
Other causes of SD
The occurrence of aortic aneurysm rupture in goats, sheep, and cattle is sporadic and must be considered a significant cause of SD (Souto et al. 2017). Most animals are reported as being found dead, but those seen alive often show a sudden reduction in milk yield, with colic and recumbency preceding a rapid death (Crawshaw et al. 2011). Hereditary defects in fibrillin metabolism, known as Bovine Marfan syndrome, have been identified as potential causes of aneurysm formation in cattle (Potter and Besser 1994), especially in mature female of Holsteins breed (Lamm et al. 2007). Obstruction by hematoma of the aortic lumen or an aortic branch may result in acute myocardial infarction and SD (Amalinei and Căruntu 2013).
In newborns, congenital defects that are incompatible with life, prematurity, septicemia due to poor immune status, and hypothyroidism are important causes of SD (Radostits et al. 2006). Similarly, SD has been associated with frequent congenital heart disease in calves (Buczinski et al. 2010). In dairy calves, acute heart failure related to the anticipation of milk feeding has been reported and death may occur during feeding or immediately after, but the exact pathophysiology remains unknown (Jones 2014). In African livestock, snakebites are among the most commonly cited causes of SD. In species with only neurotoxic venom, the signs may be limited to puncture wounds and neurological deficits (Anaeto et al. 2009). Peracute death following snakebite is due to cardiovascular troubles leading to cardiac arrest (Plumlee 2003).
Differential diagnosis
SD in ruminants is a complex syndrome that can result from multiple factors interacting simultaneously, making diagnosis challenging. When causal factors are related to each other, it can pose a problem for both clinical and necropsy diagnosis, and the pathogenesis cannot be clearly defined (e.g., acidosis, acute pneumonia, and enterotoxemia). The diagnosis of SD in ruminants must involve two steps: first, investigation of the herd, including careful observation of the remaining animals for signs of acute clinical disease, which may provide key diagnostic information; second, individual post-mortem examination and autopsy of the deceased animal. The primary reasons for conducting post-mortem examinations on domestic animals are typically to determine the cause of unexplained individual animal deaths or sudden increases in herd mortality rates (Wäsle et al. 2017). Stockholders often expect a dramatic post-mortem result and clear instructions on how to prevent further losses after a tragic event such as SD (Kelly 2003). For veterinary investigators, a careful history and a prompt post-mortem examination can provide valuable diagnostic information in most cases of unexpected ruminant death (Pierson et al. 1976). If the animals really have died quickly, with no signs being observed, some assumptions about the necropsy findings may be made (Table 1). Most importantly, many of the pathological findings are likely to be unspectacular and nonspecific (Kelly 2003). In the case of infectious or toxic causes, the main objective of the necropsy examination is to collect and process samples for further examination (Wäsle et al. 2017).
Conclusion
The diagnosis of SD in ruminants is challenging. Multiple factors are involved and several causes may be present simultaneously. In addition, diagnosis can be further complicated by variability in husbandry systems and intervals between herd visits. The definitions provided by Kelly (2003) and Anscombe (2016), “an acute death of an animal or the discovery of dead, well-fed, non-perinatal animals within two days of observation, apparently in good health” and “the sudden and unexpected death of an apparently healthy animal,” respectively, appear to be the most appropriate for SD syndrome in ruminants (Anscombe 2016; Kelly 2003). Similarly, in human medicine, there is no universally accepted definition of SD, but it is generally used to refer to deaths not preceded by significant symptoms (Sessa et al. 2021). The relevant definition of SD syndrome would be the sudden and unexpected death of an apparently healthy animal, excluding cases of loss due to diseases with obvious clinical signs. This means that livestock farmers must adopt modern means of control to better monitor herds, such as video surveillance and the widespread use of electronic chips to quickly identify sick animals and know the conditions in which sudden death occurred.
References
Abbott K (2018) The practice of sheep veterinary medicine. University of Adelaide Press
Abd-Elrahman AH et al (2020) The first identification of contagious caprine pleuropneumonia (CCPP) in sheep and goats in Egypt: molecular and pathological characterization. Trop Anim Health Prod 52(3):1179–1186
Abutarbush SM, Radostits OM (2005) Jejunal hemorrhage syndrome in dairy and beef cattle: 11 cases (2001 to 2003). Can Vet J 46(8):711
Adaska JM et al (2014) Jejunal hematoma in cattle: a retrospective case analysis. J Vet Diagn Invest 26(1):96–103
Amalinei C, Căruntu I-D (2013) Etiology and pathogenesis of aortic aneurysm. Aortic Aneurysm-Recent Advances. IntechOpen
Anaeto M et al (2009) Health and nutrition practices among smallholder sheep and goat farmers in Ogun State Nigeria. Livestock Res Rural Dev 21(11)
Andersen PH (2003) Bovine endotoxicosis–some aspects of relevance to production diseases. A review`. Acta Vet Scand 44(1):1–15
Andrews AH et al (2008) Bovine medicine: diseases and husbandry of cattle. John Wiley & Sons
Anscombe J (2016) How to investigate sudden death. Vet J 4(2):43–46
Archibald RM, Smith H (1965) Sudden death in cattle with an unusual cause. Can Vet J 6(5):121
Barrell GK, Gumbrell RC, Reid TC (1989) Artificial induction of red gut in sheep. Res Vet Sci 46:318–321
Bates N, Payne J (2017) Risk assessment and risk management of poisoning in farm animals. Livestock 22(3):146–149
Bayaroğullari H et al (2013) Liver hydatid cyst leading to bilateral pulmonary artery embolism and bilateral multiple pulmonar echinococcosis via inferior vena cava: report of a case. Clin Imaging 37(2):374–378
Bertin F et al (2013) Arsenic toxicosis in cattle: meta-analysis of 156 cases. J Vet Intern Med 27(4):977–981
Besier R et al (2016) Diagnosis, treatment and management of Haemonchus contortus in small ruminants. Adv Parasitol 93:181–238
Blowey R, Weaver AD (2011) Color Atlas of diseases and disorders of cattle e-book. Elsevier Health Sciences
Braun U (2008) Clinical findings and diagnosis of thrombosis of the caudal vena cava in cattle. Vet J 175(1):118–125
Brogden KA et al (1998) Pasteurella haemolytica complicated respiratory infections in sheep and goats. Vet Res 29(3–4):233–254
Buczinski S et al (2010) Heart disease in cattle: diagnosis, therapeutic approaches and prognosis. Vet J 184(3):258–263
Burrows GE, Tyrl RJ (1989) Plants causing sudden death in livestock. Vet Clin N Am Food Anim Pract 5(2):263–289
Caloni F et al (2018) Epidemiology of animal poisonings in Europe. Veterinary toxicology, 3rd edn. Elsevier, pp 45–56
Ceci L et al (2020) Outbreak of oleander (Nerium oleander) poisoning in dairy cattle: clinical and food safety implications. Toxins 12(8):471
Chevalier M et al (2012) Investigation of sudden death of calves after epileptic seizures due to hypomagnesaemia and hyperparathyroidism. Revista Portuguesa de Buiatria (Special Edition)
Cortese VS et al (2012) Case report: peracute to acute fatal pneumonia in cattle caused by Bibersteinia trehalosi. The Bovine Practitioner 46(2):138–142
Cortinovis C, Caloni F (2015) Alkaloid-containing plants poisonous to cattle and horses in Europe. Toxins 7(12):5301–5307
Cowan V, Blakley B (2016) Acute lead poisoning in western Canadian cattle—a 16-year retrospective study of diagnostic case records. Can Vet J 57(4):421
Cox B et al (2016) Mortality related to cold and heat. What do we learn from dairy cattle? Environ Res 149:231–238
Crawshaw T et al (2011) Idiopathic arterial aneurysm/rupture causing sudden death in dairy cattle. Vet Pathol 31:501–509
Davis AJ, Myburgh JG (2016) Investigation of stillbirths, perinatal mortality and weakness in beef calves with low-selenium whole blood concentrations. J S Afr Vet Assoc 87(1):1–6
De Sant’Ana, FJ and Barros, CS, (2010) Polioencephalomalacia in ruminants in Brazil. Braz J Vet Pathology 3(1):70–79
Debien E et al (2013) Proportional mortality: a study of 152 goats submitted for necropsy from 13 goat herds in Quebec, with a special focus on caseous lymphadenitis. Can Vet J 54(6):581
Delano ML et al (2002) Biology and diseases of ruminants: sheep, goats, and cattle. In: Laboratory Animal Medicine pp 519–614
Doncel B et al (2019) Hypomagnesemia in dairy cattle in Uruguay. Pesq Vet Bras 39:564–572
Doncel B et al (2021) Hipomagnesemia em bovinos de corte. Pesq Vet Bras 41(6). https://doi.org/10.1590/1678-5150-PVB-6826
Fahimeh Y et al (2018) Major and minor toxins of Clostridium perfringens isolated from healthy and diseased sheep. Small Rumin Res 168:1–5
Fasanella A et al (2010) Anthrax undervalued zoonosis. Vet Microbiol 140(3–4):318–331
Galyean M, Rivera J (2003) Nutritionally related disorders affecting feedlot cattle. Can J Anim Sci 83(1):13–20
Gebresilassie L, Afera Tadele B (2015) Prevalence of ovine haemonchosis in Wukro, Ethiopia. J Parasitol Res 2015
Gerspach C et al (2011) Thrombosis of the cranial vena cava in a cow with bronchopneumonia and traumatic reticuloperitonitis. Can Vet J 52(11):1228–1231
Gilmour N (1980) Pasteurella haemolytica infections in sheep. Vet Q 2(4):191–198
Glock R, DeGroot B (1998) Sudden death of feedlot cattle. J Anim Sci 76(1):315–319
Gumbrell RC (1997) Redgut in sheep: a disease with twist. N Z Vet J 45(6):217–221
Irandoust S et al (2013) Sheep shearing and sudden death. J Forensic Leg Med 20(8):944–946
Jean-Blain C, de Oliveira LA (1994) Aspects physio-pathologiques de la thiamine (vitamine B1) chez les ruminants. INRA Prod Anim 7(2):71–84
Jones TO (2014) Sudden death of calves related to anticipation of feeding. Vet Rec 174(19):486
Junior CAO et al (2020) Gas gangrene in mammals: a review. J Vet Diagn Invest 32(2):175–183
Kalender H et al (2007) Enterotoxemia in a cow due to Clostridium perfringens type A. Turkish J Vet Anim Sci 31(1):83–84
Karapinar T et al (2010) Thiamine status of feedlot cattle fed a high-concentrate diet. Can Vet J 51(11):1251
KAzI TAnI C (2014) Les plantes dangereuses pour le bétail. Une première synthèse pour la flore d’Algérie. Fourrages (versailles) 217:105–114
Kelly R (2003) Acute systemic conditions: diagnosis and management of sudden death in ruminants. Gross Pathology of Ruminants: 9–11 April 2003, Elizabeth Macarthur Agricultural Institute, Camden, NSW, Australia 350:291
King JM (1983) Sudden death in sheep and goats. The Veterinary Clinics of North America. Large Anim Rev 5(3):701–710
Koutsoumpas A et al (2013) Acute visceral cysticercosis in feed-lot lambs. Rev Med Vet 164(8/9):425–428
Kváč M, Vítovec J (2007) Occurrence of Strongyloides papillosus associated with extensive pulmonary lesions and sudden deaths in calves on a beef farm in a highland area of South Bohemia (Czech Republic). Helminthologia 44(1):10–13
Lamm CG et al (2007) Characterization of rupture of abdominal artery aneurysm in dairy cattle. J Vet Diagn Invest 19(3):273–278
Lebrun M et al (2010) Cattle enterotoxaemia and Clostridium perfringens: description, diagnosis and prophylaxis. Vet Rec 167(1):13–22
Lima SC et al (2019) Toxicity of the different vegetative stages of Amorimia pubiflora to sheep. Toxicon 158:47–50
Lincoln SD (2012) Sudden death in feeder cattle. Cattle Producer’s Handbook Western Beef Resource Committee, 3rd edn. pp 652
Lunardi M et al (2009) Neurological and epidemiological aspects of a BoHV-5 meningoencephalitis outbreak. Braz Arch Biol Technol 52:77–85
Majak W et al (2003) Bloat in cattle. Alberta Agriculture and Rural Development, Canada
Malafaia P et al (2016) Major health problems and their economic impact on beef cattle under two different feedlot systems in Brazil. Pesq Vet Bras 36:837–843
Mamak N, Börkü MK (2019) Hemorrhagic bowel syndrome in cattle. MAE Vet Fak Derg 4(2):108–112
Miller LM, Gal A (2017) Cardiovascular system and lymphatic vessels. In: Pathologic Basis of Veterinary Disease, 6th edn. pp 561–616
Mohammedi D et al (2014) Principales intoxications végétales chez les ruminants en zone méditerranéenne. Rev Elev Med Vet Pays Trop 67(4):163–171
Motta RG et al (2016) Unusual caudal vena cava thrombosis in a cow, secondary to Trueperella (Arcanobacterium) pyogenes infection. Pesq Vet Bras 36:587–590
Mõtus K et al (2017) On-farm mortality, causes and risk factors in Estonian beef cow-calf herds. Prev Vet Med 139:10–19
Nagaraja T, Lechtenberg KF (2007) Acidosis in feedlot cattle. Vet Clin North Am Food Anim Pract 23(2):333–350
Nalule A et al (2011) Ethnopharmacological practices in management of livestock helminthes by pastoral communities in the drylands of Uganda. Livest Res Rural Dev 23(2):1–27
Owens F et al (1998) Acidosis in cattle: a review. J Anim Sci 76(1):275–286
Peek S, Divers TJ (2018) Rebhun’s diseases of dairy cattle-E-Book. Elsevier Health Sciences
Pierson R et al (1976) Sudden deaths in yearling feedlot cattle. J Am Vet Med Assoc 169(5):527–529
Plumlee K (2003) Clinical Veterinary Toxicology-E-Book. Elsevier Health Sciences
Pohl P et al (1993) Escherichia coli producing CNF1 and CNF2 cytotoxins in animals with different disorders. Vet Res 24(4):311–315
Potter K, Besser T (1994) Cardiovascular lesions in bovine Marfan syndrome. Vet Pathol 31(5):501–509
Radostits OM et al (2006) Veterinary Medicine E-Book: a textbook of the diseases of cattle, horses, sheep, pigs and goats. Elsevier Health Sciences
Rao S et al (2019) Risk factors associated with the occurrence of anthrax outbreaks in livestock in the country of Georgia: a case-control investigation 2013–2015. PLoS ONE 14(5):e0215228
Redondo LM et al (2013) Sudden death syndrome in adult cows associated with Clostridium perfringens type E. Anaerobe 20:1–4
Roeber F et al (2013) Impact of gastrointestinal parasitic nematodes of sheep, and the role of advanced molecular tools for exploring epidemiology and drug resistance-an Australian perspective. Parasit Vectors 6(1):1–13
Roland L et al (2016) Invited review: influence of climatic conditions on the development, performance, and health of calves. J Dairy Sci 99(4):2438–2452
Ryan E et al (2008) Foot-and-mouth disease virus infection in young lambs: pathogenesis and tissue tropism. Vet Microbiol 127(3–4):258–274
Santos BL et al (2019) Clostridial diseases diagnosed in cattle from the South of Rio Grande do Sul, Brazil. A forty-year survey (1978–2018) and a brief review of the literature. Pesq Vet Bras 39:435–446
Sarjokari K et al (2018) On-farm deaths of dairy cows are associated with features of freestall barns. J Dairy Sci 101(7):6253–6261
Schild C et al (2017) Caudal vena cava thrombosis in a dairy cow (Bos taurus) in Argentina. Ciência Rural 47(6). https://doi.org/10.1590/0103-8478cr20160917
Schulze C et al (2016) Electrical injuries in animals: causes, pathogenesis, and morphological findings. Vet Pathol 53(5):1018–1029
Scott P et al (2011) Cattle medicine. CRC Press
Sessa F et al (2021) Sudden death in adults: a practical flow chart for pathologist guidance. In: Forensic Science and Legal Medicine A Multidisciplinary Puzzle, Healthcare. MDPI pp 870. https://doi.org/10.3390/books978-3-0365-4193-8
Shakespeare AS (2012) Aspiration lung disorders in bovines: a case report and review. J S Afr Vet Assoc 83(1):1–7
Simpson KM et al (2018) Clostridial abomasitis and enteritis in ruminants. Vet Clin N Am Food Anim Pract 34(1):155–184
Soares MP et al (2011) Amorimia exotropica poisoning as a presumptive cause of myocardial fibrosis in cattle. J Vet Diagn Invest 23(6):1226–1229
Souto E et al (2017) Sudden death caused by aortic aneurysm rupture in ruminants. Arq Bras Med Vet Zootec 69(2):398–404
Spickler A (2018) African animal trypanosomiasis. The Centre for Food Security & Public Health
Stalberger R, Kersting K (1988) Peracute toxic coliform mastitis. Iowa State Univ Vet 50(1):48–53
Stanitznig A, Wittek T (2018) Recovered case of sheep-associated malignant catarrhal fever in a gravid cow. Vet Rec Case Rep 6(1)
Underwood WJ et al (2015) Biology and diseases of ruminants (sheep, goats, and cattle). In :Laboratory animal medicine, 3rd edn. Elsevier, pp 623–694
Uzal FA et al (2014) Towards an understanding of the role of Clostridium perfringens toxins in human and animal disease. Future Microbiol 9(3):361–377
Uzal FA, Songer JG (2008) Diagnosis of Clostridium perfringens intestinal infections in sheep and goats. J Vet Diagn Invest 20(3):253–265
Van de Pypekamp H, Prozesky L (1987) Heartwater. An overview of the clinical signs, susceptibility and differential diagnoses of the disease in domestic ruminants. Onderstepoon J vet Res 54:263–266
Varga A, Puschner B (2012) Retrospective study of cattle poisonings in California: recognition, diagnosis, and treatment. Vet Med Res 3:111
Vermorel M et al (1983) Energy metabolism and thermoregulation in the newborn calf. Ann Rech Vet 14(4):382–389
Vetter J (2004) Poison hemlock (Conium maculatum L.). Food Chem Toxicol 42(9):1373–1382
Vitali A et al (2015) The effect of heat waves on dairy cow mortality. J Dairy Sci 98(7):4572–4579
Wäsle K et al (2017) The post-mortem examination in ruminants and its possible benefit to ruminant clinical medicine. J Comp Pathol 156(2–3):202–216
Wilson J et al (1975) Analyses of rumen fluid from “sudden death”, lactic acidotic and healthy cattle fed high concentrate ration. J Anim Sci 41(5):1249–1255
Wobeser BK, Schumann F (2014) Fascioloides magna infection causing fatal pulmonary hemorrhage in a steer. Can Vet J 55(11):1093
Yunker CE (1996) Heartwater in sheep and goats: a review. Onderstepoon J Vet Res 63:159–170
Acknowledgements
We wish to thank Mr. Benaoumer Bessekek for proofreading.
Author information
Authors and Affiliations
Contributions
MB, MA, and HH conceived and designed the format and the layout of the review. MB, HH, AAN, AB, and MC collected the literature and research papers. All authors interpreted the data, critically revised the manuscript for important intellectual contents, and approved the final version.
Corresponding author
Ethics declarations
Funding
This study was not supported by any funding.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Informed consent
For this type of study, informed consent is not required.
Consent for publication
The authors give their consent for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benchohra, M., Hemida, H., Ali-Nehari, A. et al. Sudden death syndrome in domestic ruminants: a review. Comp Clin Pathol 33, 489–502 (2024). https://doi.org/10.1007/s00580-024-03567-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-024-03567-5