Abstract
The cardioprotective impact of Amaranthus viridis methanolic extracts (AVMEs) and its active phytoconstituent kaempferol on isoproterenol (ISO)-induced cardiotoxicity in a rat model was examined in this study, along with some of the underlying molecular mechanisms. Prior to administering ISO (20 mg/100 mg BW) on the 31st and 32nd day to induce myocardial infarction (MI), the rats were pre-treated with AVME (250 mg/kg BW) and kaempferol (50 mg/kg BW) for 30 days each. Following ISO administration, we examined the effects of AVME and kaempferol on hemodynamic parameters, oxidative stress, and apoptotic markers in the heart tissue. The study’s findings showed that by reducing lipid peroxidation, vascular O2•̅, and NoX generation and enhancing the activities of antioxidant enzymes, AVME and kaempferol relieved the rats from hemodynamic depression and further protected them from free radical–mediated cardiac injury. Additionally, pre-treatment with AVME and kaempferol increased tissue levels of heme oxygenase (HO)-1 and nuclear factor erythroid-2-related factor-2 (Nrf-2) while de-escalating those of toll-like receptor-4 (TLR-4) and caspase-3. Furthermore, AVME and kaempferol down-regulated the expression of matrix metalloproteinases (MMP-2 and MMP-9), caspase-3, B cell lymphoma protein-2, Bcl-2-associated X, and TLR-4 while activating the Nrf-2/HO-1 pathway. Overall, the findings of the present investigation showed that up-regulation of the Nrf-2/HO-1 and concomitant down-regulation of MMP/Bax/Bcl-2/TLR-4 signaling pathways had significant ameliorative effects against ISO-induced MI by decreasing oxidative stress and apoptosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the largest risks to human health is myocardial infarction (MI), a pathological condition of the heart brought on by inadequate blood flow that results in decreased oxygen supply to the heart tissues and aberrant myocardial metabolism (Sangeethadevi et al. 2022). Due to its high prevalence and mortality, it is still a prominent study subject in the field of medicine (Zhou et al. 2020; Xing et al. 2022; Rong et al. 2023). The production of free radicals and proteolytic enzymes during an acute MI is related to an inflammatory response, oxidative stress, and a change in the extracellular matrix that leads to a modified myocardium (Boarescu et al. 2019). Isoproterenol (ISO) is a synthetic nonselective β-adrenergic agonist, and its high doses can cause energy depletion, coronary hypotension, myocardial oxidative stress, calcium overload, and other complications via acting on the heart’s β1 adrenergic receptors (Obeidat et al. 2022). To prevent the onset and progression of MI, it is crucial to look for pharmaceutical ways to reduce ISO-induced acute cardiac damage.
Oxidative stress can cause tissue damage and is crucial for the commencement of myocardial pathologic changes including inflammation and cell death, which eventually result in heart dysfunction and death (Kibel et al. 2020). The continuous reactive oxygen species (ROS) production coupled with the dysfunction of vital antioxidant defense mechanisms can induce myocardial inflammation through activating NF-κB and may elicit the stimulation of pro-apoptotic factors in cardiomyocytes, which arbitrate caspase-dependent and caspase-independent apoptotic cell death (Li et al. 2020). In order to prevent and/or treat MI and possibly other cardiovascular diseases (CVDs), it may be beneficial to reduce oxidative stress and apoptosis, activate cytoprotective pathways like nuclear factor erythroid 2-related factor 2 (Nrf-2), and inhibit matrix metalloproteinases (MMP), Toll-like receptor 4 (TLR4), and Bcl-2-associated X protein (Bax)/ B-cell lymphoma-2 (Bcl-2), which were key players in the apoptosis cascade in cardiomyocytes. Indeed, a number of antioxidant and detoxifying enzymes are activated by the significant nuclear transcriptional factor Nrf-2, which controls redox homeostasis (Uddandrao et al. 2022). Numerous investigations have shown that Nrf-2 activation mitigated cardiac dysfunction and reduced oxidative tissue damage, inflammatory responses, hypertrophy, and cell death in ISO-intoxicated animals (Sathibabu Uddandrao et al. 2018; Jansy et al. 2021).
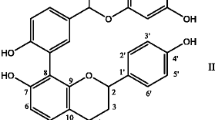
The modulation of ROS overproduction, inflammation, and Nrf-2/heme oxygenase-1 (HO-1) signaling by a number of natural products have been found to have both therapeutic and preventative effects against ISO-induced cardiac injury, according to several lines of evidence (Uddandrao et al. 2022; Abdelzaher et al. 2021; Abukhalil et al. 2021). The ubiquitous glabrous plant Amaranthus viridis (Amaranthaceae) is cultivated all over the world and has long been utilized in traditional medicine. Most studies on A. viridis have revealed that it may be used therapeutically to treat inflammatory, ulcerative, asthmatic, hyperlipidemic, diuretic, rheumatic, and analgesic conditions (Kavita and Puneet 2017). To the best of our knowledge, there is not a lot of research that has been published on the cardioprotective efficacy of A. viridis methanolic extracts (AVME) and its active phytoconstituents kaempferol. Therefore, the goal of this research is to investigate if AVME and kaempferol have any potential therapeutic benefits against ISO-induced MI in rats by reducing oxidative stress and apoptotic responses.
Materials and methods
Sample collection and preparations
A. viridis was collected from the local garden in Hyderabad, Telangana, India, and authenticated from Botanical Survey of India (BSI), Hyderabad, India-500001 (Voucher No: BSI/DRC/2022–23/Identification/556). AVME was extracted by using the soxhlet equipment and kaempferol was isolated and confirmed with liquid chromatography and mass spectrophotometry as described in our previous study. Furthermore, ISO (CAS No. 51–30-9) and α-tocopherol (CAS No. 10191–41-0) were obtained from Sigma-Aldrich Chemicals Private Limited, Bangalore, India. All other chemicals used were of analytical grade.
Animals
For this investigation, male Wistar rats weighing 150–180 g were utilized. They were fed a standardized pellet diet obtained from the National Institute of Nutrition, Hyderabad, Telangana, India, and were given access to water as required. The rats were kept in polycarbonate cages in an environment with a 12-h day/night cycle, a humidity level of 45–64%, and a temperature of 22 ± 2 °C. The Institutional Animal Ethical Committee at Jeeva Life Sciences in Hyderabad, Telangana, India, gave its approval to the study’s protocol (Approval No: CPCSEA/IAEC/JLS/14/02/21/80).
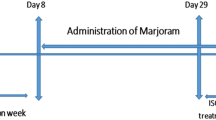
Experimental design
Group I consisted of normal control rats; Group II, MI control; Group III, MI + AVME (250 mg/kg BW); Group IV, MI + Kaempferol (50 mg/kg BW); and Group V, MI + α-tocopherol (60 mg/kg BW). Each group had six rats. Groups III to V received oral pre-treatment with the respective drugs through an intragastric tube for a total of 30 days. Rats in groups II to V were then subcutaneously treated with ISO (20 mg/100 g/BW) on the 31st and 32nd days. Following the research period, all of the rats were decapitated after being given an intraperitoneal dose of pentobarbital sodium (40 mg/kg/BW) to induce anesthesia. Blood was taken via a retro-orbital sinus puncture. Then immediately dissected hearts were straight away weighed and kept at − 80 °C until additional examination.
Hemodynamic and vascular responsiveness measurements
On the last day of the study, the animals were anesthetized by peritoneal injection of pentobarbital sodium (60 mg/kg body weight) and subjected to measurement of systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), and heart rate (HR) as described by Sathibabu Uddandrao et al. (2022).
Determination of cardiac oxidative stress markers
The generation of vascular O2•̅ was quantified using a lucigenin-enhanced chemiluminescence technique, and the concentration of NOx was evaluated using an enzymatic conversion technique. Malondialdehyde (MDA) level, the index of lipid peroxidation with Buege and Aust’s (1978) method, and reduced glutathione (GSH) were determined using colorimetric kits in accordance with the manufacturer’s instructions.
Determination of cardiac antioxidant status
The cardiac antioxidant biomarkers such as superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), glutathione reductase (GR), and glutathione-S-transferase (GST) were assessed as described by Saravanan and Ponmurugan (2011) earlier.
Measurement of Cardiac TLR-4, HO-1, Nrf-2, and Caspase-3
Cardiac TLR-4, HO-1, Nrf-2, and caspase-3 levels were assessed using ELISA kits as directed by the manufacturer (Elabscience®, USA).
RT-PCR analysis
Using the Trizol reagent (Invitrogen, Carlsbad, CA, USA) and a DNA synthesis kit (RevertAid First Strand cDNA Synthesis Kit, Thermo ScientificTM, India), total RNA was isolated from the cardiac tissue of control and experimental rats. For semi-quantitative PCR, 20 ng of cDNA was extracted and primed with specified primers, including Nrf-2, HO-1, MMP-2, MMP-9, BaX, Bcl-2, and TLR-4 (Table 1). The appropriate primers were used in 38 cycles of PCR amplification at the following cycling temperatures: 30 s of denaturation at 94 °C, 30 s of annealing at 59 °C, and 1 min of extension at 72 °C. For standardization, the housekeeping gene β-actin was employed.
Western blot analysis
A proteinase inhibitor and radioimmunoprecipitation assay lysis buffer were added to the cardiac tissue of the experimental rats to extract the protein, which was subsequently homogenised by sonication on ice for one minute. Centrifuging the supernatant at 20,000 × g for 15 min at 4 °C and 20 µl of each suspension sample was taken, placed onto a 6% sodium dodecyl sulphate gel, and then transferred to a polyvinylidene fluoride membrane utilising trans-turbo gel transfer apparatus. The primary antibodies anti-Nrf-2 (sc-81342), anti-HO-1 (sc-390991), and anti-TLR-4 (sc-52962) were purchased commercially from Santa Cruz Biotechnology, USA. They were dissolved in 3% non-fat dry milk (1:1,000) and incubated overnight at 4 °C before being rinsed with Tris-buffered saline with Tween 20 buffer. Later, the membranes were incubated with horseradish peroxidase–conjugated secondary antibodies for 1 h at room temperature with shaking.
Statistical analysis
For six animals in each group, the mean and SD were used to express all the data. Using the SPSS (28.0.1.1), all of the aggregated data were statistically assessed. One-way analysis of variance (ANOVA) and the least significant difference (LSD) tests were used to assess hypotheses. A significance threshold of P < 0.05 or 0.01 were taken to denote statistical significance.
Results
AVME and kaempferol restored altered hemodynamic parameters
Figure 1 demonstrates the effects of AVME and kaempferol on hemodynamic and vascular responsiveness in control and experimental MI rats. SBP (Fig. 1A), DBP (Fig. 1B), MAP (Fig. 1C), and HR (Fig. 1D) were notably (P < 0.05, 0.01) decreased in the ISO-induced MI control when compared to the normal control group. On the other hand, pre-treatment with AVME and kaempferol considerably restored these alterations to near normal comparable to untreated MI rats.
Effect of AVME and kaempferol on hemodynamic parameters A systolic blood pressure (SBP), B diastolic blood pressure (DBP), C mean arterial pressure (MAP), and D heart rate (HR) in control and ISO-induced MI rats. Values are expressed as mean ± SD, n = 6, values are significantly different at *P < 0.05, #P < 0.01, a vs b and b vs c or d or e
AVME and kaempferol attenuated cardiac oxidative stress
Figure 2 depicts the effect of AVME and kaempferol on cardiac oxidative stress markers in control and experimental MI rats. Administration of ISO resulted in a significant increase in the NOx levels (Fig. 2A) and vascular O2•̅ production (Fig. 2B) in MI control rats when compared with normal control. At the same time, there was a noteworthy increase in the MDA (Fig. 2C) and a concomitant decrease in the GSH content (Fig. 2D) in the heart of MI control rats. However, pre-treatment with AVME and kaempferol substantially (P < 0.05, 0.01) attenuated the cardiac oxidative stress which was confirmed with elevated GSH content and decreased lipid peroxidation along with suppression of vascular O2•̅ production and NOx noted in these groups.
AVME and kaempferol attenuated cardiac oxidative stress by reducing the levels of A vascular O2•̅, B nitric oxide (NOx), and C malondialdehyde (MDA), and enhancing the D reduced glutathione (GSH) content in ISO-induced MI rats. Values are expressed as mean ± SD, n = 6, values are significantly different at *P < 0.05, #P < 0.01, a vs b and b vs c or d or e
The antioxidant state was enhanced with AVME and kaempferol pre-treatment
Figure 3 shows that compared to normal control rats, the treatment of ISO further reduced (P < 0.05, 0.01) the activity of antioxidant enzymes such SOD (Fig. 3A), CAT (Fig. 3B), GPx (Fig. 3C), GR (Fig. 3D), and GST (Fig. 3E). As opposed to untreated MI control rats, pre-treatment with AVME and kaempferol improved antioxidant status by restoring the activity of the aforementioned enzymes in these groups.
AVME and kaempferol enhanced the activities of cardiac indigenous antioxidants A superoxide dismutase (SOD), B catalase (CAT), C glutathione peroxidase (GPx), D glutathione reductase (GR), and E glutathione-S-transferase (GST) in ISO-induced MI rats. Values are expressed as mean ± SD, n = 6, values are significantly different at *P < 0.05, #P < 0.01, a vs b and b vs c or d or e
Effect of AVME and kaempferol on cardiac Nrf-2, HO-1, TLR-4, and caspase-3
In the cardiac tissue of ISO-induced MI rats, a notable decrease in the levels of Nrf-2 (Fig. 4A) and HO-1 (Fig. 4B) and a concurrent increase in the levels of TLR-4 (Fig. 4C) and caspase-3 (Fig. 4D). Comparing treated and untreated MI control rats, pre-treatment with AVME and kaempferol revealed a notable (P < 0.01) rise in Nrf-2 and HO-1 levels and a simultaneous decrease (P < 0.05, 0.01) in TLR-4 and caspase-3 levels in the heart tissue (Fig. 4).
Effect of AVME and kaempferol on cardiac A nuclear factor erythroid 2-related factor 2 (Nrf-2), B heme oxygenase-1 (HO-1), C Toll-like receptor 4 (TLR4) and D caspase-3 in control and ISO-induced MI rats. Values are expressed as mean ± SD, n = 6, values are significantly different at *P < 0.05, #P < 0.01, a vs b and b vs c or d or e
AVME and kaempferol up-regulated Nrf-2/HO-1 and down-regulated MMP/Bax/Bcl-2/TLR-4 pathways
Figure 5 shows that when ISO was administered to rats, Nrf-2 (Fig. 5A) and HO-1 (Fig. 5B) mRNA expressions were noticeably (P < 0.05) down-regulated, whereas MMP-2 (Fig. 5C), MMP-9 (Fig. 5D), BaX (Fig. 5E), Bcl-2 (Fig. 5F), and TLR-4 (Fig. 5G) mRNA expressions were evidently (P < 0.05, 0.01) up-regulated in MI control rats. The expression of the relevant changed genes in the heart tissue was, however, successfully restored following pre-treatment with AVME and kaempferol.
Effect of AVME and kaempferol on mRNA expressions of A nuclear factor erythroid 2-related factor 2 (Nrf-2), B heme oxygenase-1 (HO-1), C matrix metalloproteinase-2 (MMP-2), D matrix metalloproteinase-9 (MMP-9), E Bcl-2-associated X protein (Bax), F B cell lymphoma-2 (Bcl-2), and G Toll-like receptor 4 (TLR4) in control and ISO-induced MI rats. Values are expressed as mean ± SD, n = 6, values are significantly different at *P < 0.05, #P < 0.01, a vs b and b vs c or d or e
In addition, we further evaluated the protein expressions of Nrf-2, HO-1, and TLR-4, which showed that in ISO-induced MI control rats, Nrf-2 (Fig. 6A) and HO-1 (Fig. 6B) were significantly (P < 0.01) down-regulated, while TLR-4 (Fig. 6C) were parallelly up-regulated. At the same time, groups that had received pretreatment with AVME and kaempferol showed a notable (P < 0.05, 0.01) up-regulation of Nrf-2 and HO-1 and a down-regulation of TLR-4 (Fig. 6).
Effect of AVME and kaempferol on protein expressions of A nuclear factor erythroid 2-related factor 2 (Nrf-2), B heme oxygenase-1 (HO-1), and C Toll-like receptor 4 (TLR4) in control and ISO-induced MI rats. Values are expressed as mean ± SD, n = 6, values are significantly different at *P < 0.05, #P < 0.01, a vs b and b vs c or d or e
Discussion
This work was inspired by a recent favorable cardioprotective effect of AVME and kaempferol in order to enquiringly investigate the mechanisms of its activity. The current research demonstrated the cardioprotective effects of AVME and kaempferol in rats with MI induced by ISO. Although catecholamines are responsible for controlling cardiac function, high doses cause ischemic heart disease such as MI. Furthermore, changes in cardiac structure and function in rats after ISO are equivalent to human MI when used to assess the potential cardioprotective impact of any novel pharmacological drug (Mohamed et al. 2021; Govindasami et al. 2020; Pavithra et al. 2020).
As a β-adrenergic receptor agonist, ISO administered subcutaneously raises blood pressure right away. However, over time, it can drop arterial pressure, which is followed by a rise in oxygen demand, hypoxia, and myocardial ischemia (Ma et al. 2020). Decreased MAP, HR, and cardiac contractility are a result of necrosis and cardiovascular injury. The drop in SBP, DBP, MAP, and HR caused by ISO infusion over 2 days in a row suggests clinically severe heart failure linked to MI. The need for oxygen increases when blood pressure and heart rate decline. As a result, the equilibrium between the supply of coronary blood and the demand placed on the heart declines, finally resulting in hypoxia and ischemic heart disease (Filipský et al. 2012). Similar to other studies, we found that pre-treatment with AVME and kaempferol protected from MI, which was supported by normal hemodynamic parameters noted in these groups. The decrease in SBP, DBP, MAP, and HR in MI control rats confirmed induction of MI, and pre-treatment with AVME and kaempferol offered protection from MI.
Additionally, mounting data demonstrates that ISO triggers the production of ROS, which in turn causes oxidative stress. The disturbance of a delicate oxidant/antioxidant balance may be one potential molecular mechanism behind ISO-induced MI, which can cause oxidative damage to the myocardium (Pavithra et al. 2020). In the current work, we showed that ISO treatment increased the rat’s production of ROS and caused oxidative damage to the myocardium. If enough antioxidant molecules are not present to prevent the reaction of free radicals formed from ROS with lipids, lipid peroxides can occur which can cause significant damage (Sathibabu Uddandrao et al. 2019). Lipids make up the majority of biological membranes; therefore, their oxidation can cause cell damage and death. The first step in the tissue becoming more vulnerable to oxidative damage appears to be a considerable rise in vascular O2•̅ production and MDA levels in ISO-induced rats. The enhanced lipid peroxidation in terms of MDA and oxidative stress indicators such as vascular O2•̅ and NoX in the current study suggest that excessive ROS generation may be the cause of the observed membrane damage. Additionally, GSH, a tripeptide that may operate as a nonenzymatic antioxidant by interacting with ROS and then oxidizing to form oxidized glutathione and other disulfides, is crucial for the regulation of a number of cellular activities as well as for protecting cells from damage caused by free radicals (Brahmanaidu et al. 2017). In contrast, myocardial levels of MDA, vascular O2•̅, and NoX were noticeably reduced by AVME and kaempferol. The studies also showed that kaempferol can better increase the antioxidant defense of the cardiomyocytes when compared to AVME and that their antioxidant properties are promising to be pharmacologically useful against heart ischemia.
The Nrf-2, which has been shown to be an essential transcription factor that controls the activation of phase 2 detoxifying and antioxidant genes, is one of the hypothesized methods for understanding the underlying biochemical and molecular processes during MI happening with ISO administration (Li et al. 2016). Therefore, we investigated the significance of Nrf-2/HO-1 signaling activation in the cardioprotective effect of AVME and kaempferol since it is crucial in preventing ISO-induced acute MI (Abdelzaher et al. 2021; Wu et al. 2022). Our study results demonstrated that ISO treatment caused Nrf-2 and HO-1 to be down-regulated in the heart, which is consistent with numerous studies (Abdelzaher et al. 2021; Wu et al. 2022; Obeidat et al. 2022). Additionally, it has been demonstrated that Nrf-2/HO-1 activation controls inflammatory responses by down-regulating NF-κB signaling and increasing anti-inflammatory cytokines (Sathibabu Uddandrao et al. 2022). Oxidative stress and inflammation are major contributors to CVDs (Jansy et al. 2021) and pharmacological strategies that target Nrf-2/HO-1 signaling might be thought of as having potential therapeutic benefits. An earlier work done by Jansy et al. (2021) and Uddandrao et al. (2022) found that Nrf-2 knockdown increased mortality, reduced antioxidant gene expression in the heart, increased cardiac fibrosis, and enhanced apoptosis in rats following pathological pressure overload confirms this hypothesis. In line with these findings, the present investigation found that ISO treatment decreased tissue Nrf-2 and HO-1 while concurrently reducing the activities of SOD, CAT, GPx, GR, and GST in the heart of MI control rats. However, the Nrf-2/HO-1 signaling pathway was markedly enhanced in the myocardium of ISO-intoxicated rats treated with AVME and kaempferol. In order to prevent cardiac damage brought on by ISO, Nrf-2/HO-1 activation mediated by the AVME and kaempferol is thought to be prophylactic.
Furthermore, our investigation showed that kaempferol outperforms AVME in reducing the rise in MMP-2 and MMP-9 levels following ISO-induced MI in rats. The anatomic substrate for the development of congestive heart failure and sudden cardiac death is extracellular matrix degradation and structural alterations of cardiomyocytes in both infarcted and non-infarcted myocardium, which are mediated by MMPs, an important proteolytic enzyme (Cabral-Pacheco et al. 2020). Following MI, AVME and kaempferol therapy promotes heart repair and alleviate cardiac dysfunction by inhibiting both MMP-2 and MMP-9 along with their potent antioxidant effect (Sangeethadevi et al. 2022). The mitigation of oxidative stress and the decreased activity of active MMPs may be the cause of AVME and kaempferol’s cardioprotective effects. On the other hand, it has been demonstrated that cardiomyocyte apoptosis is a crucial kind of cell death. The activation of caspase is a key component of the apoptotic signaling cascade. The most important apoptosis-regulating protein in the caspase family, which is triggered by numerous apoptotic triggers, is caspase-3. When the body experiences apoptotic stress, caspase-3 can be cleaved and activated by the caspase cascade, which eventually produces apoptosis (McIlwain et al. 2013). The proteins of the Bcl-2 family play crucial regulatory roles in the apoptotic process. Bax and Bcl-2 are both members of the Bcl-2 family, which have, respectively, proapoptotic and antiapoptotic functions (Hatok and Racay 2016). Here, we discover that AVME and kaempferol reduced the amount of proapoptotic caspase-3, antiapoptotic Bcl-2, and ISO-induced cardiomyocyte death. In addition, TLRs are also found in macrophages and monocytes because they are a common form of innate immune response receptor. They can recognize and interact with certain molecular proteins of host apoptosis surfaces. TLR-4 plays a key role in triggering the inflammatory response by stimulating Hsp70 in MI and mediating the release of pro-inflammatory cytokines in acute injury (Ibrahim et al. 2021). This is consistent with the current findings that the MI control’s heart had an abnormally high level of cardiac TLR-4 and up-regulated levels of TLR-4 protein and mRNA expression. However, these abnormalities were reduced by AVME and kaempferol.
Conclusion
In conclusion, the current investigation shows that AVME and kaempferol have cardioprotective effects against ISO-induced MI in rats, primarily due to their capacity to increase antioxidant response and decrease MMP expression in ISO-induced MI. Additionally, by interfering with myocardial oxidative stress and apoptosis via the Nrf-2/Ho-1 and MMP/Bax/Bcl-2/TLR-4 signaling pathways, AVME and kaempferol had notable ameliorative benefits against ISO-induced MI. In addition, kaempferol outperformed AVME in regard to its efficiency in preventing ISO-induced cardiotoxicity. In light of the fact that this study explains the cardioprotective mechanisms of AVME and kaempferol, it may be able to offer experimental support and new information on the creation of focused preventative medicines for the treatment of MI and post-MI damage.
Data availability
The data that support the findings of this study are available on reasonable request from the corresponding author, Roja Rani A.
References
Abdelzaher WY, Ahmed SM, Welson NN, Alsharif KF, Batiha GE, Labib DAA (2021) Dapsone ameliorates isoproterenol-induced myocardial infarction via Nrf2/ HO-1; TLR4/ TNF-α signaling pathways and the suppression of oxidative stress, inflammation, and apoptosis in rats. Front Pharmacol 12:669679. https://doi.org/10.3389/fphar.2021.669679
Abukhalil MH, Hussein OE, Aladaileh SH, Althunibat OY, Al-Amarat W, Saghir SA, Alfwuaires MA, Algefare AI, Alanazi KM, Al-Swailmi FK, Kamel EM, Mahmoud AM (2021) Visnagin prevents isoproterenol-induced myocardial injury by attenuating oxidative stress and inflammation and upregulating Nrf2 signaling in rats. J Biochem Mol Toxicol 35:e22906. https://doi.org/10.1002/jbt.22906
Boarescu PM, Chirilă I, Bulboacă AE, Bocșan IC, Pop RM, Gheban D, Bolboacă SD (2019) Effects of curcumin nanoparticles in isoproterenol-induced myocardial infarction. Oxid Med Cell Longev 2019:7847142. https://doi.org/10.1155/2019/7847142
Brahmanaidu P, Uddandrao VVS, Sasikumar V, Naik RR, Pothani S, Begum MS, Rajeshkumar MP, Varatharaju C, Meriga B, Rameshreddy P, Kalaivani A, Saravanan G (2017) Reversal of endothelial dysfunction in aorta of streptozotocin-nicotinamide-induced type-2 diabetic rats by S-Allylcysteine. Mol Cell Biochem 432:25–32. https://doi.org/10.1007/s11010-017-2994-0
Buege JA, Aust SD (1978) Microsomal lipid peroxidation. Methods Enzymol 52:302–310. https://doi.org/10.1016/s0076-6879(78)52032-6
Cabral-Pacheco GA, Garza-Veloz I, Castruita-De la Rosa C, Ramirez-Acuña JM, Perez-Romero BA, Guerrero-Rodriguez JF, Martinez-Avila N, Martinez-Fierro ML (2020) The roles of matrix metalloproteinases and their inhibitors in human diseases. Int J Mol Sci 21:9739. https://doi.org/10.3390/ijms21249739
Filipský T, Zatloukalová L, Mladěnka P, Hrdina R (2012) Acute initial haemodynamic changes in a rat isoprenaline model of cardiotoxicity. Hum Exp Toxicol 31:830–843. https://doi.org/10.1177/0960327112438927
Govindasami S, Uddandrao VVS, Raveendran N, Sasikumar V (2020) Therapeutic potential of biochanin-A against isoproterenol-induced myocardial infarction in rats. Cardiovasc Hematol Agents Med Chem 18:31–36. https://doi.org/10.2174/1871525718666200206114304
Hatok J, Racay P (2016) Bcl-2 family proteins: master regulators of cell survival. Biomol Concepts 7:259–270. https://doi.org/10.1515/bmc-2016-0015
Ibrahim MA, Abdelzaher WY, Ibrahim YF, Ahmed AF, Welson NN, Al-Rashed S, Batiha GE, Abdel-Aziz AM (2021) Diacerein protects rats with liver ischemia/reperfusion damage: down-regulation of TLR4/ NFκ-B signaling pathway. Biomed Pharmacother 134:111063. https://doi.org/10.1016/j.biopha.2020.111063
Jansy Isabella Rani A, Sathibabu Uddandrao VV, Sangeethadevi G, Saravanan G, Chandrasekaran P, Sengottuvelu S, Tamilmani P, Sethumathi PP, Vadivukkarasi S (2021) Biochanin A attenuates obesity cardiomyopathy in rats by inhibiting oxidative stress and inflammation through the Nrf-2 pathway. Arch Physiol Biochem 1–16. https://doi.org/10.1080/13813455.2021.1874017
Kavita P, Puneet G (2017) Rediscovering the therapeutic potential of Amaranthus species: a review. Egypt J Basic Appl Sci 4:196–205. https://doi.org/10.1016/j.ejbas.2017.05.001
Kibel A, Lukinac AM, Dambic V, Juric I, Selthofer-Relatic K (2020) Oxidative stress in ischemic heart disease. Oxid Med Cell Longev 6627144. https://doi.org/10.1155/2020/6627144.
Li H, Yang H, Wang D, Zhang L, Ma T (2020) Peroxiredoxin2 (Prdx2) Reduces oxidative stress and apoptosis of myocardial cells induced by acute myocardial infarction by inhibiting the TLR4/nuclear factor kappa B (NF-κB) signaling pathway. Med Sci Monit 26:e926281. https://doi.org/10.12659/MSM.926281.
Li H, Song F, Duan LR, Sheng JJ, Xie YH, Yang Q, Chen Y, Dong QQ, Zhang BL, Wang SW (2016) Paeonol and danshensu combination attenuates apoptosis in myocardial infarcted rats by inhibiting oxidative stress: Roles of Nrf2/HO-1 and PI3K/Akt pathway. Sci Rep 6:23693. https://doi.org/10.1038/srep23693
Ma S, Ma J, Tu Q, Zheng C, Chen Q, Lv W (2020) Isoproterenol increases left atrial fibrosis and susceptibility to atrial fibrillation by inducing atrial ischemic infarction in rats. Front Pharmacol 1:493. https://doi.org/10.3389/fphar.2020.00493
McIlwain DR, Berger T, Mak TW (2013) Caspase functions in cell death and disease. Cold Spring Harb Perspect Biol 5:a008656. https://doi.org/10.1101/cshperspect.a008656
Mohamed ME, Abduldaium MS, Younis NS (2021) Cardioprotective effect of linalool against isoproterenol-induced myocardial infarction. Life (basel, Switzerland) 11:120. https://doi.org/10.3390/life11020120
Obeidat HM, Althunibat OY, Alfwuaires MA, Aladaileh SH, Algefare AI, Almuqati AF, Alasmari F, Aldal’in HK, Alanezi AA, Alsuwayt B, Abukhalil MH (2022) Cardioprotective effect of taxifolin against isoproterenol-induced cardiac injury through decreasing oxidative stress, inflammation, and cell death, and activating Nrf2/HO-1 in mice. Biomolecules 12:1546. https://doi.org/10.3390/biom12111546
Pavithra K, Sathibabu Uddandrao VV, Chandrasekaran P, Brahmanaidu P, Sengottuvelu S, Vadivukkarasi S, Saravanan G (2020) Phenolic fraction extracted from Kedrostis foetidissima leaves ameliorated isoproterenol-induced cardiotoxicity in rats through restoration of cardiac antioxidant status. J Food Biochem 44:e13450. https://doi.org/10.1111/jfbc.13450
Rong N, Yang R, Ibrahim IAA, Zhang W (2023) Cardioprotective role of scopoletin on isoproterenol-induced myocardial infarction in rats. Appl Biochem Biotechnol 195:919–932. https://doi.org/10.1007/s12010-022-04123-z
Sangeethadevi G, VVS U, Jansy Isabella RAR, Saravanan G, Ponmurugan P, Chandrasekaran P, Sengottuvelu S, Vadivukkarasi S (2022) Attenuation of lipid metabolic abnormalities, proinflammatory cytokines, and matrix metalloproteinase expression by biochanin-A in isoproterenol-induced myocardial infarction in rats. Drug Chem Toxicol 45:1951–1962. https://doi.org/10.1080/01480545.2021.1894707
Saravanan G, Ponmurugan P (2011) Ameliorative potential of S-allyl cysteine on oxidative stress in STZ induced diabetic rats. Chem Biol Interact 189:100–106. https://doi.org/10.1016/j.cbi.2010.10.001
Sathibabu Uddandrao VV, Brahmanaidu P, Nivedha PR, Vadivukkarasi S, Saravanan G (2018) Beneficial role of some natural products to attenuate the diabetic cardiomyopathy through Nrf2 pathway in cell culture and animal models. Cardiovasc Toxicol 18:199–205. https://doi.org/10.1007/s12012-017-9430-2
Sathibabu Uddandrao VV, Brahmanaidu P, Ravindarnaik R, Suresh P, Vadivukkarasi S, Saravanan G (2019) Restorative potentiality of S-allylcysteine against diabetic nephropathy through attenuation of oxidative stress and inflammation in streptozotocin-nicotinamide-induced diabetic rats. Eur J Nutr 58:2425–2437. https://doi.org/10.1007/s00394-018-1795-x
Sathibabu Uddandrao VV, Sethumathi PP, Parim Brahma Naidu, Vadivukkarasi S, Mustapha Sabana Begum, Saravanan G (2022) Ameliorative potential of biochanin-A against dexamethasone induced hypertension through modulation of relative mRNA and protein expressions in experimental rats, advancements in cardiovascular research and therapeutics: molecular and nutraceutical perspectives 1:156. https://doi.org/10.2174/9789815050837122010011
Uddandrao VVS, Parim B, Singaravel S, Ponnusamy P, Ponnusamy C, Sasikumar V, Saravanan G (2022) Polyherbal formulation ameliorates diabetic cardiomyopathy through attenuation of cardiac inflammation and oxidative stress via NF-κB/Nrf-2/HO-1 pathway in diabetic rats. J Cardiovasc Pharmacol 79:e75–e86. https://doi.org/10.1097/FJC.0000000000001167
Wu X, Wei J, Yi Y, Gong Q, Gao J (2022) Activation of Nrf2 signaling: A key molecular mechanism of protection against cardiovascular diseases by natural products. Front Pharmacol 13:1057918. https://doi.org/10.3389/fphar.2022.1057918
Xing Z, Yang C, He J, Feng Y, Li X, Peng C, Li D (2022) Cardioprotective effects of aconite in isoproterenol-induced myocardial infarction in rats. Oxid Med Cell Longev 2022:1090893. https://doi.org/10.1155/2022/1090893
Zhou Y, Li M, Song J, Shi Y, Qin X, Gao Z, Lv Y, Du G (2020) The cardioprotective effects of the new crystal form of puerarin in isoproterenol-induced myocardial ischemia rats based on metabolomics. Sci Rep 10:17787. https://doi.org/10.1038/s41598-020-74246-y
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received funding from DST-SERB Project, UGC-Centre with Potential for Excellence in Particular Area (CPEPA) by RRA and the infrastructure facilities was partially supported by DST PURSE 2.0, Department of Science and Technology, Government of India. The fellowship was provided by UGC-RGNF, New Delhi to RKN (Fellowship No: 202021-NFST-TEL-00696; dt: 20-09-2021).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The protocol of the study was approved by the Institutional Animal Ethical Committee, Jeeva Life Sciences, Hyderabad, Telangana, India (Approval No: CPCSEA/IAEC/JLS/14/02/21/80). All the experiments were carried out as per the guidelines provided by Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), Government of India.
Informed consent
For this type of study, informed consent is not required.
Consent for publication
All the authors have read the manuscript and approved the submitted version.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Krishna, P.S., N, R.K., Swathi et al. Amaranthus viridis methanolic extract and its active compound kaempferol ameliorate myocardial infarction induced by isoproterenol through decreasing oxidative stress and cell death via Nrf-2/HO-1 and MMP/Bax/Bcl-2/TLR-4 pathways in rats. Comp Clin Pathol 32, 661–670 (2023). https://doi.org/10.1007/s00580-023-03474-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-023-03474-1