Abstract
Colonization of chicken gut by pathogenic Escherichia coli harboring mobile colistin resistance (mcr-1) gene is a huge public and animal health risk. This study was undertaken to evaluate colistin (COL) resistance transfer potentials and pathogenicity of mcr-1-positive E. coli isolates from chickens in Southeastern Nigeria (SEN). In vitro mcr-1/COL resistance transfer of 22 mcr-1-positive E. coli isolates was assayed by conjugation test. A 1:1 v/v broth culture containing 1 × 108 colony-forming unit/mL of each test isolate (donor) and sodium azide–resistant E. coli J53 (recipient) was mated overnight at 37 °C in nutrient broth (NB), and transconjugants were selected on MacConkey agar containing COL (4 µg/mL) and sodium azide (150 µg/mL). Four groups of 10 healthy 1-week-old chickens devoid of COL-resistant organism were orally inoculated with 0.5 mL of 1 × 108 cfu/mL broth culture of three strains of mcr-1-positive E. coli and E. coli J53, and one unchallenged group was used as a control. Clinical signs were monitored regularly and recorded. Periodically collected cloacal swab samples and organs obtained from animals sacrificed 21 days post-experimental challenge were cultured on selective media and isolates were characterized. Pathogenicity of the donors in the birds was assessed grossly and histomorphologically. Fifty-nine percent of the 22 mcr-1-positive isolates transferred COL resistance to E. coli J53 at a frequency of 5.0 × 10−7 to 4.5 × 10−6. Histopathologically, no lesion was observed in tissue sections of birds in the control group. But in the challenged birds, the liver had mild hyperaemia, hepatocyte degeneration/necrosis, and mononuclear cell aggregation. Their spleen had moderate to severe hyperaemia with reactive white pulp while their heart revealed mild to moderate hyperaemia, oedema of myocardial interstices, multifocal areas of myocardial fiber necrosis, and mononuclear cell infiltration. Potentially pathogenic mcr-1-positive E. coli is spreading COL resistance among Enterobacterales colonizing the gut of chickens in SEN and this has clinical and public health significance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Escherichia (E.) coli is a normal inhabitant (commensal bacterium) in the gut of humans and animals, including poultry, but opportunistically it causes intestinal and several extraintestinal disease syndromes (Nolan et al. 2020). Avian pathogenic E. coli (APEC), especially the antimicrobial-resistant strains, is a major troubling zoonotic pathogen within the poultry industry (Collingwood et al. 2014). The pathogenicity of APEC is associated with the carriage of virulence-associated genes (VAGs), but E. coli strains not carrying VAGs have also been associated with diseases in poultry birds (Collingwood et al. 2014; Koutsianos et al. 2021).
Colistin (COL) is a critically important last-resort antibiotic of the highest priority used for treating deadly infections caused by multidrug-resistant (MDR) and extensively drug-resistant (XDR) Gram-negative bacilli in human and animals. Before 2015, bacterial resistance to COL was thought to be only by mutations in the chromosomal genes such as pmrAB, phoQP, and crrAB, and therefore transferred only vertically among a clone and thus by its very nature rare and self-limiting (Carretto et al. 2018; Anyanwu et al. 2021a). In late 2015, it was discovered that a plasmid-mediated COL resistance determinant, mobile COL resistance (mcr-1) gene is threatening the clinical efficacy of COL (Liu et al. 2016). Currently, ten mcr genes (mcr-1 to mcr-10) have been described (Valiakos and Kapna 2021). Due to the promiscuous nature of conjugative plasmids, a plasmid-borne mcr gene confers horizontally transmissible COL resistance unlike mutations in chromosomal genes, chromosomally-borne mcr, and non-conjugative plasmid-borne mcr genes that are only vertically transferred in a bacterial clone (Anyanwu et al. 2021b). The mcr-1 is the most frequently detected plasmid-encoded COL resistance determinant, and reports from across the globe have shown that E. coli is the major trafficker of mcr-1 (Valiakos and Kapna 2021). The presence of transferable mcr-1 in E. coli colonizing poultry bird, meat, or environment is a huge zoonotic risk to public and animal health as it jeopardizes antimicrobial therapy. Colistin-resistant (COL-r)/mcr-1-positive organisms are potentially multi- to pandrug-resistant, thus exhibiting resistance to virtually all available antibiotics thereby making their treatment difficult and often resulting in high morbidity, hospitalization cost, and fatality (McGann et al. 2016). Disturbingly, COL-r E. coli, especially the mcr-positive strains, is one of the major causes of deadly infections associated with loss of more than 700,000 human lives per annum worldwide (Neill 2014; Anyanwu et al. 2021b).
APEC causes avian colibacillosis which causes considerable economic and welfare problems attributed to its frequent occurrence and its adverse effects on growth and health (Ask et al. 2006). Clinically, colibacillosis in birds is characterized by respiratory signs, growth retardation, reduced feed intake, and increased mortality (Ask et al. 2006; Nolan et al. 2020). Air sacculitis and fibrinous polyserositis (pericarditis, perihepatitis, and peritonitis) are the main gross lesions, and septicaemia (colisepticaemia/haemorrhagic septicaemia), sometimes acute, is also common with many other uncommon lesions (Nolan et al. 2020). Colibacillosis causes condemnation of infected carcasses at slaughter, and increased prophylaxis and treatment cost and mortality (Ibrahim et al. 2019). These negative outcomes are aggravated if COL-r E. coli, especially an mcr gene-harboring strain, is incriminated in the disease. This is because possession of plasmid-borne mcr gene often confers survival fitness cost enabling the organisms to grow even in the presence of antimicrobial agents (Anyanwu et al. 2021b).
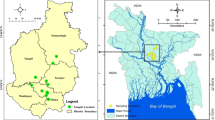
The use of COL in the Nigerian poultry sector, including in SEN, is not controlled (Anyanwu et al. 2021a, c), and there is increasing reports of treatment failure and increased mortality in cases of avian colibacillosis in Nigeria (Okorafor et al. 2019; Anyanwu et al. 2021a). Transfer of plasmids bearing VAGs and/or resistance genes from APEC to avian commensal E. coli has been shown to confer virulence (Cummins et al. 2017). This can potentially increase the losses due to outbreak of hard-to-treat diseases associated with COL resistance in poultry. Thus, there is need to understand the transferability of COL resistance and pathogenicity of Enterobacterales recovered from the poultry sector. In available literature, there exists European (Veldman et al. 2016; Alba et al. 2018; Quesada et al. 2016; Gelbíčová et al. 2019), Asian (Lim et al. 2016; Sun et al. 2016; Azam et al. 2017; Yamaguchi et al. 2018), South American (Lentz et al. 2016; Dominguez et al. 2018; Loayza-Villa et al. 2019), and African (Perreten et al. 2016; Maamar et al. 2018; Saidani et al. 2019) studies on in vitro transferability of mcr-1/COL resistance by Enterobacterales isolated from poultry. But information about COL resistance transfer by mcr gene-positive isolate from the Nigerian poultry sector is lacking in the literature. Moreover, there is paucity of information on in vivo transferability of mcr-1/COL resistance and pathogenicity/virulence of mcr-1 gene-harboring organisms (Le Devendec et al. 2018; Shen et al. 2019). Assessing the transferability of mcr-1 gene and pathogenicity of mcr-1-positive isolates is important in understanding the epidemiology and impact of COL resistance and devising effective strategies for curbing the spread of mcr genes. The objective of this study, therefore, was to evaluate the in vitro and in vivo mcr-1/COL resistance transfer and pathogenicity of mcr-1-postive E. coli isolates from chickens at farms in Southeast Nigeria.
Materials and methods
Colistin resistance transfer by mcr-1-positive E. coli isolates from chickens
Bacterial strains
Test or donor strains consisted of 22 multidrug-resistant and COL-r mcr-1-positive E. coli of diverse lineages recovered in 2018 from feces/rectal swabs of clinically healthy chickens at farms in SEN (Anyanwu et al. 2021a). Stock cultures of these isolates were sub-cultured on MacConkey agar (MCA) containing COL (4 µg/mL) and incubated at 37 °C for 18 h to ascertain purity. Recipient strain consisted of E. coli J53. E. coli J53, a plasmid-free E. coli strain without any acquired antimicrobial resistance but resistant only to sodium azide salt (Matsumura et al. 2018).
In vitro assay of colistin resistance transfer by the mcr-1-positive E. coli isolates
Ability of the 22 mcr-1-positive E. coli isolates to transfer COL resistance was assessed by conjugation assay (liquid/broth mating) following protocols described by Drali et al. (2018) with slight modification. Briefly, the recipient strain was sub-cultured on MCA supplemented with 150 µg/mL sodium azide (Dominguez et al. 2018) to ascertain for its purity. Colonies of each of the donors and that of the recipient were then inoculated into a 2-mL double-concentrated nutrient broth (NB) and adjusted to 0.5 McFarland’s turbidity to make a final concentration of 1 × 108 cfu/mL. The broth cultures were incubated for 3 h (mid-logarithmic growth stage) at 37 °C in ambient air. Thereafter, 0.5 mL of the donor’s broth culture and 0.5 mL of the recipient’s broth culture (1:1 v/v) were added to a 2-mL double-concentrated NB, and then incubated at 37 °C for 24 h in ambient air for conjugation. Transconjugants were selected by inoculating a loopful (10 µL) of the broth cultures on MCA containing COL (4 µg/mL) and sodium azide (150 µg/mL) followed by incubation at 37 °C for 48 h in ambient air. Presence of a colony on the selective agar was considered positive for conjugation. The conjugation (horizontal gene transfer [HGT]) frequency was calculated using the formular described by Lee (2019):
where Ncolony is number of transconjugant colonies on COL-supplemented selective agar plate, Vincubation is volume of the donor-recipient co-incubation cell suspension liquid that was used in spreading on the surface of COL-supplemented agar medium plate, Crecipient is concentration of recipient cells in the co-incubation liquid, and tincubation is donor-recipient co-incubation time.
The parental mcr-1-positive E. coli isolates were classified into three groups based on the HGT frequency (abundance of transconjugant colonies) as follows: group 1–one colony; group 2–two to four colonies; and group 3–five or more colonies. Isolates in group 3 (i.e., with highest HGT frequency) were selected and used for in vivo COL resistance transfer experiment. The transconjugants were sub-cultured on MCA and incubated at 37 °C for 24 h in ambient air. They were inoculated on nutrient agar slant, incubated at 37 °C for 24 h and stocked at 4 °C in the refrigerator until needed for further tests.
Evaluating non-polymyxin resistance cotransfer by the mcr-1-positive E. coli isolates
Co-resistance of transconjugants against non-polymyxin antibacterial agents was assessed using disk diffusion method (Clinical and Laboratory Standards Institute [CLSI] 2020). Briefly, colony suspension of the parental isolates and the transconjugants was made as previously described and spread-inoculated on Mueller–Hinton agar. Disks impregnated with gentamicin (CN, 10 µg), sulphamethoxazole-trimethoprim (SXT, 25 µg), and ciprofloxacin (CIP, 5 µg) were placed strategically on the inoculated plates and incubated at 37 °C for 24 h aerobically. The inhibitory zone diameter (IZD) around each disk was measured with a meter rule. Each test was performed in duplicate and the average IZD was calculated to the nearest whole millimeter (mm) for each isolate and each antibacterial agent. The IZD was interpreted as susceptible, intermediately susceptible, or resistant according to the recommendations for Enterobacterales (CLSI 2020).
In vivo assay of colistin resistance transfer by the mcr-1-positive E. coli isolates
Ethical clearance
The experiment was performed in accordance with the revised version of the Animals Scientific Procedures Act of 1986 for the care and use of animals for research purposes and the protocol was reviewed and approved (reference number: FVM-UNN-IACUC-2020–0138) by the Institutional Animal Care and Use Committee (IACUC) of the Faculty of Veterinary Medicine, University of Nigeria. The experiment was conducted in the animal facilities of the Department of Animal Health Production and Department of Veterinary Pathology and Microbiology, Faculty of Veterinary Medicine, University of Nigeria. Strict biosecurity measures were implemented to avoid contamination of the birds, including the use of unit-specific clothes/gloves, and compulsory handwashing/showering after visiting the birds.
Experimental animal
Forty 1-day-old chicks were obtained from a day-old chick distributor in Nsukka, Southeast Nigeria. Cloacal swab was collected from each of the bird upon arrival (day 0). Chick starter’s mash (Top feed®) and water were provided for them ad libitum. They were acclimatized for 1 week in the animal house of the Department of Animal Health Production in Faculty of Veterinary Medicine, University of Nigeria. During the acclimatization period, cloacal swabs were also collected from the chicks at mid-acclimatization period (day 4), and the end of acclimatization (day 7). The swabs were inoculated on MCA supplemented with COL (4 µg/mL) and incubated at 37 °C for 24–48 h in ambient air. Birds whose cloacal swabs were consistently negative for COL-r organisms in the 3 screening days were selected and used for the experiment.
Pathogens and preparation of inoculum
Three parental mcr-1-positive E. coli isolates with the highest HGT frequency–EC602 (ST126/CC10), EC400 (ST746/CC10), and EC100 (ST398/CC398)–served as donors of mcr-1/COL resistance while E. coli J53 served as the recipient. From MCA, colonies of each of the donor and the recipient were picked and inoculated into a 2-mL double-concentrated NB. The broth culture was adjusted to 0.5 McFarland’s turbidity to make a final concentration of 1 × 108 cfu/mL. The suspension was then incubated at 37 °C for 3 h in ambient air.
Animal groups and infection
The 40 1-week-old chicks negative for COL-r organisms were randomized into four groups of 10 chicks per group. Group 1, 2, and 3 were inoculated orally with 0.5 mL of 3-h broth culture of the recipient and 0.5 mL of 3-h broth culture of the donors (1:1 v/v) as follows: group 1–E. coli EC602 + E. coli J53; group 2–E. coli EC400 + E. coli J53; and group 3–E. coli EC100 + E. coli J53. Group 4 was similarly dosed with 1 mL of sterile double-concentrated NB and served as the control.
Clinical observation, sample collection, bacterial culture, and histopathology
The physical condition, morbidity, and mortality, if any, of the birds were observed and recorded for 21 days post-infection (dpi). Cloacal swabs were collected from seven randomly selected members of each group on day 2, 7, 14, and 21 post-infection (p.i.). To select for transconjugants, the swabs were inoculated on MCA supplemented either with COL (4 µg/mL), sodium azide (150 µg/mL), or combination of COL (4 µg/mL) and sodium azide (150 µg/mL). Inoculated plates were incubated at 37 °C for 24–48 h in ambient air. Growths were recorded and different morphotypes noted. For each sample, one distinct colony was picked, inoculated on MCA and incubated at 37 °C for 24 h in ambient air. The isolates were confirmed as E. coli by subjecting them to Gram staining, urease, citrate and triple sugar iron agar tests, and sub-culturing on eosin methylene blue agar.
At the termination of the experiment (21 dpi), the birds were euthanized using intramuscular injection of ketamine hydrochloride at 0.5 mg/kg body weight. Postmortem examination of the birds was carried out following the standard protocol (Bello et al. 2012). The severity of colibacillosis lesions in the right thoracic air sac, left thoracic air sac, pericardium, and liver, if any, was scored macroscopically following the criteria described by van Eck and Goren (1991). The criteria were as follows: 0 = no lesions; 0.5 = one pin head–sized inflammatory spot; 1 = two or more pin head–sized inflammatory spots; 2 = various fibrinous patches; while 3 = extensive fibrination and exudation. The maximal score per bird was 12. Mean lesion scores per group were calculated (van Eck and Goren 1991).
Sections of internal organs (intestines, spleen, heart, and liver) were collected in duplicates, one fixed in 10% buffered formalin and processed for histopathology whereas the other was unfixed-fresh tissue sample processed for bacterial isolation. The formalin-fixed tissues were embedded in paraffin, sectioned to 5 µm thickness, stained with hematoxylin and eosin, and examined microscopically under varying magnifications according to the standard procedure (Bancroft and Cook 1994). The fresh tissue samples were inoculated on MCA supplemented with either COL (4 µg/mL), sodium azide (150 µg/mL), or combination of COL (4 µg/mL) and sodium azide (150 µg/mL), and incubated at 37 °C for 24 h. Isolates were confirmed as E. coli by using standard tests mentioned above.
Data analysis
The results of the various tests were curated in Microsoft Excel version 15.0 and analyzed descriptively.
Results
In vitro COL resistance transfer by the mcr-1-positive E. coli isolates
Out of the 22 mcr-1-positive E. coli, 13 (59.1%) successfully transferred COL resistance to E. coli J53, with transfer frequency ranging from 5.0 × 10−7 to 4.5 × 10−6 (Table 1). Five (38.5%) of these 13 strains transferred COL resistance at a frequency of 5.0 × 10−6, while four (30.8%) transferred at a frequency of 1.5 × 10−6.
Non-polymyxin coresistance transfer by the mcr-1-positive E. coli isolates
Out of the 13 strains that successfully transferred COL resistance, none cotransferred resistance against CN, SXT, and CIP with COL resistance.
In vivo COL resistance transfer by the mcr-1-positive E. coli isolates
At day 2 p.i., 42.9% (3/7) and 57.1% (4/7) of birds in group 1 and 3 were colonized by COL-r E. coli, respectively (Table 2). By day 7 p.i., transconjugant (E. coli that grew on medium containing both COL and sodium azide) was recovered from 28% (2/7) of birds in group 1. On the same day, 57.1% (4/7) of birds in group 1, and 42.9% (3/7) of birds in group 2 and 3, were colonized by COL-r E. coli. By day 21 p.i., transconjugant was also recovered from 28.6% (2/7) of birds in group 3, while only one bird (14.3%, 1/7) in group 1 was colonized by COL-r E. coli on that day. COL-r Proteus was also isolated from some birds in group 1 and 2 on day 2 and 7 p.i., respectively.
Pathology of mcr-1-positive E. coli in experimentally-infected chickens
No observable clinical signs were recorded in the birds. No gross lesions were observed in birds from infected and the control groups. No organism was isolated from extraintestinal organs of the infected birds. Histologic examination of organs from the different groups showed mild to moderate changes in these organs. The liver was mildly hyperaemic in group 1 while it was moderately so in group 2 and 3 birds (Fig. 1). The periportal hepatocytes degeneration/necrosis was mild in group 1, while it was moderate in groups 2 and 3. In addition, there were multifocal areas of hepatocytes necrosis and mononuclear cell aggregation which was also mild in group 1 but moderate in groups 2 and 3. None of these changes was observed in the liver sections of birds in the control (group 4). The spleen sections of birds in group 2 were moderately to severely hyperaemic. The white pulp was moderately reactive in the same group (Fig. 2). These changes were absent in the other infected groups (1 and 3) and the control (group 4). Sections of the heart were mildly (in groups 1 and 2) to moderately (in group 2) hyperaemic (Fig. 3). There was mild to moderate edema of the myocardial interstices in all the infected groups. There were multifocal areas of myocardial fiber necrosis and mononuclear cell infiltration. The changes mentioned were absent in the carcasses of birds from the control (group 4).
Discussion
Recovery of transconjugants in the conjugation assay in this study indicates that mcr-1-positive E. coli strains colonizing chickens in SEN have potentials to transfer mcr-1 gene. The 5.0 × 10−7 to 4.5 × 10−6 conjugation frequency observed in this study indicates that the E. coli isolates transferred mcr-1 to the recipient organism by HGT at a high frequency. This suggests that mcr-1-harboring E. coli in chickens in SEN could potentially disseminate mcr-1 to other organisms in the chicken gut at a considerable frequency. Previous studies on conjugation with mcr-1-positive E. coli from chickens recorded different conjugation frequencies ranging from 2.6 × 10−1 to 5.1 × 10−2 in Spain (Queseda et al. 2016) and 5.1 × 10−3 to 9.4 × 10−5 in Vietnam (Yamaguchi et al. 2018). Yang et al. (2017) and Loayza-Villa et al. (2019) reported conjugation frequencies of 2 × 10−3 and 1 × 10−4 among mcr-1-positive E. coli isolates from chickens, respectively. Differences in conjugation frequencies could be due to ratio of donor to recipient organism used in the studies, and/or type of plasmid carrying the mcr-1 in the isolates (Potron et al. 2014; Tendon Valérie et al. 2017). It has been reported that various plasmids transfer mcr-1 to recipient organisms at different frequencies (Shen et al. 2019).
Recovery of 13 (59.1%) transconjugants among 22 parental mcr-1-positive E. coli isolates in this study supports that mcr-1 was carried on conjugative plasmid(s) in more than half of the isolates. Transfer of mcr-1 gene to a recipient organism could result in increased fold of COL resistance in the transconjugants (Sun et al. 2016; Yang et al. 2016). Thus, the 59.1% transconjugant recovery rate in this study is worrisome as development and spread of COL resistance in many poultry farms in SEN will result in a public health crisis that might be difficult to control. Considering that the poultry sector contributes hugely to the Nigerian economy, outbreak of colibacillosis associated with COL-r and mcr-1-harboring E. coli would result in huge economic loss, including increased unemployment rate and malnutrition.
The 59.1% transference in this work is significantly higher than 9.8% COL resistance transference rate among mcr-1-positive E. coli isolates from poultry birds in Bangladesh (Amin et al. 2020). It is however lower than 76.9–100% COL resistance transference rate among mcr-1-positive E. coli isolates from chickens/chicken meats in European (Veldman et al. 2016; Alba et al. 2018; Queseda et al. 2016) and Asian (Lim et al. 2016; Yamaguchi et al. 2018) countries. The result however contrasted the reports of Perreten et al. (2016), Hornsey et al. (2019), and Saidani et al. (2019) who did not recover any transconjugant among mcr-1-positive E. coli from chickens. Differences in the transference rate could be due to the recipient strain or methodology used in the studies (Hunter et al. 2008; Liu et al. 2018).
However, 9 (40.9%) out of the 22 mcr-1 donors used in this study did not transfer COL resistance to the recipient E. coli J53. As previously observed (Falgenhauer et al. 2016), carriage of mcr-1 on chromosome or non-conjugative plasmids is a possible reason as to why some E. coli strains in this study could not transfer COL resistance by conjugation (Falgenhauer et al. 2016). The implication of mcr-1 being located on sites other than conjugative plasmid is that the gene would be transferred among bacterial clones ensuring persistence of the gene in the environment (Liu and Liu 2018). Nevertheless, non-transference of COL resistance in this study might as well be due to the limitations of broth mating which has been shown to limit antimicrobial resistance transfer (Liu et al. 2019). This may also be responsible for non-transfer of coresistance against the non-polymyxins (CN, CIP, and SXT) observed in this study. Gene encoding factors responsible for resistance against the tested non-polymyxins are mostly chromosomally encoded with few that are plasmid-mediated (Schwarz et al. 2017; van Duijkeren et al. 2018). Non-transference of CN, CIP, and SXT together with COL resistance to a recipient organism has also been observed in a mcr-1 transferability study on E. coli isolates from chickens (Yin et al. 2017).
The fact that transconjugant was isolated from two birds in group 1 (by day 14 p.i.) and group 2 (by day 21 p.i.) indicates in vivo transfer of COL resistance from the donors to the recipient. The isolation of transconjugant on day 14 and 21 as against day 2 and 7 may suggest that the longer the duration of colonization of the chicken gut by COL-r organisms, the higher the likelihood of transferability of mcr-1/COL resistance to other organisms. Isolation of COL-r Proteus in this study further indicates that there was horizontal gene transfer of mcr-1/COL resistance from the donors to organisms in the chicken gut. This is plausible since none of the experimental chicken demonstrated growth of COL-r Proteus during the pre-experimental screening. Furthermore, Proteus was thought to be intrinsically resistant to COL, but recent studies showed that it is a potential carrier of mcr genes, including mcr-1 and mcr-3 (Caselli et al. 2018; Alhaj Sulaiman and Kassem 2019; Ben Khedher et al. 2020). However, non-recovery of transconjugant from some birds in the infected groups could be due to variation in host–pathogen interaction which differs with ability of pathogens to adhere to host cell receptors, as well as other factors such as hormonal variations and presence of interacting food substances in the bowel (Hunter et al. 2008).
The absence of gross lesions in the experimentally infected birds in this study was not unexpected since the birds appeared clinically healthy till the end of the experiment. Moreover, the mcr-1 E. coli isolates were recovered from healthy birds, suggesting that the strains might be commensal in nature. Nonetheless, the mild to moderate histopathologic lesions in the spleen, heart, and liver of birds in the infected groups suggest that the strains are extraintestinal pathogenic E. coli (ExPEC) strains. In fact, the three E. coli isolates (EC602, EC400, and EC100) that were used as mcr-1 gene donor in the in vivo study belonged to clonal complex (CC) CC10 and CC398. E. coli belonging to these clonal complexes has been associated with extraintestinal infections in human and poultry (Ewers et al. 2007; Yamaji et al. 2018; Manges et al. 2019). Moreover, toxins produced by some pathogenic/toxinogenic E. coli strains could elicit tissue/organ damages even in the absence of the organism itself (Kaper et al. 2004). Therefore, the E. coli isolates in this study could potentially cause extraintestinal diseases/lesions in chickens, especially when the immune system of a colonized bird is compromised. Treatment of infections associated with these organisms might be difficult since they are MDR. This could result in considerable financial losses to the farmers.
Conclusion
Colistin-resistant and mcr-1 gene-harboring E. coli in the gut of chickens in SEN is potentially pathogenic and could spread mcr-1/COL resistance to other Enterobacterales. These organisms can aggravate the negative impact associated with E. coli infections in poultry and humans. Thus, there is urgent need to restrict non-therapeutic use of COL in the Nigerian livestock sector.
References
Alba P, Leekitcharoenphon P, Franco A, Feltrin F, Ianzano A, Caprioli A, Stravino F, Hendriksen RS, Bortolaia V, Battisti A (2018) Epidemiology of mcr-encoded colistin resistance in Enterobacteriaceae from food-producing animals in Italy revealed through the EU harmonized antimicrobial resistance monitoring. Front Microbiol 9:1217
Alhaj Sulaiman AA, Kassem II (2019) First report of the plasmid-borne colistin resistance gene (mcr-1) in Proteus mirabilis isolated from domestic and sewer waters in Syrian refugee camps. Trav Med Infect Dis 2019:101482
Amin MB, Sraboni AS, Hossain MI, Roy S, Mozmader TIMAU, Unicomb L, Rousham EK, Islam MA (2020) Occurrence and genetic characteristics of mcr-1 positive colistin resistant E. coli from poultry environments in Bangladesh. J Glob Antimicrob Resist. https://doi.org/10.1016/j.jgar.2020.03.028
Anyanwu MU, Marrollo R, Paolucci M, Brovarone F, Nardini P, Chah KF, Shoyinka SVO, Carretto E (2021a) Isolation and characterization of colistin-resistant Enterobacterales from chickens in Southeast Nigeria. J Glob Antimicrob Resist 26:93–100
Anyanwu MU, Jaja IF, Okpala COR, Jaja C-JI, Oguttu JW, Chah KF, Shoyinka VS (2021b) Potential sources and characteristic occurrence of mobile colistin resistance (mcr) gene-harbouring bacteria recovered from the poultry sector: a literature synthesis specific to high-income countries. PeerJ 9:e11606. https://doi.org/10.7717/peerj.11606
Anyanwu MU, Okpala COR, Chah KF, Shoyinka VS (2021c) Prevalence and traits of mobile colistin resistance gene harbouring isolates from different ecosystems in Africa. Biomed Res Int. https://doi.org/10.1155/2021/6630379
Ask B, van der Waaij EH, van Eck JHH, van Arendonk JAM, Stegeman JA (2006) Defining susceptibility of broiler chicks to colibacillosis. Avian Pathol 35(2):147–153
Azam M, Ehsan I, Sajjad-Ur-Rahman SMK, Javed MR, Mohsin M (2017) Detection of the colistin resistance gene mcr-1 in avian pathogenic Escherichia coli in Pakistan. J Glob Antimicrob Resist 11:152–153
Bancroft JD, Cook HC (1994) Manual of histological techniques and their diagnostic application. Churchill Livingstone, Edinburgh
Bello A, Umaru MA, Baraya YS, Adamu YA, Jibir M, Garba S, Hena SA, Raji AA, Saidu B, Mahmuda A, Abubakar AA, Umar A, Musa D (2012) Postmortem procedure and diagnostic avian pathology. Sci J Zool 1(3):37–41
Ben Khedher M, Baron SA, Riziki T, Ruimy R, Raoult D, Diene SM, Rolain J-M (2020) Massive analysis of 64,628 bacterial genomes to decipher water reservoir and origin of mobile colistin resistance genes: is there another role for these enzymes? Sci Rep 10:5970
Carretto E, Brovarone F, Russello G, Nardini P, El-Bouseary MM, Aboklaish AF, Walsh TR, Tyrrell JM (2018) Clinical validation of SensiTest Colistin, a broth microdilution-based method to evaluate colistin MICs. J Clin Microbiol 56
Caselli E, D’Accolti M, Soffritti I, Piffanelli M, Mazzacane S (2018) Spread of mcr-1-driven colistin resistance on hospital surfaces, Italy. Emerg Infect Dis 24:1752–1753
Clinical and Laboratory Standards Institute (CLSI) (2020) Performance standard for antimicrobial susceptibility testing, 30th edn. Clinical and Laboratory Standards Institute, CLSI Standard M100, Wayne, PA
Collingwood C, Kemmett K, Williams N, Wigley P (2014) Is the concept of avian pathogenic Escherichia coli as a single pathotype fundamentally flawed? Front Vet Sci 1:5
Cummins ML, Reid CJ, Chowdhury PR, Bushell RN, Esbert N, Tivendale KA et al (2017) Whole genome sequence analysis of Australian avian pathogenic Escherichia coli that carry the class 1 integrase gene. Microb Genom 5(2):e000250
Dominguez JE, Redondo LM, Figueroa Espinosa RA, Cejas D, Gutkind GO, Chacana PA, Di Conza JA, Fernández Miyakawa ME (2018) Simultaneous carriage of mcr-1 and other antimicrobial resistance determinants in Escherichia coli from poultry. Front Microbiol 9:1679
Drali R, Berrazeg M, Zidouni LL, Hamitouche F, Abbas AA, Deriet A, Mouffok F (2018) Emergence of mcr-1 plasmid-mediated colistin-resistant Escherichia coli isolates from seawater. Sci Total Environ 642:90–94
Ewers C, Li G, Wilking H, Kiessling S, Alt K, Antáo EM et al (2007) Avian pathogenic, uropathogenic, and newborn meningitis-causing Escherichia coli: how closely related are they? Int J Med Microbiol 297:163–176
Falgenhauer L, Waezsada S, Gwozdzinski K, Ghosh H, Doijad S, Bunk B, Spröer C et al (2016) Chromosomal locations of mcr-1 and blaCTX-M-15 in fluoroquinolone-resistant Escherichia coli ST410. Emerg Infect Dis 22(9):1689–1691
Gelbíčová T, Baráková A, Florianová M, Jamborová I, Zelendová M, Pospíšilová L, Koláčková I, Karpíšková R (2019) Dissemination and comparison of genetic determinants of mcr-mediated colistin resistance in enterobacteriaceae via retailed raw meat products. Front Microbiol 10:2824. https://doi.org/10.3389/fmicb.2019.02824
Hornsey M, Betts JW, Mehat JW, Wareham DW, van Vliet AHM, Woodward MJ, La Ragione RM, (2019) Characterization of a colistin-resistant avian pathogenic Escherichia coli ST69 isolate recovered from a broiler chicken in Germany. J Med Microbiol 68:111–114
Hunter PR, Wilkinson DC, Catling LA, Barker GC (2008) Meta-analysis of experimental data concerning antimicrobial resistance gene transfer rates during conjugation. Appl Env Microbiol 74(19):6085–6090
Ibrahim RA, Cryer TL, Lafi SQ, Basha E, Good L, Tarazi YH (2019) Identification of Escherichia coli from broiler chickens in Jordan, their antimicrobial resistance, gene characterization and the associated risk factors. BMC Vet Res 15:159
Kaper J, Nataro J, Mobley H (2004) Pathogenic Escherichia coli. Nat Rev Microbiol 2:123–140. https://doi.org/10.1038/nrmicro818
Koutsianos D, Athanasiou L, Mossialos D, Koutoulis K (2021) Colibacillosis in poultry: a disease overview and the new perspectives for its control and prevention. J Hellenic Vet Med Soc 71(4):2425–2436
Le Devendec L, Jouy E, Paboeuf F, de Boisséson C, Lucas P, Drider D, Kempf I (2018) Development of a pig infection model with colistin-resistant Escherichia coli. Vet Microbiol 226:81–88
Lee JW (2019) Protocol measuring horizontal gene transfer from algae to non-photosynthetic organisms. MethodsX 6:1564–1574
Lentz SA, de Lima-Morales D, Cuppertino VM, Nunes Lde S, da Motta AS, Zavascki AP, Barth AL, Martins AF (2016) Letter to the editor: Escherichia coli harbouring mcr-1 gene isolated from poultry not exposed to polymyxins in Brazil. Eurosurveil 21(26):30267
Loayza-Villa MF, Salinas L, Tijet N, Villavicencio F, Trujillo R, Salas S, Rivera R, Villacís J, Satan C, Uchina L, Muñoz O, Zurita J, Melano R, Reyes J, Trueba G (2019) Diverse Escherichia coli isolates from domestic animal in the same Ecuadorian household all carry the colistin resistance gene mcr-1.1. J Glob Antimicrob Resist S2213–7165(19):30316–30319
Lim S-K, Kang HY, Lee K, Moon D-C, Lee H-S, Jung S-C (2016) First detection of the mcr-1 gene in Escherichia coli isolated from livestock between 2013 and 2015 in South Korea. Antimicrob Agents Chemother 60:6991–6993
Lima Barbieri N, Nielsen DW, Wannemuehler Y, Cavender T, Hussein A, Yan SG, Nolan LK, Logue CM (2017) mcr-1 identified in avian pathogenic Escherichia coli (APEC). PLoS One 12:e0172997
Liu Y, Wang Y, Walsh TR, Yi L, Zhang R, Spencer J, Doi Y, Tian G, Dong B, Huang X et al (2016) Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lanc Infect Dis 16:161–168
Liu BT, Li X, Zhang Q, Shan H, Zou M, Song FJ (2019) Colistin-resistant mcr-positive Enterobacteriaceae in fresh vegetables, an increasing infectious threat in China. Int J Antimicrob Agents 54:89–94
Liu J, Liao T, Huang W, Liu Y, Wu K, Lauderdale T, Tsai S, Kuo S, Kuo H (2018) Increased mcr-1 in pathogenic Escherichia coli from diseased swine. Taiwan, J Microbiol Immunol Infect. https://doi.org/10.1016/j.jmii.2018.10.011
Liu Y, Liu J-H (2018) Monitoring colistin resistance in food animals, An urgent threat. Exp Rev Anti Infect Ther 16:443–446
Maamar E, Alonso CA, Hamzaoui Z, Dakhli N, Abbassi MS, Ferjani S, Saidani M, Boutiba-Ben Boubaker I, Torres C (2018) Emergence of plasmid-mediated colistin-resistance in CMY-2-producing Escherichia coli of lineage ST2197 in a Tunisian poultry farm. Int J Food Microbiol 269:60–63
Matsumura Y, Peirano G, Pitout JDD (2018) Complete genome sequence of Escherichia coli J53, an azide-resistant laboratory strain used for conjugation experiments. Genome Announc 6:e00433-e518
McGann P, Snesrud E, Maybank R, Corey B, Ong AC, Clifford R, Hinkle M, Whitman T, Lesho E, Schaecher KE (2016) Erratum for McGann et al., Escherichia coli harboring mcr-1 and blaCTX-M on a novel IncF plasmid: first report of mcr-1 in the United States. Antimicrob Agents Chemother 60:5107
Manges AR, Geum HM, Guo A, Edens TJ, Fibke CD, Pitout JDD (2019) Global extraintestinal pathogenic Escherichia coli (ExPEC) lineages. Clin Microbiol Rev 32:e00135-e218
Neill JO’ (2014) Antimicrobial resistance: tackling a crisis for the health and wealth of nations. The review on antimicrobial resistance chaired. http://www.amr-review.org/Publications. Accessed 7 Nov 2021
Nolan LK, Vaillancourt JP, Barbieri NL, Logue CM (2020) Colibacillosis. In: Swayne DE, Boulianne M, Logue CM, McDougald LR, Venugopal N, Ames SD (eds) Diseases of poultry, 14th edn. Wiley and Sons, IW. https://doi.org/10.1002/9781119371199.ch18
Okorafor ON, Anyanwu MU, Nwafor EO, Anosa GN, Udegbunam RI (2019) Multidrug-resistant enterobacteria colonize commercial day-old broiler chicks in Nigeria. Vet World 12(3):418–423
Perreten V, Strauss C, Collaud A et al (2016) Colistin resistance gene mcr-1 in avian-pathogenic Escherichia coli in South Africa. Antimicrob Agents Chemother 60:4414–4415
Potron A, Poirel L, Nordmann P (2014) Derepressed transfer properties leading to the efficient spread of the plasmid encoding carbapenemase OXA-48. Antimicrob Agents Chemother 58:467–471
Quesada A, Ugarte-Ruiz M, Iglesias MR, Porrero MC, Martínez R, Florez-Cuadrado D, Campos MJ, García M, Píriz S, Sáez JL, Domínguez L (2016) Detection of plasmid mediated colistin resistance (MCR-1) in Escherichia coli and Salmonella enterica isolated from poultry and swine in Spain. Res Vet Sci 105:134–135
Saidani M, Messadi L, Chaouechi A, Tabib I, Saras E, Soudani A, Daaloul-Jedidi M, Mamlouk A, Ben Chehida F, Chakroun C, Madec J-Y, Haenni M (2019) High genetic diversity of Enterobacteriaceae clones and plasmids disseminating resistance to extended-spectrum cephalosporins and colistin in healthy chicken in Tunisia. Microb Drug Res. https://doi.org/10.1089/mdr.2019.0138
Schwarz S, Loeffler A, Kadlec K (2017) Bacterial resistance to antimicrobial agents and its impact on veterinary and human medicine. Vet Dermatol 28(1):82-e19
Shen Y, Lv Z, Yang L, Liu D, Ou Y, Xu C, Liu W, Yuan D, Hao Y, He J et al (2019) Integrated aquaculture contributes to the transfer of mcr-1 between animals and humans via the aquaculture supply chain. Env Int 130:104708
Sun J, Li XP, Yang RS, Fang LX, Huo W, Li SM, Jiang P, Liao XP, Liu YH (2016) Complete nucleotide sequence of an incI2 plasmid coharboring blaCTX-M-55 and mcr-1. Antimicrob Agents Chemother 60(8):5014–5017
Tendon Valérie D, Laurent P, Patrice N (2017) Transferability of the mcr-1 colistin resistance gene. Microb Drug Resist 23(7):813–814
Valiakos G, Kapna I (2021) Colistin resistant mcr genes prevalence in livestock animals (swine, bovine, poultry) from a multinational perspective. A Systematic Review Vet Sci 8:265. https://doi.org/10.3390/vetsci8110265
van Duijkeren E, Schink AK, Roberts MC, Wang Y, Schwarz S (2018) Mechanisms of bacterial resistance to antimicrobial agents. Microbiol Spect 6(1)
Van Eck JHH, Goren E (1991) An Ulster 2C strain-derived Newcastle disease vaccine: vaccinal reaction in comparison with other lentogenic Newcastle disease vaccines. Avian Pathol 20:497–507
Veldman K, van Essen-Zandbergen A, Rapallini M, Wit B, Heymans R, van Pelt W, Mevius D (2016) Location of colistin resistance gene mcr-1 in Enterobacteriaceae from livestock and meat. J Antimicrob Chemother 71(8):2340–2342
Yamaguchi T, Kawahara R, Harada K, Teruya S, Nakayama T, Motooka D, Nakamura S, Do Nguyen P, Kumeda Y, Van Dang C (2018) The presence of colistin resistance gene mcr-1 and -3 in ESBL producing Escherichia coli isolated from food in Ho Chi Minh City, Vietnam. FEMS Microbiol Lett 365(11). https://doi.org/10.1093/femsle/fny100
Yamaji R, Friedman CR, Rubin J, Suh J, Thys E, McDermott P, Hung-Fan M, Riley LW (2018) A population-based surveillance study of shared genotypes of Escherichia coli isolates from retail meat and suspected cases of urinary tract infections. mSphere 3(4):e00179–18
Yang Y-Q, Li Y-X, Song T, Yang Y-X, Jiang W, Zhang A-Y, Guo X-Y, Liu B-H, Wang Y-X, Lei C-W, Xiang R, Wang H-N (2017) Colistin resistance gene mcr-1 and its variant in Escherichia coli isolates from chickens in China. Antimicrob Agents Chemother 61:e01204-e1216
Yang Y, Zhang A, Ma S, Kong L, Li Y, Liu J, Davis MA, Guo X, Liu B, Lei C, Wang H (2016) Co-occurrence of mcr-1 and ESBL on a single plasmid in Salmonella enterica. J Antimicrob Chemother 71(8):2336–2338
Yin W, Li H, Shen Y, Liu Z, Wang S, Shen Z, Zhang R, Walsh TR, Shen J, Wang Y (2017) Novel plasmid-mediated colistin resistance gene mcr-3 in Escherichia coli. mBio 8:e00543–17
Acknowledgements
The authors are grateful to Edoardo Carretto, Head of Clinical Microbiology Laboratory, IRCCS Arcispedale S. Maria Nuova, AUSL Reggio Emilia, Italy, for the molecular characterization of the isolates. They are also grateful to Dr. José Di Conza of Faculty of Pharmacy and Biochemistry, Buenos Aires, Argentina, for providing the E. coli J53 used in the transferability study. They equally appreciate Dr. Remigius I. Onoja and Dr. (Mrs) Chinwe J. Aronu of the Faculty of Veterinary Medicine, University of Nigeria, for their animal houses used in the study. No grant was made available for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The handling of the birds used in this study was done humanely in accordance with the revised version of the Animals Scientific Procedures Act of 1986 for the care and use of animals for research purposes as approved by the Institutional Animal Care and Use Committee (IACUC) of the Faculty of Veterinary Medicine, University of Nigeria.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anyanwu, M.U., Anyogu, D.C., Chah, K.F. et al. Mobile colistin resistance (mcr-1) gene-positive Escherichia coli from chickens in Nigeria is potentially pathogenic and transfers colistin resistance to other organisms. Comp Clin Pathol 31, 323–332 (2022). https://doi.org/10.1007/s00580-022-03336-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-022-03336-2