Abstract
One of the least common malignant ovarian tumors detected during pregnancy is dysgerminoma. The association between creation dysgerminoma and pregnancy was controversial. We present here a rare and interesting case of dysgerminoma during pregnancy with literature review. A 29-year-old healthy pregnant woman presented with an acute progressive abdominal pain. The patient underwent laparotomy and left salpingo oophorectomy. A diagnosis of dysgerminoma (FIGO stage IA) was made. She had uneventful postoperative period. She referred for subsequent chemotherapy. The surgeons and radiologists, particularly at major referral emergency centers, are much more likely to be acquaint with ovarian dysgerminoma, as a solid nonhomogenous pelvic mass discovered by ultra-sonography in pregnant woman and its clinical awareness, because any misdiagnosis can delay the start of an appropriate and adequate management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian tumors are broadly classified into three types based on their origin, epithelial, sex cord, and germ cell tumors. While epithelial variety largely predominates, germ cell tumors (GCTs) are rare, comprising about 30% of all ovarian neoplasms and 3% of all ovarian malignancies (Zalel et al. 1996). Ovarian germ cell tumors, derived from the primordial germ cells, are further divided into subgroups based on the histological features. Mature teratoma being the commonest benign variety while dysgerminoma is the commonest malignant germ cell tumor (Zaloudek 1994).
The occurrence of ovarian masses during pregnancy period is common finding; of course, many of them are functional follicular originated cysts (Machado et al. 2007). Exact prevalence of ovarian masses during pregnancy is 0.1–2%. Detection of malignant ovarian tumor during malignancy is a very exceptional event (Leiserowitz et al. 2006) and is representative this fact that, incidence of malignant ovarian tumors in young subjects is low. After uterus cervix invasive carcinoma, ovarian malignancy is the most common gynecological malignancy during pregnancy period (Oheler et al. 2003).
Similar to non-pregnant age adjacent individual, during pregnancy period, germ cell tumors largely predominates. In this group, dysgerminomas and malignant teratomas are more prevalent and sex cord tumor category is rare (Zanotti et al. 2000; Zhao et al. 2006).
In pregnant patient, the clinical presentation of ovarian malignancies as an acute abdomen is very exceptional but important. The coexistence of an ovarian mass, acute surgical abdomen, and an intra-uterine pregnancy presents significant challenges for differential diagnosis. In this situation, except invasive surgical procedure, laparotomy, another noninvasive imaging investigations including ultra-sonography, computed tomography (CT), and magnetic resonance imaging (MRI), accompanied with clinical/laboratory studies, help to us for limitation of differential diagnosis but not definite diagnosis. Because one of them are subsidiary ability for precise detection of true nature of lesions. We present here a rare and interesting case of dysgerminoma during pregnancy presented with acute abdominal pain and literature review.
Case presentation
Patient is a 29-year-old healthy pregnant woman (G3P2L2) who presented with an increasing continuous acute abdominal pain in the left lower quadrant for 2 hours associated with abdominal distension, marked decreased of bowel motility, and no gas passage to the emergency room at our Hospital. During the pregnancy, she suffered from spotting and increasing of abdominal pain with urinary frequency. She denied any gastrointestinal tract-associated symptoms or weight loss. Two previous pregnancies were uneventful with normal vaginal delivery. There were not any significant past medical or surgical history. Also, there was not any family history of gynecologic malignancy in her first-degree relative.
On physical examination, she looked mildly pale with satisfactory general condition. Uterus size was 21 weeks. With one live fetus in longitudinal lie with cephalic presentation.
The patient’s abdominal pelvic physical examination revealed abdominal distension, marked decreased of bowel sound, and rebound tenderness with left flank fullness. There was a large mass measuring 10.5 × 10 × 9.5 cm. It has palpated distinct from the uterus in the left hypochondrium. Her baseline laboratory findings were all within normal range except anemia (her hemoglobin was 9.4 mg/dL) and mild leukocytosis.
Ultra-sonography examination revealed a large abdominopelvic heterogeneous mobile solid mass, measuring 9.5 × 9.3 × 5 cm in the left aspect of uterus with scant amount of ascites. The main differential diagnosis was twisted and incarcerated sarcomatous or fibromatosis lesion of mesentery and unusual leiomyoma.
Pelvic magnetic resonance imaging (MRI) without enhancement media showed a solid mass with lobulated contour in the posterior pelvic cavity, occupied the Douglas pouch with bone formation, calcification, and fat, suggestive for cystic teratoma.
The liver, uterus, and contra lateral ovary were normal. Periaortic and retroperitoneal lymphadenopathy were not found. The omentum was normal looking. Mild ascites was found in pelvic cavity.
Serum lactate dehydrogenase (LDH) level was elevated at 449 IU/L and CA-125 was normal limit (14.7 U/mL) and alpha feto-protein (AFP) also was elevated, 85.8 IU/mL (despite adjusted for gestational age).
The patient underwent laparotomy and left salpingo oophorectomy. At the time of the laparotomy, the mass shown early stage of torsion and frozen sections examination of mass reported solid unspecified malignancy, suggestive for germ cell tumor. And advised for wait to permanent. During the surgery, the uterus, right ovary, fallopian tubes, omentum, liver, intestine, and peritoneum have shown unremarkable, grossly.
Grossly, the resection left ovary converted into an encapsulated lobulated mass, 10.5 cm in diameter with smooth external surface and patchy brown discoloration (twisted). Cut surfaces shown multi-nodular solid quality and tan color homogeneous rubbery tissue with patchy brown discoloration. The left fallopian tube, M 7 × 1 cm with brown discoloration associated a paratubal cyst 0.5 cm in diameter.
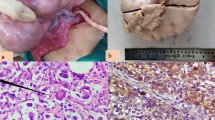
Histopathological review of resected ovarian mass revealed congested/hemorrhagic malignant infiltrative neoplasm in sheets, well-defined nests, or trabeculae growth pattern were separated by fibrous strands (Fig. 1).
And infiltrated by lymphocytes. Individual tumoral cells were uniform and had large squared off vesicular nuclei, one or more prominent elongated nucleoli, and abundant clear too finely granular cytoplasm with distinct cell borders (Fig. 2). Mitotic activity was found. Abortive yolk sac elements are present less than 7% in examined sections. Capsular invasion was found in examined sections.
A diagnosis of dysgerminoma (Federation of Obstetrics and Gynecology stage IA), FIGO stage IA, was made, straightforward. There was no evidence of malignant cells in cytopathology examination of the peritoneal fluid. She had uneventful postoperative period. She was referred to oncology multidiscipline center for adjuvant chemotherapy. During 3 years of follow-up, she had uneventful post chemotherapy period. Also, she had a healthy pregnancy following chemotherapy.
Conclusion
The coexistence ovarian malignancy in pregnant women is exceptional event. In few instances, its clinical presentation is serious and danger. These tumors may twist encircling them stalk, hemorrhage from traumatized/congested superficial neoplasm vascular channels, therefore them present as acute surgical abdomen. In these situations, for better patient management and attain best outcome, as soon as detection and optimal therapy are essential (Varras et al. 2004). The most common type of germ cell tumor is dysgerminoma. Dysgerminoma initiated by primordial germ cells escapes from primordial follicles of the embryonic gonads and in additional to survival, they had significant proliferation. On histopathology examination, growth pattern of dysgerminoma was similar to primitive gonad (Shaaban et al. 2014). The main differential diagnoses of an adnexal painful mass and acute abdominal pain in a childbearing age female are as follows: ectopic pregnancy, hemorrhagic or perforated or twisted corpus luteal, follicular and paratubal cyst, chocolate cyst, and pedunculated—twisted-infarcted adnexal leiomyoma (Jain et al. 2013).
Many researchers shown occurrence of denevo ovarian malignancies were usual in young low parity women in reproductive age (Jubb 1963). Recently, especially in developing and developed countries, age of mother in first pregnancy was significantly increased, and occurrence of pregnancy in mothers older than 30 and 40 years were raised, significantly.
Therefore, it is not specified, whether development of ovarian malignant tumor in pregnancy period is raising (Matsuyama et al. 1989), or tendency to pregnancy and childbearing in old age is accepted (Agrawal et al. 2012). This general interest causes increase of development of ovarian malignant tumor during to pregnancy period (Leslie 2002; Ferrandina et al. 2005; Méndez et al. 2003).
For conserving of ovulation and resulting fertility in young women, conservative surgery with adjuvant chemotherapy is chosen (Roberts and Oranye 2013). The ovarian dysgerminoma, FIGO stage IA, and cure rates can reach to 100%. In these cases, chemotherapy effect on menstrual cycle, pregnancy, or bearing children is nil (Zhang et al. 2012). The recurrence of ovarian dysgerminoma is exceptional event (Al-Sayed et al. 2011).
References
Agrawal A, Rijal P, Pokharel H, Karki S, Basnet P, Dahal P (2012) Ovarian dysgerminoma: unusual presentation in pregnancy with acute abdomen due to internal hemorrhage. NJOG 7(3):53–55
Al-Sayed MM, El-Sayed AA, El-Barbary TM et al (2011) Conservative surgery in patients with malignant ovarian gem cell tumours. J Egypt Soc Parasitol 41:737–744
Ferrandina G, Distefano M, Testa A, De Vincenzo R, Scambia G (2005) Management of advanced ovarian carcinoma at 15 weeks of gestation: case report and literature review. Gynecol Oncol 97:693–696
Jain M, Budhwani C, Jain AK, Hazari RA (2013) Pregnancy with ovarian dysgerminoma: an unusual diagnosis. J of dental and Medical Sciences 11(5):53–57
Jubb ED (1963) Primary ovarian cancer in pregnancy. Am J Obstet Gynecol 85:345–354
Leiserowitz GS, Xing G, Cress R, Brahmbhatt B, Dalrymple JL, Smith LH (2006) Adnexal masses in pregnancy: how often are they malignant? Gynecol Oncol 101:315–321
Leslie KK (2002) Chemotherapy and pregnancy. Clin Obstet Gynecol 45:153–164
Machado F, Vegas C, Leon J, Perez A, Sanchez R, Parrilla JJ et al (2007) Ovarian cancer during pregnancy: analysis of 15 cases. Gynecol Oncol 105:446–450
Matsuyama T, Tsukamoto N, Matsukuma K, Kamura T, Kaku T, Saito T (1989) Malignant ovarian tumors associated with pregnancy: report of six cases. Int J Gynaecol Obstet 28:61–66
Méndez LE, Mueller A, Salom E, González-Quintero VH (2003) Paclitaxel and carboplatin chemotherapy administered during pregnancy for advanced epithelial ovarian cancer. Obstet Gynecol 102:1200–1202
Oheler MK, Wain GV, Brand A (2003) Gynaecological malignancies in pregnancy: a review. Aust N Z J Obstet Gynaecol 43:414–420
Roberts OA, Oranye BC (2013) Ovarian dysgerminoma in an adolescent: a case report. Afr J Med Med Sci 42:197–200
Shaaban AM, Rezvani M, Elsayes KM et al (2014) Ovarian malignant germ cell tumors: cellular classification and clinical and imaging features. Radiographics 34:777–801
Varras M, Tsikini A, Polyzos D, Samara C, Akrivis C (2004) Internal hemorrhage caused by a twisted malignant ovarian dysgerminoma: ultrasonographic fi ndings of a rare case and review of the literature. Clin Exp Obstet Gynecol 31(1):73–78
Zalel Y, Piura B, Elchalal U, Czernobilsky B, Antebi S, Dgani R (1996) Diagnosis and management of malignant germ cell ovarian tumors in young females. Int J Gynaecol Obstet 55:1–10
Zaloudek C (1994) The ovary. In: Gompel C, Silverberg SG (eds) Pathology in gynecology and obstetrics. JB Lippincott Co, Philadelphia, pp 379–397
Zanotti KS, Belinson JL, Kennedy AW (2000) Treatment of gynaecologic cancers in pregnancy. Semin Oncol 27:686–698
Zhang R, Sun YC, Zhang GY et al (2012) Treatment of malignant ovarian germ cell tumours and preservation of fertility. Eur J Gynaecol Oncol 33:489–492
Zhao XY, Huang HF, Lian LJ, Lang JH (2006) Ovarian cancer in pregnancy: a clinicopathologic analysis of 22 cases and review of the literature. Int J Gynecol Cancer 16:8–15
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from patient included in the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Samiee-rad, F., Zangivand, A.A. The coexistence of ovarian dysgerminoma and normal intra-uterine pregnancy presented with acute abdominal pain. Comp Clin Pathol 27, 257–260 (2018). https://doi.org/10.1007/s00580-017-2592-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-017-2592-2