Abstract
Hepatocellular carcinoma (HCC) is the most common type of liver cancer, where the risk of its development is always multifactorial. Human interleukin-6 (IL-6) is a pro-inflammatory cytokine that plays a crucial role in the regulation of immune response and defense against viral infection; it was hypothesized that this cytokine may participate in the process of liver damage. The aim of our study was to investigate IL-6-572 C/G gene polymorphism in patients with HCC as compared with healthy controls in an Egyptian population, in order to see if there is a significant association between IL-6 gene polymorphism and susceptibility to HCC development. A total of 165 subjects divided into 55 HCV, 60 HCC, and 50 healthy subjects were enrolled in the study for evaluation. Genomic DNA was extracted from the peripheral blood, and genotyping was performed using RT-multiplex PCR (real-time multiplex polymerase chain reaction) methodology. G/C, G/G, and C/C frequencies in HCV patients were 16.4, 78.2, and 5.5%, respectively; furthermore, the frequencies were 18.3, 75.0, and 6.7% in HCC patients, and 28.0, 62.0, and 10.0% in the control group, respectively. The frequencies of G and C alleles in HCV patients were 86.4 and 13.6% and in HCC patients were 84.2 and 15.8% while in the control group, the frequencies were 76.0 and 24.0%, respectively. There was no significant difference between the studied groups regarding G/C, G/G, and C/C frequencies or G and C allele’s frequencies. IL-6-572 promoter gene polymorphism is neither associated with HCV infection nor with development of HCC. Further studies including bigger sample size are suggested.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is considered the fifth most common cancer worldwide (Dhir et al. 2016); nowadays, it is known to be the second global cause of cancer-related mortality. The tumor progression is fairly silent; hence, patients used to suffer late symptoms and clinical signs (Kim et al. 2016). Development of HCC is attributed to multiple factors such as hepatitis B virus, hepatitis C virus, aflatoxin, alcoholism, and smoking, yet it is most frequently seen in patients with hepatic cirrhosis (Zhu et al. 2007). To date, there is a mounting prevalence and a well-documented bond between HCC and various chronic inflammatory factors exemplified in different cytokines (Caglevic et al. 2016).
HBV and HCV are the chief offenders of HCC in Eastern Mediterranean Region countries and the Middle East; hence, their prevalence necessitated application of different strategies to tackle them accordingly. A systemic review done by Alavian and Haghbin (2016) showed that HCV-related HCC are very common in North African nations. In Egypt, hepatitis C is acknowledged as the most endemic viral infection with the uppermost prevalence rate in the world embracing a major health problem in the country (Elgharably et al. 2017). In 2008, 15% of the Egyptian population were categorized as seropositive, 10% were chronically infected, in addition to 90% infected with genotype 4. Lately, the seropositivity of HCV infection has dropped to 6.3% amid the studied Egyptian population which in turn has led to an approximate 30% decline in its prevalence between 2008 and 2015 (El-Akel et al. 2017). Currently, the government is working on monitoring the blood product processing in addition to tailoring more stringent laws regarding compensated donors especially injection drug users.
Different cytokines play key roles in the regulation of immune response and defense against viruses; a study by Lu et al. (2014) has revealed that the amount of cytokine production in various diseases is related to polymorphisms affecting the cytokine genes.
IL-6 is a multifunctional cytokine that is recently known to be an important constituent of cancer-associated cytokine complex which ultimately results in both a systemic immune stimulation together with cancer-induced immune suppression that eventually protects the cancer cells (Lippitz and Harris, 2016). Recently, IL-6 has been intensively studied, as increased levels of IL-6 have been detected in HCC patients’ serum (Lippitz and Harris, 2016).
IL-6 gene is located on the short arm of chromosome number 7, and it consists of five exons and four introns (Zhang et al. 2014). Polymorphisms in IL-6 promoter region were shown to be implicated in the pathogenesis of several immune-mediated diseases such as ankylosing spondylitis, psoriatic arthritis, Behcet’s disease, inflammatory bowel disease, and allergy. It was also proved to be involved in many cardiovascular, neuromuscular, and infectious diseases (Argiles et al. 2006).
Although the relation between IL-6 and HCC development is still unclear yet several studies have revealed that HCC progression is solely dependent on the extend of liver inflammation, hence, the balance between pro-inflammatory and anti-inflammatory cytokines is the key ingredient for controlling the disease progression; this means that IL-6 gene polymorphism could result in disturbance in this balance and development of the disease (Sghaier et al. 2017).
Despite various independent studies, the relation between IL-6 and cancer development is still in its infantile stage since there has not been a comprehensive cross-reference and/or systematic analysis made for solid establishment of an oncological concept for its role (Lippitz and Harris, 2016).
In this study, we needed to explore the correlation between IL-6 (rs 1800796) polymorphism and HCC susceptibility using real-time PCR (RT-PCR) by adopting a case-control design for implementation of proper detection of significant difference between the studied groups.
Subjects and methods
Study population and demographic information
Our study was conducted in the Tropical Medicine department at Theodor Bilharz Research Institute (TBRI) where 165 subjects were enrolled and divided into three groups; group A involved 55 patients diagnosed with HCV while group B constituted 60 patients with established diagnosis of HCC on top of chronic hepatitis C infection. Lastly, group C involved 50 healthy age- and sex-matched individuals who served as a control group. HCV patients were diagnosed by assessing HCV Ig G antibodies using enzyme-linked immunosorbent assay (ELISA) as well as detection of HCV RNA by RT-PCR; moreover, diagnosis of HCC occurrence was confirmed by CT scan and MRI radiological techniques. Exclusion criteria were made to eliminate those with HBV comorbidity, schistosomiasis, alcohol consumption, or antiviral therapy from the study. An informed consent was obtained from patients who participated in the study. Moreover, the procedures used were approved by TBRI ethics committee according to Helsinki Declaration.
Group A “HCV patients” was subdivided into 26 (46.7%) males and 29 (53.3%) females, and their age ranged from 34 to 67 years (mean ± SD = 44.3 ± 13.9). In group B “HCC patients,” there were 42 (70%) males versus 18 (30%) females with age ranged from 48 to 60 years (mean ± SD = 46.8 ± 15.9). Furthermore, group C included 40 (80%) males and 10 (20%) females with their age ranged from 32 to 57 years (mean ± SD = 46.7 ± 13.3).
Genomic DNA extraction
Genomic DNA was obtained using the QIAamp DNA Mini Kit (Qiagen; catalog no.: 51104). Five-milliliter peripheral venous whole blood was collected in a sterile vacuum tube containing EDTA for genomic DNA extraction by means of standard protocol using proteinase K. Lysis of red blood cells was done three times using lysis buffer. Afterwards, sodium dodecyl sulfate (SDS) 10% and 10 μl proteinase K in the presence of guanidine HCL were added to treat the remaining white cells for a short incubation time (10 min at 56 °C) in order to inactivate all nucleases. Cellular nucleic acids then bind to a special glass fibers pre-packed in high pure purification filter tube, and a series of “wash and spin” steps were executed using 500 μl buffer AW1 and 500 μl buffer AW2 for getting rid of PCR impurities. Finally, elution buffer (200 μl buffer AE) was added, and incubation was done for 1 min at 15–25 °C to release the nucleic acid from the glass fiber.
IL-6 genotyping
IL-6 C/G gene polymorphism (rs 1800796) was detected using Taq Man SNP genotyping assay. This assay consists of a single, ready to use tube that contain two sequences—specific primers for amplifying the polymorphism of interest together with two allele-specific Taq Man minor groove binder (MGB) probes for detecting the alleles for the specific polymorphism of interest. Each probe has a reporter dye; VIC dye is linked to the 5′ end of allele C probe while FAM dye is linked to the 5′ end of allele G probe. Each PCR reaction contained 2.5 μl of diluted DNA (5 ng/μl), 12.5 μl of ×2 TaqMan Universal PCR Master Mix, 1.25 μl of ×20 TaqMan SNP Genotyping Assay Mix, and 8.75 μl of distilled water (DW). This PCR reaction was carried out in a thermal cycler using ABI 7500, with the following programs shown in Table 1.
Finally, a threshold is set at 0.1 for analysis, using ABI Prism “genetic analyzer.” This comprises quantitation of the amplified PCR product (DNA fragments) as well as determining the size of the fragments by comparing them to fragments contained in a size standard.
Statistical analysis
The data was analyzed using Microsoft Excel 2010 and statistical program for social science (SPSS version 22.0) for windows (SPSS IBM., Chicago, IL). Continuous normally distributed variables were represented as mean ± SD with 95% confidence interval, in addition to using the alleles and genotype frequencies and percentage for categorical and non-parametric variables; p value of less than 0.05 was considered statistically significant. The Student’s t test was performed to compare the means of normally distributed variables between groups. ANOVA followed by Tukey-Kramer as a post hoc test in multigroups and χ2 test or Fisher’s exact test were used to determine the distribution of categorical variables between groups.
Results
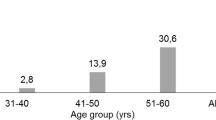
The results obtained in this study showed that there was a difference in allele frequencies between patients with HCV and control group (p = 0.1). Moreover, there was a difference between allele frequencies between HCC and control group (p = 0.3), though these differences were insignificant. G allele was remarkably “yet insignificantly” frequent among HCV and HCC patients (86.4 and 84.2%, respectively) compared to the healthy individuals (76.0%); on the other hand, C allele frequency was similar amid all the studied groups. In addition, the G/G genotype was more frequent among HCV patients (78.2%) and HCC patients (75.0%) in comparison with the control subjects (62.0%) while the frequency of C/C genotype was low among HCV patients (5.5%), HCC patients (6.7%), and controls (10.0%). Data are presented in Table 2 and Fig. 1.
Discussion
Being the leading cause of HCC, HCV-induced HCC could now be established through many genomic studies that reveal direct as well as indirect mechanisms serving in the interaction between the immune and the metabolic systems; this was done via identifying polymorphisms as regards immune, metabolic, and growth-signaling systems which may increase the risk of HCC development (Goossens et al., 2015).
The pathogenesis of HCV-induced HCC is a multistep process that typically develops within 20 to 40 years; these steps could be summarized in creation of chronic HCV infection coupled with hepatic inflammation, advanced liver fibrosis, induction of neoplastic clones together with permanent somatic genetic/epigenetic mutation, and ultimately formation of carcinogenic tissue microenvironment with progression of these neoplastic clones (Hoshida et al. 2014).
A number of studies have been recently interested in assessing the relationship between various interleukin gene polymorphisms and occurrence of HCV-induced HCC development (Zhou et al. 2017; Shi et al. 2016; Chen et al. 2016; and Zhu et al. 2016). The aim of our study was to validate the association of IL-6 gene polymorphism with HCV infection and HCC incidence. This was done through assessing 55 HCV patients and 60 HCC patients against 50 healthy controls using RT-PCR.
IL-6 is a pro-inflammatory cytokine proved to be the key player in initiation of immune response via secretion of acute phase reactants and proliferation of lymphocytes (Dondeti et al. 2016); however, more studies are required for establishing the link of IL-6 between inflammation response and liver carcinogenesis (Hsia et al. 2007), since IL-6 was implicated in apoptosis inhibition as well as initiation of metastasis (Prieto, 2008). Moreover, many studies have found an association between IL-6 and liver fibrosis and cirrhosis (Dondeti et al. 2016).
IL-6 gene is located on chromosome 7p21 with a length of 5 kbp; it has five exons with four introns interposing them (Kishimoto, 2005). To date, many researches were directed towards studying the following genetic IL-6 polymorphisms that lie in its promoter region (-597G/A, -373A/T, -174G/C, and -572G/C). These studied SNPs are characterized by strong linkage disequilibrium; thus, they retain a significant impact on IL-6 transcription, and therefore, the amount of the cytokine produced (Tang et al. 2014).
In our study, we found no significant difference in the frequency of G/C, G/C, and C/C between HCV patients, HCC patients, and the control group. There was a higher frequency of G allele among HCV and HCC patients (86.4 and 84.2%, respectively) in comparison to the healthy individuals (76.0%), yet this finding was insignificant. These findings can conclude that IL-6-572 G>C polymorphism could not be intensely associated with HCC susceptibility.
Moreover, Cussigh et al. (2011) has confirmed that there is no link between IL-6-572 promoter gene polymorphism and HCC occurrence; in addition, it emphasized the role of -174 and -597 gene polymorphisms as two unfavorable haplotypes serving in accelerating the disease progression.
Another study by Bei et al. (2014) was done to investigate the effect of six SNPs of different cytokines (IL-2, IFN-γ, IL-1β, IL-6, and IL-10) on HCC development; it demonstrated that none of these SNPs were recognized to cause an influence on HCC development when evaluated individually; however, the combined effect of these six SNPs on HCC risk was significantly pronounced.
Furthermore, a meta-analysis has been executed by Liu et al. (2014) on IL-6 gene polymorphism and risk of HCC development, showing that most of the relevant studies concluded that IL-6-174 G/C, but not -572 G/C polymorphism could lead to HCC predisposition.
Nonetheless, a current study by Sghaier et al. (2017) validated that IL-6-572 G/G genotype was more frequent in HCV patients compared to HCC patients, which was contradicting with our results that showed no difference between HCV and HCC patients.
On the contrary, some studies have concluded a potential role of IL-6-572 G/C genotype polymorphism in development and pathogenesis of HBV (Saxena et al. 2014; Chang et al. 2015).
In conclusion, IL-6-572 promoter gene polymorphism might not be a useful determinant in predicting the outcome of HCV infection or HCC susceptibility. This influences the ultimate role of HCV in solely creating a carcinogenic hepatic microenvironment without an added genetic cytokine polymorphism.
References
Alavian SM, Haghbin H. (2016) Relative importance of hepatitis B and C viruses in hepatocellular carcinoma in EMRO countries and the Middle East: a systematic review. Hepatitis Monthly 16 (3). doi:https://doi.org/10.5812/hepatmon.35106.
Argilés JM, Busquets S, López-Soriano FJ. (2006) Cytokines as mediators and targets for cancer cachexia. The Link Between Inflammation and Cancer: 199–217. doi: https://doi.org/10.1007/0-387-26283-0_9.
Bei CH, Bai H, Yu HP, Yang Y, Liang QQ, Deng YY, Tan SK, Qiu XQ (2014) Combined effects of six cytokine gene polymorphisms and SNP-SNP interactions on hepatocellular carcinoma risk in Southern Guangxi, China. Asian Pac J Cancer Prev 15(16):6961–6967. https://doi.org/10.7314/apjcp.2014.15.16.6961
Caglevic C, Silva S, Mahave M, Torres J, Rolfo C, Gallardo J, Carrasco P. (2016) Hepatocellular carcinoma in identical twins in Chile: case report. ecancermedicalscience; 10. doi:https://doi.org/10.3332/ecancer.2016.708
Chang L, Lan T, Wu L, Li C, Yuan Y, Liu Z (2015) The association between three IL-6 polymorphisms and HBV-related liver diseases: a meta-analysis. Int J Clin Exp Med T 8(10):17036
Chen D, Liu S, Chen S, Wang Z, Wu Z, Ma K, Fan J, Peng Z (2016) Donor interleukin 6 gene polymorphisms predict the recurrence of hepatocellular carcinoma after liver transplantation. Int J Clin Oncol 21(6):1111–1119. https://doi.org/10.1007/s10147-016-1001-1
Cussigh A, Falleti E, Fabris C, Bitetto D, Cmet S, Fontanini E, Bignulin S, Fornasiere E, Fumolo E, Minisini R, Pirisi M (2011) Interleukin 6 promoter polymorphisms influence the outcome of chronic hepatitis C. Immunogenetics 63(1):33–41. https://doi.org/10.1007/s00251-010-0491-7
Dhir M, Melin AA, Douaiher J, Lin C, Zhen WK, Hussain SM, Geschwind JF, Doyle MB, Abou-Alfa GK, Are C (2016) A review and update of treatment options and controversies in the management of hepatocellular carcinoma. Ann surg 263(6):1112–1125. https://doi.org/10.1097/sla.0000000000001556
Dondeti MF, El-Maadawy EA, Talaat RM (2016) Hepatitis-related hepatocellular carcinoma: insights into cytokine gene polymorphisms. World J of Gastroenterol 22(30):6800
El-Akel W, El-Sayed MH, El Kassas M, El-Serafy M et al (2017) Treatment programme of hepatitis C in Egypt: hepatitis C virus model of care. J Viral Hepat 24(4):262–267. https://doi.org/10.1111/jvh.12668
Elgharably A, Gomaa AI, Crossey MM, Norsworthy PJ, Waked I, Taylor-Robinson SD (2017) Hepatitis C in Egypt—past, present, and future. Int J Gen Med 10:1. https://doi.org/10.2147/ijgm.s119301
Goossens N, Hoshida Y (2015) Hepatitis C virus-induced hepatocellular carcinoma. Clin Mol Hepatol 21(2):105. https://doi.org/10.3350/cmh.2015.21.2.105
Hoshida Y, Fuchs BC, Bardeesy N, Baumert TF, Chung RT (2014) Pathogenesis and prevention of hepatitis C virus-induced hepatocellular carcinoma. J Hepatol 61(1):S79–S90. https://doi.org/10.1016/j.jhep.2014.07.010.
Hsia CY, Huo TI, Chiang SY, Lu MF, Sun CL et al (2007) Evaluation of interleukin-6, interleukin-10 and human hepatocyte growth factor as tumor markers for hepatocellular carcinoma. Eur J Surg Oncol 33(2):208–212. https://doi.org/10.1016/j.ejso.2006.10.036
Kim JU, Shariff MI, Crossey MM, Gomez-Romero M, Holmes E, et al., (2016) Cox IJ, Fye HK, Njie R, Taylor-Robinson SD. Hepatocellular carcinoma: Review of disease and tumor biomarkers. World journal of hepatology 8(10):471
Kishimoto T (2005) Interleukin-6: from basic science to medicine—40 years in immunology. Annu. Rev. Immunol 23:1–21. https://doi.org/10.1146/annurev.immunol.23.021704.115806
Lippitz BE, Harris RA (2016) Cytokine patterns in cancer patients: a review of the correlation between interleukin 6 and prognosis. Oncoimmunology 5(5):e1093722. https://doi.org/10.1080/2162402x.2015.1093722
Liu Y, Gao SJ, Du BX, Wang JJ (2014) Association of IL-6 polymorphisms with hepatocellular carcinoma risk: evidences from a meta-analysis. Tumor Biol 35(4):3551–3561. https://doi.org/10.1007/s13277-013-1469-5
Lu Y, Bao JG, Deng Y, Rong CZ, Liu YQ, Huang XL, Song LY, Li S, Qin X (2014) Role of IL-18 gene promoter polymorphisms, serum IL-18 levels, and risk of hepatitis B virus-related liver disease in the Guangxi Zhuang population: a retrospective case-control study. APJCP 16(14):6019–6026. https://doi.org/10.7314/apjcp.2015.16.14.6019
Prieto J (2008) Inflammation, HCC and sex: IL-6 in the centre of the triangle. J hepatol 48(2):380–381. https://doi.org/10.1016/j.jhep.2007.11.007
Saxena R, Chawla YK, Verma I, Kaur J (2014) IL-6 (− 572/− 597) polymorphism and expression in HBV disease chronicity in an Indian population. Am J Hum Biol 26(4):549–555. https://doi.org/10.1002/ajhb.22562
Sghaier I, Mouelhi L, Rabia NA, Alsaleh BR, Ghazoueni E, Almawi WY, Loueslati BY (2017) Genetic variants in IL-6 and IL-10 genes and susceptibility to hepatocellular carcinoma in HCV infected patients. Cytokine 89:62–67. https://doi.org/10.1016/j.cyto.2016.10.004
Shi YH, Zhao DM, Wang YF, Li X, Ji MR, Jiang DN, et al., (2016). The association of three promoter polymorphisms in interleukin-10 gene with the risk for colorectal cancer and hepatocellular carcinoma: a meta-analysis. Scientific reports 6. doi:https://doi.org/10.1038/srep30809.
Tang S, Yuan Y, He Y, Pan D, Zhang Y, Liu Y, Liu Q, Zhang Z, Liu Z (2014) Genetic polymorphism of interleukin-6 influences susceptibility to HBV-related hepatocellular carcinoma in a male Chinese Han population. Hum Immunol 75(4):297–301. https://doi.org/10.1016/j.humimm.2014.02.006
Zhang HY, Feng L, Wu H, Xie XD (2014) The association of IL-6 and IL-6R gene polymorphisms with chronic periodontitis in a Chinese population. Oral Dis 20(1):69–75. https://doi.org/10.1111/odi.12075
Zhou J, Liao W, Zhao Y, Chen Y, Qin L, Zhang H, Zhang S (2017) IL-10 and IL-10RB gene polymorphisms are correlated with hepatitis B-related hepatocellular carcinoma in the Chinese Han population. Transl Cancer Res 6(2):432–440. https://doi.org/10.1002/mc.21928
Zhu K, Moriarty C, Caplan LS, Levine RS (2007) Cigarette smoking and primary liver cancer: a population-based case–control study in US men. CCC 18(3):315–321. https://doi.org/10.1007/s10552-006-0105-8
Zhu SL, Zhao Y, XY H, Luo T, Chen ZS, Zhang Y, Yang SH, Zhou L, Li LQ (2016) Genetic polymorphisms-137 (rs187238) and-607 (rs1946518) in the interleukin-18 promoter may not be associated with development of hepatocellular carcinoma. Sci Rep 21:6–39404. https://doi.org/10.1038/srep39404.
Acknowledgements
We would like to express our gratitude to Theodor Bilharz Research Institute for the financial support which helped us accomplish this piece of work.
Funding
This work was part of a project done on HCC Egyptian patients regarding genetic polymorphism in inflammation pathway-related genes in Theodor Bilharz Research Institute (TBRI); it was funded by this Institute and received grant amount of 100.000 LE. (Project No.: 112T).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This project was approved by the TBRI ethical committee as well as TBRI institutional review board, FWA: 00010609. All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional ethical research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
An informed consent was obtained from all individual participants included in this study.
Additional information
Author identifying information:
Dr. Bothina Madkour is a professor of Hematology and the head of TBRI; moreover, she is the principal investigator (PI) of the project; Dr. Nariman Zahran is a professor of Hematology at TBRI and the Co-PI; Dr. Mona Salah is a professor of Hematology department at Kasr Al-Ainy Hospitals, Cairo University, she is the project’s consultant. Dr. Alaa Gad is a lecturer of Hematology department at Kasr Al-Ainy hospitals, Cairo University; she participated in this project and was responsible for writing the manuscript of the paper under the supervision of Dr. Bothina, Dr. Nariman, and Dr. Mona Salah. Finally, Dr. Mohamed Aboul-Ezz is an assistant professor of Tropical Medicine at TBRI; he participated in the project by being the clinician responsible for clinical diagnosis of the chosen cases. All authors were responsible for selection of the cases, collection of the patient’s samples as well as obtaining the informed consent from the chosen cases. They also participated in doing DNA extraction for gene polymorphism, statistical analysis, and results’ interpretation.
Rights and permissions
About this article
Cite this article
Madkour, B., Gad, A., Hamdy, M.S. et al. Interleukin-6-572 promoter gene polymorphism and its association with chronic hepatitis C-induced hepatocellular carcinoma: an Egyptian study. Comp Clin Pathol 27, 161–165 (2018). https://doi.org/10.1007/s00580-017-2571-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-017-2571-7