Abstract
Strong growing evidence supports a link between Helicobacter pylori (HP) infections and Parkinson’s disease (PD). The purpose of this study was to explore the association between infection with HP cytotoxin-associated gene A (cagA) genotype and PD in Egyptian patients and the influence of its eradication on pharmacokinetic and clinical response to l-dopa. This study was performed on 87 idiopathic PD patients and 45 age- and sex-matched controls. HP infection was diagnosed with HP stool antigen test and HP cagA genotype was detected by PCR. PD patients were subjected to UCLA parkinsonism scale, Hoehn and Yahr staging, and l-dopa plasma level detection by high-performance liquid chromatography. HP PD patients were divided into eradicated group (received standard anti-HP therapy) and placebo group (received antioxidant therapy). Four weeks after therapy, patients were reevaluated. Among PD patients, frequency of HP infection was significantly higher than controls (55.2 vs 33.3%, P = 0.02), especially with HP cagA strain (81.2 vs 40%, P = 0.002). PD was more severe in HP infected (P < 0.001), especially in HP cagA-positive patients (P = 0.04) with significant lower l-dopa plasma levels (P < 0.001). cagA strains were associated with higher risk of increased PD severity (OR, 2.139; P = 0.029). Opposing antioxidant therapy, HP eradication treatment improved PD severity (UCLA score decreases by 30%) and increased l-dopa level by 40%. There is a proved link between PD and infection with virulent HP cagA strains. HP could affect l-dopa level by mechanisms other than reactive oxygen radical’s production which need further evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is recognized as the second most common neurodegenerative disorder after Alzheimer’s disease and affects 1% of the population worldwide after the age of 65 years (Tanner and Goldman 1996; Pringsheim et al. 2014). The most common PD symptoms are related to the motor system: bradykinesia/hypokinesia, rigidity, tremor, and postural abnormality (Berg et al. 2013). Helicobacter pylori (HP) is a wide spread Gram-negative bacterium found on the luminal surface of the duodenal and gastric epithelium infecting about one half of the world population. While HP infection in developed countries ranges from 25 to 40%, it is as high as 90% in some developing countries as Egypt (Hunt et al. 2011; Khedmae et al. 2013).
HP is responsible for many gastric pathologies such as chronic gastritis, peptic ulcer, and gastric cancer as well as a variety of extra-gastric disorders including neurodegenerative, metabolic, and cardiovascular conditions, as well as hepatobiliary, pancreatic, and colorectal diseases (Roubaud-Baudron et al. 2012; Rizk et al. 2016).
Recently, complex interactions between genetic predispositions and exposure to environmental factors, such as toxins and infectious agents, have been suggested to underlie the selective but widespread and multisystem loss of neurons in PD (Pfeiffer 2009). The hypothesis of association of gastrointestinal microbiota and PD development had been postulated (Cersosimo and Benarroch 2008; Fasano et al. 2013). Chronic HP infection may trigger inflammatory and autoantibody/molecular mimicry mechanisms, which could consequently lead to the destruction of dopaminergic neurons (Dobbs et al. 1999). Interestingly, HP has also been shown to have a role in the bio-synthetic route of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), a known neurotoxic to dopaminergic neurons (Altschuler 1996).
Moreover, it is postulated that HP infection affects levodopa (l-dopa) bioavailability, hence motor fluctuation in PD by disrupting the duodenal mucosa or producing reactive oxygen species, which could inactivate the drug (Kankkunen et al. 2002).
Two putative markers of HP virulence, the cytotoxin-associated gene (cagA) pathogenicity island and the vacuolating cytotoxin genes (vacA), have been extensively studied. The highly virulent HP cagA strains were directly proportional to the severity of many extra-gastric diseases as well as the risks for ischemic stroke and atherosclerotic stroke (Esmat et al. 2012; Franceschi et al. 2014). However, there are no detailed studies on the distribution and association of HP cagA genotype in PD patients yet.
We aimed at studying the frequency of HP cagA-positive strains among Egyptian PD patients. Moreover, the impact of its eradication on both plasma level of l-dopa and the clinical response was addressed.
Materials and methods
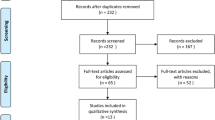
Study subjects
This is a prospective, randomized, placebo-controlled, parallel-group study carried out from October 2013 to August 2015 on 87 idiopathic PD patients attending outpatient clinic at neurology and neurosurgery center in Mansoura University. Forty-five age- and sex-matched participants who were neither complaining of neurological disease nor relatives to Parkinson’s disease patients were included as controls for this study.
Eligible patients for this study were adult whose age was equal or more than 18 years and diagnosed as having idiopathic Parkinson’s disease according to UK Parkinson’s Disease Society Brain Bank criteria. They were also required to have no associated neurologic diseases other than PD, no use of antiparkinsonian other than l-dopa ± anticholinergics, and no use of any drug potentially affecting gastrointestinal motility. We excluded those with secondary parkinsonism or Parkinson’s plus syndrome and those with a recent history of medication with proton pump inhibitors or histamine antagonist (for at least 4 weeks) or antibiotics ((last 30 days prior to inclusion). Patients were evaluated twice as follows:
First visit
At the beginning of the study, all PD patients fulfilling the inclusion criteria were subjected to baseline evaluations including demographic characteristics (age and sex), previous antibiotic use, medical and medication history, neurological clinical assessments, diagnosis of HP infection by stool antigen test, and determination of their baseline plasma level of l-dopa. Thereafter, PD patients diagnosed with active HP infection were randomly allocated, using a random computer-generated code in blocks of five, to either eradicated or placebo (antioxidant) group.
Eradicated group
Were assigned to receive triple therapy for eradication of H. pylori (omeprazole 20 mg, clarithromycin 500 mg and amoxicillin 1 g) twice daily for 14 days.
Placebo group
Were assigned to receive antioxidant therapy (selenium 55 μg, vitamin A 1500 IU, vitamin C 90 mg, and vitamin E 22 IU) twice daily for 14 days.
Second visit
Four weeks after the end of intervention therapy, successful eradication of HP was confirmed by absence of H. pylori antigen in stool. Then, all patients in both groups were neurologically re-examined and their plasma levels of l-dopa were measured.
Neurological examinations
Clinical assessment of PD before and after intervention therapy was done by a single examiner to reduce inter-observer variability. PD severity was assessed using UCLA parkinsonism scale, while staging of the PD was performed according to Hoehn and Yahr stages (Markham and Diamond 1981; Hoehn and Yahr 1967). The UCLA parkinsonism scale is of sufficient validity and reliability and is sensitive enough to detect changes within the frame of l-dopa therapy (McDowell et al. 1970). It consists of 21 sub-items, 14 of them are done by clinical examination of the patient and 7 sub-items are determined by questioning the patient or family members. Each sub-item is individually weighted. For example, “masked facies” has the weighting factor 1 and speech or gait has10. This factor is then multiplied by 0 if “absent,” 1 for “present,” or 2 for “marked.” The total disability score is the sum of all subscores and ranges from 0 to 220 (0 = no impairment and 220 = severest impairment) (Markham and Diamond 1981). Clinical fluctuations, dyskinesias, tremors, and rigidity were assessed by using the Unified PD Rating Scale, section III (UPDRS-III) (Ramaker et al. 2002). The motor scoring was done in medication on state. Clinical response to l-dopa was assessed by recording the l-dopa onset time and the duration of on time in minutes.
Laboratory diagnosis of H. pylori infection
H. pylori screening test
We used the noninvasive stool antigen test (SAT) to screen both PD patients and controls for active HP infection and considering the validity of eradication treatment status as recommended by Saha et al. (2016). They proved stool antigen test of having high sensitivity and specificity against gold standard tests such as histology, culture, and [13C] urea breath and considered it the most convenient way for diagnosing the active HP infection.
All enrolled patients and controls were screened by analysis of their stool using an immunochromatographic HP stool antigen test (Cal-Tech Diagnostics, Inc., Chino, CA, USA) according to the manufacturer’s instructions. This test was repeated 4 weeks following eradication therapy to confirm successful eradication.
Molecular detection of HP cagA strains (Agha et al. 2013)
All stool samples that showed positivity for HP antigen by the immunochromatographic rapid assay were candidates for detection of the presence of cagA gene as follows:
DNA extraction
Done using the QIAamp DNA stool minikit (Qiagen) according to the manufacturer’s instructions.
Amplification and detection of cagA gene by conventional PCR
A 349-bp target sequence from cagA gene was amplified using two primers: forward primer P1: 5′-GATAACAGGCAAGCTTTTGAGG-3′ and reverse primer P2: 5′-CTGCAAAAGATTGTTTGCGAGA-3′. The PCR was performed in a total volume of 50 μL of master mix (EzWay PCR Master Mix, Koma Biotech, Seoul, Korea) containing 1 μL of the extracted DNA and 0.5 μM of each primer.
High-performance liquid chromatography analysis of l-dopa (Muzzi et al. 2008)
One hour after the oral administration of levodopa, 2 mL of venous blood were withdrawn into EDTA tubes from PD patients and were centrifuged (2000g, 5 min, 4 °C) immediately. Then protein precipitation was performed by perchloric acid and plasma samples were frozen (−80 °C) until analysis.
l-Dopa concentration was determined by high-performance liquid chromatograph of 1260 series hp chemstation software (Agilent, USA) equipped with UV detector adjusted at 220 nm, autosampler, quaternary pump, and a ready-to-use prepacked C-18 column (15 cm, 4.6 mm I.D.). Mobile phase was 0.05 M potassium dihydrogen orthophosphate with PH adjusted at 3.5. Stationary phase was 5 μm base deactivated silica. Flow rate was 1.0 mL/min, the injection volume was 20 μl at 7 °C autosampler temperature, and the run time was 6.0 min.
Calibration curves were constructed by serial dilutions of stock solution of l-dopa standard (1.97 mg/mL) with distilled water. The range of assay was 0.01–80 mg/L (Fig. 1).
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences (SPSS) version 16. Qualitative data was presented as number and percentage. Quantitative data was presented as mean and standard deviation. The chi-square (χ 2) was used to find the association between variables of qualitative data. Student’s t test was used to compare the numerical data between two groups. Univariate and multivariate regression tests were used to examine the effects of potential confounding factors on PD severity. P value of ≤0.05 indicated a significant result.
Results
Eighty-seven PD patients and 45 healthy individuals fulfilled the inclusion criteria for this study. They were of matched age and gender ( P = 0.2, P = 0.9). We revealed that frequency of HP infection are significantly higher among PD patients (55.2%) than among controls (33.3%), P = 0.02. Also, HP cagA strains were significantly more frequent among PD patients than control group, 81.2 versus 40%, P = 0.002 (Table 1).
Baseline neurological evaluations of PD patients showed that severity of PD had not affected only by HP status of the patients but also by the presence or absence of cagA gene (Table 2). PD was more severe in the HP-positive patients as compared to the HP-negative patients (P < 0.001). Also, it was significantly more severe in HP cagA-positive patients than HP cagA-negative patients as shown by their UCLA scales (111.1 ± 26.2 vs 83 ± 23, P = 0.04). HP cagA-positive patients suffered also more tremors than HP cagA-negative patients (P = 0.001).
Despite the insignificant difference in the daily dose of l-dopa between HP-positive and HP-negative PD patients, we observed that HP-negative PD patients responded in a better way to l-dopa as evidenced by their faster “on” time (23.5 + 4.2 min) and their significant higher plasma level of l-dopa (0.8 ± 0.26 mg/L) as compared to HP-positive patients (28.1 ± 4.7 min and 0.6 ± 0.28 mg/L).
In spite that HP cagA-positive PD patients treated with a significantly higher dose of l-dopa than HP cagA-negative PD patients (613.5 ± 213.4 vs 450 ± 112.5, P = 0.03), we observed that their onset of response to l-dopa dose did not differ significantly from HP cagA-negative patients (P = 0.3) and their plasma level of l-dopa was still significantly lower than HP cagA-negative patients (0.5 ± 0.22, 0.9 ± 0.2, P < 0.001).
Four weeks after the end of this intervention therapy, all of 27 patients assigned to anti-HP treatment successfully eradicated HP but none of patients received antioxidant therapy changed to HP negative. As shown in Table 3, among eradicated group, the total UCLA score was significantly decreased after successful HP eradication as compared to their baseline score (83.1 ± 19.2 vs 120.2 ± 35.8, P < 0.001). Also, their motor symptoms in the form of tremors, fluctuations, and akinesia were improved significantly in comparison to their baseline symptoms. On the contrary, none of the patients randomized to antioxidant therapy showed clinical improvement from their baseline.
After intervention therapy, while plasma level of l-dopa seemed to increase about 40% after anti-HP treatment, it did not change and remained the same after antioxidant therapy (Fig. 2).
Linear regression analysis was used for prediction of severity in all studied patients using age, sex, l-dopa level, disease duration, and cagA as covariates. Female gender, low l-dopa level, disease duration, and cagA positive were associated with higher risk of increased severity in univariate analysis, while in multivariate analysis, only cagA positive was associated with higher risk of increased severity, odds ratio 2.139, 95% CI 1.943–4.852, P = 0.029 (Table 4).
Discussion
Helicobacter pylori (HP) infection is the most widespread gastrointestinal infection in the world and depends on age and socioeconomic status (Azevedo et al. 2009). Confirming it as a causal agent of many extra-gastric pathologies, we carried out our study on Egyptian Parkinson’s disease (PD) and revealed that frequency of HP infection was significantly higher among PD patients than healthy control subjects. This is consistent with findings from previous studies reported 36, 53, 70, and 32% prevalence of HP in PD patients (Pierantozzi et al. 2006; Lee et al. 2008; Dobbs et al. 2010; Tan et al. 2015). Furthermore, a previous case-control study conducted in our locality (Mansoura City, Egypt) on a different cohort of PD patients revealed a prevalence of 46% (Esmael et al. 2016).
Despite that several hypotheses have been postulated to explain the high frequency of HP among PD, it remains unclear why PD patients have higher tendency to develop this infection. HP could produce an inflammatory state, induces autoantibody/molecular mimicry mechanisms, which could consequently lead to the destruction of dopaminergic neurons and/or causing apoptosis of nerve cells via circulating monocytes (Dufek et al. 2015; Hirsch and Hunot 2009).
In addition to the high prevalence, HP infection affected our patients’ motor performances adversely. We showed that the severity of parkinsonism was higher in HP-infected patients than HP negative as clarified by clinical scales. This finding is matched with many studies addressing the severity of Parkinson’s diseases and HP infection (Tan et al. 2015; Tsuboi and Yamada 2008).
Our observation of a lower plasma level of l-dopa in HP infected than non-infected patients despite being matched for the total l-dopa dosage could be attributed to many hypothesis like the following: HP infection affects l-dopa absorption, inactivation of the drug by local production of reactive oxygen species, increased consumption of l-dopa by the bacteria, or delayed delivery into the duodenum (Deretzi et al. 2011; Tan et al. 2014).
To our knowledge, no previous study has assessed the possible role of cagA virulent HP strains in PD. Apart from Weller et al. (2005) who explored the extra-alimentary consequence of HP and concluded that persistence of serum cagA antibodies was predictive for PD and associated with a poor prognosis.
In the same context, our study showed that infection by the virulent HP cagA strains were significantly more frequent among Egyptian PD patients (81%), whereas cagA-negative strains have a more prevalence in controls (66%). Interestingly, HP cagA-positive strains were associated with higher risk of increased severity in PD patients confirming the hypothesis that the association between HP and PD is related to the virulence of this bacterium. Also, HP cagA-positive patients suffered more aggressive tremors than HP cagA-negative patients. However, fluctuations, rigidity, and akinesia did not differ significantly among HP-infected PD patients according to their cagA gene status.
Moreover, in our study, although HP cagA-positive PD patients received a significantly higher daily dose of l-dopa than HP cagA-negative patients, we found that the onset of response to the daily total dose of l-dopa (on time) did not differ significantly between HP cagA-positive and HP cagA-negative patients and plasma level of l-dopa was significantly lower in cagA positive and consequently duration of this “on” time state was significantly more shorter in HP cagA-positive patients than HP cagA-negative patients.
These findings could raise the possibility that implication of HP in the interference with l-dopa absorbance is due to the presence of cagA gene as a virulent factor in this bacteria. Recently, Shimoda et al. 2016 reported that cagA is present as exosomes secreted from gastric epithelial cells of infected patients. These exosomes may enter into circulation and deliver cagA to distant organs that may provoke more systemic clinical effects that are seemingly unrelated to the primary infection (Shimoda et al. 2016).
Our study was performed with two arms: HP eradication arm and placebo arm who received antioxidants drugs. Eradication of HP clarified a significant overall improvement in the motor severity score (UCLA score decreases by 30%), increased plasma level of l-dopa by about 40%, the mean l-dopa onset time shortened by 10 min (33%), and the mean duration of “on” time increased by 55 min (55%).
Most of publications considering eradication issues agreed with this finding and reported an increase of 21%, 54% in the plasma level of l-dopa after successful cure of HP infection in PD patients ((Pierantozzi et al. 2006; Lahner et al. 2009). Improved hypokinesia following antimicrobials appeared unique to Helicobacter eradication while rigidity worsened while antimicrobials for other indications had no effect (Dobbs et al. 2013).
Based on clinical evaluation, the current antioxidant-treated patient results failed to support the hypothesis that HP may affect l-dopa pharmacokinetics by reactive oxygen radical’s production (Drake et al. 1998).
Some authors reported an exacerbation of rigidity and increase in tremor associated with antimicrobial exposure and explained it by an altered admixture of intestinal microbiota that drive different pathogenic processes concerning motor manifestation of Parkinson’s disease. Those findings gave an idea of paradigm shift from cold neurodegeneration to microbe-triggered/microbe-driven immunoinflammatory processes (Dobbs et al. 2010, 2013; Charlett et al. 2009). Tan et al. (2014) confirmed the hypothesis of neuro-inflammation secondary to increased gastrointestinal microbiota (Tan et al. 2014).
Strengths of this study include recruitment of a relatively large number of subjects with a matched healthy control group. Patients underwent blinded evaluations, including objective and quantitative measures of motor function and plasma l-dopa level. Addressing the HP cagA strain effect on Parkinson severity and plasma l-dopa level occur for the first time up to our knowledge.
There are several limitations that need to be highlighted. Longer duration of follow up to 6 months post treatment is more convenient. Post eradication improvement in l-dopa absorption can be evaluated by pharmacokinetic sampling for measuring pharmacokinetics indices (area under the curve (AUC) and time to maximum plasma levodopa concentration (Cmax); however, we used only one sample for plasma l-dopa and we evaluated this improvement indirectly via the modification of plasma l-dopa concentration and through clinical scores. It was better to investigate the effect of administrating selenium, vitamin A, vitamin C, and vitamin E on the level of oxidative stress by objective quantitative measurement.
Conclusion
The current results of our study suggest higher frequency of HP infection in PD patients. Moreover, HP infection increase the severity of PD and it affect motor symptoms. Additionally, virulent HP cagA-positive infection could play a relevant role in daily clinical variations in PD. Eradication of HP improves l-dopa absorption and the overall severity of PD specifically tremors. Therefore, PD patients should be investigated for HP infection and specific antibiotic therapy against HP should be recommended for HP-positive PD patients (especially those with cagA positive) even in absence of dyspeptic symptoms. The relationship between HP and PD should be further clarified by more comprehensive studies in the future, especially the exact mechanism by which chronic HP infection could affect l-dopa absorption in PD patients.
References
Agha S, Foad MF, Awadalla N, Saudy N (2013) Helicobacter pylori cagA gene in Egyptian sewage workers. Afr J Pathol Microbiol 2:1–6
Altschuler E (1996) Gastric Helicobacter pylori infection as a cause of idiopathic Parkinson disease and non-arteric anterior optic ischemic neuropathy. Med Hypotheses 47:413–414
Azevedo NF, Huntington J, Goodman KJ (2009) The epidemiology of Helicobacter pylori and public health implications. Helicobacter 14(S1):1–7
Berg D, Lang AE, Postuma RB et al (2013) Changing the research criteria for the diagnosis of Parkinson’s disease: obstacles and opportunities. Lancet Neurol 12:514–524
Cersosimo MG, Benarroch EE (2008) Neural control of the gastrointestinal tract: implications for Parkinson disease. Mov Disord 23:1065e75
Charlett A, Dobbs RJ, Dobbs SM et al (2009) Blood profile holds clues to role of infection in a premonitory state for idiopathic parkinsonism and of gastrointestinal infection in established disease. Gut Pathogens 1:20
Deretzi G, Kountouras J, Polyzos SA et al (2011) Gastrointestinal immune system and brain dialogue implicated in neuroinflammatory and neurodegenerative diseases. Curr Mol Med 11:696e707
Dobbs RJ, Charlett A, Purkiss AG, Dobbs SM, Weller C, Peterson DW (1999) Association of circulating TNF-a and IL-6 with ageing and parkinsonism. Acta Neurol Scand 100:34–41
Dobbs SM, Dobbs RJ, Weller C et al (2010) Differential effect of Helicobacter pylori eradication on time trends in brady/hypokinesia and rigidity in idiopathic parkinsonism. Report on completion of a randomised, double-blind, placebo-controlled efficacy study. Helicobacter 15:279–294
Dobbs SM, Charlett A, Dobbs RJ et al (2013) Antimicrobial surveillance in idiopathic parkinsonism: indication-specific improvement in hypokinesia following Helicobacter pylori eradication and non-specific effect of antimicrobials for other indications in worsening rigidity. Helicobacter 18(3):187–196
Drake IM, Mapstone NP, Schoral CJ et al (1998) Reactive oxygen species activity and lipid peroxidation in Helicobacter pylori associated gastritis: relation to gastric mucosal ascorbic acid concentration and effect of H. pylori eradication. Gut 42:768–771
Dufek M, Rektorova I, Thon V, Lokaj J, Rektor I (2015) Interleukin 6 may contribute to mortality in Parkinson’s disease patients: a 4-year prospective study. Parkinsons Dis 2015:898192
Esmael A, El-Sherif M, Shabana HR, Elazzouny AA (2016) Helicobacter pylori infection in Egyptians with Parkinson’s disease: incidence and the effect on motor fluctuation and response to levodopa. Egypt J Neurol, Psychiatry Neurosurg 53(2):84–88
Esmat G, El-Bendary M, Zakarya S, Ela MA, Zalata K (2012) Role of Helicobacter pylori in patients with HCV-related chronic hepatitis and cirrhosis with or without hepatocellular carcinoma: possible association with disease progression. J Viral Hepat 19:473–479
Fasano A, Bove F, Gabrielli M et al (2013) The role of small intestinal bacterial overgrowth in Parkinson’s disease. Mov Disord 28:1241e9
Franceschi F, Tortora A, Gasbarrini G (2014) Helicobacter pylori and extragastric diseases. Helicobacter 19(S1):52–58
Hirsch EC, Hunot S (2009) Neuroinflammation in Parkinson’s disease: a target for neuro protection? Lancet Neurol 8(4):382–397
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Hunt RH, Xiao SD, Megraud F et al (2011) Helicobacter pylori in developing countries. J Gastrointestin Liver Dis 20(3):299–304
Kankkunen T, Huupponen I, Lahtinen K et al (2002) Improved stability and release control of levodopa and metaraminol using ion-change fibers and transdermal iontophoresis. Eur J Pharm Sci 16:273–280
Khedmae HI, Karbasi-Afshar R, Agah S, Taheri S (2013) Helicobacter pylori infection in the general population: a middle eastern perspective. Caspian J Intern Med 4(4):745–753
Lahner E, Annibale B, Delle Fave G (2009) Systematic review: Helicobacter pylori infection and impaired drug absorption. Aliment Pharmacol Ther 29:379–386
Lee WY, Yoon WT, Shin HY, Jeon SH, Rhee PL (2008) Helicobacter pylori infection and motor fluctuations in patients with Parkinson’s disease. Mov Disord 23:1696e700
Markham CH, Diamond SG (1981) Evidence to support early levodopa therapy in Parkinson disease. Neurology 31(2):125–131
McDowell F, Lee JE, Swift T, Sweet RD, Ogusbury JS, Kessler JT (1970) Treatment of Parkinson’s syndrome with l dihydroxyphenylalanine (levodopa). Ann Intern Med 72:29–35
Muzzi C, Bertocci E, Terzuoli L et al (2008) Simultaneous determination of serum concentrations of levodopa, dopamine, 3-O-methyldopa and alpha-methyldopa by HPLC. Biomed Pharmacother 62(4):253–258
Pfeiffer RF (2009) Neuroinflammation and Parkinson’s disease: the silent battle ground. Neurology 73:1434–1435
Pierantozzi M, Pietroiusti A, Brusa L et al (2006) Helicobacter pylori eradication and l-dopa absorption in patients with PD and motor fluctuations. Neurology 66:1824–1829
Pringsheim T, Jette N, Frolkis A, Steeves TD (2014) The prevalence of Parkinson’s disease: a systematic review and meta-analysis. Mov Disord 29(13):1583–1590
Ramaker C, Marinus J, Stiggelbout AM, Van Hilten BJ (2002) Systematic evaluation of rating scales for fluctuations in patients with Parkinson’s disease. Mov Disord 17(5):1696–1700
Rizk E, Mashaly M, Zakaria S, Abdel-Razik A, Abbas N (2016) Could Helicobacter pylori infection impair glucose tolerance in obese non-diabetic subjects? Br J Med Med Res 11(1):1–9
Roubaud-Baudron C, Krolak-Salmon P, Quadrio I, Mégraud F, Salles N (2012) Impact of chronic Helicobacter pylori infection on Alzheimer’s disease: preliminary results. Neurobiol Aging 33:1009.e11–1009.e19
Saha R, Roy P1, Das S, Kaur N, Kumari A, Kaur IR (2016) Application of a stool antigen test to evaluate the burden of Helicobacter pylori infection in dyspepsia patients. Indian J Pathol Microbiol 59(1):66–68
Shimoda A, Ueda K, Nishiumi S et al (2016) Exosomes as nanocarriers for systemic delivery of the Helicobacter pylori virulence factor CagA. Sci Rep 7(6):18346
Tan AH, Sanjiv M, Abdul MT et al (2014) Small intestinal bacterial overgrowth in Parkinson’s disease. Parkinsonism Relat Disord 20:535e40
Tan AH, Mahadeva S, Marras C et al (2015) Helicobacter pylori infection is associated with worse severity of Parkinson’s disease. Parkinsonism Related Disorder 21:221–225
Tanner CM, Goldman SM (1996) Epidemiology of Parkinson’s disease. Neurol Clin 14:317–335
Tsuboi Y, Yamada T (2008) Prevalence of Helicobacter pylori infection among patients with Parkinson’s disease: impact on clinical manifestations. Mov Disord 23:S291
Weller C, Charlett A, Oxlade NL et al (2005) Role of chronic infection and inflammation in the gastrointestinal tract in the etiology and pathogenesis of idiopathic parkinsonism. Part 3: predicted probability and gradients of severity of idiopathic parkinsonism based on H. pylori antibody profile. Helicobacter 10:288–297
Author information
Authors and Affiliations
Ethics declarations
Ethical standards
Informed consents were obtained from all participants. The local ethics committee, Mansoura University ethical committee (IRB), approved our study with a code number of R/16.07.56 and thus performed in accordance with the Declaration of Helsinki.
Conflict of interest
All authors declare that they have no competing interests.
Statement of financial support
There was no external funding received for this study.
Rights and permissions
About this article
Cite this article
Mashaly, M., Saudy, N., Belal, T. et al. Helicobacter pylori cytotoxin-associated gene A genotype in Egyptian patients with Parkinson’s disease: could eradication benefit?. Comp Clin Pathol 26, 893–900 (2017). https://doi.org/10.1007/s00580-017-2460-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-017-2460-0