Abstract
Purpose
To investigate the association between adherence to guideline-recommended risk-based postoperative nausea and vomiting (PONV) prophylaxis, the antiemetics used for PONV prophylaxis, and the incidence of PONV in patients who were underwent general anesthesia before and after 5-HT3 receptor antagonists became available.
Methods
Patients (≥ 20 years old) who were extubated after scheduled surgery and returned to general wards between January 2021 and February 2022 and between June 2022 and July 2023 were included. Risk factors included age < 50, female, motion sickness, nonsmoker, surgical factors, and postoperative opioid use. Two and three or more prophylaxis were recommended for patients with one or two and three or more risk factors, respectively. The primary outcome was the number of patients who received adequate prophylaxis, and the secondary outcomes were antiemetic agents used during anesthesia and the incidence of PONV on postoperative days 0 and 1. PONV was defined as documented PONV or rescue antiemetic administration.
Results
From January 2021 to February 2022 and from June 2022 to July 2023, 2342 and 2682 patients were included, respectively. Before ondansetron became available, more D2 receptor antagonists were used (p < 0.001), and after ondansetron became available, both ondansetron (p < 0.001) and propofol (p < 0.001) were given more frequently. Before and after ondansetron became available, the number of patients with adequate prophylaxis was 3.7% and 9.2%, respectively (p < 0.001), and the incidence of PONV on postoperative days 0 and 1 was 44.6% and 44.0%, respectively (p = 0.67).
Conclusion
The availability of ondansetron increased the number of patients with adequate PONV prophylaxis, but did not decrease the incidence of PONV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of postoperative nausea and vomiting (PONV), defined as nausea and vomiting occurred on postoperative days 0 and 1 [1], has been reported to be 30% in the general surgical population and 80% in high-risk populations [2, 3]. This can lead to patient dissatisfaction and to increased health care costs [4, 5].
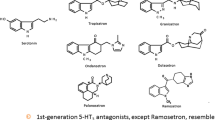
Given its high incidence and associated poor outcomes, optimal management of PONV including prophylaxis and treatment should be provided; however, no Japan’s own guideline exist and the guidelines established by the American Society of Enhanced Recovery and Society for Ambulatory Anesthesia, which was updated in 2020, are used in Japanese clinical practice [1]. This American guideline recommends escalation of the number of antiemetics (Supplementary Table 1) and acupuncture based on a preoperative estimate of PONV risk; however, several drugs are not allowed for PONV management in Japan [1]. In fact, available drugs during anesthesia are propofol, dopamine D2 receptor antagonist including droperidol and metoclopramide, and 5-hydroxytryptamine 3 (5–HT3) receptor antagonists which became available in August 2021 [6]. This denotes that after August 2021, it finally has been possible in Japan to implement antiemetics recommended by the American guideline in patients at high risk of PONV ≥ 3 risk factors.
However, despite dissemination of 5–HT3 receptor antagonists, the effects on clinical outcomes have been known. This study aimed to investigate the association between adherence to guideline-recommended risk-based PONV prophylaxis, the antiemetics used for PONV prophylaxis, and the incidence of PONV in patients who were underwent general anesthesia before and after 5-HT3 receptor antagonists became available.
Materials and methods
This retrospective study was approved by the Nara Medical University Institutional Review Board, Kashihara, Nara, Japan (Chairperson Prof. M. Yoshizumi, Approval No. 3962 on 6 September 2023).
Due to the nature of a retrospective study, the requirement for informed consent was waive. This study was conducted in accordance with the Declaration of Helsinki.
Study population
Patients aged 20 years or older who underwent elective surgery with general anesthesia and who were extubated after surgery at Nara Medical University between January 2021 and July 2023 were included. Since ondansetron became available at our institution in March 2022, a 3-month grace period was given and patients who underwent surgery between March and May 2022 of the above period were excluded. We excluded patients who underwent electric convulsive therapy, patients with long QT interval (male female; ≥ 470 ms and female female; ≥ 480 ms) for restriction of dopamine antagonists, patients who underwent surgery with motor-evoked potential monitoring in whom anesthesia is managed using propofol in our institution, patients anesthetized with remimazolam, patients given steroid during anesthesia, patients managed in the intensive care unit on postoperative day 0 and/or 1, and patients transported to general wards with tracheal intubation. Remimazolam is available in several Asian countries, including Japan, Korea, and China, which is not listed in the American guideline and its effects on PONV have been controversial [7,8,9]; thus, patients anesthetized with remimazolam were excluded. American guidelines recommend dexamethasone for PONV prophylaxis [1]; however, the use of dexamethasone as a prophylactic antiemetic is off-label in Japan. Because all steroids have glucocorticoid effects to varying degrees, cases in which steroids were used during anesthesia were excluded from this study. Patients were allowed to oral intake until 2 h before surgery and no premedication was given. Intraoperative anesthetic management, including choice of a prophylactic antiemetic, was depended on the attending anesthesiologist.
Data collection
We evaluated the patients’ characteristics, including age; height; weight; sex; smoking status; comorbidities (symptomatic stroke, hypertension, ischemic heart disease, atrial fibrillation, diabetes, and dialysis); medication (beta-blocker and statin); motion sickness; and the American Society of Anesthesiologists-physical status using their medical chart. We also collected laboratory data, including serum albumin and serum creatinine. Intraoperative data were included surgery type (gynecological, laparoscopic, cholecystectomy), anesthetics (propofol or not), antiemetics (dopamine 2 antagonist, including droperidol and/or metoclopramide, and ondansetron), fentanyl and remifentanil dose, fluid balance, anesthesia duration, and postoperative opioids’ use.
Outcomes
The primary outcome in this study was the number of patients given adequate prophylaxis strategy. The following patients were classified as the category of adequate prophylaxis strategy; ≥ 0 antiemetic agent for patients with 0 risk factor, ≥ 2 antiemetic agents for patients with 1 or 2 risk factors, and ≥ 3 antiemetic agents for patients with 3 or more risk factors [1]. Risk factors include female sex, history of PONV or motion sickness, nonsmoking, younger age (< 50 years old), postoperative opioids analgesia, and type of surgery (gynecological, laparoscopic, cholecystectomy) [1]. Patients were not necessarily asked about a history of PONV in our institution; thus, only motion sickness was included. The secondary outcomes in this study were antiemetics used during the anesthesia and the incidence of PONV on POD 0 and POD 1. PONV was defined as documented PONV and/or administration of a rescue antiemetic. Additionally, the association between the number of risk factors for PONV and the number of given antiemetics was assessed.
Statistical analysis
Continuous data are mean with standard deviation and categorical variables as number with percent.
Data among two groups were compared using the Chi-square test or Fisher’s exact test for dichotomous variables or unpaired t test for continuous variables. The odds ratio of interaction between the number of risk factors for PONV and the number of given antiemetics was estimated using a logistic regression analysis. As a descriptive tool for measuring model bias, the area under the receiver-operating characteristic curve was computed. All data were analyzed with SPSS version 25.0 (IBM Inc, Armonk, NY, USA) and P < 0.05 was considered statistically significant. Sample size was not calculated; however, at first, this study included patients who underwent surgery in a 13-month period from June 2022 to July 2023, which is the longest period, since ondansetron was available, excluding the grace period. Then, patients from February 2022 going back the same 13 months to January 2021 were included.
Results
Of 8427 eligible patients, 5024 eligible patients were included in the final analysis (Fig. 1). There were 2342 patients from January 2021 to February 2022 and 2682 patients from June 2022 to July 2023, respectively. Table 1 shows patients demographics and intraoperative data. Among two groups, the use of statin (p = 0.01) and the prevalence of motion sickness (p = 0.01) were statistically different. Regarding antiemetics, D2 receptor antagonists were used more (p < 0.001) in patients who were underwent from January 2021 to February 2022. In contrast, ondansetron (p < 0.001) and propofol (p < 0.001) were administrated more in patients who were underwent from June 2022 to July 2023. No acupuncture was performed in all patients. Postoperative opioids' use was more in patients who underwent from June 2022 to July 2023 (p < 0.001). As shown in Table 2, although the number of risk factors were statistical difference (p = 0.01), the number of recommended prophylaxis strategy was not statistical difference (p = 0.17). The number of patients given adequate prophylaxis was 3.7% (87/2342) patients who were underwent from January 2021 to February 2022 and 9.2% (263/2682) in patients who were underwent from June 2022 to July 2023, respectively (p < 0.001). The incidence of PONV on POD 0 and/or POD 1 were 44.6% (1045/2342) and 44.0% (1180/2682) from January 2021 to February 2022 and from June 2022 to July 2023, respectively, which were no statistical differences (p = 0.67). Table 3 shows association of number of risk factors for postoperative nausea and vomiting with number of taken prophylaxis. As shown in Table 4, our multiple logistic regression analysis revealed an independent association between the number of risk factors for PONV and the incidence of PONV [odds ratio (95% Confidence interval); 1.54 (1.44–1.64)], and this effect was negatively magnified in patients with increased number of antiemetics [odds ratio (95% Confidence interval); 0.93 (0.88–0.99)].
Discussion
This retrospective study including 5024 patients ≥ 20 years old who were provided general anesthesia revealed that the availability of ondansetron for POVN prophylaxis enhanced adherence of the American guideline; however, patients remain with inadequate prophylaxis and the incidence of PONV was not different among patients who were underwent during two periods. Additionally, increased antiemetic given to patients with higher risk factors contributed to a decrease in PONV.
More than 20 years ago, Apfel et al. [3] developed a simple tool to predict PONV, which triggered interest in PONV [3]; then, in 2003, the first consensus guidelines for PONV was published [10]. The fourth edition, revised in 2020, presents antiemetic doses and timing in adult patients in addition to risk factors and prophylaxis for PONV [1]; however, not all listed drugs are available in Japan and there were at most two drugs available including D2 receptor antagonists and propofol until ondansetron became available, but the advent of ondansetron allowed for a three-antiemetic strategy [6]. Ondansetron contributed to higher rate of the number of patients given adequate prophylaxis strategy; however, the use of D2 receptor antagonists were decreased. This exact reason is unknown, but it may be that risk-based prophylaxis strategy was not well known and the idea that just ondansetron should be administered arose. Other reason is the fact that the benefit of PONV prophylaxis also needs to be balanced with the risk of adverse effects. For instance, metoclopramide is a representative D2 receptor antagonist, but this is included in the Beer criteria, which is standards to recognize potentially inappropriate drug use in the elderly [11]. Moreover, nitrous oxide, which is not used to maintain general anesthesia in our cohort, was associated with a lower incidence of lung atelectasis, although it is a risk factor for PONV [12]. It is considerable that precautions may not have been taken to reduce anesthesia-related complications other than PONV, such as these.
The number of patients given adequate prophylaxis strategy increased statistically, but to a lesser extent (10%) and remained as low as before, which we conceive is why it did not make a difference in the incidence of PONV. However, just increasing the number of antiemetics did not reduce PONV, but administering more antiemetics to high-risk patients was associated with decrease in PONV (p for interaction = 0.03); thus, risk classification may have effects on decreasing PONV. Furthermore, the effects of institutional protocols for prophylaxis strategies based on risk assessment of PONV and an electronic medical record-based clinical decision support approach on decreased PONV were reported [13,14,15]; thus, these as well as risk assessment should be implemented in clinical practice.
This study had some potential limitations. First, this study was a retrospective study conducted in a single center; thus, results should be interpreted with caution. Second, one definition of PONV in this study was administration of a rescue antiemetic; however, varying threshold for use rescue antiemetics after surgery may occur among general wards where patients were managed postoperatively. Third, almost all of the use of postoperative opioid analgesia were planned before surgery, although the indication for such use was occasionally added depending on the invasion of the surgery. In such cases, it is unclear whether postoperative opioid use is considered a risk factor, which may have led to an underestimation of risk. Fourth, antiemetics’ dose and timing were not included in this study, which may have effects on the incidence of PONV. Fifth, after 5-HT3 receptor antagonists became available, the use of propofol and postoperative opioids were increased. These reasons were unclear due to retrospective study; however, these might impact the incidence of PONV. Finally, importantly, the limited availability of antiemetic drugs in Japan is probably associated with the low compliance rate and high incidence of PONV.
In conclusion, we found that the availability of ondansetron contributed to increasing the number of patients with an adequate prophylaxis for PONV; however, it did not lead to decreasing the incidence of PONV. In the future, implementation to improve compliance with the guidelines should be examined.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Gan TJ, Belani KG, Bergese S, Chung F, Diemunsch P, Habib AS, Jin Z, Kovac AL, Meyer TA, Urman RD, Apfel CC, Ayad S, Beagley L, Candiotti K, Englesakis M, Hedrick TL, Kranke P, Lee S, Lipman D, Minkowitz HS, Morton J, Philip BK. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2020;131:411–48.
Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362:1921–8.
Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91:693–700.
Myles PS, Williams DL, Hendrata M, Anderson H, Weeks AM. Patient satisfaction after anaesthesia and surgery: results of a prospective survey of 10,811 patients. Br J Anaesth. 2000;84:6–10.
Hill RP, Lubarsky DA, Phillips-Bute B, Fortney JT, Creed MR, Glass PS, Gan TJ. Cost-effectiveness of prophylactic antiemetic therapy with ondansetron, droperidol, or placebo. Anesthesiology. 2000;92:958–67.
Practical guideline for medication provided by Japanese Society of Aneshtesiology https://anesth.or.jp/files/pdf/other_medicine_20190905.pdf (final access on 20th November, 2023.)
Yunoki K, Mima H. Postoperative nausea and vomiting after artificial joint replacement surgery: comparison between remimazolam and sevoflurane, a propensity score analysis. J Anesth. 2023;37:666–71.
Suzuki Y, Kawashima S, Makino H, Doi M, Nakajima Y. Comparison of postoperative nausea and vomiting between remimazolam and propofol: a propensity score-matched, retrospective, observational, single-center cohort study Korean. J Anesthesiol. 2023. https://doi.org/10.4097/kja.22441.
Choi JY, Lee HS, Kim JY, Han DW, Yang JY, Kim MJ, Song Y. Comparison of remimazolam-based and propofol-based total intravenous anesthesia on postoperative quality of recovery: a randomized non-inferiority trial. J Clin Anesth. 2022;82: 110955.
Gan TJ, Meyer T, Apfel CC, Chung F, Davis PJ, Eubanks S, Kovac A, Philip BK, Sessler DI, Temo J, Tramèr MR, Watcha M. Department of anesthesiology, duke university medical center. consensus guidelines for managing postoperative nausea and vomiting. Anesth Analg. 2003;97:62–71.
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society. Updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;2019(67):674–94.
Peyton PJ, Liskaser G, Ho A, Marsh H, Etherington C, Torlot F, Desai M, Perrett G, Chee B, Leslie K, Myles PS. Postoperative pulmonary complications in the ENIGMA II trial: a post hoc analysis. Anesthesiology. 2023;138:354–63.
Gabel E, Shin J, Hofer I, Grogan T, Ziv K, Hong J, Dhillon A, Moore J, Mahajan A, Cannesson M. Digital quality improvement approach reduces the need for rescue antiemetics in high-risk patients: a comparative effectiveness study using interrupted time series and propensity score matching analysis. Anesth Analg. 2019;128:867–76.
Kappen TH, Vergouwe Y, van Wolfswinkel L, Kalkman CJ, Moons KG, van Klei WA. Impact of adding therapeutic recommendations to risk assessments from a prediction model for postoperative nausea and vomiting. Br J Anaesth. 2015;114:252–60.
Dewinter G, Staelens W, Veef E, Teunkens A, Van de Velde M, Rex S. Simplified algorithm for the prevention of postoperative nausea and vomiting: a before-and-after study. Br J Anaesth. 2018;120:156–63.
Acknowledgements
The authors would like to thank Editage (www.editage.com) for the English language editing.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethics approval
Ethical approval for this study (Approval No. 3962, Chairperson: Prof. M. Yoshizumi) was provided by the local ethics committee on 6 September 2023.
Informed consent
Informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Hirai, S., Ida, M. & Kawaguchi, M. Comparison of prophylaxis strategy for postoperative nausea and vomiting and its incidence before and after the implementation of 5-hydroxytryptamine 3 in surgical setting: a single-center, retrospective study. J Anesth 38, 398–404 (2024). https://doi.org/10.1007/s00540-024-03327-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-024-03327-3