Abstract
Purpose
Catheter-related bladder discomfort (CRBD) is postoperative distress caused by a urinary catheter. CRBD is related to muscarinic receptor activation. Chlorpheniramine has antimuscarinic properties. Hence, this investigation was undertaken to evaluate the efficacy of chlorpheniramine in preventing CRBD in patients undergoing transurethral resection of bladder tumor (TURBT).
Methods
Seventy-six patients scheduled for TURBT under general anesthesia were assigned into two groups. In the chlorpheniramine group (n = 38), 100 ml normal saline containing 0.1 mg/kg chlorpheniramine was infused after general anesthesia induction. In the control group (n = 38), 100 ml normal saline alone was infused. The incidence and severity of CRBD were assessed at 1, 6, and 24 h postoperatively.
Results
The 1-h postoperative incidence of CRBD was lower in the chlorpheniramine group based on the unadjusted analysis [16 (42%) vs. 28 (74%), risk difference 32%, 95% confidence interval 8–51, p = 0.005]. After adjusting the size of the urinary catheter, post hoc analysis showed that the 1-h postoperative incidence of CRBD was lower in the chlorpheniramine group (p = 0.004). The CRBD severity score was lower in the chlorpheniramine group at 1 and 6 h after operation based on the unadjusted analysis (p = 0.012 and p = 0.007, respectively). After adjusting the urinary catheter size, post hoc analysis showed that 1- and 6-h CRBD severity score was lower in the chlorpheniramine group (p = 0.012 and p = 0.008, respectively). The incidence of rescue medication was lower in the chlorpheniramine group [10 (26%) vs. 20 (53%), risk difference 26%, 95% confidence interval 3–47, p = 0.019]. The overall incidence of complications such as nausea, vomiting, dry mouth, flushing, dizziness, and blurred vision was comparable between the two groups.
Conclusions
Chlorpheniramine administration significantly reduces the incidence and severity of CRBD in the patients undergoing TURBT.
Trial registration
KCT0004880 (https://cris.nih.go.kr/)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Catheter-related bladder discomfort (CRBD) is described as a burning sensation along with an urge to void, or as distress in the suprapubic area caused by irritation of the bladder by a urinary catheter [1]. CRBD aggravates postoperative wound pain and is unresponsive to conventional treatment [2]. Muscarinic receptor blockers have been reported to alleviate CRBD [1, 3,4,5].
Male sex and urinary catheter diameter are the risk factors of CRBD [6]. The incidence of bladder cancer is higher in men than in women [7]. The early stage of bladder tumor is treated with transurethral resection of bladder tumor (TURBT) [8]. A large-sized urinary catheter is inserted for patients after TURBT for bladder irrigation; therefore, patients undergoing TURBT are at high risk of CRBD.
Chlorpheniramine is a histamine H1-receptor antagonist, which is used for allergic conditions [9]. Chlorpheniramine is also known to show an antimuscarinic effect [10]. However, possible role of chlorpheniramine in preventing CRBD due to its antimuscarinic property has not been studied.
We hypothesized that perioperative chlorpheniramine administration may decrease the incidence and severity of CRBD. We conducted this investigation to assess the efficacy of chlorpheniramine administration for reducing the incidence and severity of CRBD in patients undergoing TURBT.
Methods
This is a prospective, double-blind, single-center, parallel-arm, and randomized investigation. The clinical trial review board of Korea University in Seoul, Korea, approved this trial (Document no. 2020AN0117). This investigation was registered in the Clinical Research Information Service (KCT0004880).
We acquired written informed consent before patient enrollment. Patients with American Society of Anesthesiologist physical status I–III, aged 18–80 years, and scheduled for TURBT were enrolled from April 2020 to June 2020. Patients with seizure, allergic history to chlorpheniramine, chronic pain, current analgesic use, body mass index of > 35 kg/m2, overactive or neurogenic bladder, bladder outflow obstruction, and urinary catheter of < 18 Fr., pregnant patients were excluded from this trial.
The included patients were randomly assigned to either the chlorpheniramine or control group using Random Allocation Software (ver. 1.0.0; Isfahan University of Medical Sciences, Isfahan, Iran) and the closed envelope method. During a preoperative visit, the anesthetist educated the patient about the symptoms of CRBD (described as a burning sense with an urge to urinate or distress in the suprapubic region).
Attending anesthesiologist, nurse, and patients were blinded to the group assignment. Upon arrival at the operating room, the patient was monitored using non-invasive blood pressure measurement, electrocardiography, and pulse oximetry. The anesthetic depth was evaluated using a bispectral index monitor (A-2000 XP; Aspect Medical Systems, Newton, MA, USA), and the neuromuscular blockade quantification was monitored using acceleromyography (TOF-watch SX; MSD BV, Oss, the Netherlands). Anesthesia was induced with intravenous propofol (2 mg/kg) and remifentanil (1 μg/kg). Supraglottic airway (I-gel; Intersurgical Ltd., Berkshire, UK) insertion was facilitated with intravenous rocuronium (0.6 mg/kg) while assessing the train-of-four counts at the ulnar nerve.
After anesthetic induction, we slowly infused 100 ml of 0.9% saline with 0.1 mg/kg chlorpheniramine in the chlorpheniramine group and 100 ml of 0.9% normal saline in the control group. The investigation drug was prepared by the nurse who was aware of the group assignment.
Desflurane was inhaled and remifentanil was infused continuously to maintain anesthesia. The end-tidal concentration of desflurane and infusion rate of remifentanil were regulated to maintain a systolic blood pressure of ± 20% of the baseline value and bispectral index of 40–60. The surgeon and assistants were blinded to the group assignment. Hypotension during surgery and in the post-anesthetic care unit was treated with ephedrine 4–8 mg or phenylephrine 50–100 µg, and all incidences were recorded. At the end of surgery, train-of-four nerve stimulation was performed. When 2 out of 4 twitches were present with train-of-four, sugammadex 2 mg/kg was infused to antagonize the residual neuromuscular blockade. Time to extubation (the time from the end of the surgery to the removal of the airway device) was assessed. After removal of the airway device, the patients were transported to the post-anesthesia care unit.
When the main procedure was completed, a Foley catheter was inserted and set to the leg without any traction. Continuous bladder irrigation was performed with 0.9% saline through the Foley catheter. The urinary catheter was removed 24 h postoperatively.
CRBD was considered “absent” when the patients did not report any bladder discomfort on asking, “mild” when the patient complained of CRBD only when asked, “moderate” when the patient complained of CRBD without being questioned (and the CRBD was not accompanied by physical movements), and “severe” when the patient complained of CRBD without being questioned but with physical movements (swinging extremities, strong verbal response, and attempt to pull out the catheter) [1, 3,4,5]. The incidence and severity of CRBD were checked at 1, 6, and 24 h postoperatively by a junior anesthesiology resident or a nurse who was blinded to the group allocation. When the patients complained of moderate or severe CRBD or requested treatment for CRBD, intravenous tramadol 50–100 mg was infused as a rescue treatment. CRBD severity was also assessed using a numerical rating scale (0: no discomfort, 10: worst imaginable discomfort) at 1, 6, and 24 h postoperatively. Postoperative pain defined as tingling discomfort at the suprapubic region was evaluated using a numerical rating scale (0 = no pain to 10 = worst imaginable pain) at 1, 6, and 24 h postoperatively. When the pain score was 4 or greater on the numerical rating scale, pethidine 25 mg was administered as a rescue medication. The incidences of postoperative nausea, vomiting, and dry mouth were also evaluated. The Ramsay Sedation score was assessed at 1, 6, and 24 h postoperatively and recorded as follows: 1 (restless, agitated or anxious); 2 (tranquil, oriented and cooperative); 3 (asleep and responds to requests); 4 (brisk response to light glabellar tap or loud sound); 5 (sluggish response to light glabellar taps or loud sound); or 6 (no response) [11]. Patients with a sedation scale score of > 3 were considered sedated. Postoperative cognitive dysfunction was reviewed retrospectively during the postoperative 24 h.
The primary endpoint was the CRBD incidence at 1 h after operation. The secondary endpoints were the incidence and severity of CRBD at each time point and the number of patients treated with tramadol for CRBD.
Statistical analysis
A previous study showed that the incidence of CRBD following TURBT was 89% at 1 h after operation [5]. Chlorpheniramine administration was presumed to decrease the incidence of CRBD to 30%, which was regarded as clinically significant. Thirty-two patients per group were necessary to attain 5% alpha and 80% power in a two-sided comparison. Thirty-eight patients in each group were necessary to compensate for a compliance rate of 95% and a possible dropout rate of 10%.
Categorical outcomes, including the incidence of CRBD, nausea, vomiting, dizziness, dry mouth, sedation, and analgesic use, were analyzed using a chi-square test or Fisher’s exact test when necessary. Continuous variables were assessed for normal distribution using the Kolmogorov–Smirnov test. The Student’s t test or Mann–Whitney U test was applied according to the data distribution. We conducted statistical analyses using IBM SPSS Statistics (ver. 22.0 software; IBM CORP., Armonk, NY). Differences with a p value < 0.05 were considered statistically significant.
The incidence and severity score of CRBD were evaluated at multiple time points. Data at different time points of a single patient may be correlated because they are not independent of each other. Generalized estimating equation (GEE) was applied to consider the correlation among the data at multiple time points and detect the relationship between chlorpheniramine and the incidence and severity of CRBD after adjusting the size of urinary catheter. Unstructured correlation matrix was applied. Linear mixed model (LMM) was executed to consider the correlation among the data at multiple time points and detect the relationship between chlorpheniramine and the CRBD severity score after adjusting the size of urinary catheter. Unstructured correlation matrix was applied. Post hoc analysis after GEE and LMM was performed when the analysis of the interaction showed a certain statistical tendency (p value < 0.1). We conducted GEE and LMM using SAS (ver. 9.4 software; SAS institute, Cary, NC).
Results
Ninety-six patients were screened from April 2020 to June 2020, of whom 20 were excluded because they met the exclusion criteria (n = 10), refused to participate (n = 5), or their surgery was canceled (n = 5), leaving 76 patients for the analysis (Fig. 1). The baseline characteristics of the patients were similar between the groups (Table 1).
The unadjusted analysis showed that the 1-h postoperative incidence of CRBD was lower in the chlorpheniramine group [16 (42%) vs. 28 (74%), risk difference 32%, 95% confidence interval 8–51, p = 0.005, Table 2]. After adjusting the urinary catheter size by GEE, the interaction between group and time in the incidence of CRBD showed a certain tendency (p = 0.069) to execute the post hoc analysis. Post hoc analysis showed that the 1-h postoperative incidence of CRBD was lower in the chlorpheniramine group (p = 0.004).
The 6-h postoperative incidence of CRBD was lower in the chlorpheniramine group before adjusting the urinary catheter size [11 (29%) vs. 22 (58%), risk difference 29%, 95% confidence interval 5–49, p = 0.011]. Post hoc analysis after GEE showed that the 6-h postoperative incidence of CRBD was lower in the chlorpheniramine group (p = 0.021, respectively). The 24-h postoperative incidence of CRBD was comparable both before and after adjusting the urinary catheter size.
The unadjusted analysis showed that the incidence of moderate-to-severe CRBD was comparable at 1, 6, and 24 h after operation (p = 0.185, p = 0.529, and p = 0.152, respectively). The overall incidence of CRBD during postoperative 24 h was lower in the chlorpheniramine group before adjusting the urinary catheter size [19 (50%) vs. 31 (82%), risk difference 32%, 95% confidence interval 8–51, p = 0.004]. The effect of the urinary catheter size was adjusted using GEE. After adjusting the urinary catheter size, the interaction between group and time in the severity of CRBD did not show a significant relationship (p = 0.1515).
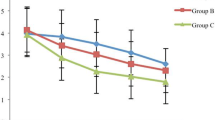
The CRBD severity score was lower in the chlorpheniramine group at 1 and 6 h after operation in the unadjusted analysis (p = 0.012 and p = 0.007, respectively; Table 3). After adjusting the urinary catheter size by LMM, the interaction between group and time in the CRBD severity score showed a certain tendency (p = 0.068) to execute the post hoc analysis. Post hoc analysis showed that 1- and 6-h CRBD severity score was lower in the chlorpheniramine group (p = 0.012 and p = 0.008, respectively).
The rate of rescue medication use was lower in the chlorpheniramine group [10 (26%) vs. 20 (53%), risk difference 26%, 95% confidence interval 3 to 47, p = 0.019, Table 4]. The incidence rates of complications such as nausea [3 (8%) vs. 3 (8%), p = 1.000], vomiting [0 (0%) vs. 1 (3%), p = 1.000], flushing [1 (3%) vs. 2 (5%), p = 1.000], dizziness [2 (5%) vs. 2 (5%), p = 1.000], and blurred vision [1 (3%) vs. 0 (0%), p = 1.000] were comparable. The incidence of dry mouth was also similar between the groups [19 (50%) vs. 11 (29%), risk difference 21%, 95% confidence interval -3 to 42, p = 0.060]. The rate of inotropic and vasopressor use in the perioperative period was comparable [8 (21%) vs. 8 (21%), risk difference 0%, 95% confidence interval -20 to 20, p = 1.000). The incidence of abnormal sedation scale score was also comparable [6 (16%) vs. 4 (11%), risk difference 5%, 95% confidence interval -13 to 23, p = 0.497]. One patient in the control group showed disorientation of space and time, and one patient in the chlorpheniramine group demonstrated anxiety, fear, irritability, and anger.
Discussion
This investigation showed that intraoperative chlorpheniramine administration decreased the CRBD incidence in the immediate postoperative period for patients who underwent TURBT, without severe complications. Intraoperative chlorpheniramine administration decreased the CRBD severity score in the immediate postoperative period and the supplemental medication uses for CRBD.
Patients with a urinary catheter often complain of CRBD after surgery. Although CRBD is a precipitating factor for the emergence agitation at the immediate postoperative period [12], it is often left untreated and neglected. Severe CRBD may induce aggressive behavioral consequences, including the patient pulling out the Foley catheter, which may result in lower urinary tract damage. Prevention of CRBD may increase the postoperative quality of life and decrease the nursing burden of patients undergoing TURBT.
In this investigation, we chose CRBD incidence at 1 h as a primary endpoint. Previous investigations regarding CRBD reported that the CRBD incidence at the postoperative 1 h is higher than that at other investigation time points [1, 4, 5]. CRBD at the immediate postoperative period may increase the workload of the medical staffs and delay the transfer to the general ward, which may increase the risk and cost. The CRBD incidence at 1 h postoperatively was chosen as a primary endpoint because the prevention of CRBD in the immediate postoperative period may have great clinical significance.
A histamine H1-receptor blocker has been used to attenuate histamine-mediated adverse events [13]. Chlorpheniramine, a histamine receptor antagonist, is known to prevent allergic reactions such as histamine release reaction during anesthetic induction using midazolam and ketamine. Its antimuscarinic effect on CRBD, however, has not been evaluated. In this investigation, intraoperative chlorpheniramine administration decreased the incidence and severity of CRBD at the immediate postoperative period. Moreover, the postoperative supplemental use of tramadol for CRBD was reduced. Prevention of moderate-to-severe CRBD may contribute to the decrease in additional medications for CRBD. Opioid analgesics such as tramadol may increase adverse effects including respiratory depression, ileus, nausea, vomiting, pruritus, and urinary retention [14]. Decreasing the number of patients requiring analgesics through CRBD prevention by chlorpheniramine may increase the postoperative safety of patients.
Previous reports regarding bladder discomfort demonstrated that type 2 and 3 muscarinic receptors are related to bladder discomfort [5, 15]. Type 3 muscarinic receptor blockers such as oxybutynin and glycopyrrolate have been investigated for the prevention of bladder discomfort [1, 5]. Chlorpheniramine blocks type 2 muscarinic receptors more selectively [10]. Type 2 muscarinic receptor activation results detrusor smooth muscle contraction [16]. Chlorpheniramine administration may reduce the incidence of bladder discomfort by preventing bladder detrusor muscle contraction. Further investigation regarding type 2 muscarinic receptor blockers and CRBD is necessary.
Previous reports regarding the effects of antimuscarinic agents on CRBD showed increased antimuscarinic side effects in patients treated with muscarinic antagonists [1, 3]. Chlorpheniramine has antimuscarinic side effects such as nausea, vomiting, dizziness, blurred vision, and dry mouth. It has cardiovascular side effects including hypotension and tachycardia. In our investigation, the incidence of antimuscarinic side effects, abnormal sedation scale score, and time to extubation were similar between the groups. The reduction in the postoperative opioid analgesic uses in the chlorpheniramine group may have contributed to the similar rate of complications such as nausea and vomiting. The rates of inotropic and vasopressor use and incidence of hypotension were not significantly different between the control and chlorpheniramine groups. Chlorpheniramine administration decreased the incidence and severity of CRBD, without serious side effects.
The incidence of CRBD, in this investigation, is relatively high compared with that in a previous report [3]. It is, however, in line with the result of investigations in post-TURBT populations [4, 5]. The population in this investigation has several risk factors of CRBD. After TURBT, a large-sized urinary catheter was inserted. Most of the patients who underwent TURBT were male. The bladder was irrigated continuously to remove blood clots after TURBT. These factors may have resulted in the relatively higher incidence of CRBD in our study. This investigation showed that chlorpheniramine is effective for the prevention of CRBD in patients at high risk of bladder discomfort.
Several limitations of the current investigation should be considered. First, a single dose of chlorpheniramine 0.1 mg/kg was provided in this study. The dose–response effect of chlorpheniramine was not assessed. Second, repeated assessment at postoperative 1, 6, and 24 h may cause additional bias. Patients might complain of CRBD symptom at postoperative 6 and 24 h. The severity of CRBD at postoperative 6 and 24 h should be interpreted cautiously. Third, although the urinary catheter size was comparable between groups, 20 Fr.-sized catheter was more frequent in the chlorpheniramine group. Relatively small-sized Foley catheter may influence the lower incidence of CRBD in the chlorpheniramine group. We applied GEE to minimize the bias regarding repeated measurements and the size of urinary catheters. Fourth, this study did not analyze postoperative cognitive dysfunction, while chlorpheniramine is associated with its development. Considering that antimuscarinic agents is associated with cognitive disorder [17], the lack of cognitive dysfunction test was a major limitation of this study. Although Ramsay sedation scale and retrospective data showed that there was no significant difference in terms of neurologic disorder, further research is required to detect the perioperative chlorpheniramine and postoperative cognitive dysfunction.
In conclusion, chlorpheniramine administration prevented the incidence of CRBD in the patients who underwent TURBT, without serious side effects. It also decreased the number of patients requiring analgesics. Therefore, we recommend the use chlorpheniramine in patients at high risk of CRBD.
References
Agarwal A, Dhiraaj S, Singhal V, Kapoor R, Tandon M. Comparison of efficacy of oxybutynin and tolterodine for prevention of catheter related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Br J Anaesth. 2006;96:377–80.
Tauzin-Fin P, Sesay M, Svartz L, Krol-Houdek MC, Maurette P. Sublingual oxybutynin reduces postoperative pain related to indwelling bladder catheter after radical retropubic prostatectomy. Br J Anaesth. 2007;99:572–5.
Agarwal A, Yadav G, Gupta D, Singh PK, Singh U. Evaluation of intra-operative tramadol for prevention of catheter-related bladder discomfort: a prospective, randomized, double-blind study. Br J Anaesth. 2008;101:506–10.
Kim HC, Lee YH, Jeon YT, Hwang JW, Lim YJ, Park JE, Park HP. The effect of intraoperative dexmedetomidine on postoperative catheter-related bladder discomfort in patients undergoing transurethral bladder tumour resection: a double-blind randomised study. Eur J Anaesthesiol. 2015;32:596–601.
Kim HC, Lim SM, Seo H, Park HP. Effect of glycopyrrolate versus atropine coadministered with neostigmine for reversal of rocuronium on postoperative catheter-related bladder discomfort in patients undergoing transurethral resection of bladder tumor: a prospective randomized study. J Anesth. 2015;29:831–5.
Binhas M, Motamed C, Hawajri N, Yiou R, Marty J. Predictors of catheter-related bladder discomfort in the post-anaesthesia care unit. Ann Fr Anesth Reanim. 2011;30:122–5.
Johansson SL, Cohen SM. Epidemiology and etiology of bladder cancer. Semin Surg Oncol. 1997;13:291–8.
Rodriguez Faba O, Gaya JM, López JM, Capell M, De Gracia-Nieto AE, Gómez Correa E, Breda A, Palou J. Current management of non-muscle-invasive bladder cancer. Minerva Med. 2013;104:273–86.
Rumore MM. Clinical pharmacokinetics of chlorpheniramine. Drug Intell Clin Pharm. 1984;18:701–7.
Yasuda SU, Yasuda RP. Affinities of brompheniramine, chlorpheniramine, and terfenadine at the five human muscarinic cholinergic receptor subtypes. Pharmacotherapy. 1999;19:447–51.
Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2:656–9.
Yu D, Chai W, Sun X, Yao L. Emergence agitation in adults: risk factors in 2,000 patients. Can J Anaesth. 2010;57:843–8.
Kimura K, Adachi M, Kubo K. H1- and H2-receptor antagonists prevent histamine release in allergic patients after the administration of midazolam-ketamine. A randomized controlled study. Inflamm Res. 1999;48:128–32.
Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse events associated with postoperative opioid analgesia: a systematic review. J Pain. 2002;3:159–80.
Ryu JH, Hwang JW, Lee JW, Seo JH, Park HP, Oh AY, Jeon YT, Do SH. Efficacy of butylscopolamine for the treatment of catheter-related bladder discomfort: a prospective, randomized, placebo-controlled, double-blind study. Br J Anaesth. 2013;111:932–7.
Yamanishi T, Chapple CR, Chess-Williams R. Which muscarinic receptor is important in the bladder? World J Urol. 2001;19:299–306.
Pagoria D, O’Connor RC, Guralnick ML. Antimuscarinic drugs: review of the cognitive impact when used to treat overactive bladder in elderly patients. Curr Urol Rep. 2011;12:351–7.
Acknowledgements
We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2018R1C1B6007539).
Author information
Authors and Affiliations
Contributions
Conceptualization: HCK, HH, SWL. Data curation: HH, JEC. Formal analysis: HCK, HH, SWL, JEC. Funding acquisition: HH. Investigation: JEC, SWL. Methodology: HCK, HH, SWL, JEC. Resources: JEC, SWL. Software: HH, HCK. Supervision: HCK. Validation: HH, SWL, JEC. Visualization: HCK. Writing—original draft: HCK, HH. Writing—review and editing: HH, SWL, JEC.
Corresponding author
Ethics declarations
Conflict of interest
No competing interests declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Huh, H., Lee, S.W., Cho, J.E. et al. Effect of chlorpheniramine administration on postoperative catheter-related bladder discomfort in patients undergoing transurethral excision of bladder tumor: a prospective randomized study. J Anesth 35, 646–653 (2021). https://doi.org/10.1007/s00540-021-02970-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-021-02970-4