Abstract
Transnasal humidified rapid insufflation ventilatory exchange (THRIVE) is a recent technique that delivers warm humidified high flow oxygen to patients, allowing for prolonged apneic oxygenation. A review of current literature was performed to determine the use of THRIVE in apneic patients undergoing surgery in a shared airway setting. An initial free hand search was done to identify keywords followed by a systematic search of major databases with no date or language restrictions. Inclusion criteria include all apneic patients who receive THRIVE for any operative procedure. Fifteen studies fulfilled the inclusion criteria. There were ten case series, two case reports, two review articles and one randomized controlled trial. All of the studies discussed the use of THRIVE during laryngopharyngeal surgeries. The median apnea time reported ranged between 13 and 27 min. There were no significant complications reported as a result of using THRIVE. Most studies identified in this review were observational in nature involving laryngopharyngeal procedures. They have demonstrated THRIVE to be effective in providing apneic oxygenation during short procedures in adult patients. Further studies are required to determine the limitations of safe use in specific populations and when THRIVE is combined with diathermy or laser use.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Transnasal humidified rapid insufflation ventilatory exchange (THRIVE) is a technique that delivers continuous, warm and humidified 100% oxygen at a high flow rate (up to 120 L min−1) via nasal cannulae to patients with clinical apnea. High flow oxygen has been used in the intensive care units, respiratory medicine and in peri-operative medicine for pre-oxygenation [1, 2]. However, apneic oxygenation solely using THRIVE in an operative setting has only been recently described by Patel and Nouraei [3].
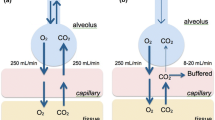
The effectiveness of THRIVE relies upon the patient having a patent upper airway. Jaw thrust during THRIVE is a useful adjunct to open the patient’s airway. During laryngopharyngeal surgery, where general anesthesia with clinical apnea is required, a patent airway is provided by suspension laryngoscopy. The continuous high flow of 100% oxygen causes denitrogenation of the anatomical dead space [4]. During apnea, alveolar oxygen absorption exceeds carbon dioxide production due to the relative differences in blood solubility, generating a negative pressure gradient that favors bulk flow of gas from the anatomical dead space into the alveoli—a phenomenon called aventilatory mass flow [5]. Some ventilation is produced as the continuous insufflation of high flow oxygen flushes out the expired carbon dioxide, reducing the rate of carbon dioxide accumulation and dead space rebreathing. This allows the extended use of THRIVE with a reduced risk of hypercapnia in an apneic patient [2,3,4, 6]. In healthy volunteers, high flow oxygen increases airway pressure by an average of 1.16 cmH2O for every 10 L min−1 increase in flow rate [7]. The positive airway pressure generated assists in alveolar recruitment which prevents atelectasis and reduces shunting, therefore improving oxygenation. 100% humidification of the oxygen also prevents drying of the nasopharyngeal and tracheobronchial mucosa, maintaining mucociliary clearance and patient comfort [2].
This is a relatively new technique in anesthesia. The optimal patient population for its use and outcomes of THRIVE in apneic patients have not yet been established, therefore a review was conducted to systematically gather evidence and determine the types of studies available to provide an overview of the use of THRIVE in clinically apneic patients undergoing surgery on the upper aerodigestive tract.
Methods
A review was performed with a systematic search strategy. This review has been conducted according to the Arksey and O’Malley framework and PRISMA guidelines [9].
Search strategy
Research aims:
Determine the scope of reported outcomes when using THRIVE in the operative setting.
Determine the types of procedures successfully performed using THRIVE only.
Inclusion criteria:
Using THRIVE, high flow is defined as oxygen flow rate at 15 L min−1 or above throughout a procedure [10].
Patients need to be clinically apneic.
Any age groups.
All types of studies.
Exclusion criteria:
Patients who are spontaneously ventilating.
High oxygen flow rate defined at a rate less than 15 L min−1.
THRIVE use for pre-oxygenation and induction of anesthesia only.
We conducted a free hand search to identify keywords for the systematic search. The three databases (PUBMED, EMBASE and PROQUEST) along with Google scholar were searched using a keyword matrix (Supplementary Appendix A) on the 21st of August 2019 with no date or language restriction. Clinicaltrials.gov and the Australian and New Zealand Clinical Trials Registry (ANZCTR) were also searched to determine any current clinical trials. Clinicaltrials.gov listed nine current clinical trials that fulfill our inclusion criteria (Supplementary Table 1). No studies were identified from ANZCTR. The PRISMA diagram is presented in Fig. 1. Level one screening of title and abstracts was performed by one reviewer (LH) and classified into three groups ‘included’, ‘excluded’, and ‘review full text’. After level two screening of full texts, fifteen studies have been identified to fulfill the inclusion criteria. No further studies were identified after reviewing the reference lists of the included articles. Studies were not excluded based on quality assessment as this is designed to be a literature review [8]. We included all the studies that met the inclusion criteria. Data were extracted by LH and verified by a second reviewer (ND).
Results
This review identified fifteen studies meeting the inclusion criteria. The reported outcomes of these studies were: type of operative procedures using THRIVE, patient demographics, ASA status, BMI or weight, duration of pre-oxygenation, need for rescue ventilation and/or intubation, lowest oxygen level, duration of apnea and highest CO2 level measured.
Study characteristics
Seven of the included studies were prospective case series, three studies were retrospective case series, two were case reports, one was a randomized single-blinded control study and two were review articles. All included studies were conducted after 2015 despite the search strategy not having a date restriction. The authors from the identified studies were affiliated with anesthesiology and otorhinolaryngology in all the studies. Three conference abstracts were identified but excluded as not enough information was provided [11,12,13]. More details on the study characteristics are presented in Table 1.
Patient population
The patient demographics are described in Table 2. Age, weight or BMI were presented as mean or median. One outlier in regards to patient characteristics was a case report that documented the successful use of THRIVE in a patient with a BMI of 40 [14]. Kotwinski discussed the use of THRIVE in a review article, therefore, a specific patient population was not discussed [15]. Ridgway also discussed THRIVE in a review article with mention of its use in the pediatric population [16].
Devices used
Ten studies used the high flow oxygen device Optiflow™, one study used Airvo2™ (Fisher & Paykel, Auckland, New Zealand) [3, 6, 14, 17,18,19,20,21,22,23,24]. Two studies reported using other devices—Peri-Operative Insufflatory Nasal Therapy System (POINT, Armstrong Medical, United Kingdom) and Comfort Flo® (Teleflex, United States) [10, 25].
Procedures performed with THRIVE
All the studies identified in this review used THRIVE in the context of laryngeal and pharyngeal surgeries. Twelve studies performed laryngeal surgery with interventions [6, 10, 14, 17,18,19,20, 23,24,25]. Interventions included: excision of lesions (granuloma, polyp, papilloma, retention cyst), rigid bronchoscopy, injection thyroplasty, biopsy of lesions, balloon dilatation of stenosis and stapling of pharyngeal pouch. Balloon dilatation was used for both supraglottic and subglottic stenosis. Two studies performed pharyngolaryngeal surgery but did not specify further details about the surgery [3, 21]. Three studies reported the use of CO2 and KTP laser with THRIVE [18, 22, 23]. Ridgway detailed that their center used THRIVE in the pediatric population for aryepiglottoplasty and laser airway surgery, however, it did not specify the operative conditions and the success of its use [16]. Details of the procedures performed in each study are presented in Table 3.
Outcome measures
Eleven studies reported using THRIVE for pre-oxygenation, all of them reporting pre-oxygenating for at least 3 min or more. The flow rate for pre-oxygenation varied between 10 and 80 L min−1 (Table 4). The flow rate increased to 50–80 L min−1 for the duration of apnea. Ridgway and colleagues reported using a flow rate of 2 L kg−1 min−1 for pediatric patients [16]. The reported mean or median apnea time ranged from 13 to 27 min (Table 4) but had been reported up to 65 min by Patel and Nouraei [3]. Details of duration and flow rates for pre-oxygenation and apnea are presented in Table 4.
The lowest documented transient peripheral oxygen saturation was 60% [19, 23]. Five studies recorded a peripheral desaturation below 90% in eight patients. The lowest recorded oxygen saturation along with highest recorded carbon dioxide levels are presented in Table 5. Four studies measured PaCO2 (arterial carbon dioxide) and six studies measured the highest ETCO2 (end-tidal carbon dioxide) at the end of the procedure. Two studies reported both measures, but five studies did not measure either PaCO2 or highest ETCO2. Four studies described pre-determined discontinuation criteria based on physiological monitoring. Forty patients in total (11%) required rescue ventilation with supraglottic jet ventilation, bag and mask ventilation or intubation (Table 4). No studies described the duration or load (area under a safe saturation threshold or above a CO2 threshold) of such conditions. Nor did they describe long term complications or complications due to hypoxemia or hypercapnia. The muscle relaxant and anesthesia medications used in each study are reported in Table 6.
Discussion
The studies included in this review have described THRIVE in a range of patients undergoing various surgeries with a shared airway setting. There are potentially significant advantages for using THRIVE compared to other conventional airway management techniques in the shared airway setting. The tubeless nature allows for better visualization, and space for intervention in the larynx. This may correspond to improved operative outcomes or reduced operative times. It avoids complications such as laryngeal trauma from an endotracheal tube and barotrauma from jet ventilation. Vocal folds are able to be visualized in the natural position when performing augmentation surgery such as injection thyroplasty. The small positive airway pressure provided by the high flow rate increases alveolar recruitment and reduces atelectasis when compared with low flow techniques [2, 6, 26].
The use of THRIVE in the operative setting appears safe with the reported longest apnea duration being 65 min [3]. However, the duration of apnea for each study which is presented in Table 4 should be interpreted with caution for the following reasons. When THRIVE is used with short surgical procedures, the apnea time will be short with completion of the procedure, therefore it could be underestimated. When THRIVE is used in longer procedures, a more accurate representation of the apnea duration will be reflected, but there is an increased likelihood that rescue ventilation may be required. All the included studies used THRIVE for upper airway surgeries therefore the duration required for the operation would be similar. As demonstrated in Table 4, desaturation is the main reason for implementing rescue ventilation [25]. While THRIVE appears to benefit the majority of patients, some studies reported dangerously low peripheral oxygen saturation at SpO2 of 60% or high carbon dioxide levels with ETCO2 measuring up to 120 mmHg. It is therefore important for both the surgeon and anesthetist to be aware of an alternate airway plan to act quickly to rectify this if required. The exact threshold for intervention will depend on multiple factors, including oxygen and carbon dioxide levels, other physiological parameters, the surgical procedure and any anticipated difficulty in implementing the backup ventilation strategy.
THRIVE has its own sets of limitations. It does not provide a definitive or secure airway; therefore, patients remain at risk of reflux and aspiration of gastric content. The high flow rate of oxygen is contra-indicated in patients with base of skull fractures and facial fractures. Patients with a markedly deviated septum or nasal pathology causing significant nasal obstruction may not achieve the expected result due to poor air flow through the nasal cavity. In our review, Tam and colleagues reported a successful case of using THRIVE at FiO2 of 1.0 with CO2 laser [18]. Huang and colleagues described turning off THRIVE prior to using KTP laser with no complications [23]. Lau and colleagues paused THRIVE intermittently or reduced FiO2 to 0.30 using an air/oxygen blender followed by suctioning out airway gasses before using CO2 laser [22]. There were no reports of airway fire involving laser with THRIVE and one case report of brief ignition while using monopolar diathermy with THRIVE within the oral cavity due to arcing [27]. However, airway fire has been described when using lasers in an oxygen-rich environment [28,29,30]. Therefore, using THRIVE during laser surgery should be done with caution due to the risk of airway fire and limited data available to support the safety of this combination.
Ventilation is required to eliminate carbon dioxide from the lung, which is achieved to a small degree with the high flow rate of THRIVE [6]. Gustafsson and colleagues demonstrated a slower accumulation of end-tidal CO2 when using THRIVE at a rate of 1.8 mmHg min−1 compared to an increase of 3.2–4.2 mmHg min−1 for low flow devices [6, 31, 32]. Even though THRIVE is able to prolong apnea to a certain degree, hypercapnia and the resulting acidemia remains the key limiting factor for the prolonged use of THRIVE [10]. Additional monitoring was implemented in ten studies to monitor carbon dioxide levels in the body. End-tidal CO2 was measured using supraglottic devices or with a bag-mask circuit in several studies [3, 6, 10, 17, 24]. It has been used as a means of obtaining an inference to the rise in arterial CO2. However, it cannot be performed during apneic oxygenation, only before or after an operation. A dangerous rise of arterial CO2 may not be detected until the end of the procedure. Transcutaneous CO2 provides an alternative method of monitoring. It is continuous and is reported to be an accurate reflection of arterial CO2 [6]. The use of transcutaneous CO2 monitor is non-invasive and may be able to clearly define an upper limit of CO2 upon which THRIVE should be discontinued and ventilation re-established. The study by Rajan and colleagues found a slightly higher CO2 level in the THRIVE group compared with the low flow O2 group [21]. This is inconsistent with the majority of the existing literature and most likely reflects a difference which arose due to chance and the small difference between the groups at baseline which was unadjusted for in their analysis. Despite the caution surrounding hypercapnia, there have been studies that demonstrate respiratory acidosis can be well tolerated when patients are well oxygenated [10, 33, 34]. Permissive hypercapnia is also used in the intensive care setting to allow lung protective ventilation [10, 34, 35]. None of the studies included in this review reported complications associated with hypercapnia. However, careful patient selection is required to avoid those who may deteriorate from hypercapnia such as those with pulmonary hypertension.
None of the reviewed studies used THRIVE alone for apneic oxygenation in the pediatric population. It was mentioned by Ridgway and colleagues in their literature review and used by Riva and colleagues during intermittent apnea interspersed with periods of intubation or bag-mask ventilation [36, 37]. High flow rate was reported at 2.0–4.0 L kg−1 min−1 in neonates and infants depending on weight [37,38,39]. Pediatric respiratory physiology differs significantly from adults in the neonatal phase, gradually approximating adult values as age increases. The pediatric population have higher oxygen demand due to increased metabolic oxygen requirement (7 ml kg−1 as a neonate compared to adults at 3.5 ml kg−1) with an unchanged functional residual capacity (FRC) on a per kg basis and a higher minute ventilation on a per kg basis (120–140 mL kg−1 as a neonate compared with 70 ml kg−1 as an adult). This results in shorter apnea time before oxygen desaturation occurs and hypercapnia develops [40, 41]. The natural intrinsic positive end expiratory pressure due to neonates being obligate nasal breathers with narrower nasal passages along with a higher closing capacity may, however, benefit from the slight positive pressure provided by THRIVE which may prevent atelectasis and reduce the ventilation-perfusion mismatch [41]. Riva demonstrated that pediatric patients can maintain a median (IQR) apnea time of 7.6 (6.2–9.1) min in the group with high flow oxygen [36]. However, it did not have a statistically significant difference in apnea time when compared to the group with low flow oxygen (0.2 L kg−1 min−1) at FiO2 of 1.0 [36]. THRIVE was shown to not help with CO2 clearance in this patient population. Apnea window of a maximum of 10–12 min was suggested. Therefore, it is unlikely to be safe to use THRIVE for procedures that require extended apneic time in the pediatric population. However, this can be extremely valuable in an emergency airway setting given the evidence of maintaining apnea for around 10 min. Our review also found limited reported data on the use of THRIVE in the obese, elderly or obstetric population and in those with reduced cardiorespiratory reserves, obstructive sleep apnea or chronic obstructive pulmonary disease.
Several studies identified in this review have cautioned the use of THRIVE in those with high body mass index (BMI) [3, 17]. Lee and colleagues described the successful use of THRIVE in a patient with class III obesity (BMI of 40) with no complications. However, several other studies reported desaturation in those with a higher BMI, requiring alternate airway management [3, 10, 17, 20, 23, 24]. Waters and colleagues demonstrated there is a significantly higher rate of desaturation at 30 min in those with higher BMI [24]. Huang and colleagues also demonstrated that patients with BMI above 30 kg m−2 or weight above 80 kg are 5.7 and 5.2 times more likely to require rescue ventilation [23]. The FRC is known to decrease in the supine position during anesthesia which increases intra-pulmonary shunt [42, 43]. Patients with a high BMI have further reduction in FRC with higher risks of gastric acid regurgitation and cardiorespiratory comorbidities [2]. The obese population has been shown to have significantly shorter durations of apnea before desaturation compared to controls with normal weight despite pre-oxygenation [44]. Therefore, the same mechanism for desaturation is likely to apply when using THRIVE. Based on this evidence, it is likely that an inverse relationship exists between weight or BMI and the maximum duration of safe THRIVE use. Although, the exact nature of the relationship and the safe limits in clinical use require further characterization.
The inclusion criteria for this review limited the search to apneic patients to explore the use of THRIVE in apneic oxygenation. THRIVE use during apnea was mainly described in otorhinolaryngology because pharyngeal and laryngeal procedures often require neuromuscular blockers. The physiology is different when applying high flow oxygen to those who remain spontaneously breathing as ventilation reduces carbon dioxide accumulation [45]. There are emerging studies using high flow oxygen in patients who remain spontaneously ventilating during video-assisted thoracoscopy and bronchoscopy [46]. However, detailed exploration of its effects in those who remain spontaneously ventilating is beyond the scope of this review.
Current evidence suggested that THRIVE is effective for use in apneic patients, especially in those undergoing pharyngeal and laryngeal surgery. However, further research into certain patient populations such as pediatrics, those with high BMI, obstructive sleep apnea, and the elderly is still required. An important limitation of this review is that the currently available studies are mainly observational case series and case reports. This is expected due to the novelty of this technique. The best method of monitoring the upper limits of carbon dioxide and pH are yet to be determined. To enable scientific progress these variables should be reported in future THRIVE studies. The findings from this review can be used to guide future research and the design of clinical trials to identify which population groups can safely use THRIVE for apneic oxygenation in the operative setting.
References
Mir F, Patel A, Iqbal R, Cecconi M, Nouraei SA. A randomised controlled trial comparing transnasal humidified rapid insufflation ventilatory exchange (THRIVE) pre-oxygenation with facemask pre-oxygenation in patients undergoing rapid sequence induction of anaesthesia. Anaesthesia. 2017;72(4):439–43.
Helviz Y, Einav S. A systematic review of the high-flow nasal cannula for adult patients. Crit Care. 2018;22(1):71.
Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015;70(3):323–9.
Moller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, Schmid O, Tatkov S. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol (1985). 2015;118(12):1525–32.
Rudlof B, Hohenhorst W. Use of apneic oxygenation for the performance of pan-endoscopy. Otolaryngol Head Neck Surg. 2013;149(2):235–9.
Gustafsson IM, Lodenius A, Tunelli J, Ullman J, Jonsson Fagerlund M. Apnoeic oxygenation in adults under general anaesthesia using transnasal humidified rapid-insufflation ventilatory exchange (THRIVE)—a physiological study. Br J Anaesth. 2017;118(4):610–7.
Parke RL, Bloch A, McGuinness SP. Effect of very-high-flow nasal therapy on airway pressure and end-expiratory lung impedance in healthy volunteers. Respir Care. 2015;60(10):1397–403.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Lyons C, Callaghan M. Apnoeic oxygenation with high-flow nasal oxygen for laryngeal surgery: a case series. Anaesthesia. 2017;72(11):1379–87.
Valdinger S, Norris A, Rollason C, Sycamore H, Evans D. Transnasal humidified rapid-insufflation ventilatory exchange in ENT surgery: a case series. Anaesthesia. 2017;72:76.
Margarson M. Nasal high flow oxygen therapy: what the anaesthetist should know. J Clin Monit Comput. 2017;31(3):498.
Davies S, Vaidya A, Shankar R, Patel S. When plan A fails. Anaesthesia. 2018;73:41.
Lee SJ, Quek KH. Facilitating airway surgery in a morbidly obese patient using transnasal humidified rapid insufflation ventilatory exchange (THRIVE). Case Rep Anesthesiol. 2018;2018:5310342.
Kotwinski D, Paton L, Langford R. The role of high flow nasal oxygen therapy in anaesthesia. Br J Hosp Med (Lond). 2018;79(11):620–7.
Ridgway R, Dumbarton T, Brown Z. Update on ENT anaesthesia in children. Anaesth Intensive Care Med. 2019;20(1):56–60.
To K, Harding F, Scott M, Milligan P, Nixon IJ, Adamson R, McNarry AF. The use of transnasal humidified rapid-insufflation ventilatory exchange in 17 cases of subglottic stenosis. Clin Otolaryngol. 2017;42(6):1407–10.
Tam K, Jeffery C, Sung CK. Surgical management of supraglottic stenosis using intubationless optiflow. Ann Otol Rhinol Laryngol. 2017;126(9):669–72.
Yang S-H, Wu C-Y, Tseng W-H, Cherng W-Y, Hsiao T-Y, Cheng Y-J, Chan KC. Nonintubated laryngomicrosurgery with transnasal humidified rapid-insufflation ventilatory exchange: a case series. J Formos Med Assoc. 2019;118:1138–43.
Maupeu L, Raguin T, Hengen M, Diemunsch P, Schultz P. Indications of transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) in laryngoscopy, a prospective study of 19 cases. Clin Otolaryngol. 2019;44:182–6.
Rajan S, Joseph N, Tosh P, Kadapamannil D, Paul J, Kumar L. Effectiveness of transnasal humidified rapid-insufflation ventilatory exchange versus traditional preoxygenation followed by apnoeic oxygenation in delaying desaturation during apnoea: a preliminary study. Indian J Anaesth. 2018;62(3):202–7.
Lau J, Loizou P, Riffat F, Stokan M, Palme CE. The use of THRIVE in otolaryngology: our experiences in two Australian tertiary facilities. Aust J Otolaryngol. 2019;2:22.
Huang L, Athanasiadis T, Woods C, Dharmawardana N, Ooi EH. The use of transnasal humidified rapid insufflation ventilatory exchange in laryngeal and pharyngeal surgery: Flinders case series. Aust J Otolaryngol. 2019;2:17.
Waters E, Kellner M, Milligan P, Adamson RM, Nixon IJ, McNarry AF. The use of transnasal humidified rapid-insufflation ventilatory exchange (THRIVE) in one hundred and five upper airway endoscopies. A case series. Clin Otolaryngol. 2019. https://doi.org/10.1111/coa.13408.
Ebeling CG, Riccio CA. Apneic oxygenation with high-flow nasal cannula and transcutaneous carbon dioxide monitoring during airway surgery: a case series. A&A Pract. 2019;12:366–8.
Ritchie JE, Williams AB, Gerard C, Hockey H. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care. 2011;39(6):1103–10.
Onwochei D, El-Boghdadly K, Oakley R, Ahmad I. Intra-oral ignition of monopolar diathermy during transnasal humidified rapid-insufflation ventilatory exchange (THRIVE). Anaesthesia. 2017;72(6):781–3.
Stuermer KJ, Ayachi S, Gostian AO, Beutner D, Huttenbrink KB. Hazard of CO(2) laser-induced airway fire in laryngeal surgery: experimental data of contributing factors. Eur Arch Otorhinolaryngol. 2013;270(10):2701–7.
Santos P, Ayuso A, Luis M, Martinez G, Sala X. Airway ignition during CO2 laser laryngeal surgery and high frequency jet ventilation. Eur J Anaesthesiol. 2000;17(3):204–7.
Casey KR, Fairfax WR, Smith SJ, Dixon JA. Intratracheal fire ignited by the Nd-YAG laser during treatment of tracheal stenosis. Chest. 1983;84(3):295–6.
Eger EI, Severinghaus JW. The rate of rise of PaCO2 in the apneic anesthetized patient. Anesthesiology. 1961;22:419–25.
Stock MC, Schisler JQ, McSweeney TD. The PaCO2 rate of rise in anesthetized patients with airway obstruction. J Clin Anesth. 1989;1(5):328–32.
Jooste KH. Anaesthesia in bronchography; endotracheal insufflation of oxygen during apnoea. Anaesthesia. 1955;10(1):59–66.
O’Croinin D, Ni Chonghaile M, Higgins B, Laffey JG. Bench-to-bedside review: permissive hypercapnia. Crit Care. 2005;9(1):51–9.
Bautista AF, Akca O. Hypercapnia: is it protective in lung injury? Med Gas Res. 2013;3(1):23.
Riva T, Pedersen TH, Seiler S, Kasper N, Theiler L, Greif R, Kleine-Brueggeney M. Transnasal humidified rapid insufflation ventilatory exchange for oxygenation of children during apnoea: a prospective randomised controlled trial. Br J Anaesth. 2018;120(3):592–9.
Riva T, Theiler L, Jaquet Y, Giger R, Nisa L. Early experience with high-flow nasal oxygen therapy (HFNOT) in pediatric endoscopic airway surgery. Int J Pediatr Otorhinolaryngol. 2018;108:151–4.
Riva T, Seiler S, Stucki F, Greif R, Theiler L. High-flow nasal cannula therapy and apnea time in laryngeal surgery. Paediatr Anaesth. 2016;26(12):1206–8.
Humphreys S, Rosen D, Housden T, Taylor J, Schibler A. Nasal high-flow oxygen delivery in children with abnormal airways. Paediatr Anaesth. 2017;27(6):616–20.
Caruso TJ, Gupta A, Sidell DR, Darling C, Rodriguez S, Fonseca A, Tsui B. The successful application of high flow nasal oxygen during microdirect laryngoscopy and bronchoscopy in patients under 7 kg. J Clin Anesth. 2019;52:27–8.
Gormley S, Crean P. Basic principles of anaesthesia for neonates and infants. BJA Educ. 2001;1(5):130–3.
Fraioli RL, Sheffer LA, Steffenson JL. Pulmonary and cardiovascular effects of apneic oxygenation in man. Anesthesiology. 1973;39(6):588–96.
Don HF, Wahba M, Cuadrado L, Kelkar K. The effects of anesthesia and 100 per cent oxygen on the functional residual capacity of the lungs. Anesthesiology. 1970;32(6):521–9.
Berthoud MC, Peacock JE, Reilly CS. Effectiveness of preoxygenation in morbidly obese patients. Br J Anaesth. 1991;67(4):464–6.
Booth AWG, Vidhani K, Lee PK, Thomsett CM. SponTaneous Respiration using IntraVEnous anaesthesia and Hi-flow nasal oxygen (STRIVE Hi) maintains oxygenation and airway patency during management of the obstructed airway: an observational study. Br J Anaesth. 2017;118(3):444–51.
Wang ML, Hung MH, Chen JS, Hsu HH, Cheng YJ. Nasal high-flow oxygen therapy improves arterial oxygenation during one-lung ventilation in non-intubated thoracoscopic surgery. Eur J Cardio-Thorac Surg. 2018;53(5):1001–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest to declare.
Ethical approval
Ethical approval is not required as this is a narrative review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
About this article
Cite this article
Huang, L., Dharmawardana, N., Badenoch, A. et al. A review of the use of transnasal humidified rapid insufflation ventilatory exchange for patients undergoing surgery in the shared airway setting. J Anesth 34, 134–143 (2020). https://doi.org/10.1007/s00540-019-02697-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-019-02697-3