Abstract
Purpose
Malignant hyperthermia (MH) is an inherited muscle disorder caused by abnormal elevations of intracellular calcium (Ca2+) in skeletal muscle. There are several reports of myotoxicity caused by local anesthetics, and the increased intracellular Ca2+ is considered to be an important cause. However, there is insufficient evidence regarding myotoxicity in MH-susceptible individuals when large doses of local anesthetics are administered. This study investigated the effect of MH predisposition on myotoxicity.
Methods
Human skeletal muscle samples were obtained from 22 individuals to determine susceptibility to MH, and were evaluated according to whether their Ca2+-induced Ca2+ release (CICR) rates were accelerated or not. This study was performed using surplus muscle that remained after the CICR rate test. We calculated the 50% effective concentration (EC50) values of three local anesthetics, namely lidocaine, levobupivacaine, and ropivacaine using the ratiometric dye Fura-2 AM. Significance was tested using the unpaired t test.
Results
In the accelerated and unaccelerated groups, respectively, the mean ± SD of the EC50 values were 1.52 ± 0.72 and 1.75 ± 0.37 mM for lidocaine (p = 0.42), 0.72 ± 0.36 and 0.79 ± 0.46 mM for levobupivacaine (p = 0.68), and 1.21 ± 0.35 and 1.62 ± 0.57 mM for ropivacaine (p = 0.06). These values were similar in individuals with and without MH predisposition.
Conclusion
The myotoxicity of local anesthetics was equivalent in individuals with and without predisposition to MH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant hyperthermia (MH) is an inherited muscle disorder induced by volatile anesthetics and depolarizing muscle relaxants. Its main characteristic is abnormal elevation of intracellular Ca2+ concentrations in skeletal muscle, a phenomenon that is closely linked to dysfunction of ryanodine receptor 1 (RYR1), and a Ca2+-releasing channel in the sarcoplasmic reticulum (SR) of skeletal muscle [1, 2]. The in vitro contracture test in Europe and the caffeine–halothane contracture test in North America have been the gold standards for the diagnosis of MH. By contrast, in Japan, the diagnosis of MH predisposition is based on the Ca2+-induced Ca2+ release (CICR) rate test, which is used to assess the Ca2+ release ability of RYR1.
There are several reports of myotoxicity caused by local anesthetics. Zink et al. reported that when 8.7 mM bupivacaine and 13.7 mM ropivacaine were continuously infused through femoral nerve catheters (8 mL/h) over 6 h in piglets, both local anesthetics produced irreversible skeletal muscle damage [3]. Furthermore, Neal et al. reported that three individuals who received adductor canal block with 63 mM lidocaine or 53 mM mepivacaine bolus followed by 6.6 mM ropivacaine at 8 mL/h developed progressive, profound weakness of the quadriceps muscles [4]. One of the primary underlying mechanisms of myotoxicity by local anesthetics is the elevation of intracellular Ca2+ [5]. Since myotoxicity of local anesthetics is suppressed by dantrolene and enhanced by caffeine [6], it is possible that RYR1 is involved in this process. In general, local anesthetics are safe to use in MH patients [7, 8]; however, there is insufficient evidence on myotoxicity in individuals predisposed to MH when large doses of local anesthetics are given, such as during peripheral nerve blocks. This lack of data might be due to the rarity of MH and the fact that it is, therefore, difficult to conduct clinical research in this area.
It has been reported that CICR is promoted by local anesthetics in the skeletal muscle of normal rats and guinea pigs [9, 10]. To date, no studies have assessed intracellular Ca2+ kinetics following the application of local anesthetics to human skeletal muscle cells derived from persons predisposed to MH. The skeletal muscles in these individuals may have disordered Ca2+ regulation, and may, therefore, exhibit elevated Ca2+ concentrations following lower doses of local anesthetics than in healthy individuals.
This study was performed to investigate the effect of local anesthetics on Ca2+ dynamics and myotoxicity in skeletal muscle cells derived from individuals predisposed to MH.
Methods
This study was approved by the ethics committee of Hiroshima University. Subjects were referred to our facility for advanced assessment because they or their families had MH or MH-like symptoms. We obtained each participant’s written informed consent prior to implementing the experimental research protocol described below. In addition, all personal information, including genetic information, was managed according to the regulations established by the university.
Human skeletal muscle specimens were obtained by biopsy of the quadriceps or biceps brachii muscles to determine susceptibility to MH. 22 individuals underwent muscle biopsy, and the CICR rate test was performed according to the protocol developed by Endo et al. [11, 12]. Information on the results was offered to all participants.
In brief, chemically stripped muscle fibers were obtained from biopsied muscle tissue using saponin, and fibers were treated with varying concentrations of Ca2+ (0, 0.3, 1.0, 3.0, and 10.0 µM). The tension of each specimen was measured using a force transducer, and CICR rates were measured. Acceleration of CICR rates was determined according to our previous studies [13]. The mean normal CICR values were determined from 12 individuals with negative in vitro contracture tests (IVCT; EMHG protocol) and caffeine–halothane contracture tests (CHCT; North American MH Group protocol). An accelerated CICR rate was defined by a CICR value 2 standard deviations (SD) above the mean of normal individuals, and indicated a predisposition to developing MH. Characteristics of the individuals and the results of the CICR rate test are shown in Table 1.
Preparation of myotubes
This study was performed using surplus muscle remaining after the CICR rate test. The skeletal muscle cells were maintained in Dulbecco’s modified Eagle’s medium (DMEM; Invitrogen, USA) supplemented with 10% heat-inactivated bovine calf serum (FBS; Sigma-Aldrich, USA) containing 1% ampicillin sodium salt, kanamycin sulfate (Sigma-Aldrich, USA), and amphotericin B (Invitrogen, USA), in 25-cm2 cell culture flasks (Corning; Corning, NY, USA) at 37 °C under 5% CO2. The medium was changed every 3 days. After 2 or 3 weeks in culture, the cells were collected with trypsin and plated on 35-mm glass-bottom culture dishes. They were cultivated for 7–10 days in DMEM supplemented with 10% FBS and then for 5–7 days in the same medium supplemented with 2% FBS. Myotubes were confirmed by morphological identification of fusiform-shaped multinuclear cells (Fig. 1).
Ca2+ imaging of myotubes
Myotubes were washed in Hank’s balanced salt solution (HBSS) containing 130 mM NaCl, 5.4 mM KCl, 20 mM HEPES, 2.5 mM CaCl2, 1 mM MgCl2, and 5.5 mM glucose (pH 7.4). The myotubes were loaded with 5.0 µM Fura-2 AM (Dojindo Molecular Technologies, Tokyo, Japan) in HBSS for 1 h at room temperature (24–26 °C), and then washed with HBSS. Measurements were performed after cells were incubated in HBSS for 30 min.
The cells were excited at 340 and 380 nm. Fluorescence emissions of Fura-2 AM were observed at 510 nm using a fluorescence microscope (Nikon, Tokyo, Japan) at 5-s intervals to evaluate intracellular Ca2+ changes. Images were acquired using a cooled high-speed digital video camera (ORCA-AG; Hamamatsu Photonics, Hamamatsu, Japan).
Each solution was added to one side of the culture dish and aspirated from the opposite side for 2 min at a rate of 1.2 mL/min at 37 °C, then washed out 2 min before addition of the next chemicals. Chemical-induced changes in Fura-2 AM fluorescence were measured using various chemical concentrations, and the 340/380 nm signal ratio was calculated using a Ca2+ imaging system (Aquacosmos 2.5; Hamamatsu Photonics).
Caffeine, 4-chloro-m-cresol (4-CmC)
To identify myotube characteristics, we examined their responses to caffeine and 4-CmC, both of which are pure RYR1-stimulating agents. HBSS containing 10 mM caffeine was added to the culture dish. Next, caffeine was tested incrementally at 0.25, 0.5, 1.0, 2.5, 5.0, 10, and 20 mM, and 4-CmC was tested incrementally at 3.0, 10, 30, 100, 300, 500, and 1000 µM.
Local anesthetics
Only the cells that demonstrated RYR1 expression, defined by increased Ca2+ concentrations in response to 10 mM caffeine, were used for experiments. HBSS containing incremental levels of lidocaine dissolved in dimethyl sulfoxide (DMSO, Sigma-Aldrich) (0.1, 0.25, 0.5, 1.0, 2.0, 4.0, 6.0, and 8.0 mM) was added to the dish. This measurement was performed within 90 min after washing away the excess Fura-2 AM. In the same way, levobupivacaine (0.025, 0.05, 0.1, 0.2, 0.4, 0.8, 1.5, and 2.0 mM) and ropivacaine (0.1, 0.25, 0.5, 1.0, 2.0, and 4.0 mM) were perfused and the respective changes in Fura-2 AM fluorescence were measured.
Data analysis
Changes in ratios were calculated as the difference between the maximal response and the preceding baseline. To trace dose–response curves for caffeine, 4-CmC, and each local anesthetic, the data were normalized to the maximal response of each cell. Then, the half-maximal effective concentration (EC50) was calculated from the acquired dose–response curves. All data were analyzed using PRISM 7.0 (GraphPad Software, San Diego, USA). The EC50 was measured in each cell and used as a summary measure, and we compared the EC50 value of the accelerated group with that of the unaccelerated group. Significance was tested via t test, and a p value of < 0.05 was considered to be statistically significant.
Results
Responses to caffeine and 4-CmC
In all cells, intracellular Ca2+ concentrations increased as the concentrations of loaded caffeine and 4-CmC increased. Each EC50 is shown in Table 2. The EC50s of the cells in the accelerated group were all lower than the cutoff value determined by Kobayashi et al. [14].
The EC50 values for caffeine were 3.11 ± 0.54 mM in the accelerated group and 4.85 ± 0.64 mM in the unaccelerated group (p < 0.0001). The EC50 values for 4-CmC were 144.8 ± 30.7 µM in the accelerated group and 249.8 ± 34.3 µM in the unaccelerated group (p < 0.0001) (Fig. 2).
EC50s for local anesthetics in myotubes
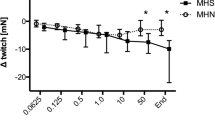
Figure 3 shows representative traces of Ca2+ responses to incremental doses of lidocaine in myotubes, and Fig. 4 shows the dose–response curves of Ca2+ release in myotubes following exposure to local anesthetics. The responses of both the accelerated and unaccelerated groups increased as the concentration of each anesthetic was increased. There were no differences in mean EC50 for lidocaine, levobupivacaine, and ropivacaine between accelerated and unaccelerated groups (Fig. 5a).
50% effective concentration (EC50) for local anesthetics (a), caffeine (b), and 4-chloro-m-cresol (4-CmC) (c) in accelerated and unaccelerated groups. There were no differences in EC50 for local anesthetics between accelerated and unaccelerated groups. EC50 for both caffeine and 4-CmC was significantly higher in unaccelerated group than accelerated group. *p < 0.0001, **p < 0.0001
In addition, the pH of each local anesthetic solution was within the range of 7.226–7.696. Ca2+ concentrations did not increase following the addition of HBSS adjusted to the same pH.
Discussion
All EC50 values of each of the three local anesthetics applied to the accelerated and unaccelerated groups were lower than the physiological concentrations, and the values were not statistically different between the groups. This indicated that the local anesthetics increase the intracellular Ca2+ concentration in MH-susceptible individuals and non-MH-susceptible individuals, but the degree of myotoxicity of local anesthetics was equivalent in individuals with and without predisposition to malignant hyperthermia. Therefore, we consider that extra caution is not warranted when using local anesthetics in MH-susceptible individuals.
Increased intracellular Ca2+ concentrations caused by local anesthetics
Regardless of the presence or absence of MH predisposition (corresponding to the accelerated and unaccelerated groups, respectively), similar increases were seen in Ca2+ concentrations following myotube treatment with each local anesthetic. These increases occurred at concentrations of 0.25 mM for lidocaine, 0.2 mM for levobupivacaine, and 0.25 mM for ropivacaine. The EC50 for levobupivacaine was the lowest, at 0.72 mM, consistent with previous reports that bupivacaine showed higher skeletal muscle toxicity than other local anesthetics [15, 16]. In general, the concentrations of local anesthetics used clinically are 0.5–2% (21–85 mM) for lidocaine, 0.25–0.75% (7.9–23 mM) for levobupivacaine, and 0.2–1% (6.6–33 mM) for ropivacaine. There have been reports of partial myotoxicity in animals following the use of local anesthetics at high concentrations or over long periods and it is considered that necrotization of skeletal muscles and the apoptosis through mitochondrial pathways are involved in [3, 17]. In humans, muscular strength decreased with prolonged administration [4]. However, skeletal muscle disorders have also often occurred during the acute phase, though these have resolved with time [18, 19], and clinically, skeletal muscle toxicity is rarely a problem in healthy persons [20]. This study showed that when local anesthetics were administered intramuscularly, Ca2+ concentrations increased locally and skeletal muscle cells were destroyed. However, since the increases in Ca2+ concentrations were not significantly different between the accelerated and unaccelerated groups, there should be no clinically meaningful difference in myotoxicity caused by local anesthetics between MH-predisposed persons and those who are healthy.
Mechanisms underlying elevated intracellular Ca2+ concentrations following administration of local anesthetics
In myotubes, the EC50 of each local anesthetic did not differ significantly between the CICR-accelerated group and those of the unaccelerated group. There are several Ca2+ regulatory mechanisms in human skeletal muscle cells. RYR1 is closely related to the l-type voltage-dependent Ca2+ channel (DHPR) on the cell membrane and regulates Ca2+ release from the sarcoplasmic reticulum [21, 22]. Previous stydies have reported that not only the RYR1 [23, 24], but also the voltage-dependent calcium channels [25] are involved in the calcium induce of local anesthetics. In myotubes, there were significant differences in the EC50s of caffeine and 4-CmC but no significant differences in the EC50s of local anesthetics between the accelerated and unaccelerated CICR groups. If local anesthetics act only on RYR1, there should be significant differences in the EC50s of local anesthetics such as caffeine and 4-CmC. Relatedly, Ca2+ inflow into skeletal muscle is mediated by store-operated channels, mechanosensitive channels, and other mechanisms [26, 27]. The elevated intracellular Ca2+ concentrations following local anesthetic administration in this study were also observed using Ca2+-free perfusate (data not shown). Therefore, while release of Ca2+ from the SR is the main cause of increased intracellular Ca2+ concentrations, it is certainly possible that the above inflow mechanisms interact with other processes outside the cell. We found that in myotubes there were no significant differences in the EC50s of local anesthetics between the accelerated and unaccelerated CICR groups, probably because the mechanism whereby local anesthetics raise intracellular Ca2+ levels involves not only RYR1 but also various Ca2+ regulatory processes. Further investigations are required.
Characteristics of myotubes
The diagnosis of MH takes into account several factors: clinical findings; genetic testing; muscle biopsy; and functional testing, specifically the caffeine–halothane contracture test in North America and the in vitro contracture test in Europe [28, 29]. In Japan, MH susceptibility is diagnosed based on the fact that CICR rates vary by Ca2+ concentrations. After muscles are chemically stripped with saponin, the CICR test can specifically detect SR abnormalities, eliminating other mechanisms related to the onset of MH, such as excitation–contraction coupling or Ca2+ homeostasis mediated by other Ca2+ transporters. The caffeine–halothane contracture test and the in vitro contracture test are based on the contracture of intact muscle fibers in the presence of halothane or caffeine as the RYR1 activator. Compared to the CICR test, which indicates only abnormalities in the SR, the caffeine–halothane contracture test /the in vitro contracture test can detect various abnormalities such as those of DHPR in the skeletal muscle. The results of the CICR rate test and the caffeine–halothane contracture test /the in vitro contracture test are not necessarily identical [13]; therefore, whether the CICR rate test can accurately assess MH predisposition remains a matter of debate. Therefore, we performed additional functional analysis using myotubes. Functional tests using myotubes can evaluate overall Ca2+ homeostasis in muscle cells, and the results were shown to correlate with those of the in vitro contracture test [30]. Our previous study demonstrated a good correlation between the CICR test and the response to RYR1 activators in human cultured myotubes [14]. Susceptibility to RYR1 agonists (caffeine and 4-CmC) was confirmed in myotubes, and all cells in the accelerated CICR group in this study had low RYR1 agonist EC50 values. This indicates that all cells in the accelerated CICR group in this study were predisposed to MH.
Limitations
The limitations of this study include its small sample size. As MH is a rare disease, few individuals underwent muscle biopsy during the study period. Various gene mutations have been reported in MH, and the muscle cells used in this study are not representative of all cases of MH. Also, some cells that demonstrated CICR acceleration was derived from individuals without apparent MH. Furthermore, whether the CICR rate test can accurately assess MH predisposition remains a matter of debate. Susceptibility to RYR1 agonists (caffeine and 4-CmC) was confirmed in myotubes, and all cells in the accelerated CICR group in this study had low RYR1 agonist EC50 values.
We used local anesthetics at lower concentrations than those used clinically. This is because the myotubes entered apoptosis when loaded with local anesthetics above the concentrations used in this study. These concentrations were considered to be the upper limits for conducting experiments with myotubes. Despite these limitations, this study showed that cells from individuals with or without MH predisposition exhibited no significant difference in fluctuations of intracellular Ca2+ dynamics caused by local anesthetics.
As MH is rare and difficult to investigate clinically, we conducted this experiment using skeletal muscle specimens from MH-susceptible individuals. We conclude that the myotoxicity of local anesthetics is equivalent in individuals with and without predisposition to MH.
References
Halsall PJ, Ellis FR. Malignant hyperthermia. Anaesth Intensive Care. 2005;14:192–4.
Schneiderbanger D, Johannsen S, Roewer N, Schuster F. Management of malignant hyperthermia: diagnosis and treatment. Ther Clin Risk Manag. 2014;10:355–62.
Zink W, Bohl JRE, Hacke N, Sinner B, Martin E, Graf BM. The long term myotoxic effects of bupivacaine and ropivacaine after continuous peripheral nerve blocks. Anesth Analg. 2005;101:548–54.
Neal JM, Salinas FV, Choi DS. Local anesthetic-induced myotoxicity after continuous adductor canal block. Reg Anesth Pain Med. 2016;41:723–7.
Benoit PW, Yagiela A, Fort NF. Pharmacologic correlation between local anesthetic-induced myotoxicity and disturbances of intracellular calcium distribution. Toxicol Appl Pharmacol. 1980;52:187–98.
Plank C, Hofmann P, Gruber M, Bollwein G, Graf BM, Zink W, et al. Modification of bupivacaine-induced myotoxicity with dantrolene and caffeine in vitro. Anesth Analg. 2016;122:418–23.
Harrison GG, Morrell DF. Response of mhs swine to i.v. infusion of lignocaine and bupivacaine. Br J Anaesth. 1980;52:385–7.
Wingard DW, Bobko S. Failure of lidocaine to trigger porcine malignant hyperthermia. Anesth Analg. 1979;58:99–103.
Ibarra MCA, Ichihara Y, Hikita M, Yoshida K, Junji S, Maehara Y, et al. Effect of bupivacaine enantiomers on Ca2+ release from sarcoplasmic reticulum in skeletal muscle. Eur J Pharmacol. 2005;512:77–83.
Maemura Y. Effect of ropivacaine on Ca function of skinned skeletal muscle. Masui. 2002;51:19–24.
Endo M, Iino M. Measurement of Ca2 + release in skinned fibers from skeletal muscle. Methods Enzymol. 1988;157:12–26.
Ohta T, Endo M, Nakano T, Morohoshi Y, Wanikawa K, Ohga A. Ca-induced Ca release in malignant hyperthermia-susceptible pig skeletal muscle. Am J Physiol. 1989;256:C358–67.
Oku S, Mukaida K, Nosaka S, Sai Y, Maehara Y, Yuge O. Comparison of the in vitro caffeine-halothane contracture test with the Ca-induced Ca release rate test in patients suspected of having malignant hyperthermia susceptibility. J Anesth. 2000;14:6–13.
Kobayashi M, Mukaida K, Migita T, Hamada H, Kawamoto M, Yuge O. Analysis of human cultured myotubes responses mediated by ryanodine receptor 1. Anaesth Intensive Care. 2011;39:252–61.
Hofmann P, Metterlein T, Bollwein G, Gruber M, Plank C, Graf BM, et al. The myotoxic effect of bupivacaine and ropivacaine on myotubes in primary mouse cell culture and an immortalized cell line. Anesth Analg. 2013;117:634–40.
Zink W, Seif C, Bohl JRE, Hacke N, Braun PM, Sinner B, et al. The acute myotoxic effects of bupivacaine and ropivacaine after continuous peripheral nerve blockades. Anesth Analg. 2003;97:1173–9 (table of contents).
Zhang C, Phamonvaechavan P, Rajan A, Poon DY, Topcu-Yilmaz P, Guyton DL. Concentration-dependent bupivacaine myotoxicity in rabbit extraocular muscle. J AAPOS. 2010;14:323–7.
Benoit PW, Belt WD. Destruction and regeneration of skeletal muscle after treatment with a local anaesthetic, bupivacaine (Marcaine). J Anat. 1970;107:547–56.
McLoon LK, Nguyen LT, Wirtschafter J. Time course of the regenerative response in bupivacaine injured orbicularis oculi muscle. Cell Tissue Res. 1998;294:439–47.
Zink W, Graf BM. Local anesthetic myotoxicity. Reg Anesth Pain Med.;29:333–40.
Melzer W, Herrmann-Frank A, Lüttgau HC. The role of Ca2+ ions in excitation-contraction coupling of skeletal muscle fibres. Biochim Biophys Acta. 1995;1241:59–116.
Schiemann AH, Stowell KM. Comparison of pathogenicity prediction tools on missense variants in RYR1 and CACNA1S associated with malignant hyperthermia. Br J Anaesth. 2016;117:124–8.
Shoshan-Barmatz V, Zchut S. The interaction of local anesthetics with the ryanodine receptor of the sarcoplasmic reticulum. J Membr Biol. 1993;133:171–81.
Hyvelin JM, Martin C, Roux E, Marthan R, Savineau JP. Human isolated bronchial smooth muscle contains functional ryanodine/caffeine-sensitive Ca-release channels. Am J Respir Crit Care Med. 2000;162:687–94.
Gordienko DV, Harhun MI, Kustov MV, Pucovský V, Bolton TB. Sub-plasmalemmal [Ca2+]i upstroke in myocytes of the guinea-pig small intestine evoked by muscarinic stimulation: IP3R-mediated Ca2+ release induced by voltage-gated Ca2+ entry. Cell Calcium. 2008;43:122–41.
Prakriya M, Lewis RS. Store-operated calcium channels. Physiol Rev. 2015;95:1383–436.
Franco-Obregón A, Lansman JB. Changes in mechanosensitive channel gating following mechanical stimulation in skeletal muscle myotubes from the mdx mouse. J Physiol. 2002;539:391–407.
Riazi S, Kraeva N, Muldoon SM, Dowling J, Ho C, Petre M-A, et al. Malignant hyperthermia and the clinical significance of type-1 ryanodine receptor gene (RYR1) variants: proceedings of the 2013 MHAUS Scientific Conference. Can J Anesth. 2014;61:1040–9.
Hopkins PM, Rüffert H, Snoeck MM, Girard T, Glahn KPE, Ellis FR, et al. European Malignant Hyperthermia Group guidelines for investigation of malignant hyperthermia susceptibility. Br J Anaesth. 2015;115:531–9.
Wehner M, Rueffert H, Koenig F, Meinecke CD, Olthoff D. The Ile2453Thr mutation in the ryanodine receptor gene 1 is associated with facilitated calcium release from sarcoplasmic reticulum by 4-chloro-m-cresol in human myotubes. Cell Calcium. 2003;34:163–8.
Acknowledgements
A Grant-in-Aid (Grant Number 16K20100) for Scientific Research from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
About this article
Cite this article
Otsuki, S., Yasuda, T., Mukaida, K. et al. Myotoxicity of local anesthetics is equivalent in individuals with and without predisposition to malignant hyperthermia. J Anesth 32, 616–623 (2018). https://doi.org/10.1007/s00540-018-2526-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-018-2526-4