Abstract
Purpose
A multimodal analgesic approach is necessary for post-thoracotomy pain, which can be severe. Intravenous access, central and peripheral nerve blocks are frequently used. The aim of this study was to evaluate the efficacy of serratus anterior plane block (SAPB) in the management of post-thoracotomy pain.
Methods
A total of 40 patients who underwent thoracotomy between January 2014 and January 2016 were retrospectively analyzed. The patients were divided into two groups: Group M (intravenous patient-controlled analgesia morphine; n = 20) and Group S (intravenous patient-controlled analgesia morphine + SAPB; n = 20). The Visual Analogue Scale (VAS) was used for pain evaluation at the 1st, 2nd, 4th, 6th, 8th, 12th and 24th postoperative hours and morphine consumption was evaluated at the 6th, 12th and 24th postoperative hours. Secondary outcomes were additional analgesic requirement, side effects, the Ramsay Sedation Scale (RSS) scores, block onset time and block level.
Results
The VAS scores and the amount of morphine consumed at the 6th, 12th and 24th hours were found to be significantly lower in Group S than in Group M (P < 0.001). No statistically significant difference was found in the rate of side effects, including nausea, vomiting, pruritus, respiratory depression, bradycardia and hypotension, and RSS outcomes between the groups.
Conclusion
Our study suggests that SAPB is an effective adjuvant treatment option for thoracotomy analgesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thoracotomy, which is used for the exploration of the thoracic cavity and for the management of pulmonary, mediastinal, diaphragmatic and esophageal pathologies, can be performed posterolaterally, anterolaterally or anteriorly. Pain following thoracotomy may result in hypoxemia, depending on the altered mechanical functions of the lungs and ventilation–perfusion mismatch [1, 2]. The main causes of postoperative pain during the early period include intercostal muscle and soft tissue damages and rib fractures [3]. Intravenous (IV) drugs such as opioids, non-steroidal anti-inflammatory drugs (NSAIDs), local anesthetic injections to the wound site and regional anesthetic techniques are used to relieve thoracotomy pain. Currently, opioids (morphine, fentanyl etc.) and drugs used as adjuvant agents (ketamine and dexmedetomidine), are administered using the IV route [3,4,5,6,7]. Among different regional anesthetics, thoracic epidural block, paravertebral block, intercostal block and intra/extrapleural block are frequently used [3]. However, symptoms such as respiratory depression, sedation and pruritus caused by increased doses of opioids, and the possibility of transient or permanent nerve damage following neuraxial block, have directed clinicians to investigate alternative methods and drugs [7,8,9,10,11]. At the present time, the increased use of ultrasonography (USG) in nerve blocks has enabled the application of different plane blocks in regional anesthesia [12, 13]. Serratus anterior plane block (SAPB), which may be a suitable approach for analgesia in thoracic surgery, is one of the recent plane blocks which can provide analgesia between the thoracic 2 (T2) and thoracic 9 (T9) levels and which can be performed under ultrasonography guidance [14]. The blockade of cutaneous branches of intercostal muscles in T2–T9 dermatomes can be achieved with this block, and can be performed in two different ways, either to the region between the serratus anterior muscle and intercostal muscle, or to the region above the serratus muscle [14]. A sensorial blockade for approximately 12 h can be achieved using SAPB which, in addition to thoracic surgery, is also used for postoperative analgesia following breast surgery [15].
In the present study, we aimed to evaluate the effect of SAPB, which is used for posterolateral thoracotomy analgesia in addition to IV patient-controlled analgesia (PCA) with morphine, on the amount of morphine consumption and the Visual Analogue Scale (VAS) scores.
Patients and methods
Patient selection
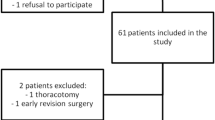
The study protocol was approved by the local Ethics Committee (decision number 2011-KAEK-25 2016/08-01). The study was conducted in accordance with the principles of the Declaration of Helsinki. As soon as the local ethics committee gave approval, the patient files were reviewed.A total of 83 patients who underwent thoracotomy between January 2014 and January 2016 were retrospectively analyzed. Patients who were deemed eligible to participate in the study were called to the hospital for a written informed consent form. A written informed consent was obtained from each patient who was included the study. Patients aged between 18 and 65 years, those who were in the American Society of Anesthesiologists (ASA) I–III class and underwent thoracotomy and those with prior standard surgical procedures by a single surgical team without any complications were evaluated within the scope of the study. Exclusion criteria were as follows: previous history of opioid use preoperatively, repeat surgery, additional imaging studies and other procedures requiring mobilization (which can alter VAS scores), allergy to local anesthetics, urgent surgery, the presence of any systemic infection, or pregnancy. Forty-three patients were excluded from the study. A total of 40 patients were divided into two groups: Group M (IV PCA morphine; n = 20) and Group S (IV PCA morphine + SAPB; n = 20) (Fig. 1).
Anesthetic management
Following premedication with IV midazolam (0.03 mg/kg), all patients were monitored in the operating room for non-invasive blood pressure, electrocardiography (ECG), heart rate (HR) and peripheral oxygen saturation (SpO2). Before induction, intravenous infusion of NaCl 0.9% was initiated and pre-oxygenation with oxygen 100% was performed for 3 min. Propofol 2–2.5 mg/kg and rocuronium bromide 0.6 mg/kg were administered IV during induction. The patients were intubated with a double-lumen endotracheal tube in appropriate sizes (35–37 French), and mechanical ventilation was performed to achieve end-tidal CO2 (ETCO2) of 30–35 mmHg. During maintenance of general anesthesia, sevoflurane at a concentration of 1–2.5% was administered in a 50% O2–50% air mixture at a flow rate of 3 L/min. Additional analgesia was met by administering fentanyl at 1 μg/kg. Twenty minutes before the end of the operation, morphine infusion with IV PCA (APM II Ambulatory Pump, Abbott Laboratories, San Diego, CA, USA) was initiated and SAPB under USG guidance was then performed. Following recurarization, patients were extubated and were followed in the post-anesthetic care unit (PACU). O2 support with a mask at a rate of 0.2–0.4 L/min was given for 24 h during the PACU stay.
Pain management
Group M (IV PCA morphine): for the morphine group, the solution was prepared at a concentration of 0.5 mg/mL, following a loading dose of 5 mg. The device was programmed to 0.5 mg/h of baseline infusion rate, 0.5 mg of bolus dose, 20 min of locking time, and 18 mg of maximum dose for 4 h.
Group S (IV PCA morphine and SAPB): for the SAPB group, in addition to the IV PCA morphine protocol used in the morphine group, SAPB was applied. It was performed at the end of the operation following the skin closure in the supine position, while the patient’s arm was above the head. After proper site cleaning, the first and second ribs were identified with a linear probe in the midclavicular line. The USG probe was advanced caudally in the sagittal plane, and the fourth and fifth ribs were visualized. The USG probe was then directed posteriorly and the serratus, latissimus dorsi and intercostal muscles were visualized. Bupivacaine 0.25% 20 mL was administered to the lower plane of the serratus muscle, using a 22-gauge 100-mm visible peripheral nerve block needle under the guidance of USG through the in-line technique. In the case of a VAS score of >5, an additional analgesic need was fulfilled using paracetamol 1 g IV at a maximum dose of three times every 8 h in both groups.
Outcome measures
Primary measures
The VAS score at the 1st, 2nd, 4th, 6th, 8th, 12th and 24th postoperative hours and the amount of morphine consumption at the 6th, 12th and 24th postoperative hours were examined.
Secondary measures
Side effects, including nausea and vomiting, pruritus, respiratory depression, bradycardia and hypotension, additional analgesic requirement, intraoperative opioid requirement, and the Ramsay Sedation Scale (RSS) scores were evaluated. The recorded time and level of blockade as confirmed with the pinprick test (from midaxillary) were also assessed at 30-min intervals.
The sedation level was evaluated using the RSS: (1) anxiety, agitation are present; (2) cooperated, awake; (3) sedated, responds to commands; (4) sleepy, immediately woken by auditory stimulus or glabella tap; (5) sleepy, deep response to auditory stimulus or glabella tap and (6) sleepy, no response to auditory stimulus or glabella tap. A RSS score of ≥5 was accepted as over-sedation and the locking time in PCA was prolonged to 40 min. Complaints of nausea and vomiting were assessed using the Nausea–Vomiting Scale (NVS): (1) no nausea is present, (2) mild nausea is present, (3) severe nausea is present, (4) vomiting is present. In the case of a NVS score of >3, an anti-emetic drug was administered. Hypotension was defined as a mean arterial blood pressure of <60 mmHg.
Statistical analysis
Statistical analysis was performed using IBM SPSS version 22.0 software (SPSS Inc., Chicago, IL, USA). Descriptive data were expressed as frequency, percentage, mean and standard deviation, and min–max values. The chi-squared test (χ 2) was used to compare qualitative data. Normal distribution of data was assessed with the Shapiro–Wilk test. The Mann–Whitney U test was used for inter-group comparisons, while the Friedman test was used to compare data between measurement intervals for intragroup analysis. Values with a probability lower than α = 0.05 were accepted as an indicator of significant differences between the groups, while values higher than α = 0.05 were accepted as an indicator of no significant differences between the groups. A p value of p = 0.05 was considered statistically significant.
Results
In the study population, 22 were males and 18 were females. The mean age was 58.4 ± 9.6 (range 18–65) years. There was no significant difference in the age and sex of the patients, surgical site and duration of surgery between the groups (Table 1). In the intragroup analysis, the VAS scores at the 2nd, 4th, 6th, 8th, 12th and 24th hours were found to be significantly lower than the scores measured at the 1st hour in both groups (p < 0.05) (Table 2). However, the VAS scores were significantly lower in Group S than Group M (p < 0.05). The amounts of PCA morphine consumption at the 6th, 12th and 24th postoperative hours were also found to be significantly lower in Group S (Table 3). There was no statistically significant difference in the frequency of side effects between the groups (p > 0.05) (Table 4).
Furthermore, seven patients in Group S and five patients in Group M needed paracetamol as rescue analgesia. However, the difference did not reach statistical significance (p > 0.05) (Table 4). The level and duration of sensorial blockade in Group S are presented in Table 5.
Discussion
In the present study, we aimed to evaluate the efficacy of IV PCA + SAPB in the management of post-thoracotomy pain. We found that the amount of morphine consumption and VAS scores were lower in the SAPB + morphine infusion group than in the morphine alone group. The intravenous route, which is the most frequently used route for the palliation of pain following thoracotomy, is one of the basic approaches necessary for multimodal analgesia. Opioids alone, or as a part of a multimodal approach, are used in the treatment [4, 6, 15,16,17]. The main disadvantages of opioid use in incremental doses include side effects, such as respiratory depression, pruritus, sedation and nausea or vomiting [5]. In the present study, in which morphine consumption was consistent with the literature data, although morphine consumption in the morphine infusion alone group was higher than the SAPB group, the difference in the frequency of side effects, such as nausea, vomiting, bradycardia and hypotension, did not reach statistical significance between the groups.
Of these alternative methods, regional anesthesia techniques are currently frequently used alone or as a part of multimodal analgesia [9,10,11]. Similar to the intravenous use of opioids, complications and side effects may be also observed during regional anesthesia [3, 17]. Total spinal block, pneumothorax and neuronal injury are the major complications which may be seen following paravertebral block [17]. In addition, side effects such as hypotension, neuraxial hematoma, vomiting and urinary retention following thoracic epidural injection have been reported in the literature [18]. Due to these side effects and complications, alternative methods and drug regimens for palliation of thoracotomy pain are still the subject of research for authors. Considering easier application and lower complication rates, we used USG-guided SAPB to manage posterolateral thoracotomy pain in the present study. Blanco et al. administered a local anesthetic and contrast agent under USG guidance into two regions, the superficial and deep parts of the serratus anterior muscle, in four volunteers [14]. With this block, which was defined as SAPB, they used a mixture of levobupivacaine 0.125% at a dose of 0.4 mL/kg and gadolinium (contrast agent). In superficial SAPB, where the mixture was administered between the serratus anterior muscle and the latissimus dorsi muscle, they detected a sensorial block of 752 min in the intercostal nerves. In deep SAPB, where the mixture was administered between the serratus anterior muscle and the intercostal muscle, they detected a sensorial block of 386 min in the intercostal nerves. They found the analgesia levels in the two methods to be T2 and T9, respectively. On the other hand, literature data related to the recently defined SAPB is limited. In two cases in the literature, SAPB was used for thoracic analgesia, and in three cases following breast surgery for the management of acute and chronic pain [15, 19,20,21,22,23]. In one study, in which the block was used for chronic pain following breast surgery, Takimoto et al. injected 10 mL of lidocaine 1% beneath the serratus anterior muscle and achieved a decrease in VAS scores from 10 to 6. They reported successful results following this block, which was applied eight times within 6 months [15]. However, in the other case report, they used 30 mL of ropivacaine 0.375% during the SAPB block for breast surgery. After a successful block in an obese patient, they reported that this could be an alternative treatment method in patients in whom it was difficult to perform a central block [19]. Furthermore, in three case reports in the literature where SAPB was used for thoracic analgesia, López-Matamala et al. performed SAPB in patients who were followed under mechanical ventilation in the intensive care unit and when weaning was complicated. They reported that weaning was successful following the infusion of levobupivacaine 0.625% to the inferior plane of the serratus anterior muscle [20]. Kunhabdulla et al. performed SAPB with 20 mL of levobupivacaine at a concentration of 0.125% and achieved pain palliation in patients with rib fractures using levobupivacaine 0.625% at a dose of 7–12 mL/h [21]. They concluded that SAPB was suitable for obese patients, as thoracic epidural anesthesia poses some risks, and it might become necessary to repeat an intercostal block in obese patients [21]. In another case report the authors achieved a decrease in VAS scores using SAPB at the 3rd postoperative day following anterior thoracotomy operation for esophageal surgery [22]. The authors reported that this technique was successful. Ohgoshi et al. injected 30 mL of ropivacaine 0.375–0.5% between the serratus muscle and external intercostal muscles in 20 patients following breast surgery in the so-called serratus–intercostal plane block. They reported that this block was effective in all patients except those undergoing axillary dissection, as it does not provide analgesia at the T1 level [23]. In previous studies, the level of block achieved by SAPB was, as described by Blanco et al., found to be at the T2 level in the cranial direction [14]. However, a block was unable to be achieved in the caudal direction at levels lower than T6 [19, 23]. In two different studies in which similar results were obtained, Daga et al. found that the distribution obtained after administering an air + saline mixture beneath the serratus muscle in seven cadavers could be between the second and fourth intercostal spaces [24]. However, in another cadaver study, the distribution was limited to between T2 and T6 following the administration of methylene blue [25]. In the present study, following the blockade using 20 mL of medication, the sensorial block was at the T2 level in the cranial direction, whereas it was in the caudal spread at the T8 level in two patients and at the T9 level in one patient. The aforementioned different levels of block described by Blanco et al. might have resulted from the fact that the contrast material they used changed the spread of the drug. In the present study, although there was a difference in the block level following local anesthetic administration between the serratus anterior and external intercostal muscles, the sensorial block of 388 ± 38.6 min was consistent with the literature findings [19,20,21,22].
Nonetheless, although SAPB seems to be an effective method for pain management following thoracotomy and breast surgery, there are still controversial issues in its applicability and efficacy. Some of these issues are as follows: SAPB may interfere with the integrity of the serratus muscle and facial plane may be disturbed at the surgical incision site and alter the drug distribution. This can explain the different block levels reported in the literature. The patients on whom Blanco et al. performed this block were healthy, and this could be an explanatory reason for the spread over a large area. Another important issue is the determination of the effective dose. Whether similar effects can be obtained after the administration of 30 mL, 10 mL or infusion remainsto be elucidated [19,20,21].
There are some limitations to this study: first, the small sample size and retrospective design of the study. Second, although block with 20 mL of bupivacaine 0.25% produced successful results for thoracotomy pain in the present study, further large-scale, prospective, randomized controlled studies are needed to confirm the efficacy of SAPB.
Conclusion
In conclusion, the results of the present study suggest that SAPB is an effective adjuvant treatment option for thoracotomy analgesia. Compared to the current methods used for thoracotomy pain which require multimodal analgesia, SAPB has some merits including its ease of use and low potential for side effects.
References
Kavanagh BP, Katz J, Sandler AN. Pain control after thoracic surgery. A review of current techniques. Anesthesiology. 1994;81:737–59.
Doan LV, Augustus J, Androphy R, Schechter D, Gharibo C. Mitigating the impact of acute and chronic post-thoracotomy pain. Review articles. Cardiothorac Vasc Anesth. 2014;28:1060–8.
Slinger PD, Campos JH. Anesthesia for thoracic surgery. In: Miller RD, editor. Miller’s anesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2015. p. 1942–2006.
Fiorelli A, Mazzella A, Passavanti B, Sansone P, Chiodini P, Iannotti M, Aurilio C, Santinİ M. Is pre-emptive administration of ketamine a significant adjunction to intravenous morphine analgesia for controlling postoperative pain? A randomized, double-blind, placebo-controlled clinical trial. Interact Cardiovasc Thorac Surg. 2015;21:284–91.
Michelet P, Guervilly C, Hélaine A, Avaro JP, Blayac D, Gaillat F, Dantin T, Thomas P, Kerbaul F. Adding ketamine to morphine for patient controlled analgesia after thoracic surgery: influence on morphine consumption, respiratory function, and nocturnal desaturation. Br J Anaesth. 2007;99(3):396–403.
Turktan M, Unlugenc H, Gulec E, Gezer S, Isik G. Coadministration of intravenous remifentanil and morphine for post-thoracotomy pain: comparison with intravenous morphine alone. J Cardiothorac Vasc Anesth. 2015;29(1):133–8.
Demirhan A, Gül R, Ganidağlı S, Koruk S, Mızrak A, Şanlı M, Oner U. Combination of dexmedetomidine and tramadol in the treatment of pain after thoracotomy. GKDA Derg. 2011;17:34–41.
Freynet A, Falcoz PE. Is transcutaneous electrical nerve stimulation effective in relieving postoperative pain after thoracotomy? Interact Cardiovasc Thorac Surg. 2010;10:283–8.
Debreceni G, Molnar Z, Szelig L, Molnar TF. Continuous epidural or intercostal analgesia following thoracotomy: a prospective randomized double-blind clinical trial. Acta Anaesthesiol Scand. 2003;47:1091–5.
Schnieder RF, Villamena PC, Harvey J, Surick BG, Surick IW, Beattie EJ. Lack of efficacy of intrapleural bupivacaine for postoperative analgesia following thoracotomy. Chest. 1993;103:414–6.
Mohammad W, Mir SA, Mohammad K, Sofi K. A randomized double blind study to evaluate efficacy and safety of epidural magnesium sulfate and clonidine as adjuvants to bupivacaine for postthoracotomy pain relief. Anesth Essays Res. 2015;9(1):15–20.
Blanco R. The ‘Pecs block’: a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011;66:847–8.
Hebbard P, Fujiwara Y, Shibata Y, Royse C. Ultra-sound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35:616–7.
Blanco R, Parras T, McDonnell JG, Prats- Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68:1107–13.
Takimoto K, Nishijima K, Ono M. Serratus plane block for persistent pain after partial mastectomy and axillary node dissection. Pain Physician. 2016;19(3):E481–6.
Zhou Y, Huang JX, Lu XH, Zhang YF, Zhang W. Patient-controlled intravenous analgesia for non-small cell lung cancer patient after thoracotomy. J Cancer Res Ther. 2015;11(Suppl 1):C128–30.
Lönqvist PA, McKenzie J, Soni AK, Conacher AD. Paravertebral blockade: failure rate and complications. Anesthesia. 1995;50:813–5.
Gulbahar G, Kocer B, Muratli SN, Yildirim E, Gulbahar O, Dural K, Sakinci U. A comparison of epidural and paravertebral catheterisation techniques in post-thoracotomy pain management. Eur J Cardiothorac Surg. 2010;37(2):467–72.
Bhoi D, Pushparajan HK, Talawar P, Kumar A, Baidya DK. Serratus anterior plane block for breast surgery in a morbidly obese patient. J Clin Anesth. 2016;33:500–1.
López-Matamala B, Fajardo M, Estébanez-Montiel B, Blancas R, Alfaro P, Chana M. A new thoracic interfascial plane block as anesthesia for difficult weaning due to ribcage pain in critically ill patients. Med Intensiva. 2014;38(7):463–5.
Kunhabdulla NP, Agarwal A, Gaur A, Gautam SK, Gupta R, Agarwal A. Serratus anterior plane block for multiple rib fractures. Pain Physician. 2014;17(5):E651–3.
Madabushi R, Tewari S, Gautam SK, Agarwal A, Agarwal A. Serratus anterior plane block: a new analgesic technique for post-thoracotomy pain. Pain Physician. 2015;18(3):E421–4.
Ohgoshi Y, Yokozuka M, Terajima K. Serratus-intercostal plane block for breast surgery. Masui. 2015;64(6):610–4.
Daga V, Narayanan MK, Dedhia JD, Gaur P, Crick H, Gaur A. Cadaveric feasibility study on the use of ultrasound contrast to assess spread of injectate in the serratus anterior muscle plane. Saudi J Anaesth. 2016;10(2):198–201.
Diéguez P, Fajardo M, López S, Alfaro P. BRILMA methylene blue in cadavers. Anatomical dissection. Rev Esp Anestesiol Reanim. 2016;63(5):307–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
About this article
Cite this article
Ökmen, K., Ökmen, B.M. The efficacy of serratus anterior plane block in analgesia for thoracotomy: a retrospective study. J Anesth 31, 579–585 (2017). https://doi.org/10.1007/s00540-017-2364-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-017-2364-9