Abstract
Purpose
Central venous catheter placement is useful but is associated with complications. Inadvertent subclavian artery (SCA) puncture is a rare complication associated with internal jugular vein (IJV) catheterization. We determined the position of the SCA by ultrasonography, and propose a needle-insertion position for avoiding inadvertent SCA puncture.
Methods
We positioned an ultrasound probe at an angle of 60° to the skin to mimic a puncture needle halfway between the clavicle and the angle of the mandible (center) and moved the probe parallel to the right IJV (RIJV) toward the clavicle until locating the SCA. We measured the distance from the clavicle to the probe 60 and from the probe to the SCA (P60–SCA) where the SCA was visible by ultrasonography.
Results
For 50 volunteers with a mean age of 27.3 years, the center position was, on average, 67 mm from the clavicle. The image of the SCA appeared within 65 mm of the clavicle. P60–SCA differed significantly between men and women (p = 0.0058). For 45 volunteers, P60–SCA was <25 mm with the probe 65 mm from the clavicle on the skin. RIJVP–SCA averaged 4.4 mm. Only P60–SCA correlated well with BMI for men (r = 0.732, p = 0.0068).
Conclusion
Puncturing the RIJV away from the center should avoid SCA puncture; puncturing it while approaching the clavicle is more dangerous. The exact location of the SCA varies from person to person; thus, confirming SCA position by ultrasonography is recommended every time before puncturing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Central venous catheter (CVC) placement is an essential aspect of anesthetic management but is associated with complications. Several case reports [1–7] have been published on inadvertent subclavian artery (SCA) injury during right internal jugular vein (RIJV) catheterization (Table 1). Although anatomical relationships between the RIJV and the SCA are described in textbooks, the position of the SCA during IJV catheterization is not well recognized. In this study we performed a detailed evaluation of the position of the SCA in relation to the clavicle and the RIJV by use of ultrasonography, and propose an appropriate position for avoiding inadvertent SCA puncture during adult RIJV catheterization.
Methods
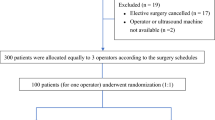
Our hospital’s ethics committee approved this study (approval number 163), and written informed consent was obtained from all volunteers by medical staff in our hospital. We enrolled 50 volunteers from September 2011 to May 2015. For measurements, volunteers were placed in a flat, supine position with the neck maximally extended and the head turned 15°–30° to the left. Initially, we measured the distance from the edge of the clavicle (C) to the angle of the mandible (M) (C–M) (bird’s-eye view, Fig. 1). We then positioned ultrasound instrument equipped with an L10-5 MHz probe (TiTAN®; Fujifilm SonoSite, Tokyo, Japan) at an angle of 60° to the skin, halfway between the C and M to observe the RIJV. To identify an optimum site for observation of the RIJV, we used the “sweep” technique, which enabled us to assess vessel size and obstacles along the vessel length. With the “sweep” technique, we maintained the probe at a 60° angle and moved it caudally along the RIJV, confirming that the RIJV stayed in the center of the image, until locating the edge of the SCA (lateral view, Fig. 2). We determined the minimum cross-sectional area of the RIJV and visualized the SCA. When the probe was directed laterally above the neck, we were unable to obtain an optimum image of the RIJV and the SCA (Fig. 3), which could have led to an inaccurate determination of distance between the RIJV and SCA, as shown in Fig. 1.
Schematic representation of the anatomic relationships among the common carotid artery (CCA), right internal jugular vein (RIJV), subclavian artery (SCA), subclavian vein (SCV), and the center of C–M (midway between the clavicle and the angle of the mandible) on the right side. The arrows indicate the distance from the probe to the SCA
Schematic representation of the distances relative to the subclavian artery (SCA) position. A probe angled at 60° is placed on the skin to locate the right internal jugular vein (RIJV) and the SCA simultaneously. The center of C–M is midway between the clavicle and the angle of the mandible. P60 is the point where the SCA is visible by ultrasonography. vSCA is the point where the vertical line from the SCA crosses the skin. The distance from the clavicle to vSCA is C–vSCA. The distance from P60 to the SCA is P60–SCA. The distance from the clavicle to P60 is C–P60, and the distance from the nearest edge of the posterior wall of the RIJV to the SCA is RIJVP–SCA. The distance from edge of the clavicle to the angle of the mandible is C–M
We defined the center portion of the probe where the SCA was visible as P60 (Figs. 2, 3) and the point where the vertical line from the SCA crossed the skin as vSCA. We directly measured the distance from the clavicle to P60 (C–P60) on the skin (Fig. 2), the distance from P60 to the SCA (P60–SCA), and the distance from the nearest edge of the posterior wall of the RIJV (RIJVP) to the SCA (RIJVP–SCA) ultrasonographically (Fig. 3). The center of C–M was indirectly calculated as (C–M)/2. The distance from the clavicle to the vSCA (C–vSCA) was calculated as C–P60 − (P60–SCA)/2. The SCA depth was calculated as (P60–SCA) × \(\sqrt 3\)/2 (Fig. 2).
Values are presented as mean ± standard deviation. GraphPad Prism® version 4.0 was used for statistical analysis. Age, height, weight, body mass index (BMI), C–M, C–P60, C–vSCA, P60–SCA, and SCA depth were compared between men and women by use of the Mann–Whitney U test. We used the Pearson’s correlation coefficient to determine the relationships between BMI or height and C–M, C–P60, P60–SCA, and RIJVP–SCA. p values less than 0.05 were considered significant.
Results
The 50 adult volunteers aged 27.3 ± 4.7 years were 161.8 ± 8.4 cm tall and weighed 52.9 ± 8.9 kg. The center of the neck was 67 ± 7.4 mm from the clavicle (Table 2). The image of the SCA began to appear only after moving the probe from the center to the furthest position 65 mm from the clavicle. P60–SCA differed significantly between men and women (p = 0.0058). For 45 (90 %) of the 50 volunteers, P60–SCA was <25 mm with the probe 65 mm from the clavicle on the skin. RIJVP–SCA was 4.4 ± 2.3 mm. Only P60–SCA (SCA depth) correlated well with BMI for men (r = 0.732, p = 0.0068, Table 3). The distribution of the SCA position related to the clavicle and the RIJV is presented in Fig. 4.
Schematic representation of the position of the subclavian artery (SCA) relative to the clavicle and the right internal jugular vein (RIJV). Representation of all 50 plots of SCA position: circles 12 males, filled rectangles, 38 females. The mean distance from the probe to the SCA (P60–SCA), the mean SCA depth, the mean distance from the clavicle to the center of C–M (midway between the clavicle and the angle of the mandible), and the mean distance from the clavicle to the probe where the SCA was visible (C–P60) were 20.8, 18.1, 67.0, and 38.0 mm, respectively
Discussion
In this study, we used ultrasonography to examine the detailed position of the SCA in relation to the clavicle and the RIJV, for volunteers, to ascertain the best position for puncturing the RIJV to avoid inadvertent SCA puncture.
Several sizes of angiocatheter (catheter-over-needle devices) or needles are commercially available for catheterization. Needle lengths are 25 mm × 22-gauge; 25, 30, or 48 mm × 20-gauge; and 30 or 48 mm × 18-gauge (BD Insyte®, Nippon Beckton–Dickinson, Tokyo, Japan); plastic catheters are 59 mm × 20-gauge; and metal needles equipped with CVCs are 34 or 67 mm × 22-gauge (Safe Guide®; Microneedle Seldinger Kit, Nippon Covidien, Tokyo, Japan). In this study, 90 % of P60–SCA distances were less than 25 mm (Fig. 4), which can be reached even with the shorter catheters, 22 and 20-gauge angiocatheters, and is thus in danger of inadvertent SCA puncture. Anesthesiologists in our hospital usually select the center of C–M as the puncture point for RIJV catheterization (the so-called “middle” approach; insertion at the inferior border of the thyroid cartilage or cricoid cartilage). Moving a 60°-angled probe to the clavicle within 65 mm of the clavicle on the skin increased the risk of puncturing the SCA. The lower approach, in which operators puncture the RIJV near the clavicle, can avoid kinking of the catheter [8] but may lead to more frequent inadvertent SCA puncture compared with use of the middle or high approach (at the superior border of the thyroid cartilage).
We used the beam from the ultrasound probe to represent the puncture needle. It might be difficult to puncture and place the guide wire when the needle is angled at approximately 90°. Thus, a smaller needle angle might be better for puncturing while avoiding arterial puncture behind the RIJV. On the basis of the literature, recommended angles for needle puncture during RIJV catheterization with ultrasound guidance include 45° [9], 60° [8], and 70° [10]. During our measurements, when the probe was angled at 45°, the edge of the probe became detached from the skin, and it was difficult to obtain ultrasound images. Furthermore, it was impossible to use the 30° angle described in the literature [11]. Thus, we selected the 60° angle.
For a child aged 13 years whose RIJV puncture site was located between the two heads of the sternocleidomastoid muscle 30 mm above the clavicle, a fistula between the right SCA and right brachiocephalic vein was found 18 months after the puncture [1]. In another case, two 14-gauge cannulae were successfully introduced with the high technique, and then a third cannula was introduced a little lower at the apex of the triangle; the “vessel” was easily located 2–3 cm deep, but the blood was noted to be a brighter color [3]. In these two cases, the puncture sites were in a lower area (using the low approach), which, according to our study, increases the risk of SCA puncture. In another case, although real-time ultrasound guidance by the short-axis method was used, and the RIJV was uneventfully punctured, the right SCA was inadvertently cannulated; the authors assumed that the puncture needle had initially been inserted into the RIJV, but had been unintentionally advanced into the right SCA (beyond the RIJV posterior wall) after the absence of arterial back flow had been established and before inserting the guide wire [7]. No authors of case reports confirmed the SCA’s location before puncturing guided by ultrasonography.
We recruited more women than men and thus might have analyzed data from more volunteers with riskier SCA positioning. Although we could not determine any determinant roles of BMI for SCA trauma via RIJV puncture, we believe we targeted a more at-risk population compared with the general population. In our study, 52 % of volunteers had a BMI <20 kg/m2, which has been shown to be a significant (p = 0.036) predictor of mechanical complications associated with CVC (59.4 % of SCV, 18.0 % of RIJV, and others) [12]. Among 894 subclavian vein catheterizations the incidence of complications was higher (16.2 %) when BMI was <20 kg/m2, average (10.4 %) when BMI was 20–30 kg/m2, and lower (4.0 %) when BMI was >30 kg/m2 [13]; neither a high (>30 kg/m2) nor a low (<20 kg/m2) BMI was associated with increased incidence of complications in 385 consecutive CVC attempts, however [14]. SCA trauma occurred during CVC placements (unknown puncture sites) for eight patients, six with BMI ≥ 30 kg/m2 and two with BMI < 30 kg/m2 [15]. In Japan, it is difficult to recruit volunteers with a BMI >30 kg/m2. In this study neither BMI nor height predicted SCA position, except for P60–SCA, and P60–SCA only correlated with BMI for men. Thus, the risk of inadvertent SCA puncture may diminish slightly with increasing BMI for men only. Anatomically, the right SCA ascends slightly above the clavicle, but the extent to which it does varies in different cases. We cannot predict the position of the SCA from patients’ characteristics. Therefore, we recommend that operators observe the position of the SCA every time before puncturing the RIJV guided by ultrasonography.
In a study of 24 patients (7 men and 17 women) with a mean age of 58 years (interquartile range, 49–67 years), one or more arterial vessels were observed for 19 of the patients by use of ultrasound images of the supraclavicular region behind the RIJV (19 SCA and 12 other vessels) [16]. Among these 19 patients, the arteries were, on average, 2.3 mm from the RIJV at the level of the mastoid; however, the distances from the RIJV to the SCA were not noted. In the same study, RIJVP–SCA averaged 6.4 mm, as described for three cadavers (one women, two men; age at death, 76–89 years), which was longer than the average of 4.4 mm in this study; it is possible that the different age ranges (21–42 years vs. 76–89 years) may have affected RIJVP–SCA. More studies of older patients are required. The SCA might be located nearer than expected, and care must be taken not to advance the puncture needle beyond the posterior wall of the RIJV. In a recent study with a lifelike vascular-access mannequin, residents accidentally penetrated the posterior vessel wall of the RIJV under ultrasound guidance in most cases; thus, care must be taken even with ultrasound-guided central catheter placement [17]. Ultrasound guidance has several advantages, including a greater likelihood of success, fewer complications, and less time spent on the procedure, and several guidelines recommend use of static ultrasound [18–21]. Real-time ultrasound-guided catheterization may not be completely reliable, however, as in cases of SCA injury [6, 7] and other arterial punctures [22]. An important caveat for use of ultrasound guidance, particularly relevant to a discussion of arterial cannulation, is that the needle and/or wire may not always be visualized in the vein, depending on the type of ultrasound equipment used and the skill of the operator [23]. A lack of understanding, with regard to visualizing the location of the needle tip, remains a major obstacle [24]. The short-axis approach can provide a false sense of security to the practitioner and can result in potentially dangerous accidental arterial cannulation [22].
In future studies, we would like to examine the position of the SCA on the left side. Several arteries behind the RIJV, for example the thyrocervical trunk, the inferior thyroid artery, the arteries in the posterior cervical triangle (lateral cervical region) [25], and the vertebral artery [26], in addition to the carotid artery and SCA, have recently also attracted attention [24, 27]. We would like to determine the detailed position of the arteries in the posterior cervical triangle by use of ultrasonography.
This study has some limitations. First, we had slight difficulty in obtaining SCA images with the probe angled at 60° by use of a commercially available protractor in the limited space above the neck surface. We might have varied by 5°–10° in measurement of the 60° angle. We thus need to develop more precise probe-positioning methods for use in a limited space. Second, because we did not puncture the volunteers we could not acquire data about the relationships between the SCA depth and incidence of complications.
In conclusion, puncturing the RIJV far away from the center of the neck seems to be safest for avoiding inadvertent SCA puncture, and puncture seems to be more dangerous for women than for men when the probe (representing the puncture needle) moved from the center to the clavicle. The SCA is located behind the RIJV between the clavicle and the center of the neck, but the exact location varies from person to person. We recommend that operators confirm the SCA position by use of ultrasonography every time before RIJV puncture.
References
Gamulin Z, Brückner JC, Forster A, Simonet F, Rouge JC. Multiple complications after internal jugular vein catheterisation. Anaesthesia. 1986;41:408–12.
Huddy SP, McEwan A, Sabbat J, Parker DJ. Giant false aneurysm of the subclavian artery. An unusual complication of internal jugular venous cannulation. Anaesthesia. 1989;44:588–9.
Powell H, Beechey AP. Internal jugular catheterisation. Case report of a potentially fatal hazard. Anaesthesia. 1990;45:458–9.
Kulvatunyou N, Heard SO, Bankey PE. A subclavian artery injury, secondary to internal jugular vein cannulation, is a predictable right-sided phenomenon. Anesth Analg. 2002;95:564–6.
Kim J, Ahn W, Bahk JH. Hemomediastinum resulting from subclavian artery laceration during internal jugular catheterization. Anesth Analg. 2003;97:1257–9.
Choi HJ, Kang BS. An uncommon arteriovenous fistula resulting from haemodialysis catheterization despite applying ultrasound guidance: malposition of catheter into right subclavian artery. Hong Kong J Emerg Med. 2011;18:166–8.
Choi JI, Cho SG, Yi JH, Han SW, Kim HJ. Unintended cannulation of the subclavian artery in a 65-year-old-female for temporary hemodialysis vascular access: management and prevention. J Korean Med Sci. 2012;27:1265–8.
Silberzweig JE, Mitty HA. Central venous access: low internal jugular vein approach using imaging guidance. AJR Am J Roentgenol. 1998;170:1617–20.
Gibbs FJ, Murphy MC. Ultrasound guidance for central venous catheter placement. Hospital Physician. 2006;42:23–31. http://www.turner-white.com/memberfile.php?PubCode=hp_mar06_venous.pdf.
Nadig C, Leidig M, Schmiedeke T, Höffken B. The use of ultrasound for the placement of dialysis catheters. Nephrol Dial Transplant. 1998;13:978–81.
Lim T, Ryu HG, Jung CW, Jeon Y, Bahk JH. Effect of the bevel direction of puncture needle on success rate and complications during internal jugular vein catheterization. Crit Care Med. 2012;40:491–4.
Ives C, Moe D, Inaba K, Castelo Branco B, Lam L, Talving P, Demetriades D, Inaba K. Ten years of mechanical complications of central venous catheterization in trauma patients. Am Surg. 2012;78:545–9.
Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331:1735–8.
Eisen LA, Narasimhan M, Berger JS, Mayo PH, Rosen MJ, Schneider RF. Mechanical complications of central venous catheters. J Intensive Care Med. 2006;21:40–6.
Wicky S, Meuwly JY, Doenz F, Uské A, Schnyder P, Denys A. Life-threatening vascular complications after central venous catheter placement. Eur Radiol. 2002;12:901–7.
Chandra M, Start S, David Roberts, Bodenham A. Arterial vessels behind the right internal jugular vein with relevance to central venous catheterization. J Intensive Care Soc. In press. http://inc.sagepub.com/content/early/2015/01/13/1751143714567434.full.pdf+html.
Blaivas M, Adhikari S. An unseen danger: frequency of posterior vessel wall penetration by needles during attempts to place internal jugular vein central catheters using ultrasound guidance. Crit Care Med. 2009;37:2345–9.
The American College of Surgeons. (ACS) Committee on Perioperative Care. Revised statement on recommendations for use of real-time ultrasound guidance for placement of central venous catheters. Bull Am Coll Surg. 2011;96:36–7.
American Society of Anesthesiologists. (ASA) task force on central venous access. Practice guidelines for central venous access. Anesthesiology. 2012;116:539–73.
Lamperti M, Bodenham AR, Pittiruti M, Blaivas M, Augoustides JG, Elbarbary M, Pirotte T, Karakitsos D, Ledonne J, Doniger S, Scoppettuolo G, Feller-Kopman D, Schummer W, Biffi R, Desruennes E, Melniker LA, Verghese ST. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38:1105–17.
Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD. Reeves ST; Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography; Society of Cardiovascular Anesthesiologists. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg. 2012;114:46–72.
Blaivas M. Video analysis of accidental arterial cannulation with dynamic ultrasound guidance for central venous access. J Ultrasound Med. 2009;28:1239–44.
Bowdle TA. Arterial cannulation during central line placement: mechanisms of injury, prevention, and treatment. http://miradorbiomedical.com/wp-content/uploads/2011/01/Review_ArterialCannulation_Bowdle_FINAL.pdf. Accessed on May 5, 2015.
Chapman GA, Johnson D, Bodenham AR. Visualization of needle position using ultrasonography. Anaesthesia. 2006;61:148–58.
Weiglein AH, Moriggl B, Schalk C, Künzel KH, Müller U. Arteries in the posterior cervical triangle in man. Clin Anat. 2005;18:553–7.
Kayashima K, Ueki M, Kinoshita Y. Ultrasonic analysis of the anatomical relationships between vertebral arteries and internal jugular veins in children. Pediatr Anesth. 2012;22:854–8.
Kayashima K. The artery behind the internal jugular vein: the vertebral artery or transverse cervical artery? Intensive Care Med. 2013;39:794.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Imai, K., Kayashima, K. Evaluating the detailed position of the subclavian artery to avoid inadvertent subclavian artery puncture during right internal jugular vein catheterization. J Anesth 29, 850–856 (2015). https://doi.org/10.1007/s00540-015-2061-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2061-5