Abstract
Back ground
Measurements with various flowmeters are affected by changes in gas mixture density. The Avance Carestation incorporates ventilator feedback controlled by a built-in flowmeter with a variable orifice sensor. We hypothesised that changes in the composition of delivered gas may cause changes in the delivered tidal volume by affecting the flow measurement unless appropriate corrections are made.
Methods
We used 100 % O2, 40 % O2 in N2 and 40 % O2 in N2O as carrier gases with/without sevoflurane and desflurane. We measured delivered tidal volume using the FlowAnalyzer™ PF 300 calibrated with the corresponding gas mixtures during volume control ventilation with 500-ml tidal volume using the Avance Carestation connected to a test lung.
Results
Change of carrier gas and addition of sevoflurane and desflurane significantly altered delivered tidal volume. Desflurane 6 % reduced delivered tidal volume by 7.6, 3.6 and 16 % of the pre-set volume at 100 % O2, 40 % O2 in N2 and 40 % O2 in N2O, respectively. Importantly, the Carestation panel indicator did not register these changes in measured expired tidal volume. Ratios of delivered tidal volume to 500 ml correlated inversely with the square root of the delivered gas density.
Conclusions
These results support our hypothesis and suggest that changing gas composition may alter delivered tidal volume of anesthesia machines with built-in ventilators that are feedback-controlled by uncorrected flowmeters due to changes in gas mixture density.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known that the density and viscosity of delivered gas affect measurement accuracy of various types of flowmeters. In flow measurement with pressure gradient across the conducting tube, the Hagen−Poiseuille law predicts that the pressure difference (∆P) can be given by the following equation for laminar flow:
where μ is the gas viscosity, L is the length of the tube, r is the radius of the tube, and v is flow [1]. For turbulent flow, the pressure difference is given by the following equation:
where ρ is the gas density, L is the length of the tube, r is the radius of the tube, and v is flow [2]. Therefore, when flow is measured with differential pressure flowmeters, the viscosity of the gas may influence laminar flow-type sensors such as the Fleisch pneumotachograph, whereas the density may affect the turbulent flow-type such as orifice flow meters [3].
An earlier study by Goto et al. [4] demonstrated that xenon and nitrous oxide disturbed the flow measurement of various flowmeters and that xenon at high concentrations dramatically induced over-readings of flowmeters using differential pressure measurement due to the increased gas density. They showed that 70 % xenon induced an over-reading of approximately 75 % for a variable orifice flowmeter for a tidal volume of 500 ml. Habre et al. [5] showed that clinical concentrations of volatile anesthetics slightly affect the viscosity of the gas mixture and significantly increase its density. They suggested the possibility that inclusion of volatile anesthetics with the carrier gases may affect flow measurement because of an increase in the density of the gas mixture [5]. To our knowledge, however, no reports have confirmed this possibility. The composition of carrier gases may also affect flow and volume measurements due to changes in density.
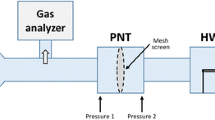
Presently, many anesthesia machines have incorporated ventilators, and some of these ventilators are feedback-controlled by built-in flowmeters. The Avance Carestation (GE Healthcare, Fairfield, CT, USA) has two built-in flowmeters located at the inspiratory and expiratory outlets. Both flowmeters are the same type and measure the pressure difference across a variable-orifice sensor. The flowmeter located at the inspiratory outlet feedback-controls the delivered tidal volume of the incorporated ventilator in a volume control mode, and the flowmeter at the expiratory outlet measures and indicates the expired tidal volume. Therefore, we hypothesised that the addition of volatile anesthetics to carrier gases may induce over-readings of the built-in flowmeter and that this causes reductions in the delivered tidal volume during volume control ventilation by feedback-control unless correction for changes in the gas composition are made. We suspected that the clinical concentration of desflurane may induce clinically significant decreases in the delivered tidal volume because its effects on the density are relatively large due to the high concentrations used clinically. We focused on changes in gas density because the flowmeters concerned are turbulent flow-type meters. We also hypothesised that changes in the composition of carrier gases may induce changes in the delivered tidal volume by affecting the flow and volume measurements. In this study, we aimed to test these hypotheses using a model respiratory circuit in conjunction with the Avance Carestation.
Methods
Correction of volume measurements with the PF300 FlowAnalyzer
We measured the volume with a FlowAnalyzer™ PF300 (Imtmedical AG, Buchs, Switzerland) by applying 500 ml of the test gases in a Super Syringe (Minato Medical Co., Tokyo, Japan). The test gases were 100 % O2, 40 % O2 in N2, and 40 % O2 in N2O. We used these test gases containing no volatile anesthetics (No VA), sevoflurane 1 % (SEV1) and 2 % (SEV2), and desflurane 3 % (DES3) and 6 % (DES6). We manually applied 500 ml of the test gases with or without volatile anesthetics to the FlowAnalyzer™ PF 300 with the Super Syringe and recorded the measured volume. The measurements were repeated 10–22 times, and the measured volumes were averaged. We calculated the ratio of 500 ml to the average of the measured volume for each test gas. In the following experiments using the anesthesia machine, we corrected the volume measured with the PF300 by multiplying the values with these ratios for the corresponding test gases.
Measurement of tidal volume delivered by the Avance Carestation built-in ventilator
We measured the tidal volume delivered by the built-in ventilator of the Avance Carestation using the FlowAnalyzer™ PF 300. A silicon respiratory circuit was attached to the anesthesia machine and was connected to the PF300 and a test lung (Test Lung 190; Maquet, Rastatt, Germany) through a Y piece. Ventilation was performed with 6 l/min of fresh gas flow of the test gases in the volume control mode. Ventilatory parameters were set as tidal volume 500 ml, frequency 10/min, I:E ratio 1:2, and positive end-expiratory pressure 0 cmH2O. Sevoflurane or desflurane was applied with a Tec7 or Tec6 Plus Vaporizer (GE Healthcare). The concentrations of oxygen and inhalation anesthetics were measured with an anesthetic gas analyzer of the side-stream type (M1019A Intellivue; Philips Healthcare, Andover, MA, USA). The sampling port for the anesthetic gas analyzer was removed from the respiratory circuit during the measurement of the tidal volume. After stabilization of the concentrations of oxygen and inhalation anesthetics, we measured the delivered tidal volume using the PF300. We recorded 10–12 consecutive respiratory cycles for each test gas and calculated the corrected delivered tidal volume. Temperature and relative humidity of the room air were measured with a Moiscope (Skynet, Tokyo, Japan), and those of the test gases were measured with the PF300.
Data analysis
The data are presented as means and SD. We examined whether the measurements of the delivered tidal volume were affected by the composition of the test gases (100 % O2, 40 % O2 in N2 and 40 % O2 in N2O) and by the addition of volatile anesthetics (No VA, SEV1, SEV2, DES3 and DES6) using two-way ANOVA. When the effects of these variables were significant, we compared the means of the delivered tidal volume between the three different test gases without volatile anesthetics by Bonferroni multiple comparisons as a post hoc test. We also compared the means of the delivered tidal volume at four different conditions for volatile anesthetics within each test gas by Bonferroni multiple comparisons. Furthernore, we analyzed the relationship between the ratio of the delivered tidal volume to 500 ml and the density of the corresponding delivered gases. The density of the delivered gases was calculated with values reported previously [5–7] (Table 1). For these calculations, temperature and altitude were assumed to be 23 °C and 1013 hPa, respectively. Linear regression was performed by least-square analysis. A p value of <0.05 was considered significant.
Results
Room temperature and relative humidity of the room air ranged from 23.8−24.6 °C and 34–39 %, respectively. Temperature and relative humidity of the test gases ranged from 23.9−24.6 °C and 8–9 %, respectively, according to measurements with the PF300.
Calibration of the PF300 revealed that it under-read the volume when sevoflurane and desflurane were added to the test gases. The ratios for the correction of the measurement with the PF300 are presented in Table 2. In the following experiments, the volume values measured with the PF300 were corrected by multiplying the volume values by these ratios for the corresponding gas compositions.
In the experiments using the Avance Carestation, the results of two-way ANOVA showed that the mean values of the delivered tidal volume were significantly affected by both the composition of the test gases and the addition of volatile anesthetics (p < 0.0001, F = 3706 for the test gases; p < 0.0001, F = 587.6 for the volatile anesthetics). The interactive terms of these variables were also significant (p < 0.0001, F = 32.67). When the mean values of the delivered tidal volume were compared between the three test gases without volatile anesthetics, that of 40 % O2 in N2 was significantly larger and that of 40 % O2 in N2O was significantly smaller compared with that of 100 % O2. In the test gases of 100 % O2 and 40 % O2 in N2O, the addition of sevoflurane and desflurane resulted in significant decreases in the delivered tidal volume at all concentrations studied compared with No VA. In 40 % O2 in N2, SEV2, DES3 and DES6 resulted in significant decreases in the delivered tidal volume compared with No VA. Desflurane dose-dependently decreased the delivered tidal volume in the three test gases, whereas the effects of sevoflurane were dose-dependent in 40 % O2 in N2 and 40 %O2 in N2O but not in 100 % O2 (Table 3). In contrast to the delivered tidal volume, there was little change in the uncorrected expiratory tidal volume displayed on the panel indicator of the Avance Carestation among the test gases with or without volatile anesthetics. The displayed values on the panel were all approximately 525 ml and remained stable. When the ratio of the delivered tidal volume to 500 ml was plotted against the square root of the density of the corresponding gas composition, this ratio was found to correlate inversely with the square root of the density (Fig. 1).
Discussion
In accordance with our hypothesis, we found that the composition of the carrier gases and the addition of volatile anesthetics to the carrier gases caused significant changes in the delivered tidal volume during volume control ventilation with the Avance Carestation when no appropriate correction for changes in gas composition was made. The results showed that sevoflurane and desflurane significantly decreased the delivered tidal volume at clinically used concentrations even though the ventilator settings or the tidal volume displayed on the indicator remained unchanged. These changes seem to be due to the changes in the density of the delivered gases because the ratios of the delivered tidal volume to 500 ml (the pre-set value) correlated inversely with the square root of the density of the delivered gases. Taken together, the changes in the composition of the delivered gases significantly changed the delivered tidal volume during volume control ventilation with the Avance Carestation due to the feedback control by the built-in flowmeter, whose measurement of flow and volume are affected by changes in the density of delivered gases.
These changes in the delivered tidal volume can be avoided when information about changes in gas composition is provided by a gas analyzer linked to the Avance Carestation and correction is automatically or manually applied. However, it seems common that data from gas analyzers are not linked to anesthesia machines and corrections for gas composition changes are not made. In addition, although it is well known that changes in the density of anesthetic gas mixtures affect the flow measurement, it has not been well studied how the delivered tidal volume is altered by changes in the composition of carrier gases and by the addition of volatile anesthetics when the ventilator is feedback controlled by uncorrected flowmeters. Therefore, we considered our findings to have practical significance.
Flowmeters of the turbulent flow type measure the pressure difference across the resistance. The pressure difference is converted to the gas flow rate and volume with integration of the flow. The pressure difference measured by these flowmeters is calculated by
where ∆P, ρ and v are pressure difference, gas density and velocity of the gas, respectively [8]. A variable orifice flowmeter has a movable flap attached at the orifice, and the area of the orifice is changed with the gas velocity. This arrangement improves the measurable flow range and applicability to long-term use [9]. The pressure difference across the orifice measured by variable orifice flowmeters is calculated as
where k(∆P) is a function of ∆P. For example, when a mixed anesthetic gas is used, the pressure difference is calculated as
where ρ (mx) is the density of the mixed anesthetic gas. However, when the flowmeter is not compensated for the gas density or is not calibrated with the anesthetic gas, the delivered gas is assumed to be oxygen. In this condition, the pressure difference is calculated as
where ρ (O2) is O2 density and vc is the calculated gas velocity. Thus:
This equation shows that the ratio of the calculated flow to the true value is proportional to the square root of the density of the mixed anesthetic gas. If the mean density of the mixed anesthetic gas is larger than that of oxygen, the uncorrected variable orifice flowmeter recognises the larger tidal volume delivered compared with the pre-set tidal volume, so the feedback control system will decrease the tidal volume. Thus, the ratio of delivered tidal volume to the pre-set volume is inversely proportional to the square root of the density of the mixed anesthetic gas.
According to the Carestation product manual, the built-in flowmeter is calibrated with 100 % oxygen as a carrier gas. Therefore, among the compositions studied, the delivered tidal volume was closest to the pre-set volume when 100 % oxygen was used. However, our results indicated that even without volatile anesthetics, changing the carrier gas from 100 % O2 to 40 % O2 in N2 increased the delivered tidal volume by approximately 9.7 %, and changing it from 40 % O2 in N2 to 100 % O2 decreased the delivered tidal volume by 8.8 %. Importantly, these changes are not accompanied by changes in the measured expired tidal volume displayed on the panel indicator of the Avance Carestation. Our study also suggested that when 6 % desflurane was added to the carrier gas, this practice reduced the delivered tidal volume by 7.6, 3.6 and 16 % of the pre-set volume at 100 % O2, 40 % O2 in N2 and 40 % O2 in N2O, respectively. These changes in the delivered tidal volume represent a reduction by 6.9, 11.4 and 10.4 % of the tidal volume delivered before addition of desflurane to 100 % O2, 40 % O2 in N2 and 40 % O2 in N2O, respectively. Taken together, changes in delivered gas compositions studied in our experiment caused changes in the delivered tidal volume by up to 16 % of the pre-set volume. According to the product manual, the built-in ventilator has a volume delivery accuracy better than 7 % for tidal volume of >210 ml, when the ventilator is operating with 100 % oxygen or it is corrected with gas composition by a gas analyzer [10]. The manual says that 60 % N2O may induce >10 % error or anesthetic agents may cause 0.95 % error for each 1 % volume agent [10]. In our study, 60 % N2O reduced the delivered volume by 6.2 and 6 % desflurane induced 6.9–11.4 % reduction depending on the carrier gases. Therefore, desflurane seemed to cause larger errors than that indicated in the product manual. However, because the amplitudes of these errors are unlikely to be large enough to induce severe clinical consequences, it would be acceptable to use the Avance Carestation without correction of gas composition in the most cases as long as the anesthesia personnel are aware of these errors in ventilator control and adjust the ventilator settings in response to changes in expired carbon-dioxide concentrations.
The effect of gas composition changes will vary depending on the type of anesthesia machine. It may be different when various types of built-in flowmeters are used and is not important when ventilators are not feedback-controlled by flowmeters.
There are several limitations to our study. First, we used the PF300 FlowAnalyzer™ PF300 to measure the actual delivered tidal volume after correction for changes in the composition of the gas mixture. The PF300 measures the differential pressure across a screen within a flow channel to determine the flow measurement. Therefore, the viscosity and density of test gases affect the flow measurement of the PF300. We corrected influences from the gas composition by calculating the ratio of the actual to the measured volume of each gas mixture. We performed this by applying 500 ml of test gases with or without volatile anesthetics to the PF300 using a Super Syringe. However, this procedure does not precisely mimic the actual flow during volume control ventilation. Because the influences due to physical properties of test gases vary depending on the flow, the correction we used may have errors. Second, the temperature and humidity of the delivered gases in our experiment are much lower than those found in clinical settings. These factors are known to influence the effects of viscosity and density on flow and volume measurements. Although the amplitudes of the influences from differences in temperature and humidity are not precisely known, changes in the humidity of delivered gases seem to have small effects on the density because changes in the concentration of the water vapour are small. The density of test gases decreases as temperature increases; however, differences in the absolute temperature are small (approximately 1 %) and would induce small decreases in the square root of the density. Third, we did not study a wide range of tidal volumes but only that of 500 ml. However, the inverse correlation between relative changes in the tidal volume and the square root of the density will remain the same over a range of flows and volumes. Finally, our findings obtained in the model system need to be confirmed to prove reliable in the clinical setting.
In conclusion, changes made in the composition of delivered gases significantly altered the delivered tidal volume during volume control ventilation with the Avance Carestation due to feedback control by the built-in flowmeter when changes in the density of the gas mixture are uncorrected, and these changes were not registered on the tidal volume panel display of the Carestation.
References
Cotes JE, Chinn DJ, Miller MR. Lung function: physiology, measurement and application in medicine. 6th ed. Oxford: Blackwell Publishing Ltd.; 2006. p. 61–3.
Hess DR, Fink JB, Venkataraman ST, Kim IK, Myers TR, Tano BD. The history and physics of heliox. Respir Care. 2006;51(6):608–12.
Schena E, Massaroni C, Saccomandi P, Cecchini S. Flow measurement in mechanical ventilation: a review. Med Eng Phys. 2015. doi:10.1016/j.medengphy.2015.01.010.
Goto T, Saito H, Nakata Y, Uezono S, Ichinose F, Uchiyama M, Morita S. Effects of xenon on the performance of various respiratory flowmeters. Anesthesiology. 1999;90(2):555–63.
Habre W, Asztalos T, Sly PD, Petak F. Viscosity and density of common anaesthetic gases: implications for flow measurements. Br J Anaesth. 2001;87(4):602–7.
The Merck Index: an encyclopedia of chemicals, drugs, and biologicals. 14th ed. N.J., USA.: Merck Research Laboratories; 2006. Nitrous oxide, Oxygen; p. 6655, 6962.
Rika Nenpyo (Chronological Scientific Tables 2012). Tokyo, Japan: Maruzen Publishing; 2011. Density of gases; p. 388.
Elliott SE, Shore JH, Barnes CW, Lindauer J, Osborn JJ. Turbulent airflow meter for long-term monitoring in patient–ventilator circuits. J Appl Physiol Respir Environ Exerc Physiol. 1977;42(3):456–60.
Osborn JJ. A flowmeter for respiratory monitoring. Crit Care Med. 1978;6(5):349–51.
Specifications and Theory of Operation. GE Healthcare. Avance User's Reference Manual. Software Revision 6.X. p. 27.
Acknowledgments
This work was presented, in part, at the Annual Meeting of the Japanese Society of Anesthesiologists, Sapporo, May 2013. This work was financially supported by the department fund.
Conflict of interest
The authors have no conflict of interests to declare.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Miyaji, T., Fukakura, Y., Usuda, Y. et al. Effects of gas composition on the delivered tidal volume of the Avance Carestation . J Anesth 29, 690–695 (2015). https://doi.org/10.1007/s00540-015-2018-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2018-8