Abstract
Irritable bowel syndrome (IBS) displays chronic abdominal pain or discomfort with altered defecation, and stress-induced altered gut motility and visceral sensation play an important role in the pathophysiology. Corticotropin-releasing factor (CRF) is a main mediator of stress responses and mediates these gastrointestinal functional changes. CRF in brain and periphery acts through two subtype receptors such as CRF receptor type 1 (CRF1) and type 2 (CRF2), and activating CRF1 exclusively stimulates colonic motor function and induces visceral hypersensitivity. Meanwhile, several recent studies have demonstrated that CRF2 has a counter regulatory action against CRF1, which may imply that CRF2 inhibits stress response induced by CRF1 in order to prevent it from going into an overdrive state. Colonic contractility and sensation may be explained by the state of the intensity of CRF1 signaling. CRF2 signaling may play a role in CRF1-triggered enhanced colonic functions through modulation of CRF1 activity. Blocking CRF2 further enhances CRF-induced stimulation of colonic contractility and activating CRF2 inhibits stress-induced visceral sensitization. Therefore, we proposed the hypothesis, i.e., balance theory of CRF1 and CRF2 signaling as follows. Both CRF receptors may be activated simultaneously and the signaling balance of CRF1 and CRF2 may determine the functional changes of gastrointestinal tract induced by stress. CRF signaling balance might be abnormally shifted toward CRF1, leading to enhanced colonic motility and visceral sensitization in IBS. This theory may lead to understanding the pathophysiology and provide the novel therapeutic options targeting altered signaling balance of CRF1 and CRF2 in IBS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Irritable bowel syndrome (IBS) displays chronic abdominal pain or discomfort with altered defecation, which is not explained by structural or biochemical abnormalities. The prevalence is quite higher in the general population (10–20 %) [1–4], impairs patients’ quality of life, and has an enormous economic impact including direct costs of health care use and indirect costs of absenteeism from work [2]. The pathophysiology of IBS has not been determined definitely but it is generally accepted that dysfunction of the bidirectional communication system between brain and gut, i.e., the brain–gut axis, contributes to symptom generation [5, 6].
Stress induces behavioral, neuroendocrine, and autonomic responses, and corticotropin-releasing factor (CRF) is the main mediator of these responses in the brain–gut axis [7–13]. Stress also alters colonic motor and sensory functions, which are thought to play an important role in IBS pathophysiology [14–16]. Several animal and a few human studies proved that CRF mediates these gut responses [16–19]. Administration of CRF alters colonic motility and increases plasma adrenocorticotropic hormone (ACTH), and these responses are exaggerated in IBS patients [17]. These lines of evidence suggest that altered brain–gut axis resulting from exaggerated response to CRF and leading to changes in colonic functions is thought to be relevant to the pathophysiology of IBS.
In this paper, we will review the actions and mechanisms of central and peripheral CRF signaling in colonic motor and visceral sensory functions, and discuss the possible role of CRF signaling in the pathophysiology of IBS. We will also present the balance theory of CRF receptor signaling, which may well explain the actions of CRF in gastrointestinal (GI) functions. Finally, the therapeutic role of CRF signaling according to this theory will be also discussed.
CRF receptors and ligands
CRF is a 41-amino-acid residue peptide that was originally isolated from ovine brain [20] and named for its property to stimulate anterior pituitary secretion of ACTH. During the last 20 years, three new mammalian CRF-related peptides, urocortins (Ucns), such as urocortin 1 (Ucn1), urocortin 2 (Ucn2), and urocortin 3 (Ucn3), have been characterized [21–24].
CRF and Ucns exert its action through the activation of two receptors, CRF receptor type 1 (CRF1) and type 2 (CRF2) [25, 26]. CRF receptors are members of the G-protein-coupled receptors family. The dominant mode of signaling for both CRF1 and CRF2 is the Gs-coupled adenylate cyclase-phosphokinase cascade [24]. However, CRF receptors coupled to other types of G proteins have also been demonstrated [25, 27], and phospholipase C-protein kinase C and extracellular signal-regulated kinase–mitogen-activated protein kinase cascades are also reported [25].
Despite sharing 70 % amino acid sequence similarity, CRF1 and CRF2 display distinct characteristic affinities for CRF and Ucns [21–23]. CRF has a higher affinity (10- to 40-fold higher) for CRF1 than for CRF2. Ucn1 binds CRF2 with 100-fold greater affinity than CRF, and CRF1 with sixfold greater affinity than CRF [21–23]. Ucn2 and Ucn3 exhibit high selectivity only for CRF2 [22, 23].
Role of CRF in stress-induced stimulation of colonic motor function
Although no specific or consistent abnormal changes in GI motility definitely related to abdominal pain or discomfort are determined, many studies reported altered colonic motility in IBS [14, 28, 29]. Several (but not all) studies showed that accelerated colonic transit is observed in diarrhea-predominant IBS [29]. In addition, IBS patients display exaggerated motility response to stress as compared to healthy controls [18], suggesting the importance of stress and altered colonic motility in symptom generation in IBS.
Central CRF receptors
Various stressors such as psychological (water avoidance), physical (restraint), or immunological (interleukin-1β) accelerate colonic transit and stimulate colonic contractions in rodents [30–36]. Central administration of CRF stimulates colonic motility such as reduced colonic transit time, stimulation of defecation, and colonic contractions [33–37]. These responses are blocked by central administration of a non-selective CRF receptor antagonist such as α-helical CRF(9–41) or astressin, and central administration of CRF mimics the responses [30, 31, 35, 38].
Meanwhile, CRF1 and CRF2 are known to display a different response in colonic motor function. CRF, Ucn1, or Ucn2 administered intracerebroventricularly (icv), increases fecal pellet output, and Ucn1 has similar potency as CRF. However, Ucn 2 is about ten and eight times less potent than CRF and Ucn1, respectively in mice [39]. In addition, restraint stress or icv CRF-induced stimulation of pellet output and acceleration of distal colonic transit were prevented by icv, a selective CRF1 antagonist, NBI-35965 but not by icv, a selective CRF2 antagonist, astressin2-B [40]. These results indicate that activation of brain CRF1 is involved in the stress-induced stimulation of colonic motor function.
Central CRF-induced altered motor function is independent from the activation of the hypothalamic–pituitary–adrenal axis because this response is observed in hypophysectomized rats [37]. Chlorisondamine or atropine (but not bretylium) blocked central CRF-induced stimulation of colonic transit, but vagotomy only reduced this response by 19 % in rats [33, 34]. Meanwhile other studies demonstrated that vagotomy completely abolished this response by CRF [37]. Thus, stimulation of central CRF receptors may activate vagal and sacral parasympathetic neurons resulting in increased enteric nervous system activity, thereby stimulating colonic motor function.
In addition, central CRF or restraint stress-induced stimulation of defecation was blocked by peripheral administration of 5-hydroxytryptamine (5-HT)3 antagonist or 5-HT4 antagonist [38, 41]. Moreover, increase in 5-HT content in the feces of rat proximal colon by intracisternal (ic) CRF or restraint stress was observed and it was inhibited by ic, a selective CRF1 antagonist, NB1-27914. These results suggest that parasympathetic cholinergic activation of colonic 5-HT3 and 5-HT4 receptors also mediates the action of CRF.
Microinjection of CRF into the specific brain nuclei reveals the responsive site to CRF. Mönnikes et al. [33, 34, 42] showed it is localized in the hypothalamus (paraventricular nucleus; PVN, arcuate nucleus) and pontine areas, such as locus coeruleus (LC). These brain nuclei are known to be involved in CRF-induced anxiety and depression [43–45]. PVN contains numerous CRF-like immunoreactive neurons and receptors, and sends direct projections to dorsal vagal complex and spinal preganglionic neurons controlling autonomic nervous system activity [46, 47]. LC noradrenergic neurons during stress can supply norepinephrine across the central nervous system and modulate the stress response [48]. Activation of LC by CRF induces increased vigilance and anxiogenic behavior [49, 50]. These results may support the role of brain CRF receptors in the pathophysiology of IBS because IBS patients are frequently comorbid with psychiatric disorders such as anxiety and depression [51] and display greater reactivity to stress [52].
Water avoidance stress (WAS) induces numerous Fos-positive cells in PVN, LC, nucleus tractus solitarius (NTS), and the parasympathetic nucleus of the lumbosacral spinal cord (L6–S1) in rats [30, 53]. Bilateral microinfusion of α-helical CRF(9–41) into the PVN before restraint or WAS abolished stress-induced alterations of colonic transit [33, 34]. These results further support the notion that stress or CRF activates PVN and LC, leading to stimulating colonic motor function mediated through vagal and sacral parasympathetic neurons.
Peripheral CRF receptors
Intravenous (iv) administration of CRF induces the stimulation of pellet output and colonic transit with a potency similar to central injection (icv) in rats [38, 54, 55]. Peripherally injected CRF antagonist, α-helical CRF(9–41) or astressin, which does not cross the blood–brain barrier, blunts the stimulation of distal colonic transit and fecal pellet output induced by acute wrap restraint or WAS in rats [38, 54–56]. Moreover, in in vitro studies, CRF increases distal colonic myoelectric activity [56], and Ucn1 or CRF stimulates contractions of colonic muscle strips [57, 58]. These results strongly suggest that CRF also acts peripheral CRF receptors to stimulate colonic motility.
Enhanced colonic motility induced by peripheral CRF is mediated through CRF1, which is supported by the following evidence. Peripheral administration of CRF reduces colonic transit time but Ucn2 or Ucn3 does not induce the response under the same conditions in rodents [59, 60]. Intraperitoneal (ip) cortagine, a selective CRF1 agonist, decreases the distal colonic transit time, increases distal and transverse colonic contractility, increases defecation, and induces watery diarrhea in rats [61]. In addition, ip administration of NBI-27914 or CP-154, 526, a selective CRF1 antagonist, abolishes the response by CRF [59, 60]. Since all now available CRF1 antagonists can cross the blood–brain barrier, these results do not indicate directly the role of peripheral CRF1. However, as described above, stress-induced stimulation of defecation is abolished by non-selective CRF receptor antagonists with peripheral limited action, and moreover, subcutaneous (sc) injection of astressin2-B does not alter accelerated distal colonic transit induced by restraint stress [60]. These results suggest that peripheral injection of CRF- or stress-induced stimulating colonic motor function is mediated through peripheral CRF1.
Recent studies demonstrated the expression of CRF receptors and ligands in the colon in various cells such as neuronal (enteric nervous system), enterochromaffin (EC), and immune cells (mast cells, lymphocytes) in rodents and humans [62–70]. Most of these studies also showed that CRF and Ucns are expressed in close proximity to the CRF receptors. Moreover, both EC cells and mast cells are not only a target of peripheral CRF to stimulate the release of chemical mediators such as serotonin, etc., but also secrete CRF itself [69, 71–73]. Luminally released serotonin from EC cells activate mucosal 5-HT3 receptors located on the vagal afferents, which stimulates colonic motility via the vagovagal reflex [74]. These results suggest that peripheral CRF and Ucns may form an autocrine/paracrine loop, thereby modulating the motility.
In addition, several studies suggested that colonic myenteric neurons are also possible action sites of peripheral CRF for the following reasons. Ip CRF induces colonic myenteric Fos expression through peripheral CRF1 and nearly all of the Fos-expressing cells are CRF1 immunoreactive [75]. Moreover, Fos activation by ip CRF is correlated with increased defecation [75]. Ucn1 evokes the contractions of rat colonic smooth muscle strips, which are blocked by a selective CRF1 antagonist, antalarmin, or the neuronal blocker tetrodotoxin [57]. Additionally, myenteric neurons in the guinea pig jejunum display an increased intracellular calcium concentration in response to CRF application, and this neuronal activation is mediated through CRF1 [76].
In contrast to the above results, Tsukamoto et al. [77] demonstrated that the stimulatory effect of peripherally administered CRF on colonic motility was abolished by truncal vagotomy, hexamethonium, atropine, and ic astressin, and suggested the possibility that peripheral injection of CRF reaches the area postrema (AP) and activates the dorsal nucleus of vagus via central CRF receptors, resulting in activation of the vagal efferent, leading to the stimulation of colonic motility. CRF does not penetrate to the brain but circumventricular organs including AP are relatively unprotected by the blood–brain barrier [78].
There is also evidence that peripheral injection of CRF activates several brain nuclei such as PVN, central amygdala (CeA), NTS, and AP [79, 80]. Additionally, CRF injection also induces Fos expression in lumbosacral spinal intermediolateral column and dorsal horn [80], which are known to contain cells that engage in ascending supraspinal projections to the NTS [81]. Moreover, it is also known that NTS receives a large proportion of efferents from AP [82]. CRF receptors are present on AP, and the cervical and subdiaphragmatic vagus [83, 84]. These results suggest that peripheral CRF may stimulate NTS possibly through humoral, i.e., by directly activating AP, and/or neural mechanisms, i.e., through vagus afferents and/or ascending projections from lumbosacral spinal cord, then NTS may transfer convergent information to the dorsal nucleus of vagus [85], leading to modulating colonic motility. As described before, PVN is a responsive site to central CRF inducing the stimulation of colonic motor function. In addition, as will be described later, CeA is thought to be one of the responsive area to brain CRF inducing visceral sensitization. In this context, we would emphasize that the possibility of contribution of central pathways to modulating colonic functions by peripheral administration of CRF has not been denied.
Role of CRF in stress-induced altered visceral sensation
It is now widely accepted that an altered visceral sensitivity plays an important role in the pathogenesis of IBS [14, 86, 87]. Previous studies indicate that 33–90 % of IBS patients display increased visceral sensitivity to rectal balloon distention [88–93]. Several factors such as various methods determining the sensitivity, etc., may contribute to the observed wide range of hypersensitivity, but in any event, these results also suggest that a significant portion of the patients do not develop visceral hypersensitivity in the basal state. Meanwhile, we and other researchers demonstrated that conditioning such as repetitive colon or rectal distention induces visceral hypersensitivity in IBS patients regardless of the baseline sensitivity, and this response is not observed in healthy controls [94, 95], which may be a reliable marker for IBS. It was reported that visceral stimulation can be interpreted as stress to IBS patients because it evokes daily symptoms and negative emotion [86]. These lines of evidence further support the importance of stress and altered visceral sensation in pathophysiology of IBS.
Central CRF receptors
Several stress models evoke visceral hypersensitivity and this response is blocked by central injection of CRF antagonist [96, 97]. Meanwhile, central administration (icv) of CRF induces visceral hypersensitivity to colorectal distention (CRD) in rats [96], which is mediated through CRF1 [98]. However, the studies evaluating the brain sites responsible for modulating visceral sensation have been limited so far. Kosoyan et al. [99] showed that LC neurons were activated by CRD or ic CRF, which was abolished by iv NBI-35965, which can cross the blood–brain barrier in rats, indicating that CRF1 signaling plays a role in visceral hypersensitivity through activating LC.
Su et al. [100] very recently demonstrated that CRF microinjected into CeA increased visceromotor response (VMR) to CRD and the response was blocked by injection of CP-15426, a selective CRF1 antagonist into this site. CRF-like immunoreactivity and gene expression in CeA are increased in response to CRD [101]. It is also known that the amygdala is an important site contributing to persistent pain, inducing negative affective states such as fear, anxiety, and depression [102].
These observations suggest the possibility of a pathogenetic role of LC and CeA in IBS. CeA contains a high density of CRF neurons [103, 104], and these neurons project to the LC and increase their firing rate, resulting in the stimulation of the ascending noradrenergic system [105]. The release of noradrenaline in the cortical and limbic rostral efferent projections from the LC or CeA [106] is known to induce arousal and anxiogenic responses along with hypervigilance to visceral input, which is commonly observed in IBS [107].
Early maternal separation, which is one of the models of IBS displaying visceral sensitization [108], induces heightened basal tone of CRF gene expression, increased levels of CRF, and upregulation of CRF1 signal transduction in the specific brain area such as LC and CeA, leading to enhanced reactivity to stress in adult rats [109–112]. Therefore, LC and CeA may be responsive sites of brain CRF-CRF1 signaling and mediate stress-induced visceral sensitization.
Peripheral CRF receptors
Peripheral CRF1 signaling also contributes to visceral hypersensitivity. It was shown that WAS-induced visceral hyperalgesia was prevented by sc astressin [113]. We also demonstrated that CRD-induced visceral hyperalgesia was prevented by ip astressin but not by ip astressin2-B [58]. In addition, peripheral CRF1 activation by ip cortagine increased VMR to CRD, which was blocked by ip astressin but not by icv [61]. These results suggest that stress-induced visceral hypersensitivity is also mediated through peripheral CRF1.
The definite action sites of peripheral CRF in modulating visceral sensation has not been determined. Since CRF receptors are proven to be expressed in dorsal root ganglia (DRG) [114], CRF may modulate visceral sensation through CRF receptors on spinal afferents directly.
As mentioned earlier, EC cells have CRF receptors and release serotonin through activating the receptors [65, 71]. Serotonin from EC cells is thought to contribute to visceral hypersensitivity through activating spinal afferents [115]. In addition, it became certain that mast cells of the GI tract also play an important role in stress-induced visceral sensitization [116]. Partial restraint stress-induced colonic hypersensitivity is prevented by doxantrazole, a mast cell stabilizer in rats [96]. Mast cells have CRF receptors at their surface [66, 67] and their degranulation is triggered by peripheral CRF in the GI tract [72]. They contain and release a large variety of mediators such as serotonin, prostaglandins, and cytokines in response to various stimuli, and these mediators were demonstrated to activate visceral afferents or DRG neurons [117, 118], leading to induction of visceral sensitization. Therefore, peripheral CRF not only acts directly on visceral afferents but also indirectly through stimulating the release of chemicals from EC and mast cells leading to activating the afferents.
Meanwhile, acute stress-induced hypersensitivity to CRD was found to be linked to an increase in colonic paracellular permeability [119]. Ait-Belgnaoui et al. [119] demonstrated that restraint stress-induced increased colonic permeability was blocked by ip α-helical CRF(9–41), and ip CRF mimicked this response. Moreover, CRF-induced increased permeability was blocked by ip doxantrazole. Therefore visceral sensitization induced by peripheral CRF signaling may result from altered colonic permeability possibly through mast cell-dependent mechanisms.
A balance theory of CRF1 and CRF2 signaling to modulate colonic motor and visceral sensation
As described above, central and peripheral CRF-CRF1 signaling is involved in the stimulatory action on colonic motility and sensation induced by stress. However, stress activates both CRF1 and CRF2 signaling. For example, restraint stress induces delayed gastric transit through CRF2 [60, 120], and simultaneously it also results in the stimulation of colonic motility through CRF1 [40]. Stress may stimulate the release of CRF and Ucns in the brain and periphery, which could activate both CRF receptors according to the distinct affinity for each CRF receptor. Thus it is thought that CRF2 may also contribute to stress-induced altered colonic functions.
In fact, we and other researchers showed that the activation of peripheral CRF2 by peripheral administration of selective CRF2 agonist such as sauvagine or Ucn2 blocked repetitive CRD-induced visceral hyperalgesia in rats [58, 114, 121], suggesting that CRF2 signaling may have a counter action to CRF1 in modulating visceral sensation. Moreover, recently this counter action was also observed in the modulation of colonic motility. Gourcerol et al. [62] showed that ip Ucn2 inhibited ip CRF-induced stimulation of defecation and ip astressin2-B further enhanced the response in rats. Moreover, restraint stress-induced stimulation of colonic contractions and WAS-induced stimulation of pellet output were prevented by ip Ucn2.
Acute stress induces integrated responses to maintain homeostasis and warrant survival of organisms. In the absence of proper counter regulation, the stress response runs in an overdrive state that can become maladaptive and fatal [122]. In this context, the existence of counter action by CRF2 signaling may be suitable for the survival of organisms under stressful conditions.
In this context, we hypothesized as follows. Colonic contractility and sensation may be explained by the state of the intensity of CRF1 signaling. CRF2 signaling may play a role in CRF1-triggered enhanced colonic functions through modulation of CRF1 activity. The signaling balance of CRF1 and CRF2 might determine the functional colonic changes induced by stress. We designated this hypothesis as balance theory of CRF1 and CRF2 signaling.
We [58] have very recently demonstrated several results supporting the hypothesis. Ip CRF increased the colonic contractions and selective CRF1 stimulation by cortagine also increased the contractility in rats. Blocking or activating peripheral CRF2 by itself did not alter the basal contractility, while blocking CRF2 enhanced the response by CRF. These results may be explained by the following (schematic illustrations are shown in Fig. 1).
Schematic illustration of our theory on the mechanism of peripheral CRF-induced stimulation of colonic contractions. In the basal condition, both CRF1 and CRF2 signaling are not activated (a). CRF activates both CRF1 and CRF2 with higher affinity for CRF1. Thus, CRF induces strong activation of CRF1 signaling prevailing over the inhibition by CRF2 signaling, resulting in enhanced colonic contractility (b). CRF1 agonist stimulates colonic contractility without interference of CRF2 signaling (c). The CRF2 agonist or antagonist does not change colonic contractility because of a lack of the activated CRF1 signaling (d, e). Meanwhile, CRF2 antagonist induces disinhibition of CRF1 signaling, and enhances the stimulatory action of colonic contractility by CRF (f). The signaling balance of CRF1 and CRF2 may determine the state of colonic contractions (g)
In the basal condition, neither type of CRF signaling is activated (Fig. 1a). CRF activates both CRF1 and CRF2, and CRF has a much higher affinity for CRF1 [21–23]. CRF induces strong activation of CRF1 signaling, prevailing over the inhibition by CRF2 signaling, leading to stimulation of colonic contractility (Fig. 1b). CRF1 agonist stimulates colonic contractility without modulation of CRF2 signaling (Fig. 1c). The CRF2 agonist or antagonist by itself does not change colonic contractility because of a lack of activation of CRF1 signaling (Fig. 1d, e). Meanwhile, CRF2 antagonist induces disinhibition of CRF1 signaling, and enhances the stimulatory action of colonic contractility by CRF (Fig. 1f). The signaling balance of CRF1 and CRF2 may determine the state of colonic contractions (Fig. 1g). Moreover, this hypothesis was also tested in an in vitro study using colonic muscle strips. CRF evoked the contractions of strips and Ucn2 abolished this response [58].
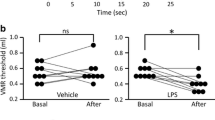
We also showed the results regarding visceral sensation, which was consistent with the hypothesis in that paper. Namely, CRD induced visceral sensitization, which was blocked by ip astressin. Ip cortagine enhanced (but Ucn2 abolished) the response. Meanwhile, ip CRF did not alter CRD-induced sensitization, but ip CRF together with CRF2 blocking further enhanced the response by CRD. These results may be explained by the balance theory as follows.
CRD may activate peripheral CRF1 and induce CRF1-dependent visceral sensitization. Then, CRF1 agonist further enhances (and CRF2 agonist reduces) the response induced by CRD. When exogenous CRF is administered in this condition, both signaling are activated simultaneously and increases the signal intensity in addition to the one induced by CRD. Although CRF has higher affinity for CRF1, activating CRF2 by ip CRF may be enough to suppress the intensity of CRF1 signaling in modulation of visceral sensation, resulting that an overall response by exogenous CRF is not remarkable. Therefore, CRF2 blocking with ip CRF further enhances the sensitization by disinhibition of CRF1 signaling.
The balance theory could explain well CRF and stress-induced altered colonic functions as described above, and moreover, we also suggested that peripheral CRF-induced altered gastric contractility may follow the same rule [123]. In this context, CRF-induced altered upper and lower GI functions might be explained by the theory.
The balance may be determined by the injected or released peptides during stress such as CRF and Ucns, and expression profile of CRF1 and CRF2 may also contribute to the signaling balance. CRF1 and CRF2 receptors are expressed in colon, and stress such as open field or CRD alters these receptor expression [124], suggesting that the dominant signaling may depend on the mode of stress.
The mechanisms of interaction between CRF1 and CRF2 signaling
How does the CRF2 signaling modulate the CRF1 signaling? Several studies showed the following evidence.
Liu et al. [125] demonstrated in myenteric plexus of guinea pig colon that CRF1 was mainly expressed in ganglion cell somas and CRF2 was expressed in varicose nerve fibers. CRF1 and CRF2 evoked depolarization of different types of myenteric neurons. In addition, they also suggested immunohistochemically that CRF2 might be expressed at pre-synaptic transmitter release sites. Therefore it is possible to think that CRF2 might regulate a neurotransmitter release, thereby modulating the neuronal activity induced by CRF1.
Gourcerol et al. showed that CRF1 and CRF2 were colocalized in the colonic myenteric plexus and CRF2 was expressed with neuronal nitric oxide in rats. On the basis of these results, they speculated the possibility that CRF2 inhibits CRF1 signaling through the release of inhibitory neurotransmitter such as nitric oxide [62].
The above findings may be possible mechanisms of the CRF1 and CRF2 interaction in modulating colonic motility. Meanwhile, there are also the results suggesting the mechanisms in modulating visceral sensation. CRF2 is proved to be expressed in DRG, and CRD induces activation of splanchnic afferents in in vitro experiments using colorectal preparation with the attached mesenteric artery and splanchnic afferent nerve, which is blunted by intra-arterial injection of Ucn2 [114]. In this context, CRF may modulate visceral sensation through CRF receptors on spinal afferents, and the interaction of CRF1 and CRF2 might occur in this level.
As described before, EC cells and mast cells are targets of CRF. Both cells have CRF1 and CRF2 [65–67] and the mediators released from these targets can modulate the visceral sensation. Therefore, CRF1 and CRF2 interaction may also occur at these cells, possibly at the cellular level. Gourcerol et al. [62] speculated that CRF2 activation may share intracellular signaling targets of CRF1, leading to inhibition of CRF1 signaling.
The rationale of our proposed theory was only suggested by the studies regarding peripheral CRF receptors-induced altered GI functions. It would be possible that the actions induced by central CRF or ones other than GI response, such as endocrine, immune, autonomic, behavioral response, etc., are also explained by the balance theory. Further studies are needed.
CRF signaling as a therapeutic target for IBS
IBS patients have exaggerated responsivity of the gut, neuroendocrine, and the brain to stress [6, 18, 126, 127]. Stress induces onset and/or exaggeration of GI symptoms in the majority of IBS patients [128, 129]. In addition, as described above, so far, altered colonic motility and visceral sensation induced by CRF-CRF1 signaling are thought to play a key role in the pathophysiology of IBS.
Exaggerated stress response in IBS patients may be explained by the abnormal expression of CRF receptors and their function. In animal studies, differential alterations of the receptors’ expression in colon are observed between Sprague–Dawley and Wister Kyoto (WKY) rats, which may explain the high stress susceptibility of WKY rats [124]. WKY rats are a stress-sensitive strain, which spontaneously exhibit a high-anxiety phenotype and altered stress responses [130] and display visceral hypersensitivity [131] and increased stress-related defecation [132]. Recently, it was also demonstrated that genetic polymorphisms and haplotypes of CRF1 are associated with IBS and related bowel patterns [133]. Single-nucleotide polymorphisms in the regulatory region of the CRF1 gene might influence the expression of CRF1 [134] and the generation of CRF1 variants with distinct structural and signaling properties [25, 135].
In any event, altered stress response in IBS may be due to increased CRF-CRF1 signaling. In other words, CRF signaling balance might be abnormally shifted toward CRF1 in IBS, particularly the diarrhea-predominant type, according to our balance theory (Fig. 2a). In this context, blocking CRF1 signaling is thought to be effective in treating IBS (Fig. 2b).
The signaling balance of CRF1 and CRF2 might be abnormally shifted toward CRF1 by endogenously released CRF receptor ligands, i.e., CRF and Ucns, leading to enhanced colonic motility and visceral sensitization in IBS (a). According to the balance theory, both CRF1 antagonist and CRF2 agonist may be useful in treating IBS. CRF1 antagonist inhibits CRF1 signaling, resulting in normalizing the signaling balance (b). CRF2 agonist increases the signal intensity of CRF2 in addition to the one induced by endogenous CRF2 ligands, thereby resetting signaling balance to a normal state (c)
Contrary to expectations, clinical trials in IBS diarrhea-predominant female patients did not show any significant beneficial effect of CRF1 antagonist, pexacerfont (BMS-562086) in IBS symptoms [136]. However, this result does not deny the usefulness of the CRF1 antagonist itself. Tested dose of the compound might not be optimal for the treatment. Additionally, IBS patients may be a heterogeneous population. Even in diarrhea-predominant IBS, colonic accelerated transit is not a consistent feature [29]. CRF1 antagonist might be effective only in the subpopulation of IBS patients, having exaggerated response to CRF-CRF1 signaling. Further studies with different protocols are needed to examine the effectiveness.
Our proposed theory also suggests that in addition to CRF1 antagonist, CRF2 agonist may be a promising tool in treating IBS by resetting the abnormally shifted signaling balance to a normal state (Fig. 2c). CRF2 in the brain induces anxiolysis, while anxiety-related behavior is mediated through CRF1 [137]. Thus, CRF2 agonist might also be beneficial for the comorbid psychological abnormality of IBS patients. Since stimulation of CRF2 reduces gastric emptying in rats [138], it might induce dyspeptic symptoms. Therefore CRF2 agonist with high organ selectivity, i.e., only targeted for colon and brain might be needed for clinical application.
The pathogenesis of IBS is thought to be multifactorial. We only mentioned colonic motility and visceral sensation, but altered intestinal barrier [139], microbiota [140], low-grade inflammation [141], abnormal pain processing in brain [142], etc., are also known to contribute to the pathophysiology. Recent studies show that these factors are also able to be modulated by CRF signaling [72, 143–145]. These observations may further support the rationale of application of CRF receptors-related drugs for the treatment.
Conclusions
Altered colonic motility and visceral sensation are thought to contribute to the generation of IBS symptoms and CRF-CRF1 signaling plays a pivotal role in the pathophysiology of IBS through modulating these functions. In addition, CRF2 signaling is also demonstrated to modulate CRF and stress-induced altered colonic functions, and it has a counter regulatory action against CRF1. We proposed a balance theory of CRF1 and CRF2 signaling, i.e., both CRF receptors would be activated during stress simultaneously, and the signaling balance may determine the functional changes in GI tract. This theory is useful for understanding the pathophysiology of IBS and may also provide the novel therapeutic options targeting altered signaling balance of CRF1 and CRF2 in IBS.
References
Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10:712–21, e1–4.
Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–80.
Saito YA, Schoenfeld P, Locke GR 3rd. The epidemiology of irritable bowel syndrome in North America: a systematic review. Am J Gastroenterol. 2002;97:1910–5.
Lau EM, Chan FK, Ziea ET, et al. Epidemiology of irritable bowel syndrome in Chinese. Dig Dis Sci. 2002;47:2621–4.
Cryan JF, O’Mahony SM. The microbiome–gut–brain axis: from bowel to behavior. Neurogastroenterol Motil. 2011;23:187–92.
Fukudo S, Nomura T, Muranaka M, et al. Brain–gut response to stress and cholinergic stimulation in irritable bowel syndrome. A preliminary study. J Clin Gastroenterol. 1993;17:133–41.
Heinrichs SC, Menzaghi F, Merlo Pich E, et al. The role of CRF in behavioral aspects of stress. Ann N Y Acad Sci. 1995;771:92–104.
Owens MJ, Nemeroff CB. Physiology and pharmacology of corticotropin-releasing factor. Pharmacol Rev. 1991;43:425–73.
Turnbull AV, Rivier C. Corticotropin-releasing factor (CRF) and endocrine responses to stress: CRF receptors, binding protein, and related peptides. Proc Soc Exp Biol Med. 1997;215:1–10.
Karalis K, Sano H, Redwine J, et al. Autocrine or paracrine inflammatory actions of corticotropin-releasing hormone in vivo. Science. 1991;254:421–3.
McInturf SM, Hennessy MB. Peripheral administration of a corticotropin-releasing factor antagonist increases the vocalizing and locomotor activity of isolated guinea pig pups. Physiol Behav. 1996;60:707–10.
Schafer M, Mousa SA, Zhang Q, et al. Expression of corticotropin-releasing factor in inflamed tissue is required for intrinsic peripheral opioid analgesia. Proc Natl Acad Sci USA. 1996;93:6096–100.
Taché Y, Mönnikes H, Bonaz B, et al. Role of CRF in stress-related alterations of gastric and colonic motor function. Ann N Y Acad Sci. 1993;697:233–43.
Drossman DA, Camilleri M, Mayer EA, et al. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–31.
Lee YJ, Park KS. Irritable bowel syndrome: emerging paradigm in pathophysiology. World J Gastroenterol. 2014;20:2456–69.
Taché Y, Martínez V, Wang L, et al. CRF1 receptor signaling pathways are involved in stress-related alterations of colonic function and viscerosensitivity: implications for irritable bowel syndrome. Br J Pharmacol. 2004;141:1321–30.
Fukudo S, Nomura T, Hongo M. Impact of corticotropin-releasing hormone on gastrointestinal motility and adrenocorticotropic hormone in normal controls and patients with irritable bowel syndrome. Gut. 1998;42:845–9.
Sagami Y, Shimada Y, Tayama J, et al. Effect of a corticotropin releasing hormone receptor antagonist on colonic sensory and motor function in patients with irritable bowel syndrome. Gut. 2004;53:958–64.
Nozu T, Kudaira M. Corticotropin-releasing factor induces rectal hypersensitivity after repetitive painful rectal distention in healthy humans. J Gastroenterol. 2006;41:740–4.
Vale W, Spiess J, Rivier C, et al. Characterization of a 41-residue ovine hypothalamic peptide that stimulates secretion of corticotropin and beta-endorphin. Science. 1981;213:1394–7.
Vaughan J, Donaldson C, Bittencourt J, et al. Urocortin, a mammalian neuropeptide related to fish urotensin I and to corticotropin-releasing factor. Nature. 1995;378:287–92.
Reyes TM, Lewis K, Perrin MH, et al. Urocortin II: a member of the corticotropin-releasing factor (CRF) neuropeptide family that is selectively bound by type 2 CRF receptors. Proc Natl Acad Sci USA. 2001;98:2843–8.
Lewis K, Li C, Perrin MH, et al. Identification of urocortin III, an additional member of the corticotropin-releasing factor (CRF) family with high affinity for the CRF2 receptor. Proc Natl Acad Sci USA. 2001;98:7570–5.
Hauger RL, Grigoriadis DE, Dallman MF, et al. International Union of Pharmacology. XXXVI. Current status of the nomenclature for receptors for corticotropin-releasing factor and their ligands. Pharmacol Rev. 2003;55:21–6.
Hillhouse EW, Grammatopoulos DK. The molecular mechanisms underlying the regulation of the biological activity of corticotropin-releasing hormone receptors: implications for physiology and pathophysiology. Endocr Rev. 2006;27:260–86.
Perrin MH, Vale WW. Corticotropin releasing factor receptors and their ligand family. Ann N Y Acad Sci. 1999;885:312–28.
Blank T, Nijholt I, Grammatopoulos DK, et al. Corticotropin-releasing factor receptors couple to multiple G-proteins to activate diverse intracellular signaling pathways in mouse hippocampus: role in neuronal excitability and associative learning. J Neurosci. 2003;23:700–7.
Soares RL. Irritable bowel syndrome: a clinical review. World J Gastroenterol. 2014;20:12144–60.
Lee OY. Asian motility studies in irritable bowel syndrome. J Neurogastroenterol Motil. 2010;16:120–30.
Bonaz B, Taché Y. Water-avoidance stress-induced c-fos expression in the rat brain and stimulation of fecal output: role of corticotropin-releasing factor. Brain Res. 1994;641:21–8.
Lenz HJ, Raedler A, Greten H, et al. Stress-induced gastrointestinal secretory and motor responses in rats are mediated by endogenous corticotropin-releasing factor. Gastroenterology. 1988;95:1510–7.
Fargeas MJ, Fioramonti J, Bueno L. Central action of interleukin 1 beta on intestinal motility in rats: mediation by two mechanisms. Gastroenterology. 1993;104:377–83.
Mönnikes H, Schmidt BG, Raybould HE, et al. CRF in the paraventricular nucleus mediates gastric and colonic motor response to restraint stress. Am J Physiol Gastrointest Liver Physiol. 1992;262:G137–43.
Mönnikes H, Schmidt BG, Taché Y. Psychological stress-induced accelerated colonic transit in rats involves hypothalamic corticotropin-releasing factor. Gastroenterology. 1993;104:716–23.
Martínez V, Rivier J, Wang L, et al. Central injection of a new corticotropin-releasing factor (CRF) antagonist, astressin, blocks CRF- and stress-related alterations of gastric and colonic motor function. J Pharmacol Exp Ther. 1997;280:754–60.
Nakade Y, Fukuda H, Iwa M, et al. Restraint stress stimulates colonic motility via central corticotropin-releasing factor and peripheral 5-HT3 receptors in conscious rats. Am J Physiol Gastrointest Liver Physiol. 2007;292:G1037–44.
Lenz HJ, Burlage M, Raedler A, et al. Central nervous system effects of corticotropin-releasing factor on gastrointestinal transit in the rat. Gastroenterology. 1988;94:598–602.
Miyata K, Ito H, Fukudo S. Involvement of the 5-HT3 receptor in CRH-induce defecation in rats. Am J Physiol Gastrointest Liver Physiol. 1998;274:G827–31.
Martínez V, Wang L, Million M, et al. Urocortins and the regulation of gastrointestinal motor function and visceral pain. Peptides. 2004;25:1733–44.
Martínez V, Wang L, Rivier J, et al. Central CRF, urocortins and stress increase colonic transit via CRF1 receptors while activation of CRF2 receptors delays gastric transit in mice. J Physiol. 2004;556:221–34.
Ataka K, Kuge T, Fujino K, et al. Wood creosote prevents CRF-induced motility via 5-HT3 receptors in proximal and 5-HT4 receptors in distal colon in rats. Auton Neurosci. 2007;133:136–45.
Mönnikes H, Schmidt BG, Tebbe J, et al. Microinfusion of corticotropin releasing factor into the locus coeruleus/subcoeruleus nuclei stimulates colonic motor function in rats. Brain Res. 1994;644:101–8.
Raadsheer FC, Hoogendijk WJ, Stam FC, et al. Increased numbers of corticotropin-releasing hormone expressing neurons in the hypothalamic paraventricular nucleus of depressed patients. Neuroendocrinology. 1994;60:436–44.
Weiss JM, Stout JC, Aaron MF, et al. Depression and anxiety: role of the locus coeruleus and corticotropin-releasing factor. Brain Res Bull. 1994;35:561–72.
Arborelius L, Skelton KH, Thrivikraman KV, et al. Chronic administration of the selective corticotropin-releasing factor 1 receptor antagonist CP-154, 526: behavioral, endocrine and neurochemical effects in the rat. J Pharmacol Exp Ther. 2000;294:588–97.
Luiten PG, ter Horst GJ, Karst H, et al. The course of paraventricular hypothalamic efferents to autonomic structures in medulla and spinal cord. Brain Res. 1985;329:374–8.
Silverman AJ, Hou-Yu A, Chen WP. Corticotropin-releasing factor synapses within the paraventricular nucleus of the hypothalamus. Neuroendocrinology. 1989;49:291–9.
Berridge CW, Waterhouse BD. The locus coeruleus-noradrenergic system: modulation of behavioral state and state-dependent cognitive processes. Brain Res Brain Res Rev. 2003;42:33–84.
Butler PD, Weiss JM, Stout JC, et al. Corticotropin-releasing factor produces fear-enhancing and behavioral activating effects following infusion into the locus coeruleus. J Neurosci. 1990;10:176–83.
Koob GF. Corticotropin-releasing factor, norepinephrine, and stress. Biol Psychiatry. 1999;46:1167–80.
Garakani A, Win T, Virk S, et al. Comorbidity of irritable bowel syndrome in psychiatric patients: a review. Am J Ther. 2003;10:61–7.
American Gastroenterology Association. American Gastroenterological Association medical position statement: irritable bowel syndrome. Gastroenterology. 2002;123:2105–7.
Million M, Wang L, Martínez V, et al. Differential Fos expression in the paraventricular nucleus of the hypothalamus, sacral parasympathetic nucleus and colonic motor response to water avoidance stress in Fischer and Lewis rats. Brain Res. 2000;877:345–53.
Castagliuolo I, Lamont JT, Qiu B, et al. Acute stress causes mucin release from rat colon: role of corticotropin releasing factor and mast cells. Am J Physiol Gastrointest Liver Physiol. 1996;271:G884–92.
Williams CL, Peterson JM, Villar RG, et al. Corticotropin-releasing factor directly mediates colonic responses to stress. Am J Physiol Gastrointest Liver Physiol. 1987;253:G582–6.
Maillot C, Million M, Wei JY, et al. Peripheral corticotropin-releasing factor and stress-stimulated colonic motor activity involve type 1 receptor in rats. Gastroenterology. 2000;119:1569–79.
Kimura T, Amano T, Uehara H, et al. Urocortin I is present in the enteric nervous system and exerts an excitatory effect via cholinergic and serotonergic pathways in the rat colon. Am J Physiol Gastrointest Liver Physiol. 2007;293:G903–10.
Nozu T, Takakusaki K, Okumura T. A balance theory of peripheral corticotropin-releasing factor receptor type 1 and type 2 signaling to induce colonic contractions and visceral hyperalgesia in rats. Endocrinology. 2014;155:4655–64.
Martínez V, Wang L, Rivier JE, et al. Differential actions of peripheral corticotropin-releasing factor (CRF), urocortin II, and urocortin III on gastric emptying and colonic transit in mice: role of CRF receptor subtypes 1 and 2. J Pharmacol Exp Ther. 2002;301:611–7.
Million M, Maillot C, Saunders P, et al. Human urocortin II, a new CRF-related peptide, displays selective CRF2-mediated action on gastric transit in rats. Am J Physiol Gastrointest Liver Physiol. 2002;282:G34–40.
Larauche M, Gourcerol G, Wang L, et al. Cortagine, a CRF1 agonist, induces stresslike alterations of colonic function and visceral hypersensitivity in rodents primarily through peripheral pathways. Am J Physiol Gastrointest Liver Physiol. 2009;297:G215–27.
Gourcerol G, Wu SV, Yuan PQ, et al. Activation of corticotropin-releasing factor receptor 2 mediates the colonic motor coping response to acute stress in rodents. Gastroenterology. 2011;140:1586–96, e1–6.
Yuan PQ, Wu SV, Wang L, et al. Corticotropin releasing factor in the rat colon: expression, localization and upregulation by endotoxin. Peptides. 2010;31:322–31.
Chatzaki E, Crowe PD, Wang L, et al. CRF receptor type 1 and 2 expression and anatomical distribution in the rat colon. J Neurochem. 2004;90:309–16.
von Mentzer B, Murata Y, Ahlstedt I, et al. Functional CRF receptors in BON cells stimulate serotonin release. Biochem Pharmacol. 2007;73:805–13.
Theoharides TC, Donelan JM, Papadopoulou N, et al. Mast cells as targets of corticotropin-releasing factor and related peptides. Trends Pharmacol Sci. 2004;25:563–8.
Wallon C, Yang PC, Keita AV, et al. Corticotropin-releasing hormone (CRH) regulates macromolecular permeability via mast cells in normal human colonic biopsies in vitro. Gut. 2008;57:50–8.
Audhya T, Jain R, Hollander CS. Receptor-mediated immunomodulation by corticotropin-releasing factor. Cell Immunol. 1991;134:77–84.
Kawahito Y, Sano H, Kawata M, et al. Local secretion of corticotropin-releasing hormone by enterochromaffin cells in human colon. Gastroenterology. 1994;106:859–65.
Muramatsu Y, Fukushima K, Iino K, et al. Urocortin and corticotropin-releasing factor receptor expression in the human colonic mucosa. Peptides. 2000;21:1799–809.
Wu SV, Yuan PQ, Lai J, et al. Activation of Type 1 CRH receptor isoforms induces serotonin release from human carcinoid BON-1N cells: an enterochromaffin cell model. Endocrinology. 2011;152:126–37.
Overman EL, Rivier JE, Moeser AJ. CRF induces intestinal epithelial barrier injury via the release of mast cell proteases and TNF-alpha. PLoS One. 2012;7:e39935.
Kempuraj D, Papadopoulou NG, Lytinas M, et al. Corticotropin-releasing hormone and its structurally related urocortin are synthesized and secreted by human mast cells. Endocrinology. 2004;145:43–8.
Fukumoto S, Tatewaki M, Yamada T, et al. Short-chain fatty acids stimulate colonic transit via intraluminal 5-HT release in rats. Am J Physiol Regul Integr Comp Physiol. 2003;284:R1269–76.
Yuan PQ, Million M, Wu SV, et al. Peripheral corticotropin releasing factor (CRF) and a novel CRF1 receptor agonist, stressin1-A activate CRF1 receptor expressing cholinergic and nitrergic myenteric neurons selectively in the colon of conscious rats. Neurogastroenterol Motil. 2007;19:923–36.
Bisschops R, Vanden Berghe P, Sarnelli G, et al. CRF-induced calcium signaling in guinea pig small intestine myenteric neurons involves CRF-1 receptors and activation of voltage-sensitive calcium channels. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1252–60.
Tsukamoto K, Nakade Y, Mantyh C, et al. Peripherally administered CRF stimulates colonic motility via central CRF receptors and vagal pathways in conscious rats. Am J Physiol Regul Integr Comp Physiol. 2006;290:R1537–41.
Perrin MH, Donaldson CJ, Chen R, et al. Cloning and functional expression of a rat brain corticotropin releasing factor (CRF) receptor. Endocrinology. 1993;133:3058–61.
Wang L, Martínez V, Vale W, et al. Fos induction in selective hypothalamic neuroendocrine and medullary nuclei by intravenous injection of urocortin and corticotropin-releasing factor in rats. Brain Res. 2000;855:47–57.
Maillot C, Wang L, Million M, et al. Intraperitoneal corticotropin-releasing factor and urocortin induce Fos expression in brain and spinal autonomic nuclei and long lasting stimulation of colonic motility in rats. Brain Res. 2003;974:70–81.
Menetrey D, De Pommery J. Origins of spinal ascending pathways that reach central areas involved in visceroception and visceronociception in the rat. Eur J Neurosci. 1991;3:249–59.
Hay M, Bishop VS. Interactions of area postrema and solitary tract in the nucleus tractus solitarius. Am J Physiol Heart Circ Physiol. 1991;260:H1466–73.
Van Pett K, Viau V, Bittencourt JC, et al. Distribution of mRNAs encoding CRF receptors in brain and pituitary of rat and mouse. J Comp Neurol. 2000;428:191–212.
Mercer JG, Lawrence CB, Copeland PA. Corticotropin-releasing factor binding sites undergo axonal transport in the rat vagus nerve. J Neuroendocrinol. 1992;4:281–6.
Davis SF, Derbenev AV, Williams KW, et al. Excitatory and inhibitory local circuit input to the rat dorsal motor nucleus of the vagus originating from the nucleus tractus solitarius. Brain Res. 2004;1017:208–17.
Mertz H, Naliboff B, Munakata J, et al. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology. 1995;109:40–52.
Mayer EA, Raybould HE. Role of visceral afferent mechanisms in functional bowel disorders. Gastroenterology. 1990;99:1688–704.
van der Veek PP, Van Rood YR, Masclee AA. Symptom severity but not psychopathology predicts visceral hypersensitivity in irritable bowel syndrome. Clin Gastroenterol Hepatol. 2008;6:321–8.
Kuiken SD, Lindeboom R, Tytgat GN, et al. Relationship between symptoms and hypersensitivity to rectal distension in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2005;22:157–64.
Mayer EA, Gebhart GF. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994;107:271–93.
Posserud I, Syrous A, Lindstrom L, et al. Altered rectal perception in irritable bowel syndrome is associated with symptom severity. Gastroenterology. 2007;133:1113–23.
Prior A, Sorial E, Sun W-M, et al. Irritable bowel syndrome: differences between patients who show rectal sensitivity and those who do not. Eur J Gastroenterol Hepatol. 1993;5:343–9.
Bouin M, Plourde V, Boivin M, et al. Rectal distention testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology. 2002;122:1771–7.
Nozu T, Kudaira M, Kitamori S, et al. Repetitive rectal painful distention induces rectal hypersensitivity in patients with irritable bowel syndrome. J Gastroenterol. 2006;41:217–22.
Munakata J, Naliboff B, Harraf F, et al. Repetitive sigmoid stimulation induces rectal hyperalgesia in patients with irritable bowel syndrome. Gastroenterology. 1997;112:55–63.
Gué M, Del Rio-Lacheze C, Eutamene H, et al. Stress-induced visceral hypersensitivity to rectal distension in rats: role of CRF and mast cells. Neurogastroenterol Motil. 1997;9:271–9.
Schwetz I, McRoberts JA, Coutinho SV, et al. Corticotropin-releasing factor receptor 1 mediates acute and delayed stress-induced visceral hyperalgesia in maternally separated Long-Evans rats. Am J Physiol Gastrointest Liver Physiol. 2005;289:G704–12.
Greenwood-Van Meerveld B, Johnson AC, Cochrane S, et al. Corticotropin-releasing factor 1 receptor-mediated mechanisms inhibit colonic hypersensitivity in rats. Neurogastroenterol Motil. 2005;17:415–22.
Kosoyan HP, Grigoriadis DE, Taché Y. The CRF(1) receptor antagonist, NBI-35965, abolished the activation of locus coeruleus neurons induced by colorectal distension and intracisternal CRF in rats. Brain Res. 2005;1056:85–96.
Su J, Tanaka Y, Muratsubaki T, et al. Injection of corticotropin-releasing hormone into the amygdala aggravates visceral nociception and induces noradrenaline release in rats. Neurogastroenterol Motil. 2015;27:30–9.
Kim SH, Han JE, Hwang S, et al. The expression of corticotropin-releasing factor in the central nucleus of the amygdala, induced by colorectal distension, is attenuated by general anesthesia. J Korean Med Sci. 2010;25:1646–51.
Neugebauer V, Li W, Bird GC, et al. The amygdala and persistent pain. Neuroscientist. 2004;10:221–34.
Phelps EA, LeDoux JE. Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron. 2005;48:175–87.
De Francesco PN, Valdivia S, Cabral A, et al. Neuroanatomical and functional characterization of CRF neurons of the amygdala using a novel transgenic mouse model. Neuroscience. 2015;289C:153–65.
Gray TS, Bingaman EW. The amygdala: corticotropin-releasing factor, steroids, and stress. Crit Rev Neurobiol. 1996;10:155–68.
Kravets JL, Reyes BA, Unterwald EM, et al. Direct targeting of peptidergic amygdalar neurons by noradrenergic afferents: linking stress-integrative circuitry. Brain Struct Funct. 2015;220:541–58.
Berridge CW. Noradrenergic modulation of arousal. Brain Res Rev. 2008;58:1–17.
Coutinho SV, Plotsky PM, Sablad M, et al. Neonatal maternal separation alters stress-induced responses to viscerosomatic nociceptive stimuli in rat. Am J Physiol Gastrointest Liver Physiol. 2002;282:G307–16.
Nemeroff CB. Neurobiological consequences of childhood trauma. J Clin Psychiatry. 2004;65(Suppl 1):18–28.
Ladd CO, Thrivikraman KV, Huot RL, et al. Differential neuroendocrine responses to chronic variable stress in adult Long Evans rats exposed to handling-maternal separation as neonates. Psychoneuroendocrinology. 2005;30:520–33.
Francis DD, Caldji C, Champagne F, et al. The role of corticotropin-releasing factor—norepinephrine systems in mediating the effects of early experience on the development of behavioral and endocrine responses to stress. Biol Psychiatry. 1999;46:1153–66.
Kalinichev M, Easterling KW, Plotsky PM, et al. Long-lasting changes in stress-induced corticosterone response and anxiety-like behaviors as a consequence of neonatal maternal separation in Long-Evans rats. Pharmacol Biochem Behav. 2002;73:131–40.
Larauche M, Bradesi S, Million M, et al. Corticotropin-releasing factor type 1 receptors mediate the visceral hyperalgesia induced by repeated psychological stress in rats. Am J Physiol Gastrointest Liver Physiol. 2008;294:G1033–40.
Million M, Wang L, Wang Y, et al. CRF2 receptor activation prevents colorectal distension induced visceral pain and spinal ERK1/2 phosphorylation in rats. Gut. 2006;55:172–81.
Mawe GM, Coates MD, Moses PL. Review article: intestinal serotonin signalling in irritable bowel syndrome. Aliment Pharmacol Ther. 2006;23:1067–76.
van den Wijngaard RM, Klooker TK, de Jonge WJ, et al. Peripheral relays in stress-induced activation of visceral afferents in the gut. Auton Neurosci. 2010;153:99–105.
Barbara G, Wang B, Stanghellini V, et al. Mast cell-dependent excitation of visceral-nociceptive sensory neurons in irritable bowel syndrome. Gastroenterology. 2007;132:26–37.
Cremon C, Carini G, Wang B, et al. Intestinal serotonin release, sensory neuron activation, and abdominal pain in irritable bowel syndrome. Am J Gastroenterol. 2011;106:1290–8.
Ait-Belgnaoui A, Bradesi S, Fioramonti J, et al. Acute stress-induced hypersensitivity to colonic distension depends upon increase in paracellular permeability: role of myosin light chain kinase. Pain. 2005;113:141–7.
Nakade Y, Tsuchida D, Fukuda H, et al. Restraint stress augments postprandial gastric contractions but impairs antropyloric coordination in conscious rats. Am J Physiol Regul Integr Comp Physiol. 2006;290:R616–24.
Million M, Maillot C, Adelson DA, et al. Peripheral injection of sauvagine prevents repeated colorectal distension-induced visceral pain in female rats. Peptides. 2005;26:1188–95.
Chrousos GP. Stress and disorders of the stress system. Nat Rev Endocrinol. 2009;5:374–81.
Nozu T, Tsuchiya Y, Kumei S, et al. Peripheral corticotropin-releasing factor (CRF) induces stimulation of gastric contractions in freely moving conscious rats: role of CRF receptor types 1 and 2. Neurogastroenterol Motil. 2013;25:190–7.
O’malley D, Julio-Pieper M, Gibney SM, et al. Differential stress-induced alterations of colonic corticotropin-releasing factor receptors in the Wistar Kyoto rat. Neurogastroenterol Motil. 2010;22:301–11.
Liu S, Ren W, Qu MH, et al. Differential actions of urocortins on neurons of the myenteric division of the enteric nervous system in guinea pig distal colon. Br J Pharmacol. 2010;159:222–36.
Posserud I, Agerforz P, Ekman R, et al. Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. Gut. 2004;53:1102–8.
Fukudo S, Kanazawa M, Kano M, et al. Exaggerated motility of the descending colon with repetitive distention of the sigmoid colon in patients with irritable bowel syndrome. J Gastroenterol. 2002;37(Suppl 14):145–50.
Fukudo S, Suzuki J. Colonic motility, autonomic function, and gastrointestinal hormones under psychological stress on irritable bowel syndrome. Tohoku J Exp Med. 1987;151:373–85.
Tanaka Y, Kanazawa M, Fukudo S, et al. Biopsychosocial model of irritable bowel syndrome. J Neurogastroenterol Motil. 2011;17:131–9.
Rittenhouse PA, Lopez-Rubalcava C, Stanwood GD, et al. Amplified behavioral and endocrine responses to forced swim stress in the Wistar-Kyoto rat. Psychoneuroendocrinology. 2002;27:303–18.
Gunter WD, Shepard JD, Foreman RD, et al. Evidence for visceral hypersensitivity in high-anxiety rats. Physiol Behav. 2000;69:379–82.
Courvoisier H, Moisan MP, Sarrieau A, et al. Behavioral and neuroendocrine reactivity to stress in the WKHA/WKY inbred rat strains: a multifactorial and genetic analysis. Brain Res. 1996;743:77–85.
Sato N, Suzuki N, Sasaki A, et al. Corticotropin-releasing hormone receptor 1 gene variants in irritable bowel syndrome. PLoS One. 2012;7:e42450.
Hsu DT, Mickey BJ, Langenecker SA, et al. Variation in the corticotropin-releasing hormone receptor 1 (CRHR1) gene influences fMRI signal responses during emotional stimulus processing. J Neurosci. 2012;32:3253–60.
Markovic D, Grammatopoulos DK. Focus on the splicing of secretin GPCRs transmembrane-domain 7. Trends Biochem Sci. 2009;34:443–52.
Sweetser S, Camilleri M, Linker Nord SJ, et al. Do corticotropin releasing factor-1 receptors influence colonic transit and bowel function in women with irritable bowel syndrome? Am J Physiol Gastrointest Liver Physiol. 2009;296:G1299–306.
Suda T, Kageyama K, Sakihara S, et al. Physiological roles of urocortins, human homologues of fish urotensin I, and their receptors. Peptides. 2004;25:1689–701.
Nozu T, Martínez V, Rivier J, et al. Peripheral urocortin delays gastric emptying: role of CRF receptor 2. Am J Physiol Gastrointest Liver Physiol. 1999;276:G867–74.
Barbara G, Zecchi L, Barbaro R, et al. Mucosal permeability and immune activation as potential therapeutic targets of probiotics in irritable bowel syndrome. J Clin Gastroenterol. 2012;46(Suppl):S52–5.
Kassinen A, Krogius-Kurikka L, Makivuokko H, et al. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology. 2007;133:24–33.
Chadwick VS, Chen W, Shu D, et al. Activation of the mucosal immune system in irritable bowel syndrome. Gastroenterology. 2002;122:1778–83.
Labus JS, Dinov ID, Jiang Z, et al. Irritable bowel syndrome in female patients is associated with alterations in structural brain networks. Pain. 2014;155:137–49.
Larauche M, Kiank C, Taché Y. Corticotropin releasing factor signaling in colon and ileum: regulation by stress and pathophysiological implications. J Physiol Pharmacol. 2009;60(Suppl 7):33–46.
Mayer EA, Savidge T, Shulman RJ. Brain–gut microbiome interactions and functional bowel disorders. Gastroenterology. 2014;146:1500–12.
Labus JS, Hubbard CS, Bueller J, et al. Impaired emotional learning and involvement of the corticotropin-releasing factor signaling system in patients with irritable bowel syndrome. Gastroenterology. 2013;145:1253–61, e1–3.
Acknowledgments
Work in the authors’ laboratory was supported by a Grant-in-Aid for Scientific Research from the Japanese Ministry of Education, Culture, Sports, Science, and Technology.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nozu, T., Okumura, T. Corticotropin-releasing factor receptor type 1 and type 2 interaction in irritable bowel syndrome. J Gastroenterol 50, 819–830 (2015). https://doi.org/10.1007/s00535-015-1086-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-015-1086-8