Abstract
Background
The significance of gastric xanthelasma in relation to gastric cancer still remains unclear. We investigated whether gastric xanthelasma would be a useful marker for predicting the development of early gastric cancer.
Methods
A total of 1823 patients who underwent a medical health checkup were enrolled. We examined the relationship between gastric xanthelasma and various clinical features, and in an endoscopic follow-up study investigated whether the presence of gastric xanthelasma was predictive of the development of early gastric cancer.
Results
In the initial endoscopic examination, gastric xanthelasma was detected in 107 (5.9 %) of the 1823 patients. The presence of gastric xanthelasma was significantly associated with age ≥65 years, male gender, open-type atrophy, and the presence of diabetes mellitus (DM) (p < 0.0001, p < 0.0001, p < 0.0001, and p < 0.0001, respectively). During the endoscopic follow-up period, early gastric cancer was found in 29 (1.6 %) of the 1823 patients. Gastric cancer occurred in 15 (14.0 %) of 107 patients with gastric xanthelasma, whereas it occurred in 14 (0.8 %) of 1716 patients without (p < 0.0001). Multivariate analysis revealed that open-type atrophy and gastric xanthelasma were independently related to the development of gastric cancer (odds ratio 7.19 [2.50–20.83]; p = 0.0003 and 5.85 [2.67–12.82]; p < 0.0001, respectively). The presence of gastric xanthelasma was significantly predictive of gastric cancer development even in the selected high-risk groups with open-type atrophy or DM (p < 0.0001 or p < 0.0001, respectively).
Conclusions
Gastric xanthelasma is a useful marker for predicting the development of gastric cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is one of the leading causes of cancer-related deaths worldwide [1, 2], mostly arising in gastric mucosa that has been infected with Helicobacter pylori (H. pylori) [3, 4]. For curative treatment of gastric cancer, early detection is essential. In this context, endoscopic surveillance examinations are an important strategy for reducing the risk of mortality due to gastric cancer. Although it seems impractical to survey all patients with H. pylori infection worldwide, not all such patients will necessarily develop gastric cancer during their lifetimes. Therefore, to improve the efficacy of such endoscopic surveillance, a useful predictive marker for development of gastric cancer is urgently needed.
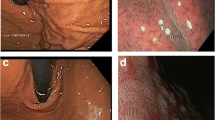
Gastric atrophy, which reflects chronic gastritis induced by H. pylori infection, is considered to be an important risk factor for gastric cancer [5–8], and accumulating evidence suggests that the severity of gastric atrophy is related to the incidence of early gastric cancer [9–11]. However, for more precise delineation of individuals who have a high risk of developing gastric cancer, additional markers are needed for detailed surveillance of patients with gastric atrophy. We and others have recently shown that diabetes mellitus (DM) is associated with an increased incidence of gastric cancer, suggesting that DM plays some role in gastric carcinogenesis [12–16]. Moreover, we have reported that gastric xanthelasma, characterized by the accumulation of lipid in histiocytic foam cells, is frequently observed in the gastric mucosa of patients with early gastric cancer [17], suggesting that gastric xanthelasma might be applicable as a predictive biomarker. In the present study, we therefore analyzed the relationship between gastric xanthelasma and clinical features of patients, including the level of serum lipid and glucose, and furthermore investigated whether, in addition to gastric atrophy, gastric xanthelasma would be a useful marker for predicting the development of gastric cancer.
Materials and methods
Patients
This study was based on historical cohort analysis of patients who underwent medical health checkups between January 2004 and December 2012 at Osaka Red Cross Hospital. Medical checkup means periodic health evaluation involving a medical history, a physical examination, laboratory tests, and endoscopic examination of the upper gastrointestinal tract without insurance coverage. For inclusion in this study, patients had to have: (i) undergone follow-up endoscopic examination of the upper gastrointestinal tract, (ii) been followed up for longer than 3 years, and (iii) had neither prior gastrectomy nor gastric cancer. Finally, a total of 1823 patients were enrolled as shown in Fig. 1. The following factors were examined retrospectively: age, sex, severity of gastric atrophy, presence of gastric xanthelasma, serum total cholesterol (T-CHO), triglyceride (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL), fasting plasma glucose (FPG), and the presence of DM. The presence of DM was determined on the basis of medical history, the result of a 75-g oral glucose tolerance test, the fasting plasma glucose (FPG) level (>126 mg/dl), or the hemoglobin A1c (HbA1c) level (≥6.5 %), as reported previously [12, 18]. Each patient underwent annual endoscopic evaluations of the upper gastrointestinal tract and was examined for the presence or absence of gastric cancer during the follow-up period. The diagnosis of gastric cancer was confirmed by histologic examination of tissue obtained by endoscopic submucosal dissection or surgical resection. This study was carried out with the approval of the Osaka Red Cross Hospital Ethics Committee, and informed consent was obtained from all patients.
Endoscopic examination and evaluation of gastric atrophy
We performed endoscopic examination of the upper gastrointestinal tract using a panendoscope (GIF-Q260, GIF-H260, or GIF-HQ290; Olympus Medical Systems, Tokyo, Japan) equipped with an electronic endoscopy system (EVIS LUCERA system; Olympus Medical Systems). Each examination was performed by an experienced endoscopist, who carefully observed the esophagus, the entire stomach, and the bulbar portion of the duodenum.
The severity of gastric atrophy was evaluated and classified according to the criteria of Kimura and Takemoto, as reported previously [19, 20]. In brief, the severity of atrophy was divided into the following types according to the location of the borderline between the fundic and pyloric gland regions: antral-type, borderline located in the angular part of the lesser curvature; closed-type, borderline located on the lesser curvature of the stomach; open-type, entire aspect of the lesser curvature was pyloric in nature, and the border was shifted orally.
Statistical analysis
The StatView 5.0J statistical software package (Abacus Concepts Inc., Berkeley, CA, USA) was used for all analyses in the present study. Data for age, T-CHO, TG, HDL, LDL, FPG, and HbA1c were expressed as the mean ± SEM. Differences in these values between two groups were analyzed by unpaired two-tailed t test or by Mann–Whitney U test when the data were not parametric. Chi-squared analyses were performed to investigate the relationships between groups and the various clinical factors, and Fisher’s exact test was also used as necessary. Multivariate stepwise logistic analysis was used to identify factors that were related to the development of gastric cancer. Cumulative incidence of gastric cancer was evaluated by the Kaplan–Meier method and analyzed by log-rank test. Multivariate Cox regression analyses were used to examine whether gastric xanthelasma was an independent predictor for the development of gastric cancer. Differences at p < 0.05 were considered to be statistically significant.
Results
Analysis of the factors related to the development of gastric cancer
The clinical features of the patients enrolled in this study are summarized in Table 1. A total of 1823 patients underwent endoscopic examination and follow-up studies. The follow-up period ranged from 36 to 108 (median 63.0) months. During the follow-up period, early gastric cancer was found in 29 (1.6 %) of the 1823 patients.
We first examined the factors related to the development of gastric cancer. Univariate analysis indicated that gastric cancer development was significantly related to age ≥65 years, male, gastric atrophy, and the presence of gastric xanthelasma (Table 1). None of the other parameters, including gastric ulcer, duodenal ulcer, reflux esophagitis, and fundic gland polyp, were significantly correlated with the development of gastric cancer. Multivariate analysis revealed that gastric atrophy and the presence of gastric xanthelasma were independently related to the development of gastric cancer (Table 2).
Regarding H. pylori status, we obtained its related data in only 236 patients at the start of endoscopic follow-up. When we analyzed these patients in terms of gastric cancer development, univariate analysis showed that age ≥65 years, male, gastric atrophy, the presence of gastric xanthelasma, and H. pylori infection were significantly related to the development of gastric cancer (Supplementary Table 1). Moreover, multivariate analysis revealed that the presence of gastric xanthelasma was independently related to the development of gastric cancer (Supplementary Table 2).
Gastric xanthelasma is related to age, sex, gastric atrophy, and the presence of DM
In the initial endoscopic examination, gastric xanthelasma was detected in 107 (5.9 %) of the 1823 patients. The patients were then divided into two groups based on the presence of gastric xanthelasma, and differences between these two groups were examined. Patients with gastric xanthelasma were significantly older than those without (62.7 ± 0.8 vs. 53.1 ± 0.3, p < 0.0001). The proportion of males was significantly higher in patients with gastric xanthelasma than in those without (75.7 vs. 56.5 %, p < 0.0001). Moreover, a significantly higher proportion of patients with gastric xanthelasma had open-type atrophy in comparison to patients without (77.6 vs. 19.2 %, p < 0.0001). None of the serum lipids, including the levels of T-CHO, TG, HDL, and LDL, were significantly related to the presence of gastric xanthelasma. Interestingly, the level of FPG was significantly higher in patients with gastric xanthelasma than in those without (107.3 ± 2.5 vs. 99.8 ± 0.4, p = 0.0002). Similarly, the level of HbA1c was significantly higher in patients with gastric xanthelasma than in those without (5.88 ± 0.07 vs. 5.68 ± 0.02, p = 0.0003). Moreover, the proportion patients with DM was significantly higher in those with gastric xanthelasma than in those without (22.4 vs. 9.1 %, p < 0.0001, Table 3).
The presence of gastric xanthelasma is associated with the development of early gastric cancer
During the follow-up period, early gastric cancer was found in 29 (1.6 %) of the 1823 patients, including 15 (14.0 %) of the 107 patients with xanthelasma and 14 (0.8 %) of the 1716 patients without. Kaplan–Meir curves clearly showed that significantly more patients with gastric xanthelasma developed early gastric cancer than those without (p < 0.0001, Fig. 2).
We next examined whether the presence of gastric xanthelasma was an independent factor predictive of early gastric cancer development. Univariate analysis showed that age ≥65 years, male gender, open-type atrophy, gastric xanthelasma, and DM were significantly related to the development of early gastric cancer (Table 4). Multivariate analysis revealed that open-type atrophy and the presence of gastric xanthelasma were independently related to the development of gastric cancer (Table 4).
Of the 29 gastric cancers developed, 26 were differentiated type and three were undifferentiated ones. Interestingly, gastric xanthelasma was detected in 15 of 26 patients with differentiated gastric cancer, whereas it was detected in none of three patients with undifferentiated gastric cancer.
The presence of gastric xanthelasma predicts the development of gastric cancer in patients with open-type gastric atrophy
As shown in Table 4, patients with open-type gastric atrophy had an increased risk for the development of gastric cancer. We then investigated the impact of gastric xanthelasma on the development of early gastric cancer in patients with open-type gastric atrophy. We divided these patients into two groups according to the presence of gastric xanthelasma and investigated the inter-group difference in the incidence of early gastric cancer. Gastric xanthelasma was detected in 83 (20.1 %) of 412 patients with open-type gastric atrophy, and during the follow-up period, 15 (18.1 %) of those 83 patients developed gastric cancer, whereas only nine (2.7 %) of the 329 patients without did so. Kaplan–Meier curves for patients with open-type gastric atrophy showed that those with gastric xanthelasma had a significantly higher incidence of gastric cancer than those without (p < 0.0001, Fig. 3).
Moreover, we compared cumulative incidence of gastric cancer between gastric xanthelasma-positive and -negative cases in 138 patients with H. pylori infection. Kaplan–Meier curves for patients with H. pylori infection showed that those with gastric xanthelasma had a significantly higher incidence of gastric cancer than those without (p < 0.0001, Supplementary Figure 1).
Gastric xanthelasma is associated with the development of gastric cancer in patients with DM
We next investigated the impact of gastric xanthelasma on the development of gastric cancer in patients with DM, who constitute a high-risk group for this type of cancer. Gastric xanthelasma was observed in 24 (13.3 %) of the 181 patients with DM, whereas it was detected in 83 (5.1 %) of the 1642 patients without DM. We divided the DM patients into two groups according to the presence of gastric xanthelasma and examined the inter-group difference in the development of gastric cancer. During the follow-up period, early gastric cancer occurred in six (25 %) of the 24 DM patients with xanthelasma, whereas it was identified in only two (1.3 %) of the 157 without. The Kaplan–Meier curves for DM patients showed that those with gastric xanthelasma had a significantly higher incidence of gastric cancer than those without (p < 0.0001, Fig. 4).
Discussion
Gastric xanthelasma has received little attention, perhaps because clinically it has been considered a benign entity. The present study is the first to have investigated the significance of gastric xanthelasma as a marker for predicting the development of early gastric cancer. Although gastric xanthelasma is characterized by an accumulation of lipids in histiocytic foam cells, its presence showed no relationship to serum lipid levels; notably, however, it was significantly associated with DM. On the other hand, since xanthelasma is thought to be the result of an inflammatory response to mucosal damage or aging, it may not be surprising that the presence of gastric xanthelasma was strongly associated with age and the severity of gastric atrophy. Interestingly, these factors related to gastric xanthelasma are known to be risk factors for the development of gastric cancer [21–23], and therefore we further investigated the clinicopathological significance of gastric xanthelasma in this context.
We have previously reported that the incidence of gastric xanthelasma is significantly higher in patients with gastric cancer [16]. Moreover, in the present study employing endoscopic follow-up examination, we clarified that the occurrence of early gastric cancer was significantly higher in patients with gastric xanthelasma than in those without. These findings strongly suggest that gastric xanthelasma is a predictive marker for the development of gastric cancer. However, univariate analysis showed that not only gastric xanthelasma but also DM, gastric atrophy, and other factors were associated with the occurrence of gastric cancer, and multivariate analysis confirmed gastric xanthelasma to be an independently predictive marker for gastric cancer development.
Why does gastric cancer develop more frequently in patients with gastric xanthelasma than in those without? Kaiser et al. have reported that increased release of oxygen free radicals may be involved in the formation of gastric xanthelasma [24]. Oxygen free radicals are well known to cause DNA damage and to play a role in the pathophysiology of various malignancies [25–28]. Accordingly, it is tempting to speculate that oxygen free radicals may play a role in gastric carcinogenesis in patients with gastric xanthelasma. On the other hand, it is possible that the presence of gastric xanthelasma may reflect the severity and long duration of chronic gastritis, and in fact gastric xanthelasma was frequently observed in patients with open-type gastric atrophy, which is known to be an important risk factor for the development of gastric cancer development. We also found that gastric xanthelasma was associated with the presence of DM. Accumulating evidence suggests that DM plays some roles in gastric carcinogenesis via hyperglycemia or hyperinsulinemia [12, 29, 30]. Previous reports suggest that production of reactive oxygen species is increased in hyperglycemia [31, 32]. At present, we cannot explain why gastric xanthelasma was associated with DM. However, it is tempting to speculate that excessive production of free radicals in hyperglycemia may be involved in the development of gastric xanthelasma in patients with DM. Although it remains unclear why patients with gastric xanthelasma show a higher prevalence of gastric cancer, it seems likely that DM as well as gastric atrophy is at least in part involved in gastric carcinogenesis.
Although both open-type gastric atrophy and DM are likely to be important risk factors for gastric cancer [9–16], only a small proportion of patients with these conditions develop gastric cancer, and the majority do not. Therefore, we investigated whether gastric xanthelasma could be used as a predictive marker for gastric cancer development in high-risk patients with DM or open-type atrophy. As shown in Figs. 3 and 4, the presence of gastric xanthelasma was significantly predictive of early gastric cancer in not only patients with DM but also those with open-type atrophy. These findings suggest that gastric xanthelasma would be a very useful marker for more precise delineation of higher-risk patients among those who already have a high risk of gastric cancer. In the present study, early gastric cancer occurred in 15 (14 %) of 107 patients with gastric xanthelasma. Interestingly, we found that gastric cancer occurred in the same location of xanthelasma in 12 (80 %) of 15 cases. These findings may suggest that gastric xanthelasma is a marker not only for predicting the development of early gastric cancer but also for predicting its location. However, since the number of gastric cancer patients with xanthelasma examined was small in this study, further studies will be required to confirm this finding. In addition, our study has some limitations. It was based on a historical cohort analysis at a single institution. Since the follow-up rate was low, the present study might have a certain degree of selection bias. Moreover, we had no complete data pertaining to H. pylori infection, and the lack of information for H. pylori eradication is also a limitation in this study. Therefore, multicenter prospective analysis including such data will be needed to clarify the value of this study.
In conclusion, we have clarified that the incidence of gastric xanthelasma is significantly higher in patients with open-type gastric atrophy or DM. Moreover, we showed that the presence of gastric xanthelasma was independently predictive of early gastric cancer in both patients overall and also high-risk patients with open-type gastric atrophy or DM. These findings suggest that gastric xanthelasma is a simple but very effective marker in patients undergoing endoscopic surveillance for development of gastric cancer.
References
Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24:2137–50.
Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–917.
Matsuo T, Ito M, Takata S, et al. Low prevalence of Helicobacter pylori-negative gastric cancer among Japanese. Helicobacter. 2011;16:415–9.
Ono S, Kato M, Suzuki M, et al. Frequency of Helicobacter pylori-negative gastric cancer and gastric mucosal atrophy in a Japanese endoscopic submucosal dissection series including histological, endoscopic and serological atrophy. Digestion. 2012;86:59–65.
Parsonnet J, Friedman GD, Vandersteen DP, et al. Helicobacter Pylori infection and risk of gastric carcinoma. N Engl J Med. 1991;325:1127–31.
Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter Pylori infection and the development of gastric cancer. N Engl J Med. 2001;345:784–9.
Yamaji Y, Mitsushima T, ikuma H, et al. Inverse background of Helicobacter pylori antibody and pepsinogen in reflux oesophagitis compared with gastric cancer: analysis 5732 Japanese subjects. Gut 2001;49:335-340.
De Vries AC, van Grieken NC, Looman CW, et al. Gastric cancer risk in patients with premalignancy lesions: a nationwide cohort study in the Netherlands. Gastroenterology. 2008;134:945–52.
Take S, Mizuo M, Ishiki K, et al. Baseline gastric mucosal atrophy is a risk factor associated with the development of gastric cancer after Helicobacter pylori eradication therapy in patients with peptic ulcer disease. J Gastroenterol. 2007;42:21–7.
Kitahara F, Shimazaki R, Sato T, et al. Severe atrophic gastritis with Helicobacter pylori infection and gastric cancer. Gastric Cancer. 1998;1:118–24.
Ohata H, Kitauchi S, Yoshimura N, et al. Progression of chronic atrophic gastritis associated with Helicobacter pylori infection increases risk of gastric cancer. Int J Cancer. 2004;109:138–43.
Ikeda F, Doi Y, Yonemoto K, et al. Hyperglycemia increases risk of gastric cancer posed by Helicobacter pylori infection: a population-based cohort study. Gastroenterology 2009;136:1234-1241.
Tian T, Zhang LQ, Ma XH, et al. Diabetes mellitus and incidence and mortality of gastric cancer: a meta-analysis. Exp Clin Endocrinol Diabetes. 2012;120:217–23.
Yoon JM, Son KY, Eom CS, et al. Pre-existing diabetes mellitus increases the risk of gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19:936–45.
Shimoyama S. Diabetes mellitus carries a risk of gastric cancer: a meta-analysis. World J Gastroenterol. 2013;19:6902–10.
Sekikawa A, Fukui H, Maruo T, et al. Diabetes mellitus increases the risk of early gastric cancer development. Eur J Cancer. 2014;50:2065–71.
Sekikawa A, Fukui H, Maruo T, et al. Gastric xanthelasma may be a warning sign for the presence of early gastric cancer. J Gastroenterol Hepatol. 2014;29:951–6.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diab Care. 2010;33(Suppl 1):S62–9.
Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;1:87–97.
Kitahara F, Kobayashi K, Sato T, et al. Accuracy of screening for gastric cancer using serum pepsinogen concentration. Gut. 1999;44:693–7.
Shipponen P, Kekki M, Siurala M. Increase risk of gastric cancer in males affects the intestinal type of cancer and is independent of age, location of the tumour and atrophic gastritis. Br J Cancer. 1988;57:332–6.
Tatsuta M, Iishi H, Nakaizumi A, et al. Fundal atrophic gastritis as a risk factor for gastric cancer. Int J Cancer. 1993;53:70–4.
Watabe H, Mitsushima T, Yamaji Y, et al. Predicting the development of gastric cancer from combining Helicobacter pylori antibodies and serum pepsinogen status: a prospective endoscopic cohort study. Gut. 2005;54:764–8.
Kaiserling E, Heine H, Itabe H, et al. Lipid islands in human gastric mucosa: morphological and immunohistochemical findings. Gastroenterology. 1996;110:369–74.
Farinati F, Cardin R, Dagan P, et al. Oxidative DNA damage accumulation in gastric carcinogenesis. Gut. 1998;42:351–6.
Kountouras J, Chatzopoulos D, Zavos C. Reactive oxygen metabolites and upper gastrointestinal diseases. Hepatogastroenterology. 2001;48:743–51.
Leufkens AM, van Duijnhoven FJ, Woudt SH, et al. Biomarkers of oxidative stress and risk of developing colorectal cancer: a cohort-nested case-control study in the European Prospective Investigation Into Cancer and Nutrition. Am J Epidemiol. 2012;175:653–63.
Cardin R, Piciocchi M, Bortolami M, et al. Oxidative damage in the progression of chronic liver disease to hepatocellular carcinoma: an intricate pathway. World J Gastroenterol. 2014;20:3078–86.
Shikata K, Ninomiya T, Kiyohara Y. Diabetes mellitus and cancer risk: review of the epidemiological evidence. Cancer Sci. 2013;104:9–14.
Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R. Diabetes and cancer. Endocr Relat Cancer. 2009;16:1103–23.
Lorenzi M, Montisano DF, Toledo S, Barrieux A. High glucose induced DNA damage in cultured human epithelial cells. J Clin Invest. 1986;77:322–5.
Dondona P, Thusu K, Cook S, et al. Oxidative damage to DNA in diabetes mellitus. Lancet. 1996;347:444–5.
Conflict of interest
The authors declare that they have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
535_2015_1081_MOESM3_ESM.tif
Supplementary Figure 1. Cumulative incidence of early gastric cancer in patients with H. pylori infection (TIFF 13522 kb)
Rights and permissions
About this article
Cite this article
Sekikawa, A., Fukui, H., Sada, R. et al. Gastric atrophy and xanthelasma are markers for predicting the development of early gastric cancer. J Gastroenterol 51, 35–42 (2016). https://doi.org/10.1007/s00535-015-1081-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-015-1081-0