Abstract
Introduction
Bones are frequent sites of metastatic disease, observed in 30–75% of advanced cancer patients. Quality of life (QoL) is an important endpoint in studies evaluating the treatments of bone metastases (BM), and many patient-reported outcome tools are available. The primary objective of this systematic review was to compile a list of QoL issues relevant to BM and its interventions. The secondary objective was to identify common tools used to assess QoL in patients with BM, and the QoL issues they fail to address.
Methods
A search was conducted on Ovid MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials databases between 1946 and 27 January 2023 with the keywords “bone metastases”, “quality of life”, and “patient reported outcomes”. Specific QoL issues in original research studies and the QoL tools used were extracted.
Results
The review identified the QoL issues most prevalent to BM in the literature. Physical and functional issues observed in patients included pain, interference with ambulation and daily activities, and fatigue. Psychological symptoms, such as helplessness, depression, and anxiety were also common. These issues interfered with patients’ relationships and social activities. Items not mentioned in existing QoL tools were related to newer treatments of BM, such as pain flare, flu-like symptoms, and jaw pain due to osteonecrosis.
Conclusions
This systematic review highlights that QoL issues for patients with BM have expanded over time due to advances in BM-directed treatments. If they are relevant, additional treatment-related QoL issues identified need to be validated prospectively by patients and added to current assessment tools.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bones are frequent metastatic sites in advanced malignancies. Bone metastases (BM) are observed in around 30 to 75% of patients and have a post-mortem incidence of up to 70% in patients with prostate and breast primaries [1, 2]. Many patients with BM will experience skeletal-related events (SREs), such as pathological fractures, bone pain, hypercalcemia, and spinal cord compression [3, 4]. These result in a wide variety of physical, functional, and psychosocial issues, which significantly affect patients’ quality of life (QoL) [5].
Surgery and radiotherapy have been used to treat patients with BM for decades. Now, with advances in medical treatments, significant changes in the treatments available for BM have further reached the aims of relieving symptoms, suppressing tumour growth, and in turn, prolonging the survival of patients [6]. There is an increase in the number of novel palliative treatment options such as radiopharmaceuticals, stereotactic body radiation therapy, percutaneous vertebroplasty, thermal ablation, cryotherapy, electrochemotherapy, high-intensity focused ultrasound, and cementoplasty [6]. Several modalities are currently undergoing further investigation to determine efficacy in minimizing the burden of BM across patient groups [7]. These treatments have shown clinical benefits but may lead to adverse side effects such as worsening pain, nausea, constipation, vomiting, and fatigue [6]. Specific complications such as osteonecrosis of the jaw from bone modifying agents (BMAs) could also be a concern for patients with BM [3, 6]. To provide more comprehensive care for patients with BM, it is important to recognize the health related QoL issues that they face. The primary objective of this systematic review was to identify the QoL issues faced by patients with BM related to the disease or its treatment. The secondary objectives were to comprehensively survey the patient-reported outcome measures (PROMs) that have been used to assess patients with BM and evaluate whether the QoL issues identified are adequately captured by these assessment scales.
Methods
This systematic review was prepared using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [8].
Search strategy
A literature search was conducted on 27 January 2023 in the following databases: Ovid MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials (CENTRAL). These databases were searched between 1946 and 27 January 2023 using keywords relating to BM and QoL, such as “bone neoplasms,” “quality of life,” and “patient reported outcome measures” (Appendix 1). The search was limited to studies written in English about adult human populations.
Article selection
Results were screened using the Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia (available at http://www.covidence.org). This collaborative web-based platform streamlines the production of systematic and other literature reviews [9]. Records were independently screened by two authors (TR, HCYW) by title and abstract according to the eligibility criteria. Potential articles were further assessed through full-text screening. Conflicts were resolved by discussion between authors or consultation with a third author (EZ). Studies were included if they (1) discussed patients with BM and (2) reported original data on QoL issues or toxicities in patients. Quantitative and qualitative data about patients with BM from prospective and retrospective studies were included. QoL issues were defined as any symptom or consequence of the patients’ disease, no matter the domains of their life it impacted. Studies were excluded if they (1) did not differentiate patients with BM, (2) did not assess or mention QoL, or if they (3) did not report original data on QoL issues or toxicities in patients.
Data collection and analysis
From the included studies, the following data were extracted: title, year of publication, first author, assessment methods, study design, total participants, primary cancer site, PROM used, and QoL issues specific to patients with BM. An exhaustive list of relevant QoL issues faced by patients with BM was compiled. These issues were extracted if they were explicitly mentioned by BM patients in the study. Issues that were assessed by the PROMs used in the study were not extracted, but rather the PROM used was extracted. Treatment related QoL issues were also extracted separately from the articles and categorized by the modality of treatment. The frequency of issues explicitly mentioned and treatment-related issues was calculated.
Results
Literature search
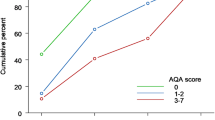
In this literature search, 6195 studies were identified through Ovid MEDLINE (n = 1827), EMBASE (n = 3350), and Cochrane Central Register of Controlled Trials (CENTRAL) (n = 1018). After duplicates were removed, 4840 studies remained for abstract and full-text screening. Of these studies, 588 met the inclusion criteria and were included in this review (Fig. 1) (Appendix 2). The most common primary cancer sites included breast, prostate, lung, skin (melanoma), and gastrointestinal. The most common treatments were radiotherapy, radionuclides, and BMAs.
Study characteristics
The search identified 588 primary research studies (Table 1). Of these studies, 333 were prospective studies and used surveys and questionnaires to quantify QoL issues. This included 89 randomized control trials (RCTs), 33 cohort studies, 14 studies on the validation or development of new questionnaires, 11 clinical trials, 11 cross-sectional studies, five pilot studies, four comparative studies, and three descriptive studies. There were also 123 retrospective reviews of prospective data, 120 case reports, and five case series. There were seven qualitative studies that used patient interviews to identify symptoms. These studies had a mean of 190 patients and a median of 42, with a range of 1 to 5500.
BM-related QoL issues
This systematic review identified three main domains of BM-related QoL issues: (1) physical, (2) psychosocial, and (3) functional. The relative number of papers that explicitly report each symptom is presented in Table 2, not including those mentioned in PROMs. The frequency by which these issues were reported in the literature was recorded, and a few selected studies with the largest and/or the most representative patient populations are discussed.
Physical issues
Physical issues: pain
Among the physical QoL issues, pain was the most frequently reported, and studies often singularly focused on pain severity among patients with BM. A qualitative study by Coward and Wilkie found that pain was not only “distressing” for patients but impacted their QoL beyond just the physical domain [10]. The site and nature of the pain varied depending on the metastatic site of BM. Back, hip, and limb were the most common pain sites among patients with BM [11, 12]. In a retrospective study by Bongiovanni et al. involving over 2000 patients, around 60% reported pain, and its nature was described as “nociceptive”, “neuropathic”, or a mixture of the two [13]. Pain was also described as “breakthrough,” “intermittent,” or “constant” by patients in other studies [10]. One patient with a primary cancer site of the prostate was interviewed by Gater et al. and remarked that, “he had not had one solid day of relief without pain whatsoever,” and that this pain was, “so different because it’s very intense,” [14]. Pain was commonly assessed through pain-specific scales, such as the Brief Pain Inventory (BPI), Visual Analog Scale (VAS), and Numeric Rating Scales (NRS).
Physical issues: non-pain
Aside from pain, several systemic physical symptoms were prevalent among patients with BM. In a prospective study with 518 patients, Chow et al. found that fatigue, drowsiness, and a lack of appetite occurred in more than 75% of patients [15]. Likewise, Shi et al. demonstrated in a prospective patient survey of 120 patients that fatigue and lack of appetite were two of the most prevalent symptoms in BM patients [16]. Patients with complicated BM resulting in compression of neural structures, experienced limb weakness, numbness, urinary difficulties, and fecal incontinence. Some patients also complained about having swelling or a mass at the affected site of BM [17,18,19,20].
Functional interference
Interference with mobility was the most frequent functional issue, ranging from difficulty in walking to being bedridden. Kim et al. found that out of 244 patients pending surgical stabilization for BM, close to 80% of patients lost their ability to walk unaided. Forty five percent required walking aids, 19% were wheelchair-bound, and 13% were bedridden [21]. Actions such as standing, sitting, and lying down were also difficult for patients [22]. Additionally, patients' range of motion of the affected joint was limited [23]. Interference with strenuous physical exercise was also a commonly observed issue. A study by Porter et al. showed that patients with BM had reduced levels of physical activity prior to receiving BM-directed interventions such as Strontium-89 [24].
As a result of impaired function, significant interference in patients’ daily activities was frequently reported in the literature [16]. BM affected patients’ self-care activities, such as bathing or dressing, sexual activity, and work [22, 25, 26]. In a qualitative study by Akakura et al., 91% of patients reported that their daily activities were affected due to their disease, and 73% described that BM impacted their ability to perform family roles. Sleep was also affected in up to 41% of patients [27].
Psychosocial issues
Unsurprisingly, BM patients experience a multitude of psychosocial issues due to their disease. In a study of 122 patients with castration-resistant prostate cancer and subsequent bone metastases, 47% had significant psychological distress due to anxiety and depression prior to treatment with Radium-223 [28]. Coward et al. performed patient interviews that included themes of psychosocial issues. Patients mentioned that the “pain reminds [them] that [their cancer] is still there,” and that “it’s so constant, it just wears you out” [10]. Additionally, BM patients remarked upon the interference of their diagnosis with social activities, hobbies, and their relationships with their friends and family [10]. In a qualitative study by Chen et al., patients often felt that they were a burden to their family [29]. Worries about medical care, general health, and impending death were additional issues mentioned by patients [27].
Treatment-related QoL issues
Patients with BM may experience QoL issues not only due to their disease, but also from BM-directed treatments. Treatment-related QoL issues were extracted separately and were categorized by treatment modality (Table 3). In this systematic review, the most common interventions were categorized as radiotherapy, surgery, BMAs, image-guided ablation, percutaneous cementoplasty, and radionuclides. In all these treatment modalities, some form of post-treatment pain was noted [30,31,32,33,34,35,36]. Nausea and fatigue were side effects common to nearly all treatments [30, 33,34,35,36].
Palliative radiotherapy was most frequently prescribed using a conventional external beam radiotherapy (cEBRT) technique for pain control in bone metastases. In a RCT of 241 patients randomized to receive two different dose schedules of cEBRT, acute treatment-related toxicities, such as erythema, nausea, vomiting, and tiredness, were present up to 35% of patients [30]. Stereotactic body radiation therapy (SBRT) allows for the delivery of a higher dose per fraction while sparing normal tissues, and has gained popularity in the recent decade for the treatment of BM. Compared to cEBRT, this treatment technique was shown to achieve higher rates of complete pain response, but also higher rates of pain flares in the first month after treatment [37]. Some patients may not tolerate SBRT due to the pain associated with the treatment position. In a Dutch RCT involving more than 100 patients, up to one in five patients receiving SBRT could not tolerate treatment due to severe pain being in treatment position [38].
Surgical options for BM include stabilization of the bones, reconstruction, and resection of tumour. Common post-operative complications reported by patients included wound complications, post-operative swelling, and pain with mobilization [31, 32].
BMAs such as zoledronic acid, pamidronate and denosumab were commonly used in the treatment of BM to prevent SREs. QoL issues reported by patients treated with BMAs included bone pain, nausea, flu-like symptoms, jaw pain due to osteonecrosis, and fatigue. Notably, bone pain could occur in up to 30% of patients, as shown in a RCT by Amadori et al., that compared two dose intervals of zoledronic acid in 425 patients with BM from primary breast cancer [33]. However, this onset of bone pain reported from the use of BMAs is transient, and long-term use of BMAs often leads to reduction of disease-related pain [33].
Studies on other interventions identified other side-effects that may negatively impact QoL. For example, radionuclides such as Radium223 and Lutetium177 caused pain flares, nausea, fatigue, and diarrhea [34]. Additionally, image-guided ablation treatments, such as radiofrequency ablation, resulted in post-procedural pain flares, skin burns, and nausea [35]. Furthermore, percutaneous cementoplasty was often associated with nausea and pain at the injection site [36].
Patient-reported outcome measures (PROMs)
A range of tools are used to assess the patient-reported outcomes of patients with BM in the literature (Table 4). These tools can be classified into the following groups: (1) pain scales, (2) generic QoL assessment tools, (3) cancer site-specific QoL assessment tools (4) BM-specific QoL assessment tools, (5) issue-specific assessment tools (e.g., for anxiety) and, (6) investigator-designed questionnaires or scales.
The pain Visual Analog Scale (VAS) and the Brief Pain Inventory (BPI) were used the most (119 studies used VAS, 89 studies used BPI). The VAS was used in conjunction with another PROM in 58% of all studies included in this systematic review (69 out of 119 studies that used VAS). The next most frequently used PROM was the European Organization of Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30), followed by study-specific questionnaires designed by the investigator. Other generic QoL tools that were commonly employed include the EORTC QLQ-C15-PAL (a shortened form of the QLQ-C30 designed for patients in palliative care), Short Form 36 Health Survey Questionnaire (SF-36), EuroQol-5 Dimension (EQ-5D), and the Functional Assessment of Cancer Therapy—General (FACT-G). Cancer site-specific QoL assessment tools, (e.g., FACT-Prostate for prostate cancer and EORTC QLQ-BR23 for breast cancer), as well as issue-specific assessment tools (e.g., Hospital Anxiety and Depression Scale), were used less frequently.
Three BM-specific QoL assessment tools were identified in this systematic review: the EORTC QLQ-BM22, Functional Assessment of Cancer Therapy-Bone Pain (FACT-BP), and BOMET-QoL-10. Of these tools, the most frequently used was the EORTC QLQ-BM22, developed in 2009 by the EORTC Quality of Life Group (QLG) [39]. This tool has a total of 22 items with subscales on pain site, pain characteristics, functional interference, and psychosocial issues [39]. The FACT-BP scale consists of 16 questions with a focus on bone pain and its impact on one’s quality of life [40]. The BOMET-QoL-10 tool utilizes 10 questions to assess the symptoms of a patient’s BM and its effects on physical, social, and mental domains of QoL [41].
QoL issues not covered by PROMs
Table 5 summarises the domains covered by PROMs that were used more than 20 times in the literature and the BM-specific assessment tools. None of these tools address all domains of issues identified in the systematic review. Since the EORTC QLQ-BM22 is recommended to be used with the EORTC QLQ-C30 in clinical trials, these two tools combined are the most comprehensive for assessing the QoL of patients with BM [39]. While all tools ask about the presence and severity of pain, only three (BPI, EORTC QLQ-BM22, and BOMET-Qol-10) assess both the site and nature of pain [39, 41, 42]. All BM specific tools assess functional interference and emotional or psychological issues [39,40,41].
BPI is the only tool that explicitly assesses the effects of treatment on patient QoL [42]. Even so, it only assesses whether patients attribute pain to BM-directed treatments such as surgery and radiotherapy [42]. The time to onset of pain, for example, whether it occurred immediately (pain flare) or constantly after treatment, is not assessed by these PROMs [39,40,41,42]. Other specific treatment-related issues, such as jaw pain due to osteonecrosis of the jaw, are also not mentioned [39,40,41,42]. Additionally, apart from pain, none of the tools assessed symptoms related to BM, such as numbness and limb weakness that could result from radiculopathy or spinal cord compression [39,40,41,42].
Discussion
To our knowledge, this is the first systematic review evaluating both the QoL issues experienced by patients with BM and the tools used to assess them. A comprehensive list of QoL issues relevant to BM was generated, demonstrating the multitude of issues faced by patients with BM related to their disease. Additionally, an exhaustive list of treatment-related issues specifically relevant to BM patients was compiled. These affect the physical health, functional capabilities, emotional well-being, and relationships with others in patients with BM.
Many PROMs have been used to assess the QoL of patients with BM. A key finding of this systematic review is that most of these tools exclusively focus on pain and its impact on patients’ daily living. Due to advances in systemic anti-cancer treatments, patients with BM have greater life expectancies, and thus have higher risks of developing SREs over time [2]. Patients with such complications, for example malignant spinal collapse or spinal cord compression, may have vastly different QoL issues compared to patients with localized BM, such as a small sclerotic BM with no soft tissue component [6]. Additionally, for patients with oligometastatic BM, the treatment goals and varying presentation of symptoms may alter the QoL issues faced, regarding pain and survival outcomes [43]. Therefore, the issues being assessed in the existing tools may not be entirely relevant.
This review has identified the EORTC QLQ-BM22 as the most frequently used BM-specific PROM in the literature. This tool was first developed in 2009 and validated internationally with BM patients [39]. According to the EORTC QLG guidelines, this tool must be used in conjunction with the EORTC QLQ-C30 [44]. When combined, these tools assess patients’ QoL far more comprehensively than other measures but unfortunately these measures still do not explicitly assess treatment-related issues. One issue commonly resulting from all BM-directed treatment modalities is worsening of pain after treatment, or pain flares. Existing tools are not specific to the pain treated by BM-related modalities, and in many studies assessed it is unclear how patients were instructed to rate their treated pain at baseline/follow-up assessments, compared to pain originating from other sources. This specification is necessary for QoL tools, in order to correctly evaluate the impact of an intervention on a patient’s pain. Due to the extended survival of patients with BM, repeat interventions may also be required, and consideration must be made for this as well in tools [5]. Psychological distress, lack of social support and poor coping has also been associated with the intensity of pain [45]. Therefore, it is important to monitor differences in pain severity between treatments.
Furthermore, patients receiving BMAs have a unique set of treatment-related issues, for example flu-like syndrome and osteonecrosis of the jaw [3]. The 2020 European Society of Medical Oncology guidelines on bone health has recommended that all patient with BM should be offered BMAs, regardless of whether the metastases are complicated or not [46]. Due to this increased use of BMAs, it is important to incorporate these issues into existing assessments.
Strengths and limitations
A major strength of this systematic review is that all types of studies reporting the experience of patients with BM were assessed, including qualitative studies and case reports. Studies that used open-ended interviews to assess QoL allowed investigators to deeply explore patients’ symptoms and discover what is the most relevant to them regarding their QoL. This enabled the discovery of new issues that are not currently covered by existing tools.
One of the main limitations of this review is that the QoL issues identified are confined to the aims and questions assessed by the studies. As a result, QoL issues faced by patients with BM may not be included in this list if it was not reported in the studies extracted. Due to the nature of BM, some of the issues identified may have been caused by the primary cancer rather than BM. Additionally, the inclusion of case reports may have introduced symptoms that were only observed in a small number of patients. Furthermore, patients with BM are a heterogeneous population with varying experiences. Treatment strategies and their impacts on QoL could vary depending on various factors, such as the site of BM, the number of metastases, the primary cancer, and expected survival time. Thus, some issues may not be applicable to all patients with BM.
Future directions
In many studies, multiple tools were used to assess the wide range of QoL issues experienced by patients. To relieve patients’ burden from answering multiple questionnaires, there is a need to update or combine existing tools to encompass all relevant QoL issues. Moving forward, interviews with patients and healthcare professionals should be conducted to comprehensively assess additional issues identified in this systematic review, in particular the non-pain physical issues and treatment-related issues. Patients recruited for the interviews should be stratified by the site of BM, their duration of being diagnosed with BM, and treatment(s) received. This will ensure that future assessment tools assess issues relevant to all types of patients with BM.
A bone metastases-specific patient reported outcome instrument that not only focuses on pain will be more comprehensive in assessing how the disease affects patients’ quality of life. Treatments aiming to effectively improve every QoL domain is important, as there is a complex relationship between pain, other physical symptoms, as well as psychosocial and functional QoL issues. Some patients presenting with spinal cord compression or pathological fractures may have difficulties with mobility at the remaining days of their life. It is reported that advanced cancer patients have spiritual concerns due to the consequences of their disease [47]. Such issues, for example difficulty in maintaining personal identity and worries about death and afterlife, were not captured in our systematic review [47]. A focused interview specifically asking these questions is needed to see whether they are relevant to certain subsets of patients with complicated BM.
Conclusion
This systematic review compiled an exhaustive list of QoL issues described by patients with BM and identified the tools used to assess them. The QoL issues spanned physical, functional, and psychosocial domains, and can act as a reference to patients and their families on the issues they may encounter after receiving the diagnosis of BM. Additionally, this QoL issue list will be helpful for healthcare professionals to better understand patients’ experience, and more effectively design treatment programs to address their needs. An update of BM-specific QoL tools based on this list is recommended to ensure they comprehensively capture the QoL issues faced by patients, especially those that relate to the newest BM-directed treatments.
Data availability
The search strategy and results can all be found in the tables and figures in the manuscript. All included articles can be found referenced in Appendix 2.
References
Tharmalingam S, Chow E, Harris K, Hird A, Sinclair E (2008) Quality of life measurement in bone metastases: A literature review. J Pain Res 1:49–58. https://doi.org/10.2147/jpr.s4572
Jiang W, Rixiati Y, Zhao B, Li Y, Tang C, Liu J (2020) Incidence, prevalence, and outcomes of systemic malignancy with bone metastases. J Orthop Surg 28(2). https://doi.org/10.1177/2309499020915989
Clézardin P, Coleman R, Puppo M et al (2021) Bone metastasis: Mechanisms, therapies, and biomarkers. Physiol Rev 101(3):797–855. https://doi.org/10.1152/physrev.00012.2019
Gainford MC, Dranitsaris G, Clemons M (2005) Recent developments in bisphosphonates for patients with metastatic breast cancer. BMJ 330(7494):769–773. https://doi.org/10.1136/bmj.330.7494.769
Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12(20):6243s–6249s. https://doi.org/10.1158/1078-0432.CCR-06-0931
Tsukamoto S, Kido A, Tanaka Y et al (2021) Current overview of treatment for metastatic bone disease. Curr Oncol 28(5):3347–3372. https://doi.org/10.3390/curroncol28050290
Gouveia AG, Chan DCW, Hoskin PJ et al (2021) Advances in radiotherapy in bone metastases in the context of new target therapies and ablative alternatives: A critical review. Radiother Oncol 163:55–67. https://doi.org/10.1016/j.radonc.2021.07.022
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372:71. https://doi.org/10.1136/bmj.n71
Veritas Health Innovation (2023) Covidence systematic review software. http://www.covidence.org. Accessed 29 Jan 2023
Coward DD, Wilkie DJ (2000) Metastatic bone pain. Meanings associated with self-report and self-management decision making. Cancer Nursing 23(2):101–108. https://doi.org/10.1097/00002820-200004000-00005
Martin M, Bell R, Bourgeois H et al (2012) Bone-related complications and quality of life in advanced breast cancer: Results from a randomized phase III trial of denosumab versus zoledronic acid. Clin Cancer Res 18(17):4841–4849. https://doi.org/10.1158/1078-0432.CCR-11-3310
Agarwal KK, Singla S, Arora G, Bal C (2015) (177) Lu-EDTMP for palliation of pain from bone metastases in patients with prostate and breast cancer: A phase II study. Eur J Nucl Med Mol Imaging 42(1):79–88. https://doi.org/10.1007/s00259-014-2862-z
Bongiovanni A, Recine F, Fausti V et al (2019) Ten-year experience of the multidisciplinary osteoncology center. Support Care Cancer 27(9):3395–3402. https://doi.org/10.1007/s00520-019-4635-5
Gater A, Abetz-Webb L, Battersby C et al (2011) Pain in castration-resistant prostate cancer with bone metastases: A qualitative study. Health Qual Life Outcomes 9:88. https://doi.org/10.1186/1477-7525-9-88
Chow E, Fan G, Hadi S, Filipczak L (2007) Symptom clusters in cancer patients with bone metastases. Support Care Cancer 15(9):1035–1043. https://doi.org/10.1007/s00520-007-0241-z
Shi Z, Qiu H, Yu S (2010) The investigation of symptoms burden and treatment status in patients with bone metastasis. Chin Ger J Clin Oncol 9(2):63–67. https://doi.org/10.1007/s10330-010-0009-7
Gottwald L, Dukowicz A, Misiewicz B, Pasz-Walczak G, Cialkowska-Rysz A (2011) An extremely rare presentation of relapse in endometrioid endometrial adenocarcinoma: Isolated metastases to the tibia and humerus. Case report and review of the literature. Eur J Gynaecol Oncol 32(5):547–550
Plancarte R, Guajardo J, Meneses-Garcia A et al (2014) Clinical benefits of femoroplasty: A nonsurgical alternative for the management of femoral metastases. Pain Physician 17(3):227–234
Moinpour C, Savage M, Troxel A et al (1998) Quality of life in advanced prostate cancer: Results of a randomized therapeutic trial. JNCI 90(20):1537–1544. https://doi.org/10.1093/jnci/90.20.1537
Lindqvist O, Rasmussen BH, Widmark A (2008) Experiences of symptoms in men with hormone refractory prostate cancer and skeletal metastases. Eur J Oncol Nurs 12(4):283–290. https://doi.org/10.1016/j.ejon.2008.03.003
Kim Y, Krishnan CK, Kim HS, Cho HS, Han I (2020) Ambulation recovery after surgery for metastases to the femur. Oncologist 25(1):e178–e185. https://doi.org/10.1634/theoncologist.2019-0107
Charles T, Ameye L, Gebhart M (2017) Surgical treatment for periacetabular metastatic lesions. Eur J Surg Oncol 43(9):1727–1732. https://doi.org/10.1016/j.ejso.2017.03.018
Antal I, Szoke G, Szendroi M et al (2023) Functional outcome and quality of life following resection of the proximal humerus performed for musculoskeletal tumors and reconstruction done by four different methods. Musculoskelet Surg. https://doi.org/10.1007/s12306-022-00771-w
Porter AT, McEwan AJ, Powe JE et al (1993) Results of a randomized phase-III trial to evaluate the efficacy of strontium-89 adjuvant to local field external beam irradiation in the management of endocrine resistant metastatic prostate cancer. Int J Radiat Oncol Biol Phys 25(5):805–813. https://doi.org/10.1016/0360-3016(93)90309-j
Harris K, Chow E, Zhang L et al (2009) Patients’ and health care professionals’ evaluation of health-related quality of life issues in bone metastases. Eur J Cancer 45(14):2510–2518. https://doi.org/10.1016/j.ejca.2009.05.024
Torvik K, Holen J, Kaasa S et al (2008) Pain in elderly hospitalized cancer patients with bone metastases in Norway. Int J Palliat Nurs 14(5):238–245. https://doi.org/10.12968/ijpn.2008.14.5.29491
Akakura K, Uemura H, Miyazaki K et al (2021) A qualitative research study in Japan investigating patients’ experience with metastatic castration-resistant prostate cancer: From diagnosis to decision for Ra-223 treatment. Future Oncol 17(36):5103–5118. https://doi.org/10.2217/fon-2021-0773
van der Doelen MJ, Oving IM, Wyndaele DNJ et al (2022) Health-related quality of life, psychological distress, and fatigue in metastatic castration-resistant prostate cancer patients treated with radium-223 therapy. Prostate Cancer Prostatic Dis 26:142–150. https://doi.org/10.1038/s41391-022-00569-8
Chen JJ, Roldan CS, Nichipor AN et al (2021) Patient-provider communication, decision-making, and psychosocial burdens in palliative radiotherapy: A qualitative study on patients’ perspectives. J Pain Symptom Manage 62(3):512–522. https://doi.org/10.1016/j.jpainsymman.2021.01.129
Nielsen OS, Bentzen SM, Sandberg E, Gadeberg CC, Timothy AR (1998) Randomized trial of single dose versus fractionated palliative radiotherapy of bone metastases. Radiother Oncol 47(3):233–240. https://doi.org/10.1016/s0167-8140(98)00011-5
Laitinen M, Nieminen J, Pakarinen TK (2011) Treatment of pathological humerus shaft fractures with intramedullary nails with or without cement fixation. Arch Orthop Trauma Surg 131(4):503–508. https://doi.org/10.1007/s00402-010-1172-6
Katzer A, Meenen NM, Grabbe F, Rueger JM (2002) Surgery of skeletal metastases. Arch Orthop Trauma Surg 122(5):251–258. https://doi.org/10.1007/s00402-001-0359-2
Amadori D, Aglietta M, Alessi B et al (2013) Efficacy and safety of 12-weekly versus 4-weekly zoledronic acid for prolonged treatment of patients with bone metastases from breast cancer (ZOOM): A phase 3, open-label, randomised, non-inferiority trial. Lancet Oncol 14(7):663–670. https://doi.org/10.1016/S1470-2045(13)70174-8
Parker CC, Pascoe S, Chodacki A et al (2013) A randomized, double-blind, dose-finding, multicenter, phase 2 study of radium chloride (Ra 223) in patients with bone metastases and castration-resistant prostate cancer. Eur Urol 63(2):189–197. https://doi.org/10.1016/j.eururo.2012.09.008
Napoli A, De Maio A, Alfieri G et al (2023) Focused Ultrasound and External Beam Radiation Therapy for Painful Bone Metastases: A Phase II Clinical Trial. Radiology 307(2). https://doi.org/10.1148/radiol.211857
Fares A, Shaaban MH, Reyad RM, Ragab AS, Sami MA (2018) Combined percutaneous radiofrequency ablation and cementoplasty for the treatment of extraspinal painful bone metastases: A prospective study. J Egypt Natl Canc Inst 30(3):117–122. https://doi.org/10.1016/j.jnci.2018.05.002
Sahgal A, Myrehaug SD, Siva S et al (2021) Stereotactic body radiotherapy versus conventional external beam radiotherapy in patients with painful spinal metastases: An open label, multicentre, randomised, controlled, phase 2/3 trial. Lancet Oncol 22(7):1023–1033. https://doi.org/10.1016/S1470-2045%2821%2900196-0
Pielkenrood BJ, van der Velden JM, van der Linden YM et al (2021) Pain response after stereotactic body radiation therapy versus conventional radiation therapy in patients with bone metastases - A phase 2 randomized controlled trial within a prospective cohort. Int J Radiat Oncol Biol Phys 110(2):358–367. https://doi.org/10.1016/j.ijrobp.2020.11.060
Chow E, Hird A, Velikova G et al (2009) The European organisation for research and treatment of cancer quality of life questionnaire for patients with bone metastases: The EORTC QLQ-BM22. Eur J Cancer 45(7):1146–1152. https://doi.org/10.1016/j.ejca.2008.11.013
Broom R, Du H, Clemons M et al (2009) Switching breast cancer patients with progressive bone metastases to third-generation bisphosphonates: Measuring impact using the Functional Assessment of Cancer Therapy-Bone Pain. J Pain Symptom Manage 38(2):244–257. https://doi.org/10.1016/j.jpainsymman.2008.08.005
Barnadas A, Muñoz M, Margelí M et al (2019) BOMET-QoL-10 questionnaire for breast cancer patients with bone metastasis: the prospective MABOMET GEICAM study. J Patient Rep Outcomes 3(1):72. https://doi.org/10.1186/s41687-019-0161-y
Cleeland CS, Gonin R, Hatfield AK et al (1994) Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 330:592–596. https://doi.org/10.1056/NEJM199403033300902
Rogowski P, Trapp C, von Bestenbostel R et al (2021) Outcomes of metastasis-directed therapy of bone oligometastatic prostate cancer. Radiat Oncol 16:125. https://doi.org/10.1186/s13014-021-01849-8
Wheelwright S, Bjordal K, Bottomley A et al (2021) EORTC quality of life group guidelines for developing questionnaire modules. Fifth edition. https://www.eortc.org/app/uploads/sites/2/2022/07/Module-Guidelines-Version-5-FINAL.pdf. Accessed 29 Jan 2023
Zaza C, Baine N (2002) Cancer pain and psychosocial factors: A critical review of the literature. J Pain Symptom Manage 24(5):526–542. https://doi.org/10.1016/S0885-3924(02)00497-9
Coleman R, Hadji P, Body JJ et al (2020) Bone health in cancer: ESMO clinical practice guidelines. Ann Oncol 31(12):1650–1663. https://doi.org/10.1016/j.annonc.2020.07.019
de Vries S, Lormans T, de Graaf E, Leget C, Teunissen S (2021) The content validity of the items related to the social and spiritual dimensions of the Utrecht Symptom Diary-4 Dimensional from a patient’s perspective: A qualitative study. J Pain Symptom Manage 61(2):287-294.e2. https://doi.org/10.1016/j.jpainsymman.2020.07.036
Acknowledgements
Consortium members and affiliations
Henry CY Wong MBBS2, 20, Samantha KF Kennedy BSc(C)1, 20, Hany Soliman MD1, 20, Vassilios Vassiliou MD, PhD3, 20, Dirk Rades MD, FASTRO4, 20, Pierluigi Bonomo MD5, 20, Shing-Fung Lee MBBS, MSc6,7, 20, Adrian Wai Chan MBBS7, 20, Agata Rembielak MD, PhD8, 9, 20, Eva Oldenburger MD10, 20, Ernesto Maranzano MD11,12, 20, Joel A Finkelstein MD, MSc14, 20, Jeremie Larouche MD, MSc14, 20, Gustavo N Marta MD, PhD16, 20, Albert JM Yee MD, MSc14, 20, Joanne M van der Velden PhD18, 20, Edward Chow MBBS1, 20, On behalf of the EORTC Quality of Life Group20
20Quality of Life Department, EORTC, Avenue E. Mounier, 83/11, 1200 Brussels, Belgium
Funding
This research was funded by the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group (QLG), grant number 005/2023. The EORTC QLG business model involves license fees for commercial use of their instruments. Academic use of EORTC instruments is free of charge.
Author information
Authors and Affiliations
Consortia
Contributions
Data extraction was conducted by TR, HCYW, and EZ. Figures and tables were prepared by TR and HCYW. The first draft of the manuscript was written by TR and HCYW and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Thenugaa Rajeswaran and Henry CY Wong contributed equally to this work as joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rajeswaran, T., Wong, H.C.Y., Zhang, E. et al. Quality of life issues in patients with bone metastases: A systematic review. Support Care Cancer 32, 18 (2024). https://doi.org/10.1007/s00520-023-08241-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-08241-0