Abstract
Purpose
To evaluate the overall efficacy of StrataXRT, a topical gel dressing, in preventing acute radiation dermatitis (RD) in breast cancer patients undergoing radiotherapy (RT).
Methods
A systematic search was conducted on April 25, 2023 in Ovid MEDLINE, Embase, and Cochrane Central Register of Controlled Trials. Randomized controlled trials (RCTs) assessing the effectiveness of StrataXRT in preventing acute RD in breast cancer patients undergoing adjuvant RT to the breast or chest wall with or without regional nodes were included. Pooled incidence odds ratio (OR) and 95% confidence interval (CI) were calculated using a random-effects model, with analysis and forest plots generated in RevMan v5.4.
Results
The analysis included three RCTs with a total of 189 patients assessed using per-protocol analysis. Two RCTs compared StrataXRT to standard of care, while the third compared it with Mepitel film and was reported separately. In the former RCTs, the odds ratio (OR) for developing acute grade 3 RD favored StrataXRT at 0.05 (95% CI, 0.01-0.22; P < 0.0001). The OR for developing acute grades 2–3 RD was 0.32 (95% CI, 0.03-3.18; P = 0.33). The RCT comparing StrataXRT with Mepitel film showed insignificant ORs for grade 3 and grades 2-3 RD. One RCT reported significantly lower erythema index (P = 0.008) and melanin index (P = 0.015) in StrataXRT patients. The use of StrataXRT did not raise additional safety concerns.
Conclusion
StrataXRT may help prevent severe acute RD in breast cancer RT patients. Further high quality, large-scale studies are needed to confirm these findings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radiation dermatitis (RD) is a common side effect experienced by patients with breast cancer receiving radiotherapy (RT) [1]. Acute RD can cause pain and discomfort which can negatively impact patients’ health-related quality-of-life (HRQoL), and in severe cases lead to treatment delays or interruptions [2]. Recent international Delphi consensus-based recommendations suggest interventions for possible prevention of RD. Among those interventions are photobiomodulation therapy, as well as usage of topical dressings such as Mepitel film, Hydrofilm, mometasone, betamethasone, and olive oil [3]. However, the aforementioned treatments can be challenging to apply in certain sites and may be associated with various side effects [4]. Therefore, identifying novel and effective interventions for preventing RD is important.
StrataXRT is a topical silicone-based gel designed to form a protective semi-permeable film barrier on the skin and promote a moist wound healing environment [5, 6]. It has been hypothesized to help prevent and manage RD by reducing trans-epidermal water loss (TEWL), inflammation and fibrosis, as well as by promoting re-epithelialization of the skin [7]. The aim of this systematic review and meta-analysis is to investigate the efficacy and safety of StrataXRT in preventing acute RD in patients with breast cancer who underwent RT.
Materials and methods
The analysis was performed and findings were reported according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guideline [8]. Two reviewers (SL and HW) independently performed the literature search, assessed study eligibility, extracted the relevant data, and performed the risk-of-bias assessment following the strategies stated below. Any disagreement between the reviewers was resolved through discussion and consensus, or arbitration by the third reviewer (AC). Forest plots were generated using RevMan v.5.4 (SS and SC).
Search strategy
Studies were identified through a systematic search on Embase, MEDLINE, and Cochrane Central Register of Controlled Trials (CENTRAL). A literature search was conducted on April 25, 2023 for articles investigating the use of StrataXRT for the prevention of acute RD due to breast cancer RT. A combination of the following search terms was used: “cancer”, “radiotherapy”, and “StrataXRT”. The detailed search strategies for each database are summarized in Appendix 1. Reference lists of relevant studies were also reviewed for possibly suitable articles. We only included human studies in the English language. Academic experts on RD were contacted to identify supplemental data.
Inclusion and exclusion criteria
Articles were included if (1) the study was a randomized controlled trial (RCT), (2) the study used StrataXRT for the prophylaxis of acute RD in breast cancer patients undergoing RT, and included in the meta-analyses only if (3) the study compared StrataXRT with a placebo/standard of care/other active treatments. We excluded studies that did not provide quantified data or sufficient statistical parameters for analysis, reported exclusively on patients aged <18 years. Duplicate reports and studies covering overlapping populations were excluded. In cases where the same study population was reported on more than once, we included the most recent article.
Data extraction
Data extracted from the included studies were first author, year of publication, country of study population, sample size (randomized and included in analysis), cancer sites and stages, RT dose-fractionations and techniques, inter- or intra-patient comparison or randomization, intervention used and its frequency and duration, and the scoring systems for rating acute RD. Any grade of acute RD was extracted. Where appropriate standard deviations and standard errors from the p-values were derived, according to the instructions in the Cochrane Handbook for Systematic Reviews of Interventions [9].
Risk of bias assessment
We used the Cochrane risk-of-bias tool for randomized trials to evaluate the quality of each included study [10]. This tool was specifically developed for use in reviewing RCTs, which may have certain methodological challenges such as selective outcome reporting.
Assessing the certainty of the evidence
The GRADE approach (Grading of Recommendations, Assessment, Development and Evaluations) to evaluate the quality (certainty) of the overall body of evidence was utilized [11]. This evaluation encompassed all relevant GRADE domains, including methodological limitations, inconsistency, imprecision, indirectness, and publication bias.
Systematic review and statistical analysis
The study findings were summarized in Tables 1 and 2. Where appropriate, we performed meta-analysis on suitable studies to investigate the relationship between StrataXRT use and its preventive effect on acute RD in breast cancer. The main summary statistics analyzed was the incidence of clinician- and/or patient-reported acute skin toxicities and grades, and their corresponding 95% confidence intervals (CIs). Heterogeneity between effect estimates among studies was quantified by two statistical tests: the Cochran Q statistical test for between-study variability and the I2 statistic for the proportion of total variation across studies due to statistical heterogeneity instead of chance [12].
We employed a random-effects model to calculate the meta-analytic summary estimate of each odds ratio (OR), along with 95% CIs [13]. This analytic approach accounts for statistical heterogeneity between studies, which may arise from variations in patient characteristics across studies, the interventions used, and the outcome assessments [13].
All p-values were two-tailed, and p-values of <0.05 were considered statistically significant. The analyses and graphs were generated using Review Manager (RevMan) [Computer program]. Version 5.4. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2015.
Results
Study characteristics
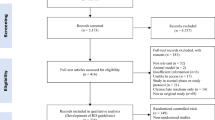
The literature search resulted in 31 studies, eight of which were duplicates. Twenty-two studies were screened by title and abstract using the inclusion/exclusion criteria, of which three met the inclusion criteria (Fig. 1). These were published from 2019 to 2022 [14,15,16]. One of three studies used an intra-patient randomization [15], in which either half of the irradiated breast was randomized to receive StrataXRT or Mepitel film (Table 1). All studies used a 1:1 allocation of patients to intervention arm and control arm. Two studies randomized patients to receive StrataXRT or the institutional standard of care (moisturizer and daily rinse, respectively) [14, 16], while one used Mepitel film as a control [15]. No significant difference in patient characteristics between the two arms was reported in all three studies.
The studies conducted by Chao et al. (2014) (n=44) used the Common Terminology Criteria of Adverse Events (CTCAE) to grade the severity of acute RD [15]. Omidvari et al. (2022) (n=100) used the Radiation Therapy Oncology Group (RTOG) scale and the size of RD was measured using a transparent paper [16]. Ahn et al. (2020) (n=56) used the CTCAE, RTOG, and the modified 10-point Catterall skin scoring profile to report healthcare provider-assessed outcome [14]. Additionally, this study assessed patient-reported symptoms using a five-point scale questionnaire, and objective skin parameters including erythema index, melanin index, TEWL, and laser Doppler flowmetry [14] (Table 2).
Outcomes
Healthcare provider-assessed RD
Omidvari et al. found that the grade 3 and grades 2–3 at week 5 of RT for StrataXRT and control were 4% and 46% respectively (OR, 0.05; 95% CI, 0.01─0.22), while grades ≥2 were 94% and 98% respectively (OR, 0.32; 95% CI, 0.03─3.18) [16]. One patient in the control group developed grade 4 RD. However, the incidence of moist desquamation was not reported in Omidvari et al. [16]. Ahn et al. reported the similar incidences of RD in both arms, all the patients developed grade 1 RD, as defined by RTOG and CTCAE, during RT until four weeks post-treatment [14]. Chao et al. compared the effect of StrataXRT and Mepitel film on either medial or lateral half of the breast [15]. The chances of developing CTCAE grades 0, 1, 2 and 3 skin toxicities were 0%, 30%, 70% and 0% respectively for the StrataXRT half, compared with 5%, 42.5%, 50% and 2.5% respectively for the Mepitel film half [15]. The incidence of moist desquamation was 12.5% and 20% for StrataXRT and Mepitel film respectively (p = 0.099) [15].
Patient-assessed RD
Only Ahn et al. evaluated patients’ symptoms related to RD including dryness, itchiness, burning sensation, and pain in the treatment site using a five-point Likert scale [14]. No statistically significant differences between the treatment arms were detected. Dryness (P = 0.470), itchiness (P = 0.672), burning sensation (P = 0.442), and pain (P = 0.858) gradually increased during RT, reached a peak at the end of RT, and then decreased [14].
Physiological skin parameters and side effects
Ahn et al. assessed skin toxicities objectively using electronic devices by dermatologists blinded to the treatment allocation [14]. Erythema index and melanin index which quantified cutaneous erythema and melanin respectively, and TEWL, were assessed [17]. Erythema index peaked at the end of RT in both groups, melanin index increased in both groups from baseline to two weeks after the completion of RT and then improved [14]. They detected a significantly lower erythema index (P = 0.008) and melanin index (P = 0.015) among patients in the StrataXRT group compared with those using moisturizer [14]. However, TEWL (P = 0.228) was not significantly different between arms [14].
In the study by Omidvari et al., the maximum area of RD was measured using transparent paper. The mean size of maximum area of RD was significantly different between the StrataXRT (36.88 cm2 ± 69.93) and control group (83.83 cm2 ± 79.34) (P = 0.002) [16].
No additional safety concerns or toxicity issues were reported with the use of StrataXRT in Ahn et al.[14]. Chao et al. and Omidvari et al. did not report on side effects [15, 16].
Risk of bias assessment and GRADE assessment
The assessment of the risk of bias of the included studies is presented in Fig. 2. Studies generally presented with low bias or some concerns with regard to random sequence generation, allocation concealment, deviations from the intended interventions, missing outcome data and their measurement, and selection of the reported result. All studies had a high level of bias for the lack of blinding of participants and/or outcome assessors. Details regarding our judgment on the risk of bias are elaborated in Supplemental Table S1. The grades of evidence as defined by the GRADE Working Group are depicted in Supplemental Table S2.
Meta-analysis
Three RCTs were included in our analysis [14,15,16]. Two RCTs compared StrataXRT to the “standard of care” (moisturizer and daily rinse, respectively) [14, 16]. Chao et al. was reported separately because it compared StrataXRT with Mepitel film instead of a standard control agent [15]. A total of 189 patients were assessed through per-protocol analysis (Table 1). Odds ratios (ORs) were estimated for Omidvari et al., as patients in Ahn et al. experienced a maximum of grade 1 RD, making ORs inestimable (Table 3). The OR for developing acute grade 3 RD favored StrataXRT at 0.05 (95% CI, 0.01–0.22; P <0.0001). The OR for developing acute grades 2–3 RD was 0.32 (95% CI, 0.03–3.18; P = 0.33). In Omidvari et al., one patient in the control group developed grade 4 RD. Forest plots were generated (Fig. 3), including this grade 4 RD patient, as a sensitivity analysis (Fig. S1). The sensitivity analysis did not change the conclusion. For Chao et al. the estimated OR for developing acute grade 3 and grades 2–3 RD, with Mepitel film as the reference group, were at 0.33 (95% CI, 0.01–8.22; P = 0.50) and 2.11 (95% CI, 0.84–5.29; P = 0.11), respectively. Other reported outcomes were not quantitatively comparable among the studies.
Discussion
This systematic review and meta-analysis comprehensively evaluated the evidence for the efficacy of StrataXRT in preventing RD in patients receiving RT for breast cancer. Promising interventions are often characterized by novel biological rationale and exceptional claims of effectiveness [18]. We assessed StrataXRT, a silicone-based film-forming gel dressing, designed to form a protective barrier to reduce TEWL and mechanical friction, with the goal of preventing, delaying, and minimizing grade 2 and 3 RD [5]. The OR for acute grade 3 RD and the physiological skin parameters in favor of StrataXRT observed provide some evidence for the efficacy of StrataXRT, although the findings are based on a limited number of studies.
Omidvari et al. observed positive results, noting a decrease in RTOG grade ≥2/3 RD for the StrataXRT arm compared to the standard of care (daily rinse). In contrast, Ahn et al. found no significant differences in CTCAE or RTOG grades between the intervention and control (moisturizer) groups. Chao et al. uniquely compared StrataXRT to Mepitel film rather than a moisturizer. Despite higher proportions of grade 2 RD in the StrataXRT group, no statistically significant difference in overall RD risk was detected, demonstrating the non-inferiority of StrataXRT to Mepitel film. Ahn et al. and Omidvari et al. also measured RD severity, however these studies used melanin index and erythema index, and RD area size, which are metrics not assessed in other studies. Subsequently, inter-study comparisons are challenging [14, 16]. Additionally, the use of per-protocol analysis raises concerns about attrition bias, as patients with greater adherence to assigned treatments may have different characteristics.[19]
In various studies, StrataXRT has shown potential in reducing the risk and severity of RD in cancer patients, including those with head and neck cancer [20,21,22]. Studies have reported reduced risks of grade 2 and 3 skin toxicity [20], delayed onset of RD symptoms [20], and faster recovery compared to control groups [21]. However, results should be interpreted with caution due to limitations such as small sample sizes [23], single-blinded designs [20], lack of randomization [22], and retrospective data [21, 22]. Patients generally found StrataXRT easy to use and comfortable [21, 22], but some reported discomfort due to its stickiness or when applied on tender skin [22]. Overall, StrataXRT may be a promising option for preventing and managing RD in cancer patients, but further research is needed to confirm its efficacy and safety.
HRQoL outcomes are essential to consider when evaluating interventions for RD, as patients' subjective experiences and well-being are crucial aspects of cancer care [24]. While the current analysis did not provide quantitative comparisons of HRQoL outcomes, the observed reduction in acute grade 3 RD incidence and the size of dermatitis area suggest that StrataXRT may potentially improve patients' experiences during RT. Future studies should incorporate comprehensive HRQoL assessments and patient-reported outcomes to better understand the impact of StrataXRT on patients' well-being and satisfaction with treatment. The development and validation of skin-specific HRQoL measures sensitive to changes in individuals experiencing RD are needed. These will help guide the creation of interventions for RD prevention and management, ultimately improving patients' HRQoL and identifying those who would gain the most from an intervention.
Cost-effectiveness is another important aspect to consider when evaluating novel interventions. Blades et al. conducted the cost-effectiveness evaluation of StrataXRT in RD prevention, drawing on the results from Chan et al.'s RCT [25]. The study did not determine willingness-to-pay thresholds or patients' financial burden, but it revealed that StrataXRT patients needed fewer nursing services and had reduced wound care expenses compared to those using 10% Glycerine (Sorbolene) [25]. Nevertheless, when accounting for all labor and care resources, the study did not identify any cost advantages for StrataXRT [25]. Although the current analysis did not provide data on the cost-effectiveness of StrataXRT compared to other RD interventions, it is essential for future research to investigate this aspect in patients with breast cancer. This information will help healthcare providers and patients make informed decisions regarding the adoption of StrataXRT as a standard preventive measure for RD in breast cancer RT.
In addition to evaluating the impact of StrataXRT on HRQoL and cost-effectiveness, future research should explore the potential benefits of this intervention for other patient populations and in different settings. For example, the efficacy of StrataXRT in preventing RD in patients receiving RT for other types of cancer, or concurrently in combination with other treatments such as immunotherapy and chemotherapy, has yet to be explored. Furthermore, the use of StrataXRT in non-cancer patients receiving RT for benign conditions may also warrant investigation.
The safety profile of StrataXRT, along with the fact that the gel does not cause a bolus effect, are important considerations for its potential widespread use in clinical practice. The current analysis reports no additional safety concerns or toxicity issues associated with StrataXRT use. This finding is in line with previous studies on silicone-based products, which generally show a favorable safety profile [6].
It is important to acknowledge the limitations of the current meta-analysis. The inclusion of only two RCTs with a relatively small total sample size of patients may limit the validity of the findings. Additionally, the relative lack of quantitatively comparable outcomes among the studies restricts the ability to draw definitive conclusions on other aspects of RD management, such as the impact of StrataXRT on patient-reported outcomes, HRQoL measures, or cost-effectiveness. As new studies emerge, it will be crucial to update this review to provide the most up-to-date evidence for clinicians and patients. Furthermore, our study has certain methodological limitations. We did not register our protocol in a public database like PROSPERO, and we restricted our literature search to English-language studies and excluded grey literature, which could introduce bias and overlook relevant research. These decisions were driven by practical considerations, yet we acknowledge their potential impact on our findings. The overall certainty of our evidence, as assessed by the GRADE methodology, was evaluated as moderate, underscoring the need for more robust studies. Despite these limitations, we adhered strictly to PRISMA guidelines throughout our reporting process. Despite these limitations, the significantly lower levels of the objectively measured skin parameters, erythema and melanin indices, that were observed in the StrataXRT group in one RCT suggest that this intervention might be effective in reducing inflammation and pigmentation changes associated with radiation-induced skin injury [14]. These findings warrant further investigation in future studies to confirm the potential benefits of StrataXRT on the overall appearance and health of the irradiated skin.
Conclusion
This systematic review and meta-analysis, supported by moderate certainty from the GRADE assessment, provide some evidence for the efficacy and safety of StrataXRT in preventing severe acute RD in patients receiving RT for breast cancer. High-quality studies with larger sample sizes and rigorous designs are needed to confirm these results and to compare the effect of StrataXRT on HRQoL and cost-effectiveness with other interventions.
Data availability
The datasets analyzed for this meta-analysis have been obtained from publicly available sources.
Code availability
The statistical code and computational methods employed in this meta-analysis are available upon reasonable request.
References
Hymes SR, Strom EA, Fife C (2006) Radiation dermatitis: Clinical presentation, pathophysiology, and treatment 2006. J Am Acad Dermatol 54:28–46
Ryan JL (2012) Ionizing radiation: the good, the bad, and the ugly. J Invest Dermatol 132:985–993
Behroozian T, Bonomo P, Patel P, Kanee L, Finkelstein S, van den Hurk C, Chow E, Wolf JR, Behroozian T, Bonomo P, Patel P, Kanee L, Finkelstein S, van den Hurk C, Chow E, Ryan Wolf J, Banerjee S, Becherini C, Boers-Doets C et al (2023) Multinational Association of Supportive Care in Cancer (MASCC) clinical practice guidelines for the prevention and management of acute radiation dermatitis: international Delphi consensus-based recommendations. Lancet Oncol 24:e172–e185
Behroozian T, Goldshtein D, Ryan Wolf J, van den Hurk C, Finkelstein S, Lam H, Patel P, Kanee L, Lee SF, Chan AW, Wong HCY, Caini S, Mahal S, Kennedy S, Chow E, Bonomo P, Behroozian T, Goldshtein D, Ryan Wolf J et al MASCC clinical practice guidelines for the prevention and management of acute radiation dermatitis: part 1 systematic review. eClin Med
Stratpharma. StrataXRT: Radiation Dermatitis Gel. Basel, Switzerland: Stratpharma. In: Book Stratpharma. StrataXRT: Radiation Dermatitis Gel. Basel, Switzerland: Stratpharma, City.
Chan RJ, Blades R, Jones L, Downer T-R, Peet SC, Button E, Wyld D, McPhail S, Doolan M, Yates P (2019) A single-blind, randomised controlled trial of StrataXRT®–A silicone-based film-forming gel dressing for prophylaxis and management of radiation dermatitis in patients with head and neck cancer. Radiother Oncol 139:72–78
Mustoe TA (2008) Evolution of silicone therapy and mechanism of action in scar management. Aesthetic Plast Surg 32:82–92
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700
Higgins JPT GS Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://www.cochrane-handbook.org. Accessed 19 June 2023
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA (2011) The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Guyatt G, Gutterman D, Baumann MH, Addrizzo-Harris D, Hylek EM, Phillips B, Raskob G, Lewis SZ, Schünemann H (2006) Grading strength of recommendations and quality of evidence in clinical guidelines: report from an american college of chest physicians task force. Chest 129:174–181
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Ahn S, Sung K, Kim HJ, Choi YE, Lee YK, Kim JS, Lee SK, Roh JY (2020) Reducing Radiation Dermatitis Using a Film-forming Silicone Gel During Breast Radiotherapy: A Pilot Randomized-controlled Trial. In Vivo 34:413–422
Chao MWTSS, Kai C, Baker C, Jassal S, Law M, Cheng M, Zantuck N, Yu V, Stoney D, Loh SW, Bevington E, Chew G, Hyett A, Guerrieri M, Ho H, Ng M, Wasiak J, Foroudi F (2019) StrataXRT is non inferior to Mepitel Film in preventing radiation induced moist desquamation. Radiother Oncol 133:S704–S705
Omidvari S, Eskandari Z, Nasrollahi H, Ahmadloo N, Ansari M, Hamedi SH, Khanjani N, Kadkhodaei B, Mosalaei A, Mohammadianpanah M (2022) The Investigation of Prophylactic Effect of StrataXRT Gel on Radiation-Induced Dermatitis in Breast Cancer Patients: A Randomized Clinical Trial. Middle East J Cancer 13:293–298
Wright CY, Karsten AE, Wilkes M, Singh A, du Plessis J, Albers PN, Karsten PA (2016) Diffuse Reflectance Spectroscopy Versus Mexameter® MX18 Measurements of Melanin and Erythema in an African Population. Photochem Photobiol 92:632–636
Freedman GM (2014) Topical Agents for Radiation Dermatitis in Breast Cancer: 50 Shades of Red or Same Old, Same Old? Int J Radiat Oncol Biol Phys 90:736–738
Tripepi G, Chesnaye NC, Dekker FW, Zoccali C, Jager KJ (2020) Intention to treat and per protocol analysis in clinical trials. Nephrology 25:513–517
Chan RJ, Blades R, Jones L, Downer TR, Peet SC, Button E, Wyld D, McPhail S, Doolan M, Yates P (2019) A single-blind, randomised controlled trial of StrataXRT® - A silicone-based film-forming gel dressing for prophylaxis and management of radiation dermatitis in patients with head and neck cancer. Radiother Oncol 139:72–78
O’Dell K, Kearney R (2018) Feasibility study: use of a silicone gel in head and neck skin care. J Med Radiat Sci 65(S1)
Rutten LI (2018) Feasibility of Strata XRT in the Treatment of Radiation Dermatitis in Head and Neck Cancer Patients (Thesis, Bachelor of Radiation Therapy with Honours). University of Otago
Villandiego I, Aramberri S (2018) The Use of an Innovative Film-Forming Wound Dressing in the Treatment of Radiation Dermatitis during Concomitant Chemotherapy. J Cancer Ther 09:1048–1056
Montazeri A (2009) Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008. Health Qual Life Outcomes 7:102
Blades R (2020) A cost-effectiveness analysis of a silicone film-forming gel versus 10% glycerine in patients with head and neck cancer. In: Book A cost-effectiveness analysis of a silicone film-forming gel versus 10% glycerine in patients with head and neck cancer. Queensland University of Technology, City
Acknowledgments
None.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Shing Fung Lee and Henry Wong performed title and abstract screening, full-text screening, resolved conflicts in screening and data extraction. Adrian Wai Chan, Milena Gojsevic, KiHoon Sung, Samantha K.F. Kennedy, Thenugaa Rajeswaran assisted with systematic review, analyses, and manuscript drafts. Tara Behroozian, Pierluigi Bonomo, and Mami Ogita provided expertise on methodology, interpretation of results, and revision of manuscript drafts. Pierluigi Bonomo, Mami Ogita, Jason C. Ye, David Chia, Michael Chao provided clinical expertise on radiation therapy, interpretations of results, and manuscript drafts. Raymond Chan provided expertise in StrataXRT utilization and methodology. Edward Chow is the senior author of the manuscript and provided oversight for the whole project. Shing Fung Lee and Saba Shariati wrote the main manuscript text and prepared all figures and tables. Saverio Caini and Saba Shariati helped prepare figures. Julie Ryan Wolf and Corina van den Hurk are co-Chairs of MASCC Oncodermatology Study Group and assisted with revision of manuscript for final version, as well as supportive oversight for the project. All authors edited the manuscript and provided comments. All authors have read and approved the final version.
Corresponding author
Ethics declarations
Ethics approval
Not applicable for systematic review and meta-analysis.
Consent for publication
Not applicable for systematic review and meta-analysis.
Consent for participate
Not applicable for systematic review and meta-analysis.
Competing interests
Edward Chow received the free supply of StrataXRT in a pilot study of StrataXRT in the prevention of radiation dermatitis in breast cancer. Raymond J Chan received funding support from Moogoo and Stratpharma to conduct clinical trials and delivering educational sessions in relation to prevention and management of radiation dermatitis. All other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 148 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, S.F., Shariati, S., Caini, S. et al. StrataXRT for the prevention of acute radiation dermatitis in breast cancer: a systematic review and meta-analysis of randomized controlled trials. Support Care Cancer 31, 515 (2023). https://doi.org/10.1007/s00520-023-07983-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07983-1