Abstract
Aim
To assess clinical use and patient outcome of photobiomodulation (PBM) for oral mucositis (OM) prevention and treatment among specialized practitioners.
Methods
A poll was emailed to the members of the Mucositis Study Group of MASCC/ISOO. The PBM parameters used by the respondents were analyzed using exploratory statistical methods to identify combinations of PBM parameters (patterns) that characterize the variance in the protocols (principal component analysis).
Results
Responses were received from 101 MSG members, with 78 providing analyzable data. Most of the responders were dental practitioners or oral medicine specialists. PBM was used by 59% of the responders for OM or targeted therapy stomatitis. Technical parameters varied widely. Most responders used wavelengths ∼650 nm intra-orally. The spot-size and distance from the tissue were the main factors driving the variation. All PBM users noted that PBM relieved pain, either immediately or a delayed effect. High likelihood of pain relief (measured as responder’s report of pain relief in 67–100% of patients) was reported by 22% and 19% of PBM users for immediate pain relief and delayed pain relief, respectively. The most common reported barriers to using PBM were financial considerations, time constraints, lack of training or experience and concern about the potential for malignant transformation or increased risk of cancer recurrence.
Conclusions
The use of PBM for OM prevention or treatment is in early phases of adoption in practices, facing some obstacles to implement it. A wide variation in technical parameters was found. Nonetheless, responses indicate that PBM provided pain relief.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral mucositis (OM) is a major complication of cancer therapies including chemotherapy (CT), radiotherapy (RT), and hematopoietic cell transplantation (HCT) [1]. More recently, the scope of OM was broadened to include targeted therapy-associated oral toxicities and immunotherapy-related oral adverse effects [2]. OM is associated with significant pain and impaired function, often reported to be the most debilitating toxicity of cancer treatment [3, 4]. In addition, OM may have systemic sequelae such as infection and in the setting of HCT, it is associated with increased mortality [5]. OM may cause cancer therapy dose reductions and even complete treatment cessation, obviously interfering with anti-cancer treatments [5, 6]. Consequently, OM leads to significant health care costs due to the increase in supportive care measures and extended hospitalizations [5,6,7]. These serious issues have driven much research into prevention and/or treatment of OM.
PBM is a form of light therapy that uses non-ionizing light sources including lasers, light-emitting diodes, and broadband light, in the visible and near infrared spectrum [8]. It is a non-thermal process involving endogenous chromophores that elicit photophysical and photochemical events in various biological pathways [8, 9]. PBM promotes wound healing, provides pain relief and has anti-inflammatory effects [8,9,10].
Evidence-based recommendations for the management of OM have been provided by the Clinical Practice Guidelines of the Multinational Association of Supportive Care in Cancer and International Society of Oral Oncology (MASCC/ISOO) [1]. A systematic review assessing the use of photobiomodulation (PBM) for prevention and treatment of OM was performed and evidence-based clinical guidelines were developed for specific cancer patient populations [10]. The panel recommended the use of intra-oral PBM therapy for the prevention of OM in (1) Adult patients treated with HCT conditioned with high-dose CT, with or without total body irradiation; (2) adults treated with RT or RT-CT for head and neck cancer (HNC). Specific PBM treatment parameters were recommended for each indication.
The PBM protocols used to manage OM reported in the literature vary greatly [10, 11], and clinicians may also be using unreported protocols successfully. Therefore, the objective of this poll was to assess the actual clinical use of PBM for the prevention and treatment of OM among specialized practitioners who are members of the Mucositis Study Group (MSG) of the MASCC/ISOO, and the possible challenges and barriers to implementing this treatment modality.
Methods
MSG poll process
The poll was sent as an online questionnaire to the 430 MSG members using the MASCC/ISOO electronic distribution list, out of which 352 are clinicians. Two weeks after the first message, a reminder email was sent. The poll was closed 1 month after the first message was sent.
Questionnaire
The questionnaire (Appendix 1) included questions regarding clinical conditions in which PBM is applied for prevention or treatment of OM in adults, technical parameters of PBM used for OM prevention and treatment, estimated efficacy based on the responder’s experience, and challenges and barriers encountered in implementing PBM.
There were also similar questions about PBM therapy in pediatric patient population, including questions about the acceptance of PBM therapy by the children patients and their parents, and the technical parameters used for OM prevention and/or treatment.
The questionnaire also included questions about responder’s age, gender, profession, type of institute, main cancer patient population treated, years of experience and country of practice. In some questions, the respondents were able to indicate more than one answer, as can be seen in the questionnaire that is provided as supplementary information (Appendix 1). The results were calculated as percentage of responders or responses, as appropriate in each question. Questions regarding treating children were provided in a separate questionnaire.
The questionnaire was validated before distribution by a group of MSG volunteers.
Ethical considerations
The study was approved by the Institute Review Board of the Faculty of Medicine, at the Hebrew University, Jerusalem, Israel (#25052021). The MSG members were informed that the research would not necessarily benefit them, but may provide information for other health care professionals managing patients with OM. Participants could opt-out at any time. The anonymity of the responders was maintained. All data was stored in a secure manner and only accessible to authorized personnel.
Study sample and data cleaning
The dataset was assessed for logical inconsistencies based on the following exclusion criteria: responses from non-clinicians, and non-analyzable data (i.e., no response to any of the questions). Likewise, spot size units were standardized to metric dimensions (centimeter square). After clearing the inconsistencies, the dataset was locked.
Statistical analysis
Data was tabulated and descriptive analysis performed using MS Excel software. The treatment protocols were stratified based on wavelength, fluence, duration of treatment and efficacy. Protocols used for prevention were assessed for ‘immediate efficacy’ and ‘delayed efficacy’. Treatment protocols were assessed for immediate efficacy only, assuming that pain relief is noted immediately.
Principal component analysis (PCA) was conducted using Stata Statistical Software (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). PCA is an exploratory method that is used to identify combinations of characteristics of PBM setting that capture the largest possible variation across all PBM characteristics in the responses. Eigenvectors of eigenvalue >1 were considered as a strong indication of a repeated pattern.
Results
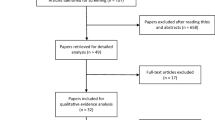
Response rate
One hundred and one entries were recorded. After removing entries with no answers and responses from non-clinicians, 78 entries with analyzable data remained (78 out of 352; 22.2% response rate).
Demographics
The average age of the responders was 48.8 ±11.7 years (range 27–75). The female-to-male ratio was 65:35. Most of the responders were dental practitioners or oral medicine professionals (65%), followed by physicians (18%), nurses (7%) and clinical researchers (4%). Most of the responders were affiliated with a university medical center (51%) or with a hospital (29%). Other responders worked in a private practice (12%), research institutes (6%), or in community clinics (2%).
Most of the responders had extensive clinical experience providing care for cancer patients, with 29% having more than 25 years of experience, 22% having 16–25 years, 35% having 6–15 years, and the remaining 14% with 0–5 years. We received responses from almost all continents. Most of the responders were from Brazil (27%), followed by USA (16%) and Italy (16%), Canada (5%), Australia (5%) and Japan (4%). Additional responses were received from India, Portugal, the Netherlands, Austria, Belgium, France, Greece, Israel, the UK, Spain and Turkey. The main cancer patient populations treated by the responders were HNC patients (29%), hematologic cancer patients (22%), solid cancer patients (20%), HCT patients (18%) and other oncologic patients (11%).
The estimated number of patients with cancer therapy–associated OM that the responders encountered during the 3 months before the poll was over 15 patients by 43% of the responders; 6–15 patients by 32%; 1–5 patients by 17%; 7% estimated no direct patient care.
Clinical use of PBM and type of OM treated with PBM
Fifty-nine percent of the responders reported using PBM for OM prevention or treatment while 41% reported that they do not use PBM for this purpose. The most common type of OM treated with PBM was due to RT to the head and neck (29%) as well as due to CT (29%), followed by HSCT (26%) and targeted therapy (16%).
Technical PBM parameters for OM prevention
The parameters reported for OM prevention varied greatly (Table 1), according to 28 out of the 48 responders whose survey included the details of the protocol they used. Two responders used an extra-oral approach, 24 used an intra-oral approach and 2 responders used both. Among those using an intra-oral approach, 17 different protocols using red-light (including 630, 645, 650, 660, 670 nm wavelengths) were reported with wide variation among the parameters (Table 1). One responder taking an intra-oral approach used near-infra-red (NIR) range (880 nm). The two responders using both intra-oral and extra-oral approaches used red-light. Additional 7 responders included a partial description of their protocol. When broken down according to the country of origin, the laser setting parameters varied greatly.
Technical PBM parameters for OM treatment
The technical parameters reported to be used for OM treatment are summarized in Table 1 with 27 responses recorded. Three responders reported employing a combined approach, and 24 used an intra-oral approach. Fourteen protocols using red-light were reported for the intra-oral approach with wide variation among the various parameters (Table 1). Three responders using an intra-oral approach utilized NIR range (880 nm and 970 nm). Of those using a combined approach, two used red-light and one used NIR (880 nm). Seven additional protocols with partially missing data were recorded. When broken down according to country of origin, the laser setting parameters were extremely variable.
PBM parameters for OM in pediatric patients
Over 15% of responders reported using PBM for OM prevention and treatment in pediatric patients. The majority (68.4% and 79%, respectively) reported a 100% parental acceptance rate and an 80–100% patient acceptance rate.
Technical PBM parameters for OM prevention in pediatric patients
The technical parameters reported to be used for pediatric OM prevention varied greatly (Table 2). Eight responders used an intra-oral approach and 4 responders used both an extra-oral and intra-oral approach. They used two red-light wavelengths (645 and mainly 660 nm), with wide variation among the parameters (Table 2). The PBM was performed with a steady beam in a single spot by 83.3% of respondents and hovering above by 16.7%.
Technical PBM parameters for OM treatment in pediatric patients
The technical parameters reported to be used for pediatric OM treatment are summarized in Table 2. Nine responders reported employing an intra-oral approach, 2 responders used a combined approach, 1 did not respond. All responders used two red-light wavelengths (645 and mainly 660 nm), with wide variation among the parameters (Table 2). The PBM was performed with a steady beam in a single spot by 75% of respondents and by hovering above by 16.7%.
Pain reduction efficacy
Total of 37 responses were received from 25 responders (more than one answer was possible for this question). All responders estimated some level of pain reduction efficacy of PBM therapy. Overall, responses indicated there was immediate pain relief more commonly than delayed pain relief. The immediate effect was estimated in up to 33%, 34–66% and 67–100% of patients by 16%, 24% and 22% of the responses, respectively. Delayed pain relief was estimated in up to 33%, 34–66% and 67–100% of patients by 3%, 16% and 19% of the responses, respectively.
Table 3 presents all the protocols reporting an immediate effect that were fully described by the responders. The protocols are stratified by the duration of treatment, ordered by the wavelength and fluence, alongside their reported efficacy. These protocols were used for PCA.
Among the 12 responses regarding short course protocols aimed at OM treatment, immediate efficacy of less than 33% was reported by 4 participants, of 34–66% by 5 participants, and of 67–100% by 3 participants. Delayed efficacy of 67–100% was reported by one responder for short course protocols aimed at OM treatment.
Among 14 responses regarding short courses protocols using red-light aimed at OM prevention, an immediate efficacy of up to 33% was reported by 4 participants, 34–66% by 5 participants, and 67–100% by 5 participants. Delayed efficacy for the prevention protocols was reported as 34–66% by 3 participants, and 67–100% by 6 participants.
Due to the variability of the parameters of the treatment protocols, Exploratory Principal Component Analysis was used to identify combinations of the 12 variables in the PBM protocols that explain the immediate efficacy of treatment reported by the responders (Table 4). The first 4 principal components (PCs) explained 79% of the total variance, and had an Eigenvalue >1. The first PC (PC1) explains 34% of the variance and the second PC (PC2) explained 22% of the variance. Table 5 presents the combination of PBM parameters that forms each of the four principal components. The PC1 is characterized by ‘hovering above’ (as opposed to ‘steady’), combined intra-oral and extra-oral approach, more days of PBM treatment, using a non-red-light wavelength (800–808, 940–970 nm), more time per spot, and larger spot size (Table 5). PC2 is characterized by a combination of larger spot size, greater distance from the tissues, and using a red-light wavelength (630–670 nm). The third principal component (PC3) is characterized by a combination of using 940 nm wavelength and higher fluence. Finally, the fourth principal component (PC4) is characterized by a combination of higher irradiance and a greater number of sites.
Challenges and barriers to PBM use
The most common reported barrier was ‘financial considerations’, in both users and non-users, 45% and 50%, respectively (Figure 1). Other common hindrances reported by users were time, ‘concerns about malignant transformation or recurrence’, ‘country-specific regulations’ and ‘patient refusal’. Among non-users, additional common barriers were ‘lack of experience’, ‘time’, and ‘lack of scientific evidence’. In respect to the country of origin, among the countries with the highest number of responses (Brazil, Italy, USA), ‘financial considerations’ was the most common barrier among responders from Brazil and USA, whereas ‘time constraints’ was the most common barrier among responders from Italy.
Barriers for using PBM therapy in users and non-users. The x-axis represents the percentage of responses out of the number of clinicians that use PBM therapy (‘users’) (n=64) and number of clinicians that do not use PBM therapy (‘non-users’) (n=32). The question about barriers for implementation of PBM therapy allowed multiple answers per responder
Discussion
There is strong evidence for PBM therapy use for OM prevention and management of OM related pain [1]. However, the literature does not describe how long after treatment pain relief is usually experienced and the evidence for an immediate reduction in pain is relatively weak [12]. Although there are a lot of publications on PBM therapy, they describe many protocols for the prevention of OM, with different laser devices; therefore, it is very challenging to formulate a universally applicable protocol based on the literature. In this study, we gathered information regarding PBM therapy protocols for the management of OM in cancer patients from a large international group of professionals.
The results of the survey show that PBM is frequently used to treat established OM, not only for OM prevention. An intra-oral approach was employed more often than a combined intra and extra-oral approach. We found great variability in PBM protocols, as previously reported [1, 13]. Most responders used wavelengths ∼650 nm (range 630–670 nm), also consistent with the literature [13]. This may reflect the wavelengths that are emitted by the commercially available laser devices, and not necessarily the preferences of the clinician.
All users noted that PBM reduced pain to a certain extent as expected among professionals choosing this treatment modality. Overall, there were more reports of immediate pain relief than delayed effects (62% vs. 38%). Interestingly, among the long courses (i.e., those used to prevent OM), immediate pain relief was reported only in a smaller portion of the patients (relief in up to 33% of patients was reported by 20% of responders, and relief in 34–66% of patients was reported by 40% of the responders). This suggests that many of the patients did not experience immediate relief during these PBM therapy courses. Delayed pain relief from the long courses benefited some, but not all, patients (20% of the responders reported delayed pain relief in 67–100% of patients). While we do not have a way to predict the response to the PBM therapy, it is important to inform patients that the treatment may not be effective at all, or that the beneficial effect of treatment is built up over time. Furthermore, the low efficacy highlights the need to assess the cost-to-benefit ratio regarding expense, time, and manpower required to deliver PBM treatment. For example, if a long duration protocol leads to a modest immediate pain relief of established OM, it may be better to invest the time and manpower in other protocols for treatment of established OM with proven immediate pain relief.
Our vision was to be able to find a formula that would consider and integrate the data regarding each parameter of the PBM protocol and be used to predict treatment outcome. Unfortunately, the data did not lend itself to this type of analysis as the sample size did not allow estimation of relationships between the parameters and outcomes. Therefore, due to the complexity and variation in the protocols involved, we used exploratory principal component analysis to identify combinations of parameters that identified the most prevalent combinations of parameters in protocols reporting immediate pain relief. PCA is a multivariate technique that analyzes data in which observations are described by several inter-correlated quantitative dependent variables [14]. It extracts important information and represents it as a set of new orthogonal variables called principal components. This analysis shows which features (i.e., PBM treatment parameters) are most important in capturing the variance in the data. Four repeating patterns (4 PCs) explained most of the variance between the protocols. For each PC, the analysis identified the main parameters that influenced it. The PCA identified that spot-size and the distance from the tissue were the PBM parameters that accounted for most for the variance in protocols reporting immediate effect when using a 630–670 nm laser (described in PC2). Since the spot-size is determined by the laser device, the distance from the tissue seems to be a critical factor in treatment success. The PCA identified that the driving PBM parameters for the protocols using wavelengths ∼800 nm and 940–970 nm were hovering hand-motion, a combined approach (extra- and intra-oral), longer treatment duration per site, and longer treatment courses. However, the number of observations was small. Future large-scale studies should examine whether these parameters explain the superior efficacy of certain protocols.
This survey revealed that a minority of specialists use PBM in pediatric patients. As with PBM for adults, there was a high variability in the PBM parameters employed. PBM was used for both prevention and treatment of established OM, most protocols used wavelength of 645 nm and 660 nm, with an intra-oral approach. This aligns with the results of this survey for adults as well as with those reported in the literature for pediatric patients [1, 13, 15]. PBM therapy may be regarded as a patient-friendly treatment option for pediatric patients who may find it difficult to adhere to other therapeutic interventions. Nonetheless, the challenges to PBM in pediatric patient populations are the necessity for cooperation from patients and their parents, including the anxiety while wearing protective eyewear and issues of access and visibility in smaller mouths.
PBM has been proposed as a therapeutic and prophylactic modality with numerous indications in the field of supportive care for cancer patients [16], especially OM and other complications in the head and neck area [17, 18]. Despite the advantages of PBM as a friendly and non-pharmacological treatment [19], it has not yet been fully adopted by clinicians and medical centers. The main barrier to PBM use is financial, reported by both users and non-users. For users, this is probably related to chair time or manpower, whereas for non-users, it may be due to the cost of the laser device. There were also group-specific barriers. For users these were time, concerns about malignant transformation or recurrence, country-specific regulation and patient refusal. Among the non-users, the barriers were lack of experience, time, and insufficient scientific evidence.
The strengths of this study include data collection from professionals focusing on the management of OM, many with extensive experience in laser treatment. Data was collected internationally enabling analysis of the efficacy of different protocols, including quantifying the efficacy of protocols which are usually not described in the literature. In addition, we piloted the use of PCA and noted the value of this type of analysis which may be used in future research. The limitation of the study is the low number of responders providing all the details of their PBM protocol parameters. The global distribution of the poll did not compensate for the fact that PBM is an emerging treatment modality, and there was insufficient data for a regression analysis. Given that PBM is not yet embedded into routine clinical care universally, it seems that this limitation is inevitable. Finally, the nature of survey-type studies is that they rely on the recollections of the responders which may be inaccurate.
In summary, PBM therapy is used worldwide both for prevention and treatment of OM. The highly variable protocols yield beneficial effects that are not consistent in terms of response timing (immediate or delayed) or response rate. The main barrier for using PBM therapy is financial, with additional obstacles that are specific to responders who were able to use the technology versus those who were not. More studies are needed to identify PBM protocols that produce a consistent treatment outcome.
References
Elad S, Cheng KKF, Lalla RV, Yarom N, Hong C, Logan RM, Bowen J, Gibson R, Saunders DP, Zadik Y, Ariyawardana A, Correa ME, Ranna V, Bossi P (2020) MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer 126:4423–4431
Elad S, Yarom N, Zadik Y, Kuten-Shorrer M, Sonis ST (2021) The broadening scope of oral mucositis and oral ulcerative mucosal toxicities of anticancer therapies. CA Cancer J Clin 29:21704
Bellm LA, Epstein JB, Rose-Ped A, Martin P, Fuchs HJ (2000) Patient reports of complications of bone marrow transplantation. Support Care Cancer 8:33–39
Rose-Ped AM, Bellm LA, Epstein JB, Trotti A, Gwede C, Fuchs HJ (2002) Complications of radiation therapy for head and neck cancers. The patient’s perspective. Cancer Nurs 25:461–467
Haverman TM, Raber-Durlacher JE, Rademacher WM, Vokurka S, Epstein JB, Huisman C, Hazenberg MD, de Soet JJ, de Lange J, Rozema FR (2014) Oral complications in hematopoietic stem cell recipients: the role of inflammation. Mediators Inflamm 378281:10
Sonis ST, Oster G, Fuchs H, Bellm L, Bradford WZ, Edelsberg J, Hayden V, Eilers J, Epstein JB, LeVeque FG, Miller C, Peterson DE, Schubert MM, Spijkervet FK, Horowitz M (2001) Oral mucositis and the clinical and economic outcomes of hematopoietic stem-cell transplantation. J Clin Oncol 19:2201–2205
Elting LS, Cooksley C, Chambers M, Cantor SB, Manzullo E, Rubenstein EB (2003) The burdens of cancer therapy: clinical and economic outcomes of chemotherapy‐induced mucositis. Cancer: Interdisciplinary International Journal of the American Cancer Society 98:1531–1539
Hamblin MR (2016) Photobiomodulation or low-level laser therapy. J Biophotonics 9:1122–1124
Hamblin MR (2017) Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys 4:337–361
Zadik Y, Arany PR, Fregnani ER, Bossi P, Antunes HS, Bensadoun RJ, Gueiros LA, Majorana A, Nair RG, Ranna V, Tissing WJE, Vaddi A, Lubart R, Migliorati CA, Lalla RV, Cheng KKF, Elad S (2019) Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer 27:3969–3983
Elad S, Arany P, Bensadoun RJ, Epstein JB, Barasch A, Raber-Durlacher J (2018) Photobiomodulation therapy in the management of oral mucositis: search for the optimal clinical treatment parameters. Support Care Cancer 26:3319–3321
Sandoval RL, Koga DH, Buloto LS, Suzuki R, Dib LL (2003) Management of chemo- and radiotherapy induced oral mucositis with low-energy laser: initial results of A.C. Camargo Hospital. J Appl Oral Sci 11:337–341
da Silva BM, Prosdócimo ML, Gasparini LR, de Araujo MR, Amenábar JM (2022) Most used photobiomodulation dosimetry parameters to treat oral mucositis after preconditioning for hematopoietic stem cell transplantation: systematic review and meta-analysis. Support Care Cancer 30:3721–3732
Konishi T (2015) Principal component analysis for designed experiments. BMC Bioinform 18:1471–2105
Patel P, Robinson PD, Baggott C, Gibson P, Ljungman G, Massey N, Ottaviani G, Phillips R, Revon-Rivière G, Treister N, White M, Cabral S, Dupuis L, Sung L (2021) Clinical practice guideline for the prevention of oral and oropharyngeal mucositis in pediatric cancer and hematopoietic stem cell transplant patients: 2021 update. Eur J Cancer 154:92–101
Robijns J, Nair RG, Lodewijckx J, Arany P, Barasch A, Bjordal JM, Bossi P, Chilles A, Corby PM, Epstein JB (2022) Photobiomodulation therapy in management of cancer therapy-induced side effects: WALT position paper. Front Oncol 12:927685
Gavish L, Zadik Y, Raizman R (2021) Supportive care of cancer patients with a self-applied photobiomodulation device: a case series. Support Care Cancer 29:4743–4749
Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR, Barasch A, Migliorati CA, Milstein DM, Genot MT, Lansaat L, van der Brink R, Arnabat-Dominguez J, van der Molen L, Jacobi I, van Diessen J, de Lange J, Smeele LE, Schubert MM, Bensadoun RJ (2016) Low-level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 2: proposed applications and treatment protocols. Support Care Cancer 24:2793–2805
Zadik Y (2019) Photobiomodulation for the palliation of oral mucositis in cancer patients: the future is here. Future Oncol 15(32):3647–3649
Acknowledgements
The authors are grateful Praveen Arany, DDS, PhD, Eduardo Fregnani, DDS, PhD and Alessandra Majorana, DMD, MS, PhD for their helpful advice. This endeavor would not have been possible without MASCC/ISOO and its Mucositis Study Group, who continually strive to improve the supportive care of people with cancer. The authors thank MASCC/ISOO executive teams for their continuous support, and to the MASCC administrators for distributing the survey. Likewise, the authors thank for the members of the Mucositis Study Group of MASCC/ISOO for participating in this survey.
Availability of data and materials
At request.
Author information
Authors and Affiliations
Contributions
Ragda Abdalla-Aslan, Yehuda Zadik and Sharon Elad created the concept and composed the content of the poll, with feedback from all the coauthors. Sharon Elad coordinated the distribution of the survey. Noam Yarom managed the logistics of the electronic survey platform. Yehuda Zadik managed the IRB application. Orna Intrator conducted the statistical analysis. Sharon Elad and Ragda Abdalla-Aslan wrote the main manuscript. Elena Bardellini initiated and drafted the manuscript’s part about the pediatric patient population. All the coauthors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institute Review Board of the Faculty of Medicine, at the Hebrew University, Jerusalem, Israel (#25052021). ). This study was carried out in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Consent to participate
Informed consent was obtained from all individuals participating in the study by agreeing to fill in the survey.
Consent for publication
There is no personal data published in this study. However, all participants were informed that their deidentified data may be published for scientific purposes.
Conflict of interest
Yehuda Zadik reports personal fees for lectures, and equipment receipt, from Erika Carmel Ltd, outside the submitted work. Paolo Bossi reports consultation fees from Angelini. The remaining authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abdalla-Aslan, R., Zadik, Y., Intrator, O. et al. Clinical use of photobiomodulation for the prevention and treatment of oral mucositis: the real-life experience of MASCC/ISOO members. Support Care Cancer 31, 481 (2023). https://doi.org/10.1007/s00520-023-07919-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-023-07919-9