Abstract
Purpose
Being able to work improves the quality of life of patients with cancer. Much is known about the return to work process of cancer survivors. Yet, studies focusing on the experiences of patients with advanced cancer who want to return to work or stay employed are scarce. Therefore, we aimed to explore the perceptions of patients with advanced cancer regarding work resumption and work retention and the barriers and facilitators they may experience.
Methods
Semi-structured interviews were conducted. Patients were included if they: (1) were diagnosed with advanced cancer, (2) worked in paid employment at time of diagnosis, and (3) were currently back in paid employment or had the intention to return to paid employment. Participants were recruited through clinicians and patient organizations. Interviews were transcribed and thematically analysed using ATLAS.ti.
Results
Fifteen patients (87% female, mean age 52 (SD 4; range 41–64)) were individually interviewed. Four main themes emerged from the data: (1) holding on to normalcy, (2) high understanding and divergent expectations, (3) social discomfort calls for patient-initiated alignment, and (4) laws and regulations require patient empowerment.
Conclusion
Paid employment can contribute to the quality of life of patients with advanced cancer. The findings of this study might correct erroneous preconceptions about the work ability and work intention of patients with advanced cancer. Tools already developed for employers to support reintegration of patients with cancer should be further explored and translated to patients with advanced cancer.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In Europe, there are an estimated 3.9 million new cancer diagnoses annually [1]. In the Netherlands, it concerns approximately 124,000 individuals, of which an estimated 38,000 have advanced cancer [2]. About half of the patients diagnosed with advanced cancer is between 18 and 65 years old and thus of working age [2]. Improvements in medical care are enabling patients with cancer to live longer and to increase their ability to work during and following treatment [3]. While the financial incentive to remain in paid employment can be considerable, being able to work additionally contributes to a sense of normalcy, daily structure, and social belonging for patients with cancer [4]. Work participation can therefore significantly increase cancer patients’ quality of life [5].
Work resumption and work retention are already challenging for cancer patients who have been treated with curative intent. That is, the overall risk of unemployment among cancer survivors is 1.4 times higher than those who have never been diagnosed with cancer [6]. Numerous obstacles, such as physical and/or psychosocial consequences of a cancer diagnosis and related treatment [7], but also a perceived lack of support and understanding from the work environment, may hinder cancer patients from participating in paid work [8, 9]. It is expected that these obstacles are even more complex for patients with advanced cancer.
Previous studies showed that, at the beginning of the cancer diagnosis and treatment trajectory, there is generally a strong motivation from the employer to facilitate return to work (RTW). This declines later on, during (long-term) sick leave, especially when the disease remains stable for a while [9]. Additional issues regarding RTW and work retention in patients with advanced cancer include the impact of the disease on their work capabilities, regular medical appointments, and coping with the reality of dying within an uncertain timeframe. Nonetheless, Glare and colleagues indicated that work continues to stay a meaningful topic in a growing group of patients with advanced cancer [10].
Currently, little is known about the experiences of patients with advanced cancer regarding work participation, and elaboration of their perceptions on work resumption and retention is needed. Therefore, we aimed to qualitatively explore the experiences and perspectives of patients with advanced cancer, regarding work resumption and work retention.
Methods
Design and participants
A qualitative study was performed, in which semi-structured interviews with patients with advanced cancer were conducted. Patients were eligible to participate if they were: (i) diagnosed with advanced cancer (i.e. incurable cancer, usually metastatic) and aware of the incurability of their disease; (ii) between 18 and 65 years of age at time of the interview; (iii) working in paid employment at time of diagnosis and the year prior to diagnosis; (iv) in paid employment, or (partly) on sick leave, or receiving (partial) disability benefit/unemployment benefits at time of the interview; (v) having the intention to return to paid employment, if not at work; and (vi) able to speak Dutch. Patients with severe psychological symptoms were excluded. The advanced, incurable stage of their disease was assessed by an explicit question in the brief questionnaire completed by the patients. Also, via telephone contact, all inclusion criteria were explicitly confirmed by the patients, including the first criterion ‘diagnosed with advanced cancer (i.e. incurable cancer, usually metastatic) and aware of the incurability of their disease’. An assessment of mental health problems was made by physicians based on medical records and their expertise. In the case of recruitment through social media, the researcher checked by telephone whether patients were able to participate in the study.
Study procedure and data collection
A purposive sampling strategy was applied, and participants were included and interviewed until data saturation was reached, i.e. no new (sub-)themes arose from the data. Clinicians recruited patients during outpatient clinic visits at the oncology or pulmonology departments of two different hospitals: one academic hospital and one teaching hospital. Patients with lung cancer are seen at the pulmonology department. In recent years, many new therapies have become available for these patients, making them a specific group, sometimes able to live longer with incurable lung cancer. If a patient was interested in participation, an information package was provided by the clinician, containing an information letter, informed consent form, a short questionnaire indexing sociodemographic details, work-related characteristics and disease-related information, and a prepaid return envelope. Upon receipt of the completed documents, eligible patients were invited for an interview. Furthermore, study information was announced on various social media platforms, including the platforms of the Dutch Federation of Cancer Patients Organisations. Interested patients could contact the research team, after which the procedure was identical to the clinician route described above.
A semi-structured interview guide was compiled based on previous studies on the RTW experiences of patients with cancer [4, 7,8,9, 11] and on the expertise of the research team (Appendix 1). The interview guide was tailored to three possible employment situations: (1) those who were on sick leave and received sickness and/or (partial) disability benefits, (2) those who had successfully (partially) returned to their former or a new employer, and (3) those who were job seeking. The predefined interview guide consisted of five themes: (i) changes in work situation (from pre-diagnosis until time of the interview); (ii) the meaning of work; (iii) the role of the employer in returning to work and/or work retention and experienced support (e.g. support from colleagues, work accommodations, or non-workplace support); (iv) Dutch (long-term) sick leave legislation (e.g. regarding reintegration, sickness and disability benefits); and (v) work-related needs and recommendations.
From March 2021 to May 2021, fifteen interviews (with a mean duration of 56 min) were conducted by two research interns trained in conducting qualitative research (DB and EvA). Both interns were supervised by authors AZ, LB, and SD (a PhD candidate, postdoctoral researcher, and senior researcher, respectively, all with a research focus on psychosocial oncology and/or palliative care and experience in conducting qualitative research (e.g. [12,13,14])). Due to COVID-19, the interviews were conducted online through Microsoft Teams or by telephone. Interviews were audio-recorded and transcribed verbatim. No repeat interviews were held, and transcripts were not returned to participants. For reporting, the COnsolidated criteria for REporting Qualitative research (COREQ) checklist was used [15].
Data analysis
Thematic analyses were conducted based on the six phases described by Braun et al. [16], using the qualitative software package ATLAS.ti 8 [17]. Two researchers (DB and LB) independently coded two transcripts to establish inter-observer reliability of the coding procedure [18]. The constant comparative method was used to compare codes within and between interviews. Frequent meetings with the research team (DB, LB, SD, AZ, EvA) led to understanding of the participants’ experiences and subsequently the identification of main themes and their interrelationships. Relevant quotes have been selected to illustrate (sub)themes. IBM SPSS Statistics version 24 was used to analyse data from the questionnaire.
Results
Participant characteristics
Fifteen participants (87% women) between 41 and 64 years of age (mean age 52; SD 4) were interviewed. Although diagnoses varied, most participants were diagnosed with an advanced form of breast cancer (47%). Participants were divided into three different employment situations: on sick leave at current employer (n = 5), working (n = 8), and job seeking (n = 2) (Table 1).
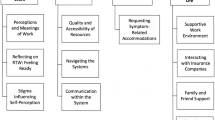
In total, four themes have been identified. The identified themes follow the emotional and practical journey patients with advanced cancer may go through when it concerns RTW or work retention. This process starts with the advanced cancer diagnosis and the initial impact it may have on a normality, such as work, in theme 1. This is followed by a phase, in which contradictions may occur, when an advanced cancer patient aims to RTW after sick leave, but the environment struggles because of different expectations, as described in theme 2. In theme 3, the focus is on the initiative the patient has to take to align with the environment and deal with issues, such as social discomfort, when it concerns RTW and work retention, and advanced cancer. Specific issues regarding laws and regulations and the attitude a patient is required to have throughout the whole journey are described in theme 4.
Holding on to normalcy
The key issue of this theme concerns the urgency of patients with advanced cancer to hold on to normality, when it concerns work, after receiving the diagnosis. After receiving the diagnosis of advanced cancer, participants said to feel detached from ordinary life and felt the urge to hold on to things that made them feel normal. They felt vulnerable in relation to the uncertain course of the disease, in which the prospect of dying is a persistent threat. Work was portrayed as a valuable asset in coping with these uncertainties:
It is necessary to hold on to things that belong to your life and work is part of that, even if it is only for a limited amount of hours per week. It prevents you from getting lost and keeps you going. I experienced this very strongly when it turned out that I had metastasized cancer. (Female, age 62)
For many participants, work became more meaningful after their advanced cancer diagnosis. Being able to work in general was said to contribute to their identity and allowed them to actively participate in society. Besides financial motives, most participants stated that being able to work also facilitates the opportunity to partake in social relations, e.g. to talk about something besides their advanced cancer, and to take part in the lives of other people, just like any other person. It provides a welcome distraction from the constant confrontation of being incurably ill:
Whether I’m at home or at work, the pain is there anyway. […] When I work, I forget everything. And yes, that is important to me. You don’t have to worry, you can just take care of others. The disease isn’t there for a while. (Female, age 60)
According to participants, tailored support is needed in order to RTW or retain work. Most participants described the need of one central person of contact, who could either address their work-related questions or refer them to appropriate support. Some expressed how helpful their occupational physician (OP) had been for them, whereas others said the OP’s support was not meaningful. While participants mentioned they valued the support of a clinician, most described a lack of attention for ways to maintain or regain a sense of normalcy, including through work, in hospitals:
I think it would have helped a lot if work had been included in my process from day one as a topic of conversation. I mean, that is such a big part of your life, for me anyway, you can’t just ignore it. (Female, age 64)
Some participants expressed that they did not voice their work-related concerns in the hospital setting, presuming that clinicians do not offer work-related guidance, especially when it concerns advanced cancer. In addition, some participants experienced differences in work-related support received at the hospital, when previously diagnosed with an early stage of their disease (i.e. work being more often discussed in the curative setting), compared to the current advanced stage.
High understanding and divergent expectations
The key issue of this theme is that employers generally have high understanding towards patients with advanced cancer during sick leave, but do not necessarily support patients with advanced cancer to (return to) work. Although experiences varied greatly, most participants experienced compassion, flexibility, and understanding from their employers regarding their (advanced) cancer diagnosis and subsequent sick leave:
My manager said: ‘Take your time, you’re not doing this for us, but you’re doing it for yourself, so do it at your own pace’. When that happened, a switch flipped for me, or so to speak. The tension was gone and I could finally relax. (Female, age 48)
While the understanding from employers was described as high, participants felt they did not seem to fulfil the expectation of their surroundings regarding their intention to RTW. For example, to be incurably ill and to RTW are usually perceived as incompatible extremes by the general public. Although participants experienced vast amounts of emotional support, they felt that family, friends, and employers often misunderstand participants’ desire to work:
There are some people who just don’t understand why I’m going to work at all or why I want to do that. They don’t understand. They don’t understand why I value work so much. (Male, age 49)
Many participants emphasized the importance of dispelling the stigma associated with advanced cancer. Choosing to work while being incurably ill was perceived as incompatible with society’s view of how people with incurable illness should fill their time. For example, they should primarily spend their time with loved ones and not bother about work. They said to feel an urgency in continuing a valuable and normal life while still possible. Moreover, they explicitly mentioned the urge to show that they are still a valuable member of society:
At one point, I really wanted to go back to my old contract, four days, and everyone just thought I was crazy for wanting that, but I thought, I’ll show them that I can come back. (Female, age 64)
Social discomfort calls for patient-initiated alignment
The key issue of this theme is that employers and colleagues may experience social discomfort when a patient with advanced cancer expresses the wish to RTW, during the actual reintegration process, and during work retention. In response to the apparent discomfort of employers and colleagues, patients may feel necessitated to initiate all communication regarding RTW/work retention planning with the social and work environment. During treatments, side-effects and the overall disease burden dominated the lives of participants. After treatment, the main issues hindering the transition to occupational reintegration were said to be the lingering side-effects such as decreased energy, concentration problems, and pain. Most participants said that despite being optimistic about their work capabilities, returning to work is difficult and overwhelming:
When I came home after the very first day back at work, I was so extremely tired and overwhelmed that I couldn’t do it the next day. I was actually supposed to come the next day, but I just couldn’t. I was exhausted for the rest of the week. (Female, age 48)
While struggling with the daily frustrations regarding the uncertainty of the course of the disease in relation to their future working life, it was considered important to gradually build up confidence and increase the workload. Often, changes in participants’ responsibilities, such as performing less physically demanding tasks or a decrease in working hours, helped them, for example, to manage fatigue. An employer who facilitates these options can be considered a great advantage.
Participants stressed the importance of social support and encouragement from colleagues, which was highly valued in the reintegration process:
If I didn’t have colleagues who were personally involved with me, and the other way around, I wouldn’t even be able to function. (Female, age 62)
Some participants stated being aware that the employer and colleagues are dealing with an employee who may bring uncertainty and social discomfort. However, in their opinion, there is a lack of discussion and insufficient attention for their situation, due to overly cautious behaviour from colleagues.
In the beginning, it was like, if you have lung cancer stage four, you’re not supposed to work anymore and that was emphasized by my colleagues, which I found quite difficult. (Female, age 64)
Participants described their situation as ‘social exclusion’. It felt like a burden to constantly demonstrate and explain the situation to colleagues. Furthermore, some mentioned that at the time of their diagnosis of advanced cancer, there was less interest from their colleagues compared to their previous curative cancer diagnosis:
The second time, when it becomes advanced, you notice that it’s actually a lot less [the support]. You get flowers, because it’s on the agenda, you get a coffee chat because that is how it should be, but then eventually that kind of stops I think that has to do with being treated with advanced care, because people don’t expect you to come back. (Male, age 49)
Due to the social discomfort in the workplace, participants felt necessitated to take initiative in most work-related communication, such as aligning expectations concerning RTW. Participants preferred a more open dialogue in the workplace, to ensure their concerns and needs were understood and their feelings were validated:
Dare to ask questions, because of course it’s intense when an employee comes up to you like, sorry, I don’t know how long I have to live. It could be just one year. It is understandable than an employer struggles to initiate the conversation, but don’t leave it up to the patient. (Female, age 40)
Laws and regulations require patient empowerment
The final theme is an overarching theme, in which the need for patient empowerment in dealing with difficulties in laws and finances is discussed. Participants generally experienced little difficulty in dealing with the Employee Insurance Agency, i.e. the Dutch institute responsible for implementing employee insurances. According to Dutch legislation, employees who have been absent from work for 2 years undergo a work disability assessment (or sooner, in case of an unfavourable prognosis) to evaluate their eligibility for disability benefits. One participant explained the ease with which the agency would hand out disability benefits to patients with advanced cancer:
The moment you mention the words ‘cancer’ and ‘terminal’, well in this case palliative, then yes, all the doors at the Employee Insurance Agency open. (Female, age 40)
In addition, participants felt OPs and employers were sometimes too eager in suggesting that they should apply for partial or full disability benefits:
When the radiotherapy was finished, they said: ‘Maybe we can start an early process to apply for the IVA (Full Invalidity Benefit Regulations)Footnote 1’. I thought that was very strange. I was only on sick leave for half a year and I thought, we are not there yet. I wondered if it was financially more beneficial for my employer. (Female, age 61)
One participant expressed her frustration regarding being a valuable employee, but not having had a salary raise in 10 years. She explained it as ‘a complex situation’, because a raise would lead to a decrease in her disability benefit:
People around me have had salary increases, but not me, because I would just get less disability benefits, which would amount to the same salary. In the past, this might not have been a problem, because people used to die much earlier. But now, I think a lot of people run into this problem. (Female, age 55)
Participants who had to seek a new job after treatment said to have dealt with constant rejection and setbacks in the process of job applications, even if they were overqualified for the job:
The fact that you are being treated with advanced care, does not make you attractive to employers, regardless of what you have to offer in terms of qualifications. [...] People just find it very uncomfortable. (Female, age 50)
Furthermore, participants mentioned that sometimes, they were only welcome at work as a volunteer. This did not bring them any satisfaction and made them feel underappreciated:
What bothered me at a certain point was that I was welcome in quite a few places, but just as a volunteer. […] It’s not right that I’m doing the same work as my colleague who has a fixed employment contract, and I do it as a volunteer, and I get a daily allowance of five euros. That doesn’t even cover my gasoline costs. (Female, age 50)
To be able to navigate the system and its regulations, participants identified patient empowerment as a key facilitating factor. They described how returning to sustainable work greatly depends on the participants’ strength and determination. Those who said to have an assertive attitude, who knew they wanted to retain work from diagnosis onwards, seemed to have more success in reintegration:
It all piled up quickly, but then again I am a fighter yes, in a sense that you can’t get rid of me. I’m just going to do my best to show them that I matter, which I did and it worked out well. (Female, age 62)
Discussion
Interpretation of main findings
Being diagnosed with advanced cancer can have a substantial impact on work participation. Firstly, the majority of participants explained how work became more meaningful in the face of advanced cancer, because it allowed them to contribute to society, instead of feeling rejected by it. This aligns with previous studies in the curative setting, describing how women with breast cancer often want to leave their sick role behind and secure their work role [19,20,21]. Many participants in our study wanted to continue a valuable life through work while still possible and get rid of the stigma. Several studies underlined the importance of being able to perform paid work while being in advanced cancer care [22, 23]. However, to be able to return to or retain work, the right support is needed. Previous research has shown that the support from a clinician in returning to work is often regarded as insufficient [9, 24]. Our study showed that patients value the support of a clinician, but experience low attention for work-related issues in the hospital.
Secondly, participants explained that employers were very understanding during sick leave, but did not expect participants to RTW and in some cases showed less understanding when participants expressed their desire to RTW. This is in contrast with a study of patients in the curative setting who experienced high support from their employer while reintegrating [25]. Although patients treated with curative intend may experience problems regarding employer’s support as well, patients with advanced cancer more often do not seem to fulfil the expectation of their social environment regarding being sick. Their work capabilities were often viewed with scepticism. This could be due to existing confusion of society at large between incurable or advanced cancer and terminal cancer. While participants’ perceptions of their own work capabilities and work intention were more or less optimistic, they preferred changes in work tasks and hours. This is consistent with previous research, which demonstrated how reduced work capability in patients with cancer can be managed [26, 27].
Thirdly, regarding the third theme, participants described their reintegration at work as tough and overwhelming. They highly valued active involvement and compassion from their employer and colleagues, of which the importance has been described in previous studies [28, 29]. However, participants experienced feelings of social discomfort among colleagues regarding their wish to RTW while undergoing advanced cancer treatment. This aligns with a Korean study, in which it was illustrated how individuals can have uncomfortable attitudes and are sensitive to topics relating to death [30]. The confrontation of a colleague with advanced cancer might cause them to reflect on their own mortality [31]. Nevertheless, patients felt that this required them to initiate and align communication regarding work and related expectations, which is experienced as burdensome.
Lastly, when it concerns ‘laws and regulations’, participants stressed the importance of being proactive and empowered while dealing with work-related legislation. Patients with advanced cancer explained that applying for jobs can be more difficult compared to the curative setting, due to the aforementioned complexity and stigma. Overall, participants emphasized the importance of their inner determination to go against all expectations of their surroundings. This was also reported by Brusletto et al. [32], who described the most important assets to return to sustainable work among cancer survivors as being their own strength, determination, and adaption skills.
Strengths and limitations
The main strength of this study is the added value of this topic, which was largely unexplored so far. Also, this study concerns a patient population that will inevitably grow in the future [33]. Further, the characteristics of the participants showed a broad range in age, diagnoses, and employment statuses, which offers an explorative insight.
However, some limitations must be taken into consideration. Firstly, selection bias, presumably due to volunteer bias, might be present, as most participants were women and highly educated. Due to this selection, differences regarding perspectives on cancer and return to and retaining work may be absent [34,35,36]. In addition, it is likely that patients with advanced cancer who are not doing well have declined participation or have not been asked by their physician to participate. The latter may be due to clinician gatekeeping: the tendency by which healthcare providers prevent access to patients who are eligible for participation [37]. Finally, it is possible that the point of view of patients who failed to RTW is missing in our study, as only patients who had the intention to RTW and/or felt physically well enough to do so signed up for participation.
Implications for practice and future research
Our findings underline the importance of addressing the stigma that ‘patients with advanced cancer are not able to work and/or should have no intention to work’. Creating awareness among employers about the abilities, work intention, and needs of patients with advanced cancer would contribute to their RTW and work retention. The findings also indicate that one point of contact, such as a specialized nurse or a case manager, to refer patients to adequate support would facilitate the work-related needs of patients. It is also recommended for clinicians to be more active in paying attention to work-related issues of the patients receiving advanced care. Support from hospital-based professionals can help to facilitate reintegration for these patients, by determining work readiness and making work a topic of discussion. This is not yet systematically offered, as described by Zegers et al. [38]. Yet, this may be offered by a specialized OP, who advises patients, their clinicians, and their employers regarding cancer and work. Since these implications align with those deriving from studies in the curative setting, reintegration interventions for the curative patient group might also be transferrable to the palliative setting.
Regarding future research, it would be preferable to include a larger sample size with more representation of the male gender and different educational backgrounds. More qualitative and quantitative research is recommended. Findings should be used to raise awareness on the possibilities of RTW and work retention of patients with advanced cancer among researchers, clinicians, stakeholders, and society. Interventions should be developed addressing stigma, improving communication, and increasing knowledge in general, about advanced cancer care and possibilities for RTW/work retention, to support these patients towards sustained employment. We recommend healthcare professionals to offer patients with advanced cancer tools focusing on increasing self-management and communication skills to support, empower, and navigate them through the process of RTW and work retention. Finally, we suggest to include patients with advanced cancer in RTW and work retention programmes or clinical trials.
Conclusion
Work can still be an important issue in the lives of patients with advanced cancer. Support from hospital staff and proactive attitudes from employers are needed, as patients have so far had to initiate almost all work-related communication themselves. Expectations regarding work between patients and relevant others do not always align, which may lead to social discomfort. Our findings might correct erroneous preconceptions about these patients’ work ability and work intention and enhance their overall experience during reintegration. Tools already developed for employers to support patients with cancer in reintegration should be further investigated and translated to advanced cancer patients.
Data availability
Not applicable.
Code availability
Not applicable.
Notes
In the Netherlands, the WIA (Work and Income according to Labour Capacity Act) contains four categories, of which the IVA (Full Invalidity Benefit Regulations) is the benefit for those durable and completely disabled. The WIA assessment regularly takes places after 2 years of sick leave, in which (most) employees receive 100% of their salary during the first and 70% of their salary during the second year of sick leave.
References
Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M et al (2018) Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 103:356–387. https://doi.org/10.1016/j.ejca.2018.07.005
IKNL (2020) Uitgezaaide Kanker In Beeld. Utrecht: IKNL, pag. 83–6. https://iknl.nl/getmedia/6ddb80c4-254f-4763-943f/1a50f5321b83/IKNL_uitgezaaidekankerinbeeld_rapport.pdf. Accessed 19-2-2021
Pryce J, Munir F, Haslam C (2007) Cancer survivorship and work: symptoms, supervisor response, co-worker disclosure and work adjustment. J Occup Rehabil 17(1):83–92. https://doi.org/10.1007/s10926-006-9040-5
Moore PM, Rivera S, Bravo-Soto GA, Olivares C, Lawrie TA (2018) Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003751.pub4
Duijts SF, Kieffer JM, van Muijen P, van der Beek AJ (2017) Sustained employability and health-related quality of life in cancer survivors up to four years after diagnosis. Acta Oncol 56(2):174–182. https://doi.org/10.1080/0284186X.2016.1266083
Braspenning I, Tamminga S, Frings-Dresen MH, Leensen M, de Boer A, Tikka C Verbeek JHAM, Munir F, Hemming S, Amir Z, Smith L, Sharp L, Haste A (2018) Rehabilitation and return to work after cancer—instruments and practices. Loughborough University, EU-OSHA. https://doi.org/10.2802/170868
Brown RF, Owens M, Bradley C (2013) Employee to employer communication skills: balancing cancer treatment and employment. Psychooncology 22(2):426–433. https://doi.org/10.1002/pon.2107
Ebede CC, Jang Y, Escalante CP (2017) Cancer-related fatigue in cancer survivorship. Med Clin 101(6):1085–1097. https://doi.org/10.1016/j.mcna.2017.06.007
Hoefsmit N, de Rijk A, Houkes I (2013) Work resumption at the price of distrust: a qualitative study on return to work legislation in the Netherlands. BMC Publ Health 13(1):1–14. https://doi.org/10.1186/1471-2458-13-153
Glare PA, Nikolova T, Alickaj A, Patil S, Blinder V (2017) Work experiences of patients receiving palliative care at a comprehensive cancer center: exploratory analysis. J Palliat Med 20(7):770–773. https://doi.org/10.1089/jpm.2016.0478
Hees HL, Nieuwenhuijsen K, Koeter MW, Bültmann U, Schene AH (2012) Towards a new definition of return-to-work outcomes in common mental disorders from a multi-stakeholder perspective. PLoS ONE 7(6):e39947. https://doi.org/10.1371/journal.pone.0039947
Zegers AD, Coenen P, Bültmann U, van Hummel R, van der Beek AJ, Duijts SF (2022) Tailoring work participation support for cancer survivors using the stages of change: perspectives of (health care) professionals and survivors. J Cancer Surviv 1–14. https://doi.org/10.1007/s11764-022-01196-x
Brom L, De Snoo-Trimp JC, Onwuteaka-Philipsen BD, Widdershoven GAM, Stiggelbout AM, Pasman HRW (2017) Challenges in shared decision making in advanced cancer care: a qualitative longitudinal observational and interview study. Health Expect 20(1):69–84. https://doi.org/10.1111/hex.12434
Duijts SF, van Egmond MP, Gits M, van der Beek AJ, Bleiker EM (2017) Cancer survivors’ perspectives and experiences regarding behavioral determinants of return to work and continuation of work. Disabil Rehabil 39(21):2164–2172. https://doi.org/10.1080/09638288.2016.1219924
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357. https://doi.org/10.1093/intqhc/mzm042
Braun V, Clarke V (2006) Using thematic analysis in psychology. Qual Res Psychol 3(2):77–101. https://doi.org/10.1191/1478088706qp063oa
Muhr T (1991) ATLAS/ti—a prototype for the support of text interpretation. Qual Sociol 14(4):349–371. https://doi.org/10.1007/BF00989645
Strauss A (1998) Basics of qualitative research: techniques and procedures for developing grounded theory. Sage publications
Tiedtke C, de Rijk A, Donceel P, Christiaens MR, de Casterlé BD (2012) Survived but feeling vulnerable and insecure: a qualitative study of the mental preparation for RTW after breast cancer treatment. BMC Publ Health 12(1):1–13. https://doi.org/10.1186/1471-2458-12-538
Miedema B, Hamilton R, Easley J (2007) From “invincibility” to “normalcy”: coping strategies of young adults during the cancer journey. Palliat Support Care 5(1):41–49. https://doi.org/10.1017/s147895150707006x
Lilliehorn S, Hamberg K, Kero A, Salander P (2013) Meaning of work and the returning process after breast cancer: a longitudinal study of 56 women. Scand J Caring Sci 27(2):267–274. https://doi.org/10.1111/j.1471-6712.2012.01026.x
Svidén GA, Tham K, Borell L (2010) Involvement in everyday life for people with a life threatening illness. Palliat Support Care 8(3):345–352. https://doi.org/10.1017/S1478951510000143
von Post H, Wagman P (2019) What is important to patients in palliative care? A scoping review of the patient’s perspective. Scand J Occup Therapy 26(1):1–8. https://doi.org/10.1080/11038128.2017.1378715
Söderman M, Friberg E, Alexanderson K, Wennman-Larsen A (2019) Women’s experiences of encounters with healthcare professionals’ regarding work after breast-cancer surgery and associations with sickness absence: a 2-year follow-up cohort study. Support Care Cancer 27(4):1197–1206. https://doi.org/10.1007/s00520-018-4453-1
Blinder VS, Murphy MM, Vahdat LT, Gold HT, de Melo-Martin I, Hayes MK, Scheff RJ, Chuang E, Moore A, Mazumdar M (2012) Employment after a breast cancer diagnosis: a qualitative study of ethnically diverse urban women. J Community Health 37(4):763–772. https://doi.org/10.1007/s10900-011-9509-9
Mehnert A, Veers S, Howaldt D, Braumann KM, Koch U, Schulz KH (2011) Effects of a physical exercise rehabilitation group program on anxiety, depression, body image, and health-related quality of life among breast cancer patients. Oncol Res Treat 34(5):248–253. https://doi.org/10.1159/000327813
Spelten ER, Verbeek JHAM, Uitterhoeve ALJ, Ansink AC, Van Der Lelie J, De Reijke TM, Kammeijer M, de Haes JCJM, Sprangers MAG (2003) Cancer, fatigue and the return of patients to work—a prospective cohort study. Eur J Cancer 39(11):15621567. https://doi.org/10.1016/S0959-8049(03)00364-2
Tamminga SJ, De Boer AG, Verbeek JH, Frings-Dresen MH (2012) Breast cancer survivors’ views of factors that influence the return-to-work process-a qualitative study. Scand J Work Environ Health 38(2):144–154. https://doi.org/10.5271/sjweh.3199
Islam T, Dahlui M, Abd Majid H, Nahar AM, Taib NAM, Su TT (2014) Factors associated with return to work of breast cancer survivors: a systematic review. BMC Publ Health 14(3):1–13. https://doi.org/10.1186/1471-2458-14-S3-S8
Tang PL, Mayer DK, Chou FH, Hsiao KY (2016) The experience of cancer stigma in Taiwan: a qualitative study of female cancer patients. Arch Psychiatr Nurs 30(2):204–209. https://doi.org/10.1016/j.apnu.2015.08.015
Abtahi LS (2021) Examining how employees deal with their colleagues’ death. J Crit Rev 8(2):272–277. https://doi.org/10.31838/jcr.08.02.30
Brusletto B, Torp S, Ihlebæk C, Vinje HF (2018) A five-phase process model describing the return to sustainable work of persons who survived cancer: a qualitative study. Eur J Oncol Nurs 34:21–27. https://doi.org/10.1016/j.ejon.2018.03.003
De Rijk A, Amir Z, Cohen M, Furlan T, Godderis L, Knezevic B, Miglioretti M, Munir F, Popa AE, Sedlakova M,Torp S, Yagil D, Tamminga SJ, De Boer AG (2019) The challenge of return to work in workers with cancer: employer priorities despite variation in social policies related to work and health. J Cancer Surviv 14:188–199. https://doi.org/10.1007/s11764-019-00829-y
Patel-Kerai G, Harcourt D, Rumsey N, Naqvi H, White P (2017) The psychosocial experiences of breast cancer amongst Black, South Asian and White survivors: do differences exist between ethnic groups? Psychooncology 26(4):515–522. https://doi.org/10.1002/pon.4187
Vrinten C, Wardle J, Marlow LA (2016) Cancer fear and fatalism among ethnic minority women in the United Kingdom. British J Cancer 114(5):597–604. https://doi.org/10.1016/j.apnu.2015.08.015
Marcu A, Black G, Vedsted P, Lyratzopoulos G, Whitaker KL (2017) Educational differences in responses to breast cancer symptoms: a qualitative comparative study. Br J Health Psychol 22(1):26–41. https://doi.org/10.1111/bjhp.12215
Sharkey K, Savulescu J, Aranda S, Schofield P (2010) Clinician gate-keeping in clinical research is not ethically defensible: an analysis. J Med Ethics 36(6):363–366. https://doi.org/10.1136/jme.2009.031716
Zegers AD, Coenen P, van Belzen M, Engelen V, Richel C, Dona DJ, Duijts SF et al (2021) Cancer survivors’ experiences with conversations about work-related issues in the hospital setting. Psychooncology 30(1):27–34. https://doi.org/10.1002/pon.5529
Acknowledgements
We wish to acknowledge and thank all patients who contributed to this research project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Donna Beerda, Amber Zegers, Emma van Andel, Saskia Duijts, and Linda Brom. The first draft of the manuscript was written by Donna Beerda, and all authors commented on previous versions of the manuscript. All authors read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study has been conducted according to the declaration of Helsinki. The study protocol has been reviewed by the Medical Ethical Committee of the Amsterdam University Medical Center (Amsterdam UMC), the Netherlands (METC2020.0736). The METC has exempted this observational research from ethical review, accordingly to the Dutch Medical Research Involving Human Subjects Act (WMO). Written informed consent for participation (and recording) was obtained from all individual participants. Furthermore, in data collection and analyses procedures, the Dutch Personal Data Protection Act was followed.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Saskia F. A. Duijts and Linda Brom shared last authorship
Appendix 1. Topics within the interview guide, indexing information on work resumption, and retention in patients with advanced cancer
Appendix 1. Topics within the interview guide, indexing information on work resumption, and retention in patients with advanced cancer
-
1.
Experienced changes in work situation since diagnosis (e.g. in position/tasks/hours)
-
2.
Consequences of advanced cancer (physical, mental, psychosocial) on (return to) work
-
3.
Possibility for work adjustments and level of satisfaction with potential work adjustments
-
4.
Changes in the meaning of work
-
5.
Communication with friends, family, and health professionals about work resumption
-
6.
Practicalities related to the process of RTW
-
7.
Role of the employer in RTW and communication with the employer during RTW
-
8.
Experienced support (e.g. support from colleagues, healthcare professionals) during RTW/work retention
-
9.
Dutch (long-term) sick leave legislation (e.g. regarding reintegration, sickness and disability benefits) and financial issues in general
-
10.
Work-related (unmet) needs, wishes, and recommendations
-
11.
Any additional work-related topics not previously discussed
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Beerda, D.C.E., Zegers, A.D., van Andel, E.S. et al. Experiences and perspectives of patients with advanced cancer regarding work resumption and work retention: a qualitative interview study. Support Care Cancer 30, 9713–9721 (2022). https://doi.org/10.1007/s00520-022-07436-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07436-1