Abstract
Purpose
The aim of this study was to study the nutritional profile of node-negative and node-positive patients undergoing treatment for head and neck squamous cell cancer (HNSCC).
Methods
This prospective cohort study was conducted between 2018 and 2020. Patients diagnosed with HNSCC, planned for treatment, were enrolled after written informed consent. In node-negative (N0) and node-positive (N +) cohorts of patients, nutritional status was determined using anthropometric measures and Subjective Global Assessment (SGA) scale pre-treatment, and during and after treatment. Statistical analysis was performed using SPSS version 22. Data was analyzed using parametric and non-parametric tests, and p value of 0.05 was considered significant.
Results
In total, 161 patients were analyzed, 73 N0 and 88 N + cohorts. Pre-treatment, 9.6 to 20.4% patients in N0 and 23.9 to 32.8% patients in N + cohorts were malnourished. Incidence of malnutrition at completion of treatment was 40.8 to 52.5% overall, 20.5 to 41.1% N0, and 39.5 to 62.8% N + . Mean reduction in weight (11.1% ± 7.82 vs 6.26% ± 8.3, p = 0.000), mean reduction in BMI (2.57 ± 1.87 vs 1.29 ± 1.62, p = 0.000), median reduction in MUAC (2 cm vs 1 cm, p = 0.000), and median increase in SGA score (13 vs 6, p = 0.000) were higher in multi-modality as compared to those in a single-modality treatment. Similar findings were noted in N0 and N + cohorts.
Conclusion
As compared to N0, N + patients had higher burden of malnutrition at diagnosis, and more worsening of nutritional parameters during treatment. More decline in nutritional status was seen in patients receiving multi-modality as compared to single-modality treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Head and neck squamous cell cancer (HNSCC) is the 6th most common cancer in the world; in 2018, there were 890,000 new cases and 450,000 deaths. The incidence is anticipated to increase by 30% by 2030 (Global Cancer Observatory (GLOBOCAN)) [1,2,3]. In India, the estimated age-standardized rate for incidence of HNSCC was > 10.7 per 100,000 (GLOBOCAN 2018); in the USA, this is 7.5–10.7 per 100,000. The high incidence in the South Asian region is associated with consumption of carcinogenic-containing products like oral tobacco and areca nut, and alcohol abuse, whereas oropharyngeal infection with HPV contributes to the high incidence in the West [4,5,6]. HNSCC is treated with a single-modality or multi-modality approach—surgical resection, radiation, or chemotherapy plus radiation depending on the disease stage.
Malnutrition is seen in 30–50% of HNSCC patients; around 30% patients have severe malnutrition and weight loss since 6 months prior to diagnosis. Chemotherapy worsens the nutritional intake due to digestive tract–related symptoms like loss of taste, mucositis, nausea, and vomiting [7]. Impairment related to swallowing and speech and xerostomia occur in ~ 50% of HNSCC patients following radiotherapy and these are often persistent long term [8]. The 2-year prevalence of dysphagia in HNSCC survivors is 45%; this is 4–8 times more than those who never had cancer [9]. Several studies have shown higher rates of treatment interruptions and less treatment effectiveness with high-grade mucositis [10]. Increased mortality and worse prognosis have been proposed to be associated with fat-free body mass loss related to malnutrition in cancer patients [11]. Indian data on nutritional profile of patients undergoing treatment for HNSCC with regard to node-negative and node-positive cohorts is lacking.
The aim of this study was to study the nutritional profile of node-negative and node-positive patients undergoing treatment for HNSCC.
Methods
This prospective cohort study was carried out at Cancer Research Institute, Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Dehradun, India, between 2018 and 2020, under Institutional Ethics Committee clearance number SRHU/HIMS/ETHICS/2018/115. The study population were patients starting treatment for HNSCC.
Inclusion criteria
Patients with diagnosed and previously untreated HNSCC planned for treatment.
Exclusion criteria
-
1.
Previously treated for HNSCC with surgery, radiotherapy, or chemotherapy.
-
2.
Metastatic disease at presentation.
-
3.
Patient with skin, nasopharynx, or esophagus cancer or with metastasis from primary sites other than the head and neck.
-
4.
Age less than 18 years.
Patients once diagnosed with HNSCC and planned for curative or palliative oncological treatment with single or multi-modality were approached for enrollment in the study and an informed written consent was obtained. They were assessed for nutritional status before starting treatment, at the end of each treatment modality, and at completion of planned treatment. The following data were recorded:
-
(a)
Baseline data regarding patient demographics, disease, and treatment plan.
-
(b)
ECOG performance status (PS).
-
(c)
Nutritional status: weight, Subjective Global Assessment (SGA) score, mid-upper arm circumference (MUAC), body mass index (BMI), and hemoglobin
Based on the assumption that nutritional status may be different in patients with or without neck nodal metastasis, two cohorts were made based on the neck node status of the patient:
-
(a)
N0 cohort: patients with no node metastasis at presentation
-
(b)
N + cohort: patients with node metastasis at presentation
The data were recorded, anonymized, and analyzed using the following statistical methods.
Statistical analysis
The data were entered in MS Excel 2010. Statistical analysis was performed using SPSS software version 22. The one-sample Kolmogorov–Smirnov test was used to determine whether datasets were different from normal distribution. Normally distributed data was analyzed using a parametric test: unpaired Student T test, paired-sample T test; non-normally distributed data using non-parametric tests: Mann–Whitney U test, Wilcoxon-signed rank test, marginal homogeneity test; and categorical data using Pearson Chi-square test. The level of significance was taken as p < 0.05.
Results
A total of 161 patients were enrolled in the study: 73 in N0 and 88 in N + cohorts, 88.2% were male, mean age 56.32 (± 13.27 SD) years, 60.8% in T3/4 stage, 40.4% patients received single-modality and 59.6% multi-modality treatment. The pre-treatment mean weight was 57.75 (± 11.77 SD) kg; BMI 21.58 (± 4.2 SD); hemoglobin 13.42 (± 1.77 SD) g/dl; MUAC 24.71 (± 3.78 SD) cm. The distribution of central tendencies of these parameters was similar in N0 and N + cohorts. Pre-treatment mean weight loss in N0 and N + cohorts was 4.25% and 7.93% (p = 0.004), mean SGA score 36.95 and 42.74 (p = 0.000) respectively (Table 1). In N0 and N + cohorts, 13.7% and 28.4% (p = 0.034) patients had lost more than 10% weight pre-treatment, 9.6% and 22.8% (p = 0.036) patients had low MUAC, 10.9% and 27.2% (p = 0.015) had SGA score of ≥ 50, and 4.1% and 18.2% (p = 0.006) patients had Bitot spots respectively (Table 2).
Nutritional parameters in node-negative and node-positive cohorts
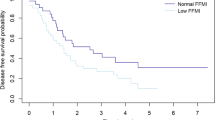
gMean weight in kilograms (± SD) reduced from 57.83 (11.79) to 52.22 (10.51) (p = 0.000), 58.94 [12] to 53.66 (11.24) (p = 0.000), and 56.74 (11.56) to 51 (9.75) (p = 0.000) in overall, N0, and N + cohorts (Tables 3, 4, 5). Mean % reduction in weight in kilograms (SD) at the end of the first treatment modality was 4.69 (6.46) overall, 6.21 (5.84) N0, and 3.59 (6.73) N + ; at the end of the second treatment modality was 7.49 (6.99) overall, 6.71 (8.19) N0, and 8.04 (6.03) N + ; at completion of all treatment 9.17 (8.33) overall, 8.93 (7.97) N0, and 9.37 (8.66) N + . Weight loss ≥ 10% was seen at the end of the first treatment modality in 27.2% patients overall, 26.4% N0, and 27.9% N + ; at the end of the second modality treatment in 38.1% overall, 37% N0, and 38.9% N + ; at completion of all treatment 45.3% overall, 41.1% N0, and 48.8% N + . Mean reduction in BMI (95% confidence interval) at the end of the first treatment modality was 1.45 (1.2–1.7) overall, 1.52 (1.2–1.9) N0, and 1.39 (1.0–1.7) N + ; at the end of the second treatment modality was 2.71 (2.2–3.2) overall, 2.83 (2.0–3.7) N0, and 2.62 (1.9–3.3) N + . Low BMI was present at baseline in 22.8% patients overall, 20.9% N0, and 24.4% N + ; at the end of the first treatment modality 38% overall, 33.3% N0, and 41.9% N + ; at the completion of all treatment 43.4% overall, 35.5% N0, and 50% N + . Low MUAC was found at baseline in 17.2% patients overall, 9.6% N0, and 22.7% N + ; at the end of the first treatment 27.2% overall, 18.1% N0, and 34.9% N + ; at the completion of all treatment 30.8% overall, 20.5% N0, and 39.5% N + . The median SGA score at baseline was 39 overall, 34 N0, and 42 N + ; at the end of the first treatment 47 overall, 46.5 N0, and 48 N + ; at completion of all treatment 50 overall, 48 N0, and 53 N + . SGA score of > 40 was found in 47.2% patients overall, 34.2% N0, and 58% N + at baseline; 69.6% overall, 63.9% N0, and 74.4% N + at the end of the first treatment; 87.4% overall, 79.5% N0, and 94.2% N + at completion of all treatment. Moderate to severe anemia was found at baseline in 6.3% patients overall, 7.1% N0, and 5.7% N + ; at the end of the first treatment 16.3% overall, 12.5% N0, and 18.6% N + ; at completion of treatment 16.9% overall, 14.1% N0, and 19% N + .
Pattern of change in nutritional parameters in patients having received single-modality versus multi-modality treatment
Overall, there was no significant difference in PS, mean weight, mean BMI, median MUAC, mean hemoglobin, or median SGA score at completion of treatment between single- and multi-modality groups. Mean reduction of weight was higher (11.1% ± 7.82 vs 6.26% ± 8.3, p = 0.000), mean reduction in BMI was higher (2.57 ± 1.87 vs 1.29 ± 1.62, p = 0.000), median reduction in MUAC was higher (2 cm vs 1 cm, p = 0.000), and median increase in SGA score was higher (13 points vs 6 points, p = 0.000) in the multi-modality group (Table 6). In the node-negative cohort, mean reduction of weight was higher (10.85% ± 8.13 vs 6.79% ± 7.31, p = 0.028), mean reduction in BMI was higher (2.66 ± 1.98 vs 1.44 ± 1.64, p = 0.006), median reduction in MUAC was higher (2 cm vs 1 cm, p = 0.009), and median increase in SGA score was higher (15 points vs 8 points, p = 0.009) in the multi-modality group. In the node-positive cohort, mean reduction of weight was higher (11.12% ± 87.69 vs 6.95% ± 5.12, p = 0.005), mean reduction in BMI was higher (2.52 ± 1.81 vs 1.1 ± 1.61, p = 0.001), median reduction in MUAC was higher (3 cm vs 2 cm, p = 0.001), and median increase in SGA score was higher (12 points vs 4 points, p = 0.009) in the multi-modality group.
Discussion
The center where this study was conducted is a tertiary care cancer center, located at the foot of Himalayas in India. Approximately 1200 new cancer patients are treated at this center every year, 300 diagnosed with head and neck cancer. The patients are usually from low to middle socioeconomic strata. The median age at diagnosis for non-HPV-associated HNSCC is 66 years and that of HPV-associated oropharyngeal cancer is ~ 53 years in literature [12]. In the present study, the mean age was 56.3 years, as in India HNSCC is usually more non-HPV related, patients in this study were a decade younger. A majority of patients in this study were T3/4 stage, which is in keeping with other reports [13], and required multi-modality treatment in ~ 60% patients. Malnutrition in head and neck cancer affects 30–50% of patients [10, 13]. In a review article published in 2017 [14], it was noted that up to 80% of HNSCC patients are malnourished because of one their lifestyle and second the risk factors associated with HNSCC. In the present study among node-negative patients, only 13.7% had lost the critical ≥ 10% weight within 6 months prior to starting treatment, only 10.9% had SGA score ≥ 50, only 9.6% had low MUAC, and 20.4% patients had low BMI. Thus, 9.6 to 20.4% patients were observed to suffer from malnutrition at diagnosis in the node-negative cohort. This is lower than the international literature. In the node-positive cohort, 28.4% patients had lost ≥ 10% weight within 6 months prior to starting treatment, 27.2% had SGA score ≥ 50, 32.8% had low MUAC, and 23.9% low BMI. Thus, 23.9 to 32.8% patients were malnourished in the node-positive cohort at diagnosis. The burden of malnutrition was found to be higher in node-positive patients; this could be due to multiple factors like a more advanced disease causing symptoms like swallowing or chewing difficulty, longer duration of disease with longer nutritional challenges, pain, and other symptoms associated with advanced disease which reduce oral intake. In HNSCC patients, cancer is close to structures vital for eating, leading to numerous nutritional challenges before, during, and after treatment. They experience treatment side effects, like odynophagia, dysphagia, xerostomia, dysgeusia, mucositis, sticky saliva, fatigue, nausea, and vomiting [15]. These further impair patient’s ability to sustain adequate intake orally. A systematic review found “dysphagia” to be the most commonly studied symptom during treatment for HNSCC [16]. During or after treatment, malnutrition and unintentional weight loss in HNSCC patients are associated with increased morbidity and mortality, poor treatment outcome, and poor quality of life [17]. The nutritional journey, as experienced by HNSCC patients undergoing treatment, may be different from the measured nutritional parameters. A qualitative study on 10 HNSCC patients undergoing treatment aimed to study the experience of patients regarding their nutritional situation and perception of nutritional support during treatment. Patients experienced surgery as a poor starting point for radiotherapy from the nutritional aspect. Patients customized their diet as radiotherapy started; they experienced virtually no oral food intake about halfway into radiotherapy. This leads to tube-feeding and hospital admissions. All patients were recommended ONS, but supplements became unbearable eventually. After completion of radiotherapy, patients experienced discouragement from persistent side effects; this prevented patients from eating [18].
The response to treatment, in HNSCC patients, is affected by their unique nutritional problems. To adequately manage these patients, the treating team must accurately and systematically assess nutritional status and execute timely metabolic treatment [19]. In the present study, all nutritional parameters declined significantly from baseline during the treatment. At the end of treatment, the mean reduction in weight was 9.17% (± 8.33 SD) from baseline weight; ≥ 10% weight loss was present in 45.3% patients, low BMI 43.4% patients, low MUAC 40.8% patients, ≥ 50 SGA score 52.5% patients, and moderate to severe anemia 16.9% patients. The incidence of malnutrition at completion of treatment in this study was 40.8 to 52.5% overall, in the node-negative cohort 20.5 to 41.1%, and in the node-positive cohort 39.5 to 62.8%. In the node-positive cohort, 15% more patients had low BMI, 19% more patients low MUAC, and 23% more patients ≥ 50 SGA score at completion of treatment as compared to the node-negative cohort. The nutritional challenges for patients undergoing treatment for node-positive HNSCC are far greater than those for node-negative patients. A retrospective study published in 2019 aimed to assess the impact of prophylactic feeding gastrostomy (FG) and predictors of malnutrition in patients undergoing treatment for HNSCC [20]. They studied 111 patients and found that patients without prophylactic FG had more hospital readmissions (p = 0.042), greater relative weight loss at 6 weeks (p < 0.0001), symptoms like dysphagia, and higher rate of severe malnutrition. They found factors like node-positive status, oral intake difficulty, concomitant chemo-radiotherapy, primary tumor sites like nasopharynx, and hypopharynx tumor site were significantly associated with malnutrition. A systematic review [21] published much prior (in 2013) analyzed the effect of nutritional interventions like individualized dietary counseling, oral nutritional supplements (ONS), nasogastric (NG) tube feeding, and percutaneous endoscopic gastronomy (PEG) on nutritional status, quality of life (QoL), and mortality in HNSCC patients receiving radiotherapy or chemo-radiotherapy. They found beneficial effects on nutritional status and QoL for individualized dietary counseling only; ONS, NG tube, and PEG tube feeding were not consistently associated with benefit.
The detrimental effects of treatment for HNSCC on the nutritional status of a patient may vary according to the oncological treatment. Early-stage HNSCC is usually treated with single-modality treatment like surgery or radiotherapy, whereas locally advanced HNSCC is treated with a multi-modality treatment like surgery followed by radiotherapy or chemo-radiotherapy or radical chemo-radiotherapy, depending on the location of primary tumor. Some patients, with locally advanced HNSCC, receive a single-modality treatment with a palliative intent. Nutritional parameters of a single-modality treatment and multi-modality treatment groups were compared in the present study. At completion of treatment, we found that the ECOG performance status and mean weight were not different in both groups. But the mean reduction in weight was 4.75% more, mean reduction in BMI was 1.28 kg/m2 more, and median increase in SGA score was 7 points more in the multi-modality group as compared to those of a single-modality group (all statistically significant). Similar findings were noted in both node-negative and node-positive cohorts. In a prospective study published in the year 2020 [22], patients undergoing a single-modality treatment with radiotherapy for HNSCC were followed up for nutritional status and nutrition impact factors. Similar to the present study, they used a SGA score and found that 56% patients were malnourished at baseline and this increased to 100% after completion of treatment, and the mean weight loss was 4.53 ± 0.41 kg, 7.39%. They also reported taste changes and dry mouth in 100% patients. Another study published in the same year compared the health-related QoL in 19 HNSCC patients undergoing multi-modality treatment with chemo-radiotherapy. They found that well-nourished patients had fewer QoL issues like pain, sticky saliva, fatigue, chewing difficulty, appetite loss, and social eating as compared to malnourished (p < 0.05). They found a statistically significant association (but weak strength, r = − 0.37, p = 0.012) between global QoL score and SGA score [23]. A randomized controlled trial [24] on HNSCC patients receiving radiotherapy compared nutritional counseling alone versus ONS along with nutritional counseling. ONS resulted in smaller weight loss (mean 1.6 kg, 95%CI 0.5–2.7, p = 0.006), improved QoL and higher protein-calorie intake, and reduced need for plan changes in oncological treatment (HR = 0.40, 95%CI 0.18–0.91, p = 0.029). The QoL of a patient is inter-related with psychological distress; an RCT aimed to improve the nutritional status of HNSCC patients receiving radiotherapy, using the psychological technique “Eating as Treatment” (EAT) program, delivered by the dietitians. The control group had 151 patients and the intervention group, 156. SGA score was used to assess the primary end point, nutritional status. Intervention group had better SGA score, less percent weight loss, less treatment interruptions, lower depression scores, and higher QoL [25]. This RCT demonstrated effectiveness of psychological intervention (EAT) in improving nutrition in HNSCC patients undergoing treatment. The negative impact of treatment usually continues in the survivorship period too. In a qualitative study, 31 HNSCC survivors were interviewed to acquire a comprehensive understanding of their lived experience of chronic Nutrition Impact Symptoms (NIS) burden [26]. It was interesting to note that they found at least one or more chronic NIS in all survivors, but before treatment 40% were unaware of the potential for chronically persistent NIS. The present study highlights the need for supportive therapies in cancer care, especially nutritional services. Low- and middle-income countries like India face disparities in health care systems with regard to these supportive care services. There are limitations in availability of nutrition specialists, cancer dieticians, and even nutritional supplements in low-cost cancer centers, where a majority of cancer patients are treated.
In 2016, “Nutritional management in head and neck cancer: United Kingdom National Multidisciplinary Guidelines” was published [27]. The following recommendations were made regarding treatment of HNSCC:
-
The multidisciplinary team should include a specialist dietitian.
-
Nutritional assessment should be performed using a validated tool before starting treatment and at regular intervals.
-
High-risk patients should be referred for early dietary intervention.
-
Appropriate nutritional support and malnutrition treatment should be offered without delay.
-
They recommended SGA and patient-generated SGA as validated tools for nutritional assessment.
-
Pre-treatment nutritional assessment should be offered.
-
Patients well-nourished pre-treatment should receive regular dietary assessment and intervention.
-
They recommended energy intake of a minimum 30 kcal/kg/day and protein intake 1.2 g/kg/day.
-
Enteral nutrition to be started in the food intake is < 60% of the estimated energy expenditure.
-
Gastrostomy is recommended over NG tube if long-term (4 weeks) tube feeding is anticipated.
-
Nutritional interventions like dietary counseling and diet supplements should be offered up to 3 months after treatment.
-
QoL parameters related to nutrition should be estimated pre-treatment, during treatment, and post-treatment at regular intervals.
In conclusion, HNSCC patients may be malnourished at presentation, and the nutritional status deteriorated in a vast proportion of patients during treatment. Node-positive patients had a higher burden of malnutrition at diagnosis, and higher worsening of nutritional parameters during treatment as compared to node-negative patients. A higher decline in nutritional status was seen in patients receiving a multi-modality as compared to a single-modality treatment. Thus, node-positive HNSCC patients receiving a multi-modality treatment have the highest burden of malnutrition.
Data availability
Available.
Code availability
SPSS version 22.
References
Ferlay J et al (2019) Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 144:1941–1953
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Ferlay J et al (2018) Global Cancer Observatory: cancer today. Lyon, France: International Agency for Research on Cancer (accessed 18 September 2020). IARC. https://gco.iarc.fr/today
Hashibe M et al (2007) Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. J Natl Cancer Inst 99:777–789
Mehanna H et al (2013) Prevalence of human papillomavirus in oropharyngeal and nonoropharyngeal head and neck cancer–systematic review and meta-analysis of trends by time and region. Head Neck 35:747–755
Jiang H et al (2019) Can public health policies on alcohol and tobacco reduce a cancer epidemic? Australia’s experience. BMC Med 17:213
Isenring EA, Capra S, Bauer JD (2004) Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br J Cancer 91(3):447–452
Rinkel RN et al (2016) Prevalence of swallowing and speech problems in daily life after chemoradiation for head and neck cancer based on cut-off scores of the patient-reported outcome measures SWAL-QOL and SHI. Eur Arch Otorhinolaryngol 273:1849–1855
Hutcheson KA et al (2019) Two-year prevalence of dysphagia and related outcomes in head and neck cancer survivors: an updated SEER-Medicare analysis. Head Neck 41:479–487
De Luis DA, Izaola O, Aller R (2007) Nutritional status in head and neck cancer patients. Eur Rev Med Pharmacol Sci 11(4):239–243
Tchekmedyian NS, Zahyna D, Halpert C, Heber D (1992) Assessment and maintenance of nutrition in older cancer patients. Oncology (Williston Park) 6(2 Suppl):105–111
Windon MJ et al (2018) Increasing prevalence of human papillomavirus-positive oropharyngeal cancers among older adults. Cancer 124:2993–2999
Bossola M (2015) Nutritional interventions in head and neck cancer patients undergoing chemoradiotherapy: a narrative review. Nutrients 7(1):265–276
Urs Müller-Richter C, Betz S Hartmann et al (2017) Nutrition management for head and neck cancer patients improves clinical outcome and survival. Nutr Res 48:1–8. https://doi.org/10.1016/j.nutres.2017.08.007
Bossola M (2015) Nutritional interventions in head and neck cancer patients undergoing chemoradiotherapy: a narrative review. Nutrients 7(1):265–276. https://doi.org/10.3390/nu7010265
Bressan V, Stevanin S, Bianchi M et al (2016) The effects of swallowing disorders, dysgeusia, oral mucositis and xerostomia on nutritional status, oral intake and weight loss in head and neck cancer patients: a systematic review. Cancer Treat Rev 45:105–119. https://doi.org/10.1016/j.ctrv.2016.03.006
Ackerman D, Laszlo M, Provisor A et al (2018) Nutrition management for the head and neck cancer patient. Cancer Treat Res 174:187–208. https://doi.org/10.1007/978-3-319-65421-8_11
Sandmael JA, Sand K, Bye A et al (2019) Nutritional experiences in head and neck cancer patients. Eur J Cancer Care (Engl) 28(6):e13168. https://doi.org/10.1111/ecc.13168
Wood RM, Lander VL, Mosby EL et al (1989) Nutrition and the head and neck cancer patient. Oral Surg Oral Med Oral Pathol 68(4):391–395. https://doi.org/10.1016/0030-4220(89)90134-5
Yanni A, Dequanter D, Lechien JR et al (2019) Malnutrition in head and neck cancer patients: impacts and indications of a prophylactic percutaneous endoscopic gastrostomy. Eur Ann Otorhinolaryngol Head Neck Dis 136(3S):S27–S33. https://doi.org/10.1016/j.anorl.2019.01.001
Langius JAE, Zandbergen MC, Eerenstein SEJ et al (2013) Effect of nutritional interventions on nutritional status, quality of life and mortality in patients with head and neck cancer receiving (chemo)radiotherapy: a systematic review. Clin Nutr 32(5):671–8. https://doi.org/10.1016/j.clnu.2013.06.012
Neoh MK, Zaid ZA, Daud ZAM et al (2020) Changes in nutrition impact symptoms, nutritional and functional status during head and neck cancer treatment. Nutrients 12(5):1225. https://doi.org/10.3390/nu12051225
Mulasi U, Vock D, Jager-Wittenaar H et al (2020) Nutrition status and health-related quality of life among outpatients with advanced head and neck cancer. Nutr Clin Pract 35(6):1129–1137. https://doi.org/10.1002/ncp.10476
Cereda E, Cappello S, Colombo S et al (2018) Nutritional counseling with or without systematic use of oral nutritional supplements in head and neck cancer patients undergoing radiotherapy. Radiother Oncol 126(1):81–88. https://doi.org/10.1016/j.radonc.2017.10.015
Britton B, Baker AL, Wolfenden L et al (2019) Eating As Treatment (EAT): a stepped-wedge, randomized controlled trial of a health behavior change intervention provided by dietitians to improve nutrition in patients with head and neck cancer undergoing radiation therapy (TROG 1203). Int J Radiat Oncol Biol Phys 103(2):353–362. https://doi.org/10.1016/j.ijrobp.2018.09.027
Crowder SL, Najam N, Sarma KP et al (2020) Head and neck cancer survivors’ experiences with chronic nutrition impact symptom burden after radiation: a qualitative study. J Acad Nutr Diet 120(10):1643–1653. https://doi.org/10.1016/j.jand.2020.04.016
Talwar B, Donnelly R, Skelly R et al (2016) Nutritional management in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 130(S2):S32–S40. https://doi.org/10.1017/S0022215116000402
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Material preparation, and data collection and analysis were performed by Anshika Arora, Sunil Saini, and Meenu Gupta. The first draft of the manuscript was written by Anshika Arora and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethics committee approval number: SRHU/HIMS/ETHICS/2018/115.
Consent to participate
A written informed consent was obtained from all participants.
Consent for publication
Consent for publication was obtained from the Institutional Research Committee.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arora, A., Saini, S. & Gupta, M. Pattern of nutritional status in node-negative versus node-positive head and neck cancer patients undergoing treatment: a prospective cohort study. Support Care Cancer 30, 8029–8039 (2022). https://doi.org/10.1007/s00520-022-07245-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07245-6