Abstract
Purpose
Family caregivers of palliative cancer patients experience various supportive care needs. Appropriate self-reported instruments with robust psychological properties are required to identify these needs of family caregivers. Therefore, we conducted a systematic review to identify self-reported supportive care needs assessment instruments for family caregivers of palliative cancer patients and assess their contents, psychometric properties, and applicability.
Methods
Systematic searches were conducted in six English databases and four Chinese databases from inception to October 2020 and updated in June 2021. The instruments identified were evaluated using an 18-item checklist consisting of six domains: conceptual model, content validity, reliability, construct validity, scoring and interpretation, and respondent burden and presentation.
Results
Six articles, describing four self-reported needs assessment instruments, were included in the review. These instruments varied significantly in terms of contents, constructs, scoring methods, and applicability. Three of these instruments were developed to assess the comprehensive supportive care needs of family caregivers, while one was specifically developed to assess the spiritual needs of family caregivers. With respect to psychometric properties, none of the instruments identified met all the criteria. Three major shortcomings were identified, namely, lack of longitudinal validity, lack of a strategy for interpreting missing data, and lack of a description of the literacy level required to understand the questions. Additionally, the instrument development processes assessed in this study lacked qualitative elements.
Conclusions
End-users need to consider contents, psychometric properties, and applicability when choosing an appropriate needs assessment instrument according to individual purpose and context. Further evaluation or development of needs assessment for the family caregivers of palliative cancer patients is needed, with a particular emphasis on caregivers’ perspectives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Family caregivers (FCs) play a vital role in adult cancer patients’ disease journey, from diagnosis to the terminal stages [1]. During this time, FCs provide direct care and support to these patients [2], which can be physically and psychologically demanding for the FCs and lead to health problems [3,4,5]. FCs caring for cancer patients undergoing palliative care may experience more challenges than those caring for patients receiving curative treatments because the patients’ condition can deteriorate rapidly and become increasingly complex [6]. These challenges, coupled with the FCs’ own potential health problems, can lead to various supportive care needs [7]. Supportive care needs of caregivers, a concept derived from patient-oriented research, refer to a range of services and supports relating to the physical, social, emotional, psychological, spiritual, and practical domains [8]. To support the FCs, it is crucial to assess these needs accurately. This process has been identified as one of the most effective interventions to support FCs in end-of-life care [9].
Needs assessment is a process that identifies the comprehensive or specific needs of individuals and can offer insight into the extent of each specific need and what kind of help or care is required [10]. During this process, an appropriate self-reported instrument with robust psychological properties is needed. The self-reported nature of the instrument allows the respondents to describe their needs from their own perspective rather than being observed and interpreted by others, facilitating person-centred care [11]. In a previous systematic review [10], seven instruments used to assess the needs of informal caregivers of cancer survivors were identified. As this systematic review excluded instruments designed for the caregivers of terminal cancer patients or at bereavement, these seven instruments could not comprehensively assess the holistic needs of FCs of palliative cancer patients.
FCs who support palliative cancer patients experience distinct issues from those caring for cancer patients who are receiving active treatment or are in remission, leading to different needs [12]. For example, for caregivers of cancer patients in the treatment stage or under palliative care, communication with medical staff and access to information are essential [13, 14]. However, for caregivers in the palliative context, information about the process of dying and what to do at the time of death may also be required [15]; these were unique for caregivers of palliative cancer patients. In addition, caregivers of palliative cancer patients may have needs for coping with patients’ death [16]. Therefore, a comprehensive and sensitive instrument is essential to identify the needs of FCs of palliative cancer patients. Inappropriate use of instruments may produce misleading information or miss important information [10].
As the importance of the needs of FCs of cancer patients in the palliative context began to be widely appreciated, instruments targeted to the needs of this population emerged. However, needs assessment instruments show significant differences in terms of contents, methods, and psychometric properties. Selecting and implementing these instruments on a case-by-case basis remains an issue. Therefore, the objective of this review was to identify the various needs assessment instruments available for the FCs of palliative cancer patients and analyse the content, quality of psychometric properties, and their applicability, so as to provide recommendations on the most appropriate instruments through the synthesis of previous evidence.
Methods
The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) was used to guide the structure of this review [17].
Search strategy
Relevant literature was identified from six English databases (PubMed, Embase, Cochrane Library, CINAHL, PsycINFO, OVID) and four Chinese databases (China National Knowledge Infrastructure (CNKI), Wan Fang Data, Chongqing VIP (CQVIP), and the Chinese Biomedical Literature Database (CBM)) in October 2020 and updated in June 2021. The search terms “needs assessment”, “family caregivers”, “palliative care”, and “cancer” were combined to interrogate each database using both free-text terms and Medical Subject Headings (MeSH) where available. The search strategies used for each specific database are presented in Supplemental Table 1. Additionally, the research team identified further relevant literature by searching the key references of the identified studies.
Inclusion and exclusion criteria
Studies meeting the following criteria were included: (1) described a self-reported instrument to directly identify the needs of the FCs of cancer patients receiving palliative care; (2) aimed to evaluate the development or perform validation of at least one psychometric property of the instruments in the FCs of cancer patients receiving palliative care; (3) included FCs aged above 18 years old who are caring for palliative cancer patients aged above 18 years old; and (4) reported in English or Chinese. Studies aiming to develop instruments to test the needs of FCs of patients with other chronic illnesses were excluded. Interventional studies, qualitative studies, discussion papers, literature reviews, guidelines, comments, editorials, protocols, conference articles, case reports, opinion pieces, commentaries, letters, retrospective studies, reviews, or secondary research were also excluded. In addition, grey literature was excluded as it rarely impacted the results and conclusions of a systematic review [18].
Two independent reviewers performed the literature selection procedure. First, the titles and abstracts of all articles were screened by one reviewer, with the other reviewer checking and verifying the results. Next, full texts of relevant articles were retrieved to determine eligibility. The two reviewers checked the full texts and assessed them in detail against the inclusion and exclusion criteria. Any disagreements that arose during the screening process were resolved by discussion.
Data extraction
Two reviewers extracted the relevant information from each study according to the pre-designed tables (one reviewer extracted data from the included studies, and another double-checked the extracted data). The information extracted from each study was the name of the instrument(s), authors, year of publication, country and setting, validation population, conceptual model, the number of items, dimensions, response options, scoring method, time for completion, and purpose (research or clinical use). Data describing the psychometric properties (internal consistency reliability, test-retest reliability, content validity, and construct validity) of each instrument were also collected.
Appraisal of the needs assessment instruments
Several tools exist for appraising needs assessment instruments, with the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) being a commonly used standardised tool for assessing patient-reported outcome measures [19, 20]. However, it is complex, with more than 110 items and 10 categories, limiting its utility in systematic reviews [21]. Therefore, we used a simplified checklist that incorporated the critical features highlighted in COSMIN to appraise all instruments included in this systematic review [21]. The checklist was designed to assess the developmental measurement properties and applicability of the patient-reported outcome measures. It consists of 18 items divided into six domains relevant to the development of the questionnaires: conceptual model, content validity, reliability, construct validity, scoring and interpretation, and respondent burden and presentation. Detailed descriptions of these domains are presented in Supplemental Table 2 [21]. Each item is dichotomous (0 = criterion not met, 1 = criterion met). However, this tool is not meant to yield a total score. It is a guide to identify whether important measurement properties are present for each instrument.
Two reviewers assessed each instrument using the checklist. First, the two reviewers conducted a trial evaluation on one instrument and reached a consensus on understanding and using this checklist. Subsequently, they assessed each instrument independently, compared the assessment results, and discussed disagreements. All disagreements in this process were resolved by discussion between the two reviewers and a senior expert.
Synthesis method
As each instrument was found to have high heterogeneity in terms of construct and methodology, the data were not appropriate for aggregation or meta-analysis. Instead, narrative synthesis was performed for each instrument characteristic, including study population, instrument contents, and psychometric properties.
Results
Search results and study selection
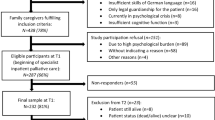
A total of 19,078 articles were identified through systematic searching and 17 articles from citation checking. After removing duplicates and title/abstract screening, 61 relevant articles were selected for full-text review. A total of six studies met the inclusion/exclusion criteria, and four different instruments were identified. A flow diagram is presented as Fig. 1.
Characteristics of the study populations
All instruments were validated in FCs of cancer patients receiving palliative care or who were terminally ill (Table 1). The sample sizes for validation ranged from 30 to 649 individuals. Some validation populations were recruited from hospitals [22,23,24,25], and others were from hospice care units/services [24, 26, 27].
Characteristics of the needs assessment instruments
Of the six articles included, four studies aimed to determine the psychometric properties of the instruments for their target populations [22,23,24, 27], and two described both the development process and psychometric properties [25, 26]. In total, four needs assessment instruments for the FCs of palliative cancer patients were identified: Family Inventory of Needs (FIN) [22, 23, 26], Home Caregiver Need Survey (HCNS) [24], Questionnaire about the Needs of the Dependents of Advanced Cancer Patients (QNDACP) [25], and the Spiritual Needs Inventory (SNI) [27] (Table 1).
Two instruments were originally developed in the USA (HCNS and SNI), and one in each of Canada (FIN) and China (QNDACP). Among these instruments, FIN showed the most cross-cultural adaptations (i.e., German, Czech, Portuguese, and Icelandic versions) [22, 23, 28, 29]. As the Portuguese version of FIN [28] was not validated among FCs of palliative cancer patients and the original validation data of the Icelandic version of the FIN [29] cannot be acquired although we tried to contact the authors, these two versions of FIN were not included in this review. The total number of items included in each instrument ranged from 17 to 90. Most of the instruments were multidimensional except for the English and German versions of the FIN [22, 26]. All the instruments were self-reported and could be used to assess the FCs’ needs directly. Regarding application, two instruments (FIN and QNDACP) were developed for research and clinical practice. The HCNS was originally designed for use as both a research instrument and an assessment guide. However, further investigation is required to determine whether it can be used in a clinical setting.
Summary and appraisal results of the needs assessment instruments
The other characteristics of the included instruments (conceptual model, items and dimensions, response options and scoring, completion time) were summarised in Table 1. The reliability and validity assessments and the appraisal results of the measurement properties of each needs assessment instrument are presented in Tables 2 and 3.
Family Inventory of Needs
FIN was developed to assess both the supportive care needs of FCs of advanced cancer patients and the extent to which these needs were met as perceived by them. Guided by fulfilment theory, the development of the FIN was based on another existing scale—the Critical Care Family Needs Inventory (CCFNI)—that was developed to measure the extent to which family care needs exist [26]. A panel of family members was also involved in developing the instrument to improve the clarity, apparent internal consistency, and content validity. It was originally developed in Canada and English language [26], then translated into other languages. This instrument has 20 items in total and can be unidimensional (English and German version) and multidimensional (Czech version): basic information, information on treatment and care, support, and patient comfort. The English version was validated in 109 FCs of terminal cancer patients and showed good internal consistency, structural validity, and construct validity. Different versions showed acceptable reliability and validity (Table 2). In validation of German version, the authors found high rates of missing responses on six questions. Therefore, they suggested to exclude these six questions to increase the scale’s overall acceptability [22]. Regarding scoring and interpreting, the FIN used two-subscale scoring. One subscale measured the importance from 0 (not at all important) to 10 (very important) to indicate the importance of each need. Another subscale was answered by the options of not met (0), met (1) or not met (0), partly met (0.5), and met (1), indicating whether these needs being met. The total or mean scores were calculated for each subscale to determine the importance and degree of fulfilment of each need.
Based on this information, the three versions of FIN met 12–13 criteria of the checklist. As the German version did not provide a justification for its dimensions, a score of “0” was given to the 9th criterion. The known-group and longitudinal validity were not tested in three versions of FIN; “0” was given to the 11th and 12th criteria. Moreover, the plan for missing data and the literacy level required to understand this instrument was also not reported. Therefore, 14th and 17th criteria were rated as “0”. The average time required to complete the questions was not described. However, the FIN consists of 20 items in total, which is considered reasonable respondent burdensome. Therefore, “1” was given to the 16th criterion for all versions.
Home Caregiver Need Survey
HCNS was an instrument used to assess caregiver needs from the perspectives of “importance” and “satisfaction”. It was originally developed by Hileman et al. [30] and based on needs as perceived by the caregiver, as well as those learned from experts and literature. HCNS has 90 items in total and assesses the caregivers’ needs from six dimensions, including information, household, patient care, personal care, spiritual, and psychological needs. All items were scored using two 7-point Likert-type scales that measure the importance and satisfaction of each self-identified need. The responses range from “very important” to “not important”, and from “very satisfied” to “not satisfied”. A response is also available for “does not apply”. A higher score indicates greater importance or satisfaction. The HCNS was validated in 30 FCs of hospice cancer patients and showed acceptable reliability (internal reliability) and validity (construct validity) [24]. As HCNS has a relatively large number of items, it takes approximately 30 min for respondents to complete. The reading level of the HCNS is targeted in fifth grade.
Based on the description of HCNS, it met 12 criteria of the checklist. However, as there was no conceptual model and the convergent validity, longitudinal validity, and plan for missing data were not tested and reported, “0” were given to the 3rd, 10th, 12th, and 14th criteria. Moreover, it takes a relatively long to complete the scale; it was scored a “0” in the 16th criterion.
Questionnaire about the Needs of the Dependents of Advanced Cancer Patients
QNDCAP was developed to evaluate the support care of FCs of advanced cancer patients in the Chinese Mainland. It had a total of 36 items and involved seven dimensions: maintaining health, support from healthcare professionals, knowledge about the disease and treatment, support on funeral, information on hospice care, psychological support for patients, and symptom control for patients. These items were stemmed from literature review, clinical observations, expert consultation, and pilot investigation among caregivers. All items were rated from “high need” to “not applicable”, with scores ranging from 5 to 1. A total score and scores for different dimensions were calculated to indicate the total needs and different dimensional needs. The QNDACP was validated in 649 FCs of advanced cancer patients who were terminally ill and was found to have good reliability (internal consistency) and validity (structural validity).
Based on the above information, QNDACP met 11 criteria of the checklist. As there was no conceptual model and the convergent validity, known-group validity, longitudinal validity, and plan for missing data were not tested and reported, “0” were given to the 3rd, 10th, 11th, 12th, and 14th criteria. The literacy level required to understand the content and average completion time was not reported. However, this instrument has 36 items in total, which is reasonable. Hence, “1” and “0” were given to the 16th and 17th criteria. The items are not viewable, so the 18th criterion was rated as “0”.
Spiritual Needs Inventory
The SNI was the only included instrument specifically to assess the spiritual needs of FCs of palliative cancer patients in this review. The SNI was an instrument originally developed for patients in end-of-life care and was developed from qualitative interviews with such patients guided by Maslow’s theory of motivation as the theoretical framework [31]. Later it was validated among 410 caregivers of cancer patients receiving hospice home care and showed acceptable reliability (internal consistency) and construct validity to assess caregivers’ spiritual needs. The SNI has 17 items and assesses the caregivers’ spiritual needs from three dimensions: religious needs, outlook needs, and community needs. All items are responded with two parts. One part consists of a Likert-type scale ranging from 1 (never) to 5 (always) to indicate the extent of spiritual needs. A higher score indicates a greater spiritual need. The second part uses “yes” or “no” questions to determine whether the FCs’ needs are met.
As such, SNI met 12 criteria of the checklist. Since the conceptual model did not predefine the construct, the 3rd criterion was “0”. The content of the SNI may lack FCs’ perspectives. Therefore, a score of “0” was given to the 4th criterion. The known-group validity, longitudinal validity, and plan for missing data were not tested or reported; “0” was given to the 11th, 12th, and 14th criteria. Moreover, the literacy level required to understand the content and average completion time was not reported. However, it consists of only 17 items, which is thought to be reasonable. Hence, “1” and “0” were given to the 16th and 17th criteria.
Overall, the contents varied across different instruments. Most instruments showed acceptable reliability and validity. Among all instruments identified, none described longitudinal validity or provided instructions for dealing with missing data. Only one instrument (HCNS) defined the literacy level required to understand the questions and reported the average time for completion.
Discussion
In this review, we identified four instruments for FCs of palliative cancer patients. The four instruments addressed different aspects of FCs’ needs. The SNI specifically assesses the spiritual needs of the FCs, while the other three (FIN, HCNS, and QNDACP) assess the comprehensive needs of FCs. Instrument contents can be broadly divided into two major categories: needs relating to caregivers’ own health and well-being and support needs relevant to patients, such as patient care, funeral support, and information needs. These contents were mainly developed from literature, expert panel, pilot investigations, etc. To ensure content validity, the involvements of the intended respondent population and content experts in instrument development were assessed by the 4th and 5th criteria, respectively [21]. The experts participated in the development of three instruments (HCNS, QNDACP, and SNI) through expert consultation and panels. Caregivers were involved in the development of three instruments (FIN, HCNS, and QNDACP) by participating in reviews or pilot investigations. It has previously been suggested that target population involvement in instrument development, through qualitative reviews or focus groups, can contribute to item development and make items more relevant to the target population [21]. This is an important aspect of content validation as qualitative methods allow researchers to capture caregivers’ perspectives of their needs and evaluate their comprehension and acceptance of the items [32, 33]. However, qualitative reviews or focus groups were not applied in the development of any of the included instruments. Lacking caregivers’ qualitative perspectives may lead to missing needs that may be important for caregivers of palliative cancer patients. For example, a systematic review, which synthesised findings for the needs of FCs in palliative and hospice care, found that they need to cope with the patients’ death, such as death education and funeral support [16]. However, these kinds of needs were only mentioned in QNDACP and neglected by most of the instruments. Further development of needs assessment instruments for FCs of palliative cancer patients, involving the participation of the FCs through qualitative methods, was needed.
Ideally, every instrument should undergo some form of psychometric testing before it is used in a clinical setting, evidence-based practice project, or research study [34]. The included four instruments were validated among 30 to 649 targeted individuals. It was generally suggested that validation sampling be optimised for factor/principal component analysis-based methods and/or that there be more than 100 individuals involved [35]. Three instruments (FIN, QNDACP, and SNI) met this requirement. For the remaining one instrument validated in a limited number of target individuals, the applicability and generalisability of the instruments need to be considered.
We also found that the four instruments showed significant discrepancies in terms of the methods when evaluating the psychometric properties. The four instruments met 11 to 13 criteria of the checklist. However, none of the instruments tested all psychometric properties in the checklist. Overall, three main shortcomings were identified for the instruments examined, namely, lack of longitudinal validity, lack of a strategy for interpreting missing data, and lack of information regarding the literacy level required to understand the questions.
None of the instruments had been longitudinally validated, which requires evidence of both test-retest reliability and responsiveness to change or explicitly not intending to measure change over time. Unless the self-reported measurements were intended for cross-sectional or screening purposes, longitudinal validity was property to monitor change over time to assess the comparative effectiveness of the intervention [21]. To adequately show the responsiveness to change of an instrument, no change was expected in test-retest reliability while changes were expected in responsiveness (e.g. change in expected direction after intervention) [21]. The lack of evidence surrounding longitudinal construct validity indicated that the end-users need to consider the appropriateness of using the instruments in clinical trials to compare effectiveness. However, when the end-users intended to explore FCs’ needs at a single time, there was no need to consider this property when choosing instruments [21].
None of the instruments reported a method to handle missing data, despite this being a common phenomenon in both research and clinical practice. Missing data could lead to bias, especially when the missing responses were systematic [36]. Moreover, a significant level of missing data might lead to doubts surrounding the instrument’s applicability. Although many techniques for dealing with incomplete data existed [37], no instrument provided a specific framework. Only one instrument described the literacy level required to understand and complete the assessment. We recommend end-users assess the respondents’ literacy levels and conduct a pilot investigation to determine whether the respondents can understand the questions adequately.
Strengths and weaknesses/limitations of the study
To our knowledge, this was the first systematic review to examine the needs assessment instruments for FCs of palliative cancer patients and evaluate their psychometric properties. However, limitations should be acknowledged. Firstly, we only included English and Chinese articles, which might cause selection bias because instruments published in other languages likely exist. Secondly, although we contacted the original authors of other translated versions of the instrument for missing data or validation information, we did not get a response, or the emails were no longer valid. These missing data might have led to the exclusion of an instrument or bias of synthesis. Thirdly, the appraisal results may be prone to the risk of subjectivity, although two reviewers assessed each included instrument to minimise this risk.
Implications
As the first systematic review to synthesise needs assessment instruments for the FCs of palliative cancer patients, we identified four relevant instruments. The end-users need to have an understanding of the characteristics of the instruments before applying them for clinical or research initiatives. Through comprehensive analysis of each instrument from the contents, psychometric properties, and applicability, the review results can provide a reference for end-users when choosing needs assessment instruments for FCs of palliative cancer patients according to their own specific purposes and contexts. Despite the good evidence for some psychometric properties, further evaluation or development of needs assessment for FCs of palliative cancer patients is needed considering the limited number of instruments. As most of the instruments are used to assess the comprehensive needs, more instruments can be developed for the specific needs of FCs of palliative cancer patients.
Conclusion
Four needs assessment instruments were identified for the FCs of palliative cancer patients. However, these instruments varied significantly in terms of contents, psychometric properties, and applicability. The SNI specifically assessed the spiritual needs of the FCs, while the other three instruments (FIN, HCNS, and QNDACP) assessed the comprehensive supportive care needs of the FCs. Furthermore, the four instruments showed significant discrepancies in terms of the methods used to evaluate the psychometric properties. Three major shortcomings were found among most of the instruments: lack of longitudinal validity, lack of a strategy for interpreting missing data, and lack of a description of the literacy level required to understand the questions. Additionally, the instrument development processes assessed lacked qualitative elements. Therefore, further evaluation or development of needs assessment tools, especially to identify the specific needs of the FCs of palliative cancer patients, is warranted, with a greater emphasis on the caregivers’ perspectives. Additionally, we suggest that end-users consider the contents, psychometric properties, and applicability of each instrument when choosing an appropriate tool, according to individual purpose and context.
Availability of data and material
The authors confirm that the data supporting the findings of this study are available within the article.
Code availability
Not applicable.
References
Glajchen M (2004) The emerging role and needs of family caregivers in cancer care. J Support Oncol. 2(2):145–155
Rowland C, Hanratty B, Pilling M, van den Berg B, Grande G (2017) The contributions of family caregivers at end of life: a national post-bereavement census survey of cancer carers’ hours of care and expenditures. Palliat Med. 31(4):346–355
Maltby KF, Sanderson CR, Lobb EA, Phillips JL (2017) Sleep disturbances in caregivers of patients with advanced cancer: a systematic review. Palliat Support Care. 15(1):125–140
Areia NP, Fonseca G, Major S, Relvas AP (2019) Psychological morbidity in family caregivers of people living with terminal cancer: prevalence and predictors. Palliat Support Care. 17(3):286–293
Grande G, Rowland C, van den Berg B, Hanratty B (2018) Psychological morbidity and general health among family caregivers during end-of-life cancer care: a retrospective census survey. Palliat Med. 32(10):1605–1614
Kim Y, Carver CS, Ting A (2019) Family caregivers’ unmet needs in long-term cancer survivorship. Semin Oncol Nurs. 35(4):380–383
Hashemi M, Irajpour A, Taleghani F (2018) Caregivers needing care: the unmet needs of the family caregivers of end-of-life cancer patients. Support Care Cancer. 26(3):759–766
Fitch M (2000) Supportive care for cancer patients. Hosp Q. 3(4):39–46
Becque YN, Rietjens JAC, van Driel AG, van der Heide A, Witkamp E (2019) Nursing interventions to support family caregivers in end-of-life care at home: a systematic narrative review. Int J Nurs Stud. 97:28–39
Prue G, Santin O, Porter S (2015) Assessing the needs of informal caregivers to cancer survivors: a review of the instruments. Psychooncology. 24(2):121–129
Weldring T, Smith SM (2013) Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Serv Insights. 6:61–68
Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Lo SK, Wain G (2007) The development and evaluation of a measure to assess cancer survivors’ unmet supportive care needs: the CaSUN (Cancer Survivors’ Unmet Needs measure). Psychooncology. 16(9):796–804
Sklenarova H, Krumpelmann A, Haun MW, Friederich HC, Huber J, Thomas M, Winkler EC, Herzog W, Hartmann M (2015) When do we need to care about the caregiver? Supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer. 121(9):1513–1519
Lee J, Cha C (2017) Unmet needs and caregiver burden among family caregivers of hospice patients in South Korea. J Hosp Palliat Nurs. 19(4):323–331
Clark K (2017) Care at the very end-of-life: dying cancer patients and their chosen family’s needs. Cancers (Basel) 9(2):11–20
Zhu S, Zhu H, Zhang X, Liu K, Chen Z, Yang X, Sun C, Xie W, Xu Q, Li W, Pang D, Cui Y, Wang H (2021) Care needs of dying patients and their family caregivers in hospice and palliative care in mainland China: a meta-synthesis of qualitative and quantitative studies. BMJ Open. 11(11):e051717
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hrobjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Hartling L, Featherstone R, Nuspl M, Shave K, Dryden DM, Vandermeer B (2017) Grey literature in systematic reviews: a cross-sectional study of the contribution of non-English reports, unpublished studies and dissertations to the results of meta-analyses in child-relevant reviews. BMC Med Res Methodol. 17(1):64
Terwee CB, Prinsen CA, Ricci Garotti MG, Suman A, de Vet HC, Mokkink LB (2016) The quality of systematic reviews of health-related outcome measurement instruments. Qual Life Res. 25(4):767–779
Mokkink LB, de Vet HCW, Prinsen CAC, Patrick DL, Alonso J, Bouter LM, Terwee CB (2018) COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res. 27(5):1171–1179
Francis DO, McPheeters ML, Noud M, Penson DF, Feurer ID (2016) Checklist to operationalize measurement characteristics of patient-reported outcome measures. Syst Rev. 5(1):129–140
Schur S, Neubauer M, Amering M, Ebert-Vogel A, Masel EK, Sibitz I, Watzke H, Schrank B (2015) Validation of the family inventory of needs (FIN) for family caregivers in palliative care. Palliat Support Care. 13(3):485–491
Buzgova R, Kozakova R (2016) Psychometric evaluation of a Czech version of the family inventory of needs. Palliat Support Care. 14(2):142–150
Harrington V, Lackey NR, Gates MF (1996) Needs of caregivers of clinic and hospice cancer patients. Cancer Nurs. 19(2):118–125
Song L, Zhou L, Meng H, Zhao J (2008) Formulation, reliability and validity assessment of questionnaire about the needs of dependents of advanced cancer patients. Journal of Nursing (China) 15(6):6–9
Kristjanson LJ, Atwood J, Degner LF (1995) Validity and reliability of the family inventory of needs (FIN): measuring the care needs of families of advanced cancer patients. J Nurs Meas. 3(2):109–126
Buck HG, McMillan SC (2012) A psychometric analysis of the spiritual needs inventory in informal caregivers of patients with cancer in hospice home care. Oncology Nursing Forum. 39(4):E332–E339
Areia NP, Major S, Relvas AP (2017) Measuring family needs of people living with cancer. Portuguese validation and descriptive studies of the family inventory of needs. Eur J Oncol Nurs. 30:22–28
Fridriksdottir N, Sigurdardottir V, Gunnarsdottir S (2006) Important needs of families in acute and palliative care settings assessed with the family inventory of needs. Palliat Med. 20(4):425–432
Hileman JW, Lackey NR, Hassanein RS (1992) Identifying the needs of home caregivers of patients with cancer. Oncol Nurs Forum. 19(5):771–777
Hermann C (2006) Development and testing of the spiritual needs inventory for patients near the end of life. Oncol Nurs Forum. 33(4):737–744
Magasi S, Ryan G, Revicki D, Lenderking W, Hays RD, Brod M, Snyder C, Boers M, Cella D (2012) Content validity of patient-reported outcome measures: perspectives from a PROMIS meeting. Qual Life Res. 21(5):739–746
Patrick DL, Burke LB, Powers JH, Scott JA, Rock EP, Dawisha S, O’Neill R, Kennedy DL (2007) Patient-reported outcomes to support medical product labeling claims: FDA perspective. Value Health. 10(Suppl 2):S125–S137
Mayo AM (2015) Psychometric instrumentation: reliability and validity of instruments used for clinical practice, evidence-based practice projects and research studies. Clin Nurse Spec. 29(3):134–138
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC (2007) Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 60(1):34–42
Rotnitzky A, Wypij D (1994) A note on the bias of estimators with missing data. Biometrics. 50(4):1163–1170
Schafer JL, Graham JW (2002) Missing data: our view of the state of the art. Psychol Methods. 7(2):147–177
Author information
Authors and Affiliations
Contributions
WKWS and QQC designed the review. QQC and BBX developed the search strategies and carried out the literature screening. QQC and HLZ performed data extraction and critical appraisal and continuously discussed uncertainties with WKWS. QQC wrote this manuscript. WKWS and MSNN provided guidance and revised the manuscript critically for intellectual content. All the authors have approved the final version for publication.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheng, Q., Xu, B., Ng, M.S.N. et al. Needs assessment instruments for family caregivers of cancer patients receiving palliative care: a systematic review. Support Care Cancer 30, 8441–8453 (2022). https://doi.org/10.1007/s00520-022-07122-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-07122-2