Abstract
Purpose
Colorectal cancer (CRC) surgeries are major, complex, and often associated with debilitating symptoms or significant deconditioning that may impair patients’ quality of life. Little is known about how patients and family caregivers cope and their unmet needs during this daunting perioperative phase. This study aimed to explore the experiences and needs of CRC patients who undergo surgery and their family caregivers.
Methods
An exploratory qualitative design was adopted. A total of 27 participants comprising fifteen outpatients who had undergone colorectal cancer surgery and twelve family caregivers were recruited through purposive sampling from a public tertiary hospital in Singapore between December 2019 and November 2020. Individual, audio-recorded, semi-structured interviews were conducted, transcribed verbatim, and analyzed using thematic analysis.
Results
Four themes emerged: initial reactions to the diagnosis, impact of the illness and surgery, personal coping, and external support. The lack of apparent assessments on the psychological well-being of patients was found despite several participants exhibiting early signs of distress. Access to psychological support provided by healthcare professionals or peers was selective, and knowledge deficit was prevalent, especially in the preoperative stage.
Conclusion
Psychological priming and strengthening are important for CRC patients’ and their caregivers’ adaptive coping throughout the treatment continuum. Technology-based, dyadic psychoeducation should be offered preoperatively to ease CRC patients’ acceptance of their diagnosis and adjustment to life after surgery while at the same time reduce the burden of family carers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Colorectal cancer (CRC) is one of the top three most common cancers in both men and women globally [1]. With its rising incidence rates [2], more are expected to undergo curative surgeries, which are the mainstream treatment for this disease [3]. Over the years, despite advancements in medical technology which led to enhanced surgical outcomes and increased survival rates from 25 to 60% [4], the perioperative phase remains stressful and traumatic for some [5]. Preoperatively, CRC patients are plagued with a spectrum of overwhelming emotions including devastation, helplessness, fear and apprehension toward potential treatment complications and the fluctuating illness trajectory [6]. Postoperatively, they are confronted with fatigue, bowel incontinence, nausea or vomiting, distressing discomfort and bodily changes interjected with feelings of embarrassment and loss of dignity [7,8,9]. The double whammy of physical and psychological setbacks encountered often sends them into a state of crisis and vulnerability [10]. Caregivers, in parallel, suffer high levels of strain and burden from disrupted schedules and finances, degradations in physical health, and poor psychological health [11,12,13]. The effect of this turmoil is exacerbated by the shortened length of stay (LOS) following surgery and the shift of complex cancer recovery from hospital to home [14].
Consistent evidence has supported the need for interventions to mitigate the aforementioned detrimental effects of this disease. However, the majority of existing studies have either only examined postoperative experiences in isolation of preoperative events [7, 9, 14,15,16,17] or reported sporadic findings on potential predictors of CRC patients’ quality of life [10, 18, 19]. There is an incomplete understanding of perioperative experiences in their entirety, the extent of impact exerted by the disease and surgery, and how it shapes the individual’s response. Little is known about the coping behaviors and patterns, support availability, and unmet needs of this population and their caregivers. Furthermore, current literature also falls short in demonstrating how dyadic and social relationships define or contribute to the perioperative experience. Hence, the present study aimed to explore the perioperative experiences and needs of patients who undergo CRC surgery and their family caregivers.
Methods
Design and sampling strategy
This was a descriptive qualitative study. Potential participants were approached and recruited in person from the colorectal center of a public tertiary hospital in Singapore between December 2019 and November 2020. This center provides perioperative education, counseling, training, and follow-up medical consultations for patients with colon, rectum and anal-related disorders [20]. Eligible participants were outpatients who had undergone colorectal cancer surgery at least 1 month before this study’s commencement and/or their primary family caregivers. Those with a medical diagnosis or any known cognitive impairment(s) were excluded. To yield a diversified and panoramic understanding of this naturalistic inquiry, participants were recruited through purposive, maximum variation sampling based on the length of time since surgery, type of surgery, disease stage, presence of stoma after surgery, age, and type of patient-caregiver relationship (e.g., spouse, parent–child, and sibling). A total of 36 potential participants were approached, of which four refused participation due to time constraints, and three dropped out because they could only converse in a mixture of language and dialect that could not be transcribed. After accounting for those involved in pilot testing, the final sample comprised 27 participants.
Data collection
This study received ethical approval from the institutional review board of the study hospital. Upon obtaining written informed consent, each participant completed a socio-demographic and clinical information sheet followed by an individual, audio-recorded, semi-structured in-depth interview. The interview guide developed based on Lazarus and Folkman’s theory of stress and coping [21] was reviewed by clinical and qualitative experts and underwent pilot testing (Appendix S1). A postgraduate, female researcher (WSW) who did not have any prior interaction with the participants conducted all interviews in person (before Covid-19) or via telephone (during Covid-19). The interviewer who is a registered nurse equipped with communication skills received further training on interview techniques and approaches from her PhD supervisor (HHG). Data saturation was achieved at the 11th patient and 9th caregiver. The interviews were conducted in English and lasted between 28 and 84 min.
Data analysis
All interviews were transcribed verbatim by the interviewer alone (WSW), cross-checked for accuracy by another team member, and analyzed concurrently with data collection. Inductive thematic analysis was undertaken [10]. Audio recordings were replayed repetitively to facilitate data familiarization and immersion. Thereafter, two independent researchers performed systematic line-by-line open coding on the raw transcripts (WSW and HHG). The coding tree is displayed in Appendix S2. Triangulation of the data (i.e., the corroboration of sociodemographic, clinical and interview data from patients and caregivers) and among study team researchers took place during regular peer debriefing sessions [22]. Constant comparative analysis was utilized so that the researchers could achieve a better conceptual understanding and validate preliminary assumptions in the subsequent interviews [11]. A thematic map illustrating the connection between the themes and subthemes generated was drawn up after findings were compared and harmonized by a third researcher (CCS) (Appendix S3). The eventual set of themes and subthemes was formulated, refined, renamed, and arranged in sequence. Rigor was ensured through prolonged data engagement, consistent interviewer and transcription, keeping an audit trail, use of a reflexive diary, and researcher triangulation.
Results
A total of 27 participants (15 patients and 12 caregivers) were interviewed, comprising five patient-caregiver pairs. The characteristics of our participants are summarized in Table 1 with details of each participant shown in Appendix S4 and S5.
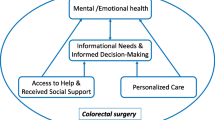
Four themes were generated from the thematic analysis of the interview data (Fig. 1): (i) initial reactions to the diagnosis; (ii) impact of the illness and surgery; (iii) personal coping; and (iv) external support. The following quotations from patients are denoted by a P and caregiver by a C to preserve anonymity.
Initial reactions to the diagnosis
This theme summarizes both patients’ and caregivers’ initial negative emotional reactions to the diagnosis that were influenced by various personal and situational factors.
Health beliefs and disease mismatch
Both patients and caregivers expressed feelings of shock and disappointment when they received news of their diagnosis, owing to preconceived ideas about healthy living and protective factors against CRC, as well as how plausible it was for the individual to have CRC based on his or her present health status. To some patients, the diagnosis did injustice to the healthy behaviors they cultivated and maintained throughout the years before the illness. One patient verbalized how upset she was when the diet regime she believed was ideal and had been adhering to could not keep her cancer-free.
So I was quite sad and worried, how come I have cancer suddenly, especially colon cancer? People who say you eat a lot of fibre things, you would not get cancer in the colon, but actually, that is not true because all my life is all vegetable. (P1)
Similar reactions of surprise and bewilderment followed by sadness and guilt were mirrored among caregivers who saw no genetic link nor found any abnormality in their care recipients’ bowel habits.
Yeah, it was a shock because… she never had any issue with her bowel and all that, only one time she went for the check-up, she got cancer already. (C6)
I thought I’ve done a fantastic job looking after their health but how would I know I missed such a very major one [care recipient having colorectal cancer]? Oh that one is a real, big surprise. We never suspect that, to be very frank. (C7)
Knowledge deficit about the disease and treatment
Both patients and caregivers were overwhelmed with many concerns at the point of diagnosis. Patients felt clueless and unprepared about the uncertainties relating to treatment, while caregivers struggled to figure out the unknowns that were necessary for the provision of care.
That time is starting to worry before the surgery… because we don’t know about how the surgery will go on all these things anyway, how it can be done, and by what sort or form of surgery you know. (P6)
In relation to cancer, well it came as a shock definitely… so it really was a new thing, we had no idea what it is about. (C11)
Patients who were more highly educated, however, displayed milder reactions to the diagnosis. They also appeared to be more forthcoming in addressing their fears and knowledge inadequacy. For instance, one patient who was a university graduate shared how he immediately acted on finding out more about CRC which was foreign to him.
It did not really affect me much, apart from telling that I should be a bit more cautious and not take life for granted. And that I must try to know much about this cancer and go for immediate assistance to arrest this situation. (P13)
Costly treatment and loss of income
Despite the caregivers reporting reasonable amounts of monthly household income per capita, our participants were stressed by hefty bills incurred from surgery and long-term expenses on follow-up treatment and purchase of medical appliances.
So initially is the financial thing is quite tough for me. (P9)
Because initially, it was for piles it is a small surgery, and so the cost was rather affordable. However, when we found out that it became a tumor, the cost was exponential and humongous. At that point in time, the fear is really around the money. (C8)
Impact of the illness and surgery
This theme puts into perspective the magnitude of disruption both patients and caregivers had to contend with after CRC surgery. Patients unanimously reported signs of functional decline as a result of restrictions and limitations in dietary options, body movements, fitness, and energy levels. This led to significant impairments in work and social activities. In the same light, caregivers encountered disruption to schedules in addition to the emotional and practical challenges faced during the provision of postoperative care.
Decreased physical capacity and disruption to work and schedules
Following surgery, a handful of patients highlighted that they could ‘no longer’ carry out certain tasks nor keep up with their usual or routine activities. Several patients experienced the crippling effects of CRC surgery, including being unable to climb stairs, squat, bend and exert strength which greatly affected work performance, self-owned businesses, and schedules.
I cannot play those ball games anymore. I can walk, but I cannot run anymore. (P3)
Like now, difficult to do my work already because my body got one stoma down here, like working that time you want to squat down, bend down like that, all very difficult already. (P12)
Some caregivers were constantly ‘on the move’. Others were physically exhausted and stretched thin from having to attend to their care recipients and fulfill other commitments simultaneously. Many caregivers had to take time off from work, balance household duties, and sort out their priorities due to the vast amount of time spent on multiple follow-up visits after the surgery.
Sometimes it affects me also because I have to run over to look after my dad, then run over to my own family to take care of my own family. So it is quite tiring, running here running there. (C4)
Ya, I quit my job to look after her because I think for her this is a big surgery and because she’s going to put a stoma, somebody will have to help her in case of changing her stoma, learning how to fix the stoma, how to clean the stoma (C12).
A minor finding observed was that those who had a live-in domestic helper were equally affected to similar extents. One caregiver indicated devoting more than 8 h a day to caregiving tasks which were heavily centered on monitoring her care recipients’ recovery progress.
Definitely not a small portion, definitely more than half of my time [spent attending to care recipient]… we have a helper but most of the time like his food I have to make sure what he eat, how many meals he eats, his diet, and make sure he’s safe, not falling down. (C10)
Conversely, those with prior caregiving experience were more ready to take on the caregiver role when such a need arose.
I’m quite prepared for it because like I said, she has been sick quite some time. (C6)
Loss of pleasure in eating and social engagement
More than half of the patients (8 out of 15) lamented the need to watch their dietary consumption, do away with specific food preferences and make changes to the way meals were prepared.
Coz I was a “foodie” person, I eat everything, I am adventurous, I enjoy eating. And because of cancer, I cannot (eat whatever I want to). Of course for me it ruins everything. (P4)
In terms of social activity, two patients reported a significant reduction in their time spent outside socializing with others.
But after the surgery, in my working place I do not mix around, I became very quiet. (P14)
To a certain extent, caregivers were also robbed of their personal time due to the constant need to ‘be there’ with and for the care recipient.
Of course, I might have no freedom [laughs] for a while because I need to stay with him all the time. (C10)
Altered bowel pattern and stoma-related challenges
Although changes to bowel habits after surgery were common, some patients suffered from severe bowel symptoms to the point of resorting to diaper use. Those with stoma had their fair share of difficulty manipulating and finding the best fit for the appliance to function well.
Leakage is one of the main issues because every day I have to be worrying about whether the bag will overflow…because it happened where the bag is too heavy and the whole thing just, you know, just… snapped and dropped. (P10)
One caregiver recounted a panic episode of having to rush over from one location to another to attend to her mother’s leaking stoma bag.
I had an experience where my mum was outside. I was outside too, but we were at different places and her stoma suddenly got leakage, she had to call me, “Emergency! Come quickly, come and fix my stoma.” (C12)
Personal coping
This theme illustrates the coping patterns and strategies used by our participants throughout their surgery and caregiving experience. Participants’ coping strategies followed a staged approach and often included a combination of self-help techniques.
Accept, face, and go through the journey
Acceptance was a critical approach undertaken by most of our participants in response to the fluctuating course of CRC throughout the perioperative phase. According to their narratives, acceptance was attained through the recalibration of one’s mindset so that one no longer resists but reconciles with sickness being part and parcel of life and recognizes the need for treatment to recover from the illness.
Have to accept it, whatever. I mean during that period what type of food to take…go according to the instruction of the doctor. (P5)
Yeah, so we just accepted things as they were. (C5)
Rationalize and do ‘what I can’
Some participants attempted to make sense of what had happened, rationalized what could and needed to be done next and pursued what helped move forward, such as avoiding pessimistic or excessive thinking and instead, motivating themselves to confront their fears bravely.
I have to face it and overcome the fear. Umm, that is the main thing I can do... to overcome all the fear and to follow the doctor's instructions. (P10)
I am very calm, yeah, of course, I feel upset that he has this illness. But I have to face it, I cannot tell why. Since I do not know why, so I can only do whatever I can do. (C10)
Build positive self-talk and look forward
Participants also elaborated how they subsequently engaged in positive self-talk through statements such as “I can manage” and “I will survive”, as well as look forward to recovery and tell themselves to “be strong” for significant others to keep their spirits up.
Keeping and thinking positive, like ‘tomorrow will be good’. (P11)
I just have to tell myself I try to be strong for her. (C6)
Take practical actions
Besides positive reframing, a few patients normalized the sick role by continuing with their daily activities. Some proactively adopted a more flexible lifestyle, set time aside for personal hobbies, or devised personalized strategies to optimize stoma care and accommodate the demands of the illness.
My usual routine thing I just do accordingly like nothing happen… Don’t behave like you are so pitiful. (P5)
This method of problem-focused coping was more prevalent among caregivers, as evidenced by how caregivers in general sourced for practical ways to adapt and relieve themselves from the occasional stress build-up.
Initially, maybe we are not too sure what is the best way [to care for the stoma]. Then as we go along, we find ‘oh this is better, or this angle is better [referring to attaching the stoma appliance].’ You learn it along the way. (C3)
Swimming is the one I can relax… so when I’m at my parents’ place the whole day, when they have nothing, I just watch my own programme, when they need then I attend to them. (C7)
External support
This theme expounds on the various types and sources of support received or deemed lacking by our respondents during the perioperative period.
Emotional encouragement and companionship
Almost all participants acknowledged receiving emotional support. For patients, support came through informal counseling, companionship, words of reassurance, encouragement, comfort, and concern. For caregivers, support came through exchanging relatable experiences with others, opportunities to confide, vent frustrations, and psychological preparation from listening to survivors' stories. Several participants drew strength through religious prayers.
And I have a great husband, who is very supportive, plus my son and my daughter-in-law, they are all very nice. They will come and talk to me, laugh, and they have a good laugh and joke. (P3)
They will come and then we will sit and talk, then we will eat together, all these. (C1)
Some patients and caregivers likewise also illuminated how the relationship with each other influenced mutual coping through the spread of negative mood or positive energy.
My family is very encouraging, they told me do not worry, everything will be okay… so I was not worried much about this thing. (P8)
My mum has been very optimistic, so her positive attitude also helped us in a sense to move on. (C12)
Information and instructional guidance
Patients appreciated healthcare professionals for keeping them informed in advance with relevant and valuable instructions about their treatment.
I think the doctors and nurses gave a lot of advice, support, useful information – what is going on with me and what would be the outcome after surgery or chemo. (P10)
On the contrary, caregivers expressed their needs for more detailed information on the following: how to prepare their care recipients for surgery, how to manage symptoms after the surgery, and reliable information about available home-care services, as shown by their lack of confidence in the provision of care after their care recipients’ discharge from the hospital.
I think it would be good to conduct some seminars or some information sessions to equip the caregivers on how to look after patients with a stoma… and the food they can take and how. Maybe some recipes about how to cook the food to help those caregivers to make sure that patients can recover better. (C12)
Tangible assistance and government subsidies
Our respondents described diverse forms of practical support. For patients, these included help with changing their stoma appliance, cooking, washing, and grocery shopping, among other household chores, as well as fetching or accompanying them for medical appointments. Three patients received financial aid (i.e. subsidies or grants) for their medical care through the hospital’s medical social worker.
My wife every day she cooks for me, fish, protein, soup all these. She took care of me, you know. And then see a doctor also every time go with me together. (P6)
For caregivers, support came in the form of family members providing relief to their caregiving duties and having supportive leaders at their workplace who granted work flexibility.
It really helps me a lot, coz if my father needs help, like umm, he wants to go for his check-ups, sometimes my husband is not working, or he is on leave, he will be accompanying me and my father. (C4)
Follow-up help and services
A couple of patients were provided with helplines, which they could turn to under non-emergency situations.
(If there is) anything, there is a hotline (for patients) to call them. If in doubt…there is a cancer hotline. (P6)
In contrast to the resources availed to patients, the lack of follow-up initiatives communicated by caregivers reflected an unmet need that was essential for caregiving as well as maintaining their well-being.
Umm…the other thing is the department can ask the caregivers whether they have any problem… then advise them or let them know. (C3)
Discussion
To our knowledge, this is the first study to encapsulate insights from both CRC patients and family caregivers to solicit a comprehensive understanding of their experiences and needs throughout the entire perioperative continuum. Like other cancers, the CRC diagnosis aroused a spectrum of unpleasant responses which were similar to those previously identified [5, 9, 16, 17, 23]. However, our study was unique in elucidating the deep-seated misconceptions and wrongful assumptions behind these negative emotions, which were more evident among the less-educated respondents. Upon diagnosis, many patients raced to deny any health-harming behaviors. However, some were not aware of the warning cues for colorectal cancer. The lack of knowledge about CRC misled them into assuming that they had been in good health all along and that CRC would more likely occur in others who were less health-conscious or had pre-existing illnesses. Moreover, patients’ perceptions of CRC were largely shaped by their loved ones’ encounters and unfounded rumors on how fatal, aggressive and disabling the disease was. As such, they became vulnerable to the danger of fear, despair and pessimism. This was also true of those who without understanding, heavily relied on information provided by their primary physician, although such a source of support was vital before operation [24]. That being said, this phenomenon should not be taken lightly as the resultant appraisal of CRC as a perceived threat may impede coping [25]. Efforts to eradicate unhelpful emotions and impart knowledge about CRC should begin as early as from the point of diagnosis [26], and our findings lend support to the need for psychoeducation interventions.
Congruent to earlier qualitative studies, our participants cited varying degrees of change to their lifestyles after surgery, and caregivers were not spared from these disruptions [14,15,16, 27]. Again, those with a stoma and their caregivers experienced greater distress and appeared to be constantly on tenterhooks because of unprecedented ostomy-related mishaps [28, 29]. These findings attest to why quantitative studies often report a poorer quality of life in this group [30, 31]. Moreover, although prior caregiving experience gave advantage to quicker assimilation into the caregiver role [32], it was interesting to discover that the presence of a live-in domestic helper did not seem to alleviate caregivers of their burden. This could be due to the multiple and sparsely arranged medical appointments caregivers had to be involved in. Additionally, the constant need for caregivers to “be present” implied that their care recipients were dependent on them to a substantial extent. Given the positive correlation between patient self-efficacy and caregiver physical health [33], there is an imperative need for more interventions targeted at enhancing self-efficacy. Otherwise, caregivers will be at risk of physical burnout and psychological morbidity when attending to care recipients with adjustment issues over extended periods of time [34, 35].
The coping techniques and types of support delineated by our participants were synonymous with previous findings [36,37,38]. However, our study revealed CRC patients to be more emotionally focused as opposed to caregivers who were more problem-focused. Information-seeking behaviors and greater demand for access to external care services, self-training courses, follow-up help, and resources may reflect the responsibility caregivers take to prepare themselves for decision-making moments. However, clinicians should be careful not to encourage passiveness among patients when providing informational support. Differences aside, it may be advantageous to leverage these complementary coping styles when designing future dyadic interventions. Meanwhile, the current practice of availing peer support only to those deemed to be at risk of distress should also be reviewed. The merit of peer support should not be undermined as it can potentially bridge gaps between self-care and professional help [39], and promote the active reconstruction of life after surgery.
Study limitations
This study recruited patients of varying duration since surgery. Although the diversity was intentional, our findings may have been limited by recall bias. Secondly, the selection of outpatients may have inadvertently filtered out those severely affected by the surgery. In this regard, readers should exercise discretion on our findings’ transferability based on the provided background and contextual descriptions.
Conclusion
Having known the perioperative journey to be an arduous one, clinicians ought to upscale the provision and availability of training, educational and psychosocial resources to match this population’s multifaceted perioperative needs and coping styles. Besides optimizing physical and psychological prehabilitation, regular, formal mental health assessments are crucial for detecting morbidity, especially among caregivers who are not direct care recipients. In light of the current Covid-19–related face-to-face restrictions and time constraints faced by caregivers in particular, healthcare providers ought to consider the use of novel interactive health technologies in the remote delivery of psychosocial care. Finally, peer support and dyadic psychosocial interventions should be incorporated into surgery care paths in order for the effect of Enhanced Recovery Protocols (ERPs) to be fully harnessed.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Code availability
Not applicable.
References
Douaiher J, Ravipati A, Grams B, Chowdhury S, Alatise O, Are C (2017) Colorectal cancer-global burden, trends, and geographical variations. J Surg Oncol 115(5):619–630
Keum N, Giovannucci E (2019) Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol 16(12):713–732
Gustafsson UO, Scott MJ, Hubner M, Nygren J, Demartines N, Francis N et al (2019) Guidelines for perioperative care in elective colorectal surgery: enhanced recovery after surgery (ERAS®) society recommendations: 2018. World J Surg 43(3):659–695
Chawla N, Butler EN, Lund J, Warren JL, Harlan LC, Yabroff KR (2013) Patterns of colorectal cancer care in Europe, Australia, and New Zealand. J Natl Cancer Inst Monogr 2013(46):36–61
Hildebrandt C, Mayer H, Koller A (2019) Experiences of patients with colorectal cancer from diagnosis until completion of treatment: a meta-ethnography approach. Psychooncology 28(2):219–227
Worster B, Holmes S (2008) The preoperative experience of patients undergoing surgery for colorectal cancer: a phenomenological study. Eur J Oncol Nurs 12(5):418–424
Landers M, McCarthy G, Savage E (2012) Bowel symptom experiences and management following sphincter saving surgery for rectal cancer: a qualitative perspective. Eur J Oncol Nurs 16(3):293–300
Nikoletti S, Young J, Levitt M, King M, Chidlow C, Hollingsworth S (2008) Bowel problems, self-care practices, and information needs of colorectal cancer survivors at 6 to 24 months after sphincter-saving surgery. Cancer Nurs 31(5):389–398
Worster B, Holmes S (2009) A phenomenological study of the postoperative experiences of patients undergoing surgery for colorectal cancer. Eur J Oncol Nurs 13(5):315–322
Graça Pereira M, Figueiredo AP, Fincham FD (2012) Anxiety, depression, traumatic stress and quality of life in colorectal cancer after different treatments: a study with Portuguese patients and their partners. Eur J Oncol Nurs 16(3):227–232
Maguire R, Hanly P, Hyland P, Sharp L (2018) Understanding burden in caregivers of colorectal cancer survivors: what role do patient and caregiver factors play? Eur J Cancer Care 27:e12527. https://doi.org/10.1111/ecc.12527
Hanly P, Maguire R, Hyland P, Sharp L (2015) Examining the role of subjective and objective burden in carer health-related quality of life: the case of colorectal cancer. Support Care Cancer 23(7):1941–1949
Cal A, Avci IA, Cavusoglu F (2017) Experiences of caregivers with spouses receiving chemotherapy for colorectal cancer and their expectations from nursing services. Asia Pac J Oncol Nurs 4(2):173–179
Mizuno M, Kakuta M, Ono Y, Kato A, Inoue Y (2007) Experiences of Japanese patients with colorectal cancer during the first six months after surgery. Oncol Nurs Forum 34(4):869–876
Lim SH, Chan SW, He HG (2015) Patients’ experiences of performing self-care of stomas in the initial postoperative period. Cancer Nurs 38(3):185–193
Lu LC, Huang XY, Chen CC (2017) The lived experiences of patients with post-operative rectal cancer who suffer from altered bowel function: a phenomenological study. Eur J Oncol Nurs 31:69–76
Jonsson CA, Stenberg A, Frisman GH (2011) The lived experience of the early postoperative period after colorectal cancer surgery. Eur J Cancer Care 20(2):248–256
Gray NM, Hall SJ, Browne S, Macleod U, Mitchell E, Lee AJ et al (2011) Modifiable and fixed factors predicting quality of life in people with colorectal cancer. Br J Cancer 104(11):1697–1703
Yost KJ, Hahn EA, Zaslavsky AM, Ayanian JZ, West DW (2008) Predictors of health-related quality of life in patients with colorectal cancer. Health Qual Life Outcomes 6(1):66
National University Hospital N. Surgery (2020) Available from: https://www.nuh.com.sg/our-services/Specialties/Surgery/Pages/default.aspx. Accessed 22 Feb 2021
Lazarus RS, Folkman S (1984) Stress, Appraisal, and Coping: Springer Publishing Company
Silverman D (2006) Interpreting Qualitative Data: Methods for Analyzing Talk, Text and Interaction. SAGE Publications
Changyai K, Kongvattananon P, Somprasert C (2020) The experiences of colorectal cancer patients in postoperative recovery: integrative review. J Health Res 34(3):259–269
Beaver K, Latif S, Williamson S, Procter D, Sheridan J, Heath J et al (2010) An exploratory study of the follow-up care needs of patients treated for colorectal cancer. J Clin Nurs 19(23–24):3291–3300
Anderson AS, Steele R, Coyle J (2013) Lifestyle issues for colorectal cancer survivors–perceived needs, beliefs and opportunities. Support Care Cancer 21(1):35–42
Foster C, Haviland J, Winter J, Grimmett C, Chivers Seymour K, Batehup L et al (2016) Pre-Surgery depression and confidence to manage problems predict recovery trajectories of health and wellbeing in the first two years following colorectal cancer: results from the CREW Cohort Study. PLoS One 11(5):e0155434
Mosher CE, Adams RN, Helft PR, O’Neil BH, Shahda S, Rattray NA et al (2016) Family caregiving challenges in advanced colorectal cancer: patient and caregiver perspectives. Supportive Care Cancer 24(5):2017–2024
Liao C, Qin Y (2014) Factors associated with stoma quality of life among stoma patients. Int J Nurs Sci 1(2):196–201
Alwi F, Setiawan, Asrizal (2018) Quality of life of persons with permanent colostomy: a phenomenological study. J Coloproctology 38(4):295–301
Campos Kd, Bot LHB, Petroianu A, Rebelo PA, Souza AACd, Panhoca I (2017) The impact of colostomy on the patient’s life. J Coloproctology 37(3):205–10
Cotrim H, Pereira G (2008) Impact of colorectal cancer on patient and family: implications for care. Eur J Oncol Nurs 12(3):217–226
Scherbring M (2002) Effect of caregiver perception of preparedness on burden in an oncology population. Oncol Nurs Forum 29(6):E70–E76
Kershaw T, Ellis KR, Yoon H, Schafenacker A, Katapodi M, Northouse L (2015) The interdependence of advanced cancer patients’ and their family caregivers’ mental health, physical health, and self-efficacy over time. Ann Behav Med 49(6):901–911
Fitzell A, Pakenham KI (2010) Application of a stress and coping model to positive and negative adjustment outcomes in colorectal cancer caregiving. Psychooncology 19(11):1171–1178
ÖztürkKaynar G, Vural F (2018) Assessment of the caregiver burden of caregivers of colorectal cancer patients. Turk J Colorectal Dis 28(4):164–171
Asiedu GB, Eustace RW, Eton DT, Radecki BC (2014) Coping with colorectal cancer: a qualitative exploration with patients and their family members. Fam Pract 31(5):598–606
Houldin AD (2007) A qualitative study of caregivers’ experiences with newly diagnosed advanced colorectal cancer. Oncol Nurs Forum 34(2):323–330
Abelson JS, Chait A, Shen MJ, Charlson M, Dickerman A, Yeo H (2019) Coping strategies among colorectal cancer patients undergoing surgery and the role of the surgeon in mitigating distress: a qualitative study. Surgery 165(2):461–468
Bui LL, Last L, Bradley H, Law CH, Maier BA, Smith AJ (2002) Interest and participation in support group programs among patients with colorectal cancer. Cancer Nurs 25(2):150–157
Acknowledgements
We appreciate the immense support from all medical and nursing staff at the Colorectal Centre of the National University Hospital, Singapore. We thank Dr Jennie Wong, Medical & Scientific Communications, Research Support Unit, National University Health System, Singapore, for editing this manuscript and the Centre for Medical Education at the National University of Singapore for providing methodological expertise. Our heartfelt gratitude goes to all participants who were willingly and graciously sharing their valuable experiences.
Funding
This study was funded by the 2018 Singapore Cancer Society grant.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, participant recruitment and data collection were conducted by Wan Su Wei, Chong Choon Seng, and Jee Xin Pei, and analysis performed by Wan Su Wei, Chong Choon Seng and He Hong-Gu. The first draft of the manuscript was written by WAN Su Wei and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study received ethical approval from the National Healthcare Group-Domain Specific Review Board (NHG DSRB ref no.:2019/00846) in Singapore on 26 November 2019 and conformed to standards by the Declaration of Helsinki. Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wan, S.W., Chong, C.S., Jee, X.P. et al. Perioperative experiences and needs of patients who undergo colorectal cancer surgery and their family caregivers: a qualitative study. Support Care Cancer 30, 5401–5410 (2022). https://doi.org/10.1007/s00520-022-06963-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-022-06963-1