Abstract
Background
Frailty is emerging as an important determinant for health. Compared with Western countries, research in the field of frailty started at a later stage in China and mainly focused on older community dwellers. Little is known about frailty in Chinese cancer patients, nor the risk factors of frailty. This study aimed at investigating the prevalence of frailty and its risk factors in elderly inpatients with gastric and colorectal cancer.
Methods
This cross-sectional study was conducted at a tertiary hospital in China from Mar. 2020 to Nov. 2020. The study enrolled 265 eligible inpatients aged 60 and older with gastric and colorectal cancer who underwent surgery. Demographic and clinical characteristics, biochemical laboratory parameters, and anthropometric data were collected from all patients. The Groningen Frailty Indicator was applied to assess the frailty status of patients. A multivariate logistic regression model analysis was performed to identify the risk factors of frailty and to estimate their 95% confidence intervals.
Results
The prevalence of frailty in elderly inpatients with gastric and colorectal cancer was 43.8%. A multivariate logistic regression analysis showed that older age (OR = 1.065, 95% CI: 1.001–1.132, P = 0.045), low handgrip strength (OR = 4.346, 95% CI: 1.739–10.863, P = 0.002), no regular exercise habit (OR = 3.228, 95% CI: 1.230–8.469, P = 0.017), and low MNA-SF score (OR = 11.090, 95% CI: 5.119–24.024, P < 0.001) were risk factors of frailty.
Conclusions
This study suggested a relatively high prevalence of frailty among elderly inpatients with gastric and colorectal cancer. Older age, low handgrip strength, no regular exercise habit, and low MNA-SF score were identified as risk factors of frailty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The aging population is accelerating rapidly. As of the end of 2017, there were 241 million people aged 60 and older in China, accounting for 17.3% of the total population [1]. Age, is an important risk factor for cancer, as extended lifespan is often accompanied by increased exposure to carcinogenic factors and the prolonged accumulation of genetic changes [2]. Gastric and colorectal cancers are common worldwide, respectively, ranking the third and fifth in terms of incidence but the second and third in terms of mortality, as reported in Global Cancer Statistics 2018 [3]. In China, a large proportion of new cancer cases are diagnosed at age 60 years and older [4], with age-related declines in the immunity system [5], organs function, and physical performance [6], thus posing a challenge to promote patients’ recovery and reduce their adverse clinical outcomes.
Frailty, the most problematic aspect of population aging [7], refers to the state of increased vulnerability for the development of increased dependency and/or death when being exposed to stressors [8]. As per previous studies, it can be observed that frailty is an important risk factor for the prediction of postoperative complications [9], readmission [10], and mortality [11] in cancer patients who accepted surgery. For those older cancer patients, the internal complicated biological changes of aging, together with immune senescence, inflammation, age-related chronic diseases, and external environmental and psychosocial factors, can have an impact on the development of individual malignancies, as well as on the patients’ physiological reserves and vulnerability [12]. Besides, frailty was also significantly associated with worse long-term health-related quality of life in older patients with breast cancer [13]. As we all know, both cancer itself and cancer treatments can be significant additional stressors that challenge the physiological reserves of older patients, all of which could increase the risk of frailty. It is also challenging for clinical staff to decide the optimum treatment for older patients who are heterogeneous in terms of comorbidities, disability, physical reserves, and geriatric conditions [14]. Therefore, the geriatric frailty assessment should be applied to provide an appropriate surgical risk assessment for clinical staff to help guide cancer treatments.
Although there is no golden standard for the assessment of frailty [15], several common frailty assessment tools have been used in clinical practices. The comprehensive geriatric assessment (CGA) is a systematic procedure for the detection of vulnerability in elderly cancer patients, focusing on functional, somatic, and psychosocial domains [14]. Nevertheless, conducting CGA is time-consuming [14] and may not be feasible in an oncology ward with limited resources. The Groningen Frailty Indicator (GFI), originally developed by Steverink et al. [16], is a frailty screening tool with good predictive performance [17], and it has been widely used for screening frailty in cancer patients. Recently, Xiang et al. [18] has translated the GFI into Chinese, and the Chinese version of GFI displays good internal consistency (Cronbach’s α = 0.712), excellent test–retest reliability (ICC = 0.939), and satisfactory criterion validity (AUC = 0.823) among Chinese nursing home residents.
Compared with Western countries, research in the field of frailty started at a later stage in China and mainly focused on older community dwellers [19]. It has been reported in recent studies that the prevalence of frailty among Chinese community residents aged 60 and older, with the results ranging from 38.6 to 60.5% based on the GFI criterion [18, 20]. A meta-analysis by He et al. [21] showed that being female, increasing age, ADL disability, and developing three or more chronic diseases were risk factors for frailty in older community dwellers. However, to our best knowledge, little is known about the prevalence of frailty in Chinese cancer patients, nor the risk factors of frailty. Therefore, the aim of this study was to investigate the prevalence of preoperative frailty in elderly inpatients with gastric and colorectal cancer and to further explore the factors that were associated with frailty in this population.
Material and methods
Study design and participants
The patients who successfully underwent surgery participated in this cross-sectional study, and they were all consecutively recruited from the First Affiliated Hospital of Anhui Medical University (Anhui province, China) from Mar. 2020 to Nov. 2020. The inclusion criteria were as follows: (1) diagnosed with gastric or colorectal cancer; (2) ≥ 60 years old; (3) had normal upper and lower limbs mobility; and (4) signed an informed consent. The exclusion criteria were as follows: (1) with precancerosis, mesothelioma, or benign lesions by postoperative histopathology; (2) recurrence of gastric/colorectal cancer or tumor metastasis; (3) admission for acute intestinal obstruction/gastrointestinal hemorrhage; and (4) with poor cardio-pulmonary function or severe infection/inflammation within 1 month.
Ethical considerations
Ethical approval was granted by the Clinical Medical Research Ethics Committee of the First Affiliated Hospital of Anhui Medical University (No. PJ2020-03–29). This study conformed to the standards of the Declaration of Helsinki and was registered with the Chinese Clinical Trial Registry (No. ChiCTR2000031250).
Laboratory parameters
After a 12-h overnight fast, all patients’ preoperative venous blood samples, including plasma protein (prealbumin, PA; albumin, ALB; globulin, GLO; total protein, TP), blood routine (white blood cell, WBC; red blood cell, RBC; hemoglobin, HGB; reticulocyte, RET; lymphocyte, LYMPH), and tumor markers (alpha-fetoprotein, AFP; carcino-embryonic antigen, CEA; carbohydrate antigen 125, CA125; carbohydrate antigen 19–9, CA19-9; carbohydrate antigen 72–4, CA72-4), were collected together in the morning. Plasma protein, blood routine, and tumor markers were detected with an automatic chemistry analyzer (Cobas 8000, Roche, Germany), an automatic blood analyzer (XN-9000, Sysmex, Japan), and an automatic electrochemiluminescence immunoassay analyzer (Cobas 6000, Roche, Germany), respectively. Tumor stage, area, and histological grade were also collected after finishing surgery.
Demographic and clinical characteristics
A self-designed questionnaire that included sex, age, body mass index (BMI), educational degree, marriage status, smoking/drinking history, past medical history, regular exercise habit, preoperative chemoradiotherapy, cancer type, and blood transfusion before or after surgery, was used to collect the general demographic and clinical data of all patients. Regular exercise habit was defined as participants who did at least 30 min of moderate-intensity exercise (e.g., jogging and brisk walking) per time, with no less than 5 times per week. Smoking/drinking history was defined as the patients who are currently smoking cigarettes/drinking alcohol, or they used to smoke cigarettes/drink alcohol, but they are now abstaining from smoking cigarettes/drinking alcohol.
GFI questionnaire
Frailty was assessed with the self-report version of GFI that has been revised by Peters et al. [22], and it contains 15 items on physical, cognitive, social, and psychological domains. The answer to each item has a score of either 0 or 1, with 1 indicating a dependent problem. The total score of GFI ranges from 0 to 15, and higher scores indicate greater frailty. The cut-off value of GFI ≥ 3 was considered frail in geriatric oncology [17]. The GFI was proved to show moderate internal consistency (Cronbach’s α ranged from 0.68 to 0.712) [18, 22]. All patients filled out the GFI questionnaires within 3 days of their hospital admission for surgery. All items in the revised and Chinese versions of GFI were shown in the Appendix.
Short-Form Mini-Nutritional Assessment (MNA-SF) questionnaire
The MNA-SF, revised by Rubenstein et al. [23] based on the Mini-Nutritional Assessment, is a validated tool to screen malnourished hospitalized patients. The sensitivity, specificity, and diagnostic accuracy of MNA-SF for the prediction of malnutrition were 97.9%, 100%, and 98.7%, respectively [23]. It contains 6 items, namely, weight loss, BMI, stress or illness, mobility, dementia or depression, and loss of appetite. The total score of MNA-SF ranges from 0 to 14, with the score > 11 (≤11) being well-nourished (at risk of malnutrition or malnutrition). The trained researchers routinely obtained patients’ MNA-SF scores within 3 days of their hospital admission for surgery.
Handgrip strength
Preoperative handgrip strength was measured in kilograms (kg) with a handheld dynamometer based on the digital strain gauge sensors (Jamar® Plus + , Performance Health Supply, Inc., Cedarburg, WI, USA). Measurements were conducted with the patients seated, shoulders adducted and neutrally rotated, elbow in 90° flexion, and the forearm and twist in a neutral position [24]. All patients were asked to squeeze the dynamometer as much as possible with the dominant hand. The test was performed twice with a rest interval of at least 30 s, and the maximum value of the two tests was recorded. If the two results differed over 10%, a third test would be carried out [25]. Low handgrip strength was defined as < 26 kg for male and < 18 kg for female [26].
Four-meter walk test
Preoperative walking speed was carried out by means of a 4-m walk test, adding 2 m at the beginning and the end of the walkway, which was provided for acceleration or deceleration [27]. Patients in standing still position were asked to walk at their usual pace (normal gait speed) with or without using auxiliary aids (e.g., canes and walkers). Walking time was recorded by trained researchers using a digital stopwatch (PS-60, China) from the moment that the patient’s first foot crossed the 2-m line until the moment that the patient’s first foot completely crossed the 6-m line. The test was performed twice, and the shortest time was applied for analysis. Slow gait speed was defined as ≤ 0.8 m/s [26].
Mid-upper arm circumference (MUAC) and calf circumference (CC)
Preoperative MUAC and CC were measured to the nearest 0.1 cm with a non-elastic tape (Deli, China) without compressing the subcutaneous tissue. MUAC was measured at the mid-point around the arm between the acromion and the ulnar olecranon, with the patient’s upper limbs in a state of natural hanging [28]. CC was measured around the widest part of the calf, with the patients standing with their legs shoulder-width apart [28].
Statistical analysis
The Kolmogorov–Smirnov test was conducted to verify the normal distribution of continuous variables. All data were expressed as mean ± standard deviation, or median and inter-quartile range, or frequency numbers (percentages). Differences in demographic and clinical characteristics and biochemical laboratory parameters data between frail and non-frail patients were tested using two independent-samples t test or non-parametric test. To determine the risk factors that were associated with frailty, and to estimate their 95% confidence intervals (CI), independent variables with a P value < 0.05 (set at a stringent level) on univariate analysis as described above were entered into a multivariate logistic regression model analysis by adopting the Forward LR method. Data analyses were performed with SPSS 23.0 software package (IBM, Armonk, NY, USA). A two-tailed P value < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics in all patients
Overall, 330 (100%) patients from the general surgery ward signed the informed consent and were all successfully screened for frailty. Among them, a total of 65 (19.7%) patients were excluded for poor cardiac function/tumor metastasis by MRI/CT (n = 12), refusing/waiting for surgery (n = 25), performing exploratory laparotomy without successfully resecting tumor (n = 10), and nonmalignant tumor/diffuse large B cell lymphoma by postoperative histopathology (n = 18). Hence, 265 (80.3%) patients were included in the final analysis, with 116 (43.8%) in the frail group and 149 (56.2%) in the non-frail group. The detailed process of recruiting subjects was shown in Fig. 1.
As seen in Table 1, when compared with the non-frail group, the frail group tended to be older and contained more females (less males) (P < 0.05). MUAC, CC, 4-m gait speed (Slow gait speed: 24.1% vs. 8.7%), handgrip strength (Low strength: 31.9% vs. 5.4%), and MNA-SF score (Low score: 91.4% vs. 47.7%) were significantly lower in the frail group than that in the non-frail group (P < 0.05). The frail group had significantly less regular exercise habits (79.3% vs. 92.6%) and more blood transfusion before or after surgery (23.3% vs. 12.1%) compared with the non-frail group (P < 0.05). However, no significant differences in BMI, educational degree, marriage status, smoking/drinking history, Charlson comorbidity index, and preoperative chemoradiotherapy were found between the two groups of subjects (P > 0.05).
Biochemical laboratory parameters in all patients
The comparisons of biochemical laboratory parameters between the two groups were presented in Table 2. HGB, PA, and ALB were significantly lower in the frail group than that in the non-frail group (P < 0.05), while the tumor area was significantly higher in the frail group than that in the non-frail group (P < 0.05). However, no significant differences in WBC, RBC, RET, LYMPH, GLO, TP, AFP, CEA, CA125, CA19-9, CA72-4, cancer type, T stage, N stage, M stage, histological grade, and signet ring cells on histological examination were discovered between the two groups of subjects (P > 0.05).
Description of variable assignment
The assignment of the dependent variable and significant independent variables was described in Table 3.
Risk factors of frailty in patients with gastric and colorectal cancer
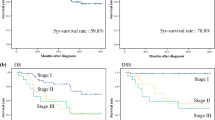
The multivariate logistic regression analysis showed that older age (OR = 1.065, 95% CI: 1.001–1.132, P = 0.045), low handgrip strength (OR = 4.346, 95% CI: 1.739–10.863, P = 0.002), no regular exercise habit (OR = 3.228, 95% CI: 1.230–8.469, P = 0.017), and low MNA-SF score (at risk of malnutrition or malnutrition) (OR = 11.090, 95% CI: 5.119–24.024, P < 0.001) were identified as risk factors of frailty in inpatients with gastric and colorectal cancer (see Fig. 2).
Discussion
This study currently investigated the frailty status of elderly inpatients with gastric and colorectal cancer with a GFI instrument and also analyzed its risk factors. The results showed that the prevalence of frailty was 43.8% and that older age, low handgrip strength, no regular exercise habit, and low MNA-SF score were risk factors of frailty.
To date, the prevalence of frailty in cancer patients is inconsistent worldwide. A systematic review has pooled 20 studies evaluating 2,916 older cancer patients mainly from North America and Europe, suggesting that the median prevalence of frailty was 42% [29]. It can be observed that the prevalence of frailty was similar to the results of our study. However, the review also revealed that the prevalence of frailty varies greatly among different studies (range 6–86%) due to the differences in the content and approach of frailty assessment [29]. For cancer patients, cancer itself can be one of the significant additional stressors that challenges patients’ physiologic reserve, and thus the prevalence of frailty in older cancer patients is usually higher [30]. In addition, various cancer types (e.g., urological, colorectal, breast, and lung), assessment instruments (e.g., CGA, phenotype, GFI, FRAIL, and FI), and research sites (e.g., inpatient, outpatient, and general practice) may also contribute to the differences of frailty prevalence in this population [29, 30]. Chinese researchers have reported that the prevalence of frailty among elderly inpatients ranged from 18 to 36.2% [19, 31]. However, the details of specific disease types among inpatients in these studies were unclear. Another Chinese study showed that the prevalence of frailty in gastric cancer patients aged 80 and over was 32.7% based on the three baseline frailty traits, namely, albumin, hematocrit, and creatinine [9]. Given the inconsistent results on the frailty prevalence, and especially higher in cancer patients, clinical staff should promptly assess the frailty status of those people. Subsequently, a series of measures such as personalized exercise, combined with nutrition supplements containing dairy, protein-rich foods, fruits, and nuts, as well as cognitive training, should be taken to reduce the burden of frailty on this population.
Age is an important risk factor of frailty in this study. It has been shown in a systematic review that the risk of frailty in the elderly people increased significantly with the increase of age [21]. As mentioned earlier, older patients experienced much more age-related biological changes, multiple diseases, diseases treatments, and social-psychological factors, all of which may eventually induce the onset of frailty [12]. The aging process can be depicted as a time-dependent decline in physiological organ function, resulting in the development of diseases, including cancer [32]. To a certain extent, the related toxicity of cancer treatments could cause severe impairments in the body function, and some evidences have proved that cancer treatments might be associated with accelerated aging [33]. Considering these facts, aging, cancer, and cancer treatments might interact with the onset of frailty.
Low handgrip strength was identified as an important risk factor of frailty in the present study. Handgrip strength serves as a reliable proxy index of an individual hand motor abilities [34], and measuring handgrip strength is a simple and feasible measure of muscle strength [26]. Xue et al. [35] conducted a prospective cohort study of 352 elderly women and observed that lower baseline handgrip strength was significantly correlated with the higher risk of frailty, which was consistent with our findings. Interestingly, Puts et al. [36] put forward that in newly diagnosed elderly cancer patients, only low grip strength could predict therapeutic toxicity, which may help clinicians gain insight into the effects of cancer treatments. In addition, for older adults of the same age, handgrip strength might be a more important single marker of frailty than chronological age alone [37]. Furthermore, it has been proved to be an effective screening tool for frailty in older patients with newly diagnosed hematological cancer [38]. Based on these facts, we could understand that handgrip strength is closely connected with frailty in both normal individuals and cancer patients.
No regular exercise habit usually meant physical inactivity or being sedentary, and it was significantly associated with frailty in our study. Haider et al. [39] concluded that among community dwellers, performing no regular physical activity was substantially linked with the higher risk of frailty, which was in line with our findings. In addition, da Silva et al. [40] also indicated that among Brazilian older adults, the frailty prevalence increased with physical inactivity combined with excessive time spent in sedentary behavior. Hopefully, accumulating studies [41, 42] give the information that physical activity offers a model of improving the function of dysregulated multiple physiologic systems, thereby preventing or alleviating the progress of frailty.
Low MNA-SF score implied that these patients were at risk of malnutrition or malnutrition, and it was an important risk factor of frailty in the present study. This result was consistent with an earlier study [43], which indicated that low MNA score (at risk of malnutrition/malnutrition) was strongly correlated with frailty (OR = 2.72 and OR = 17.4, respectively) among 6,045 older community residents in Singapore. Recently, Liu et al. [44] showed that poor nutritional status was associated with an increased risk of frailty (OR = 2.66) among 705 Chinese nursing home residents. Meanwhile, Gabrovec et al. [45] also highlighted that malnutrition or being at risk of malnutrition were risk factors of frailty in aging. Nevertheless, Zhang et al. [46] revealed that frailty was significantly associated with the risk of malnutrition (OR = 3.82) in older cancer patients. We speculated that the close connection between frailty and malnutrition in cancer patients might be attributed to share common pathophysiological pathways, including inflammation, reduced body tissue, cognitive disorder, poor physical performance, and pernicious sociodemographic characteristics [47]. Malnutrition is common in older cancer patients and is mostly caused by tumor invasion, side effects of cancer treatments, cachexia, and anorexia of aging. Consequently, there is an urgent need for clinical staff to early identify malnutrition in these patients and then take targeted therapy to improve their nutritional status.
Although we did hope to explore some specific disease-related risk factors of frailty among these elderly cancer patients, the findings of this study only displayed some non-specific common factors in this population. As a result, there are several inevitable limitations in our study. Firstly, we did not detect laboratory biomarkers, as several potential biomarkers that might be involved in the development of frailty. Secondly, this was an observational study and the underlying cellular and molecular mechanisms of frailty were far from being understood, thus necessitating further researches to elucidate this. Thirdly, this study was performed at a single center, and multicenter studies should be conducted soon. Apart from this, the long-term outcomes of cancer patients after surgery such as complications and mortality should also be concerned in the future.
In conclusion, the prevalence of frailty is relatively high among elderly inpatients with gastric and colorectal cancer in this study. Older age, low handgrip strength, no regular exercise habit, and low MNA-SF score are risk factors of frailty. Frailty is emerging as an important determinant for health and the mentioned risk factors should be considered when implementing interventions to improve the health outcomes of frail cancer patients.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author after the paper is published.
Code availability
N/A
References
241 million people aged 60 and older in China, accounting for 17.3% of the total population (online). Available at: www.gov.cn/xinwen/2018-02/26/content_5268992.htm. Accessed 26 Feb 2018 (in Chinese)
Swaminathan D, Swaminathan V (2015) Geriatric oncology: problems with under-treatment within this population. Cancer Biol Med 12(4):275–283
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66(2):115–132
Nikolich-Zugich J (2018) The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol 19(1):10–19
Milanovic Z, Pantelic S, Trajkovic N, Sporis G, Kostic R, James N (2013) Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging 8:549–556
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K (2013) Frailty in elderly people. The Lancet 381(9868):752–762
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J et al (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397
Lu J, Cao LL, Zheng CH, Li P, Xie JW, Wang JB, Lin JX, Chen QY, Lin M, Tu RH et al (2017) The preoperative frailty versus inflammation-based prognostic score: which is better as an objective predictor for gastric cancer patients 80 years and older? Ann Surg Oncol 24(3):754–762
Choe YR, Joh JY, Kim YP (2017) Association between frailty and readmission within one year after gastrectomy in older patients with gastric cancer. J Geriatr Oncol 8(3):185–189
Tegels JJ, de Maat MF, Hulsewe KW, Hoofwijk AG, Stoot JH (2014) Value of geriatric frailty and nutritional status assessment in predicting postoperative mortality in gastric cancer surgery. J Gastrointest Surg 18(3):439–445 (>discussion 445-436)
Zhang X, Meng X, Chen Y, Leng SX, Zhang H (2017) The biology of aging and cancer: frailty, inflammation, and immunity. Cancer J 23(4):201–205
Williams GR, Deal AM, Sanoff HK, Nyrop KA, Guerard EJ, Pergolotti M, Shachar SS, Reeve BB, Bensen JT, Choi SK et al (2018) Frailty and health-related quality of life in older women with breast cancer. Support Care Cancer 27(7):2693–2698
Hamaker ME, Jonker JM, de Rooij SE, Vos AG, Smorenburg CH, van Munster BC (2012) Frailty screening methods for predicting outcome of a comprehensive geriatric assessment in elderly patients with cancer: a systematic review. Lancet Oncol 13(10):e437–e444
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP (2019) Frailty: implications for clinical practice and public health. The Lancet 394(10206):1365–1375
Steverink N, Slaets JPJ, Schuurmans H, Lis MV (2001) Measuring frailty: developing and testing the GFI (Groningen frailty indicator). Gerontologist 41(1):236–237
Baitar A, Van Fraeyenhove F, Vandebroek A, De Droogh E, Galdermans D, Mebis J, Schrijvers D (2013) Evaluation of the Groningen Frailty Indicator and the G8 questionnaire as screening tools for frailty in older patients with cancer. J Geriatr Oncol 4(1):32–38
Xiang W, Cheng Y, Li Z, Han J, Li K (2020) Cross-cultural adaptation and validation of the Groningen Frailty Indicator in Chinese nursing home residents. Aging Clin Exp Res 32(6):1035–1042
Liang YD, Zhang YN, Li YM, Chen YH, Xu JY, Liu M, Li J, Ma Z, Qiao LL, Wang Z et al (2019) Identification of frailty and its risk factors in elderly hospitalized patients from different wards: a cross-sectional study in China. Clin Interv Aging 14:2249–2259
Tian X, Qiao X, Dong L, Liu N, Si H, Jin Y, Liu X, Wang C (2020) Cross-cultural adaptation and psychometric properties of the Groningen Frailty Indicator (GFI) among Chinese community-dwelling older adults. Geriatr Nurs 41(3):236–241
He B, Ma Y, Wang C, Jiang M, Geng C (2019) X Chang, Ma B, Han L: Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and meta-analysis. J Nutr Health Aging 23(5):442–450
Peters LL, Boter H, Buskens E, Slaets JP (2012) Measurement properties of the Groningen Frailty Indicator in home-dwelling and institutionalized elderly people. J Am Med Dir Assoc 13(6):546–551
Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56(6):M366-372
Fess E, Moran C (1981) Clinical assessment recommendations, 1st edn. American Society of Hand Therapists, Chicago
Stenholm S, Sallinen J, Koster A, Rantanen T, Sainio P, Heliovaara M, Koskinen S (2011) Association between obesity history and hand grip strength in older adults—exploring the roles of inflammation and insulin resistance as mediating factors. J Gerontol A Biol Sci Med Sci 66(3):341–348
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O et al (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15(2):95–101
Peters DM, Fritz SL, Krotish DE (2013) Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther 36(1):24–30
Yang LJ, Wu GH, Yang YL, Wu YH, Zhang L, Wang MH, Mo LY, Xue G, Wang CZ, Weng XF (2019) Nutrition, physical exercise, and the prevalence of sarcopenia in elderly residents in nursing homes in China. Med Sci Monit 25:4390–4399
Handforth C, Clegg A, Young C, Simpkins S, Seymour MT, Selby PJ, Young J (2015) The prevalence and outcomes of frailty in older cancer patients: a systematic review. Ann Oncol 26(6):1091–1101
Ethun CG, Bilen MA, Jani AB, Maithel SK, Ogan K, Master VA (2017) Frailty and cancer: implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin 67(5):362–377
Yang F, Chen QW (2018) Evaluation of frailty and influencing factors in old people in hospital institution: evidence for a phenotype of frailty. Medicine (Baltimore) 97(3):e9634–e9640
Aunan JR, Watson MM, Hagland HR, Soreide K (2016) Molecular and biological hallmarks of ageing. Br J Surg 103(2):e29-46
Hurria A, Jones L, Muss HB (2016) Cancer treatment as an accelerated aging process: assessment, biomarkers, and interventions. Am Soc Clin Oncol Educ Book 35:e516–e522
Ong HL, Abdin E, Chua BY, Zhang Y, Seow E, Vaingankar JA, Chong SA, Subramaniam M (2017) Hand-grip strength among older adults in Singapore: a comparison with international norms and associative factors. BMC Geriatr 17(1):176
Xue Q, Walston JD, Fried LP, Beamer BA (2011) Prediction of risk of falling, physical disability, and frailty by rate of decline in grip strength: the women’s health and aging study. Arch Intern Med 171(12):1119–1121
Puts MT, Monette J, Girre V, Pepe C, Monette M, Assouline S, Panasci L, Basik M, Miller WH Jr, Batist G et al (2011) Are frailty markers useful for predicting treatment toxicity and mortality in older newly diagnosed cancer patients? Results from a prospective pilot study. Crit Rev Oncol Hematol 78(2):138–149
Syddall H, Cooper C, Martin F, Briggs R, Sayer AA (2003) Is grip strength a useful single marker of frailty? Age Ageing 32(6):650–656
Velghe A, De Buyser S, Noens L, Demuynck R, Petrovic M (2016) Hand grip strength as a screening tool for frailty in older patients with haematological malignancies. Acta Clin Belg 71(4):227–230
Haider S, Grabovac I, Drgac D, Mogg C, Oberndorfer M, Dorner TE (2020) Impact of physical activity, protein intake and social network and their combination on the development of frailty. Eur J Public Health 30(2):340–346
da Silva VD, Tribess S, Meneguci J, Sasaki JE, Garcia-Meneguci CA, Carneiro JAO, Virtuoso JS Jr (2019) Association between frailty and the combination of physical activity level and sedentary behavior in older adults. BMC Public Health 19(1):709–714
Fried LP (2016) Interventions for human frailty: physical activity as a model. Cold Spring Harb Perspect Med 6(6):a025916
Nascimento CM, Ingles M, Salvador-Pascual A, Cominetti MR, Gomez-Cabrera MC, Vina J (2019) Sarcopenia, frailty and their prevention by exercise. Free Radic Biol Med 132:42–49
Wei K, Nyunt MSZ, Gao Q, Wee SL, Ng TP (2017) Frailty and malnutrition: related and distinct syndrome prevalence and association among community-dwelling older adults: Singapore longitudinal ageing studies. J Am Med Dir Assoc 18(12):1019–1028
Liu W, Chen S, Jiang F, Zhou C, Tang S (2020) Malnutrition and physical frailty among nursing home residents: a cross-sectional study in China. J Nutr Health Aging 24(5):500–506
Gabrovec B, Veninsek G, Samaniego LL, Carriazo AM, Antoniadou E, Jelenc M (2018) The role of nutrition in ageing: a narrative review from the perspective of the European joint action on frailty- ADVANTAGE JA. Eur J Intern Med 56:26–32
Zhang X, Pang L, Sharma SV, Li R, Nyitray AG, Edwards BJ (2019) Prevalence and factors associated with malnutrition in older patients with cancer. J Geriatr Oncol 10(5):763–769
Norazman CW, Adznam SN, Jamaluddin R (2020) Malnutrition as key predictor of physical frailty among Malaysian older adults. Nutrients 12(6):1713–1724. https://doi.org/10.3390/nu12061713
Acknowledgements
We would like to thank all volunteers who participated in this study for their effort and precious time.
Funding
This work was funded by the Clinical Medicine Discipline Construction Project of Anhui Medical University (No. 2020lcxk032).
Author information
Authors and Affiliations
Contributions
Study concepts and design: Qianqian Zhang, Yanyan Zhang, Shihui Yu, and Aman Xu. Data acquisition: Qianqian Zhang and Meng Zhang. Quality control of data and algorithms: Shihui Yu and Aman Xu. Data analysis and interpretation: Meng Zhang and Shaohua Hu. Statistical analysis: Lei Meng and Jing Xi. Manuscript preparation: Qianqian Zhang, Shaohua Hu. Manuscript editing: Jing Xi, Lei Meng, and Yanyan Zhang. Manuscript review: Shihui Yu and Aman Xu.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the Clinical Medical Research Ethics Committee of the First Affiliated Hospital of Anhui Medical University (No. PJ2020-03–29) and complied with the Declaration of Helsinki.
Consent to participate
All participants were fully informed about the research purpose before they provided signed consent.
Consent for publication
All authors critically reviewed the manuscript and approved the final version submitted for publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Q., Zhang, M., Hu, S. et al. Prevalence and risk factors of preoperative frailty in Chinese elderly inpatients with gastric and colorectal cancer undergoing surgery: a single-center cross-sectional study using the Groningen Frailty Indicator. Support Care Cancer 30, 677–686 (2022). https://doi.org/10.1007/s00520-021-06483-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-021-06483-4